![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
82 Cards in this Set
- Front
- Back
|
cardiovascular (circulatory) system consists of the:
|
1. Heart - which serves as a pump to maintain an adequate flow of blood
2. Blood vessels - which serve as a closed system of ducts to transport blood, beginning and ending at the heart * The heart and blood vessels function together to push blood to and from the organs, tissues, and cells of the body |
|
|
circulatory system
|
* manages the delivery of oxygen and nutrients and the removal of carbon dioxide and waste products by way of:
1. Arteries, arterioles, and capillaries, which carry oxygen-rich blood away from the heart to nourish the body 2. Veins and venules - which carry oxygen-poor blood back through the heart to the lungs for oxygenation and removal of wastes * one of the body systems that ages visibly * also transports nutrients from digested food to the body |
|
|
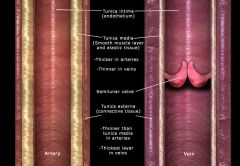
tunica externa or tunica adventitia
|
* made of connective tissue of blood vessels or fibers to reinforce the wall of the vessel so that it will not burst under pressure
* outermost coat of a blood vessel (arteries and veins) * thinner than tunica media in arteries * thickest layer in veins |
|
|
phlebitis
|
* inflammation of a vein
commonly caused by: irritation by an intravenous catheter |
|
|
ischemia
|
* decreased blood supply to a tissue, involves the gradual death of cells and may lead to complete tissue death
* reduced flow of blood to tissue resulting in impairment of cell function. * ischemia of heart muscle can lead to a heart attack |
|
|
necrosis
|
* complete tissue death
* due to an obstruction or loss of blood supply to an area causing death to the tissue, which eventually results in gangrene |
|
|
tunica intima
|
* endothelium cells
* innermost coat of a blood vessel (arteries and veins) * actually a single layer of squamous epithelial cells called endothelium that lines the inner surface of the entire circulatory system. * Prevents the accidental formation of blood clots * sometimes includes a thing layer of elastic fibrous tissue |
|
|
aneurysm
|
* weakening of the arterial wall
* an abnormal widening of an arterial wall due to weakening. * sometimes form a saclike extension of the arterial wall * promote the formation of thrombi, which can turn into an embolism (blockage) in the heart or other vital tissue. * have a tendency to burst, causing severe hemorrhaging that may result in death. * a brain aneurysm may lead to a stroke, or CVA cerebrovascular accident. |
|
|
hemorrhoids
|
* varicose veins of the rectum
* caused by straining during defecation creating pressure, this can also cause varices of the rectum * common during pregnancy from the pressure of carrying a child aka. piles * treatment: advanced cases is surgery. symptoms of milder cases can be relieved by removing the pressure that caused the condition. |
|
|
arteries
|
* carry oxygen-rich blood away from the heart to nourish the body (toward the arterioles) and then to the capillaries in all parts of the body
* 20 major arteries make a path through your tissues, where they branch into smaller vessels called arterioles which further branch into capillaries. * Thick tunica media (elastic fibers) * Thin tunica externa (connective tissue) * No valves * Largest artery in the body is the aorta * has 3 coats of structure: tunica externa, tunica media and tunica intima * Most of the time, arteries carry oxygenated blood ie. arch of aorta is an artery |
|
|
arterioles
|
* carry oxygen-rich blood away from the heart to nourish the body to capillaries in all parts of the body.
* Arterioles further branch into capillaries * by constricting or dilating, arterioles help maintain arterial blood pressure at a normal level. * smallest of the arteries * composed primarily of smooth muscle and spend most of their time contracting and relaxing * by changing their diameter, the arterioles affect resistance to the flow of blood * a narrow vessel offers an increased resistance to blood flow and a wider vessel offers less resistance to blood flow. |
|
|
capillaries
|
* where the actual exchange of nutrients and respiratory gases occurs between the blood and tissue fluid around the cells - in capillary beds
* After the capillaries deliver oxygen and nutrients to the tissues and pick up carbon dioxide and other waste, they return the blood back through wider vessels called venules * extreme thinness, extremely thin - only one layer of flat, endothelial cells composes (the tunica intima) the capillary membrane instead of three layers or coats * helps carry oxygen-rich blood away from the heart to nourish the body * microscopic * substances such as glucose, oxygen, and wastes can quickly pass through it on their way to or from cells. * function as exchange vessels. ie. glucose and oxygen move out of capillaries into interstitial fluid and then into cells; Carbon dioxide and other substances move in the opposite direction (into the capillary blood from the cells). fluid is also exchanged between capillary blood and interstitial fluid. |
|
|
veins
|
* deliver the blood back to your heart to pick up oxygen from the capillaries
* Carry blood away from the capillaries and toward the heart * Thin tunica media (elastic fibers) * Thick tunica externa (connective tissue) * Have valves to prevent pooling of blood in the extremities * Largest vessels (veins) are the superior vena cava and inferior vena cava * has 3 coats of structure: tunica externa or tunica adventitia, tunica media and tunica intima * also serve as blood reservoirs because they carry blood under lower pressure (than arteries) and can expand to hold a larger volume of blood or constrict to hold a much smaller amount of blood. * have a unique feature of one-way valves not present in arteries. * help carry oxygen-poor blood back through the heart to the lungs for oxygenation and removal of wastes * Most of the time veins carry deoxygenated blood |
|
|
venules
|
* they return the blood back to the heart from the capillaries
* eventually increase in size and form veins * also serve as blood reservoirs because they carry blood under lower pressure (than arteries) and can expand to hold a larger volume of blood or constrict to hold a much smaller amount of blood. * help carry oxygen-poor blood back through the heart to the lungs for oxygenation and removal of wastes |
|
|
tunica media
|
* middle layer of tunica in blood vessels (arteries and veins) made of smooth muscle tissue so its controlled by the autonomic nervous system
* it is thicker in arteries to resist great pressures generated by ventricular systole * thinner in veins * critical in arteries to maintain blood pressure and controlling blood distribution |
|
|
Disorders of Blood Vessels
|
one of the body systems that ages visibly
* The walls of the arteries thicken and become less elastic. * Blood flow to vital organs decreases and blood pressure begins to increase. * Varicose veins (varices) may appear. * Breathing often becomes more labored, activity decreases, and cardiac symptoms may occur as the circulatory system progresses through the life span. treatment: Medication and surgical procedures have allowed us to live with, or correct, many of these disorders successfully. |
|
|
balloon angioplasty
|
* catheter is inserted into the vessel until it reaches the affected region. a probe with a metal tip is pushed out the end of the catheter into the blocked region of the vessel. the balloon is inflated, crushing the plaque in order to restore blood flow. sometimes stents are inserted to keep the vessel open
* 70% of procedures use a stent * other types of angioplasty use lasers, drills, or spinning loops or wire to clear blockage |
|
|
stent
|
* a metal coil or stent that is inserted during balloon angioplasty to keep a vessel open
|
|
|
atherosclerosis
|
* caused by the lipid buildup and other matter on the walls of the vessels.
* high blood levels of blood lipids such as triglycerides and cholesterol are associated with this disease. * a type of arteriosclerosis * can be caused by high-fat, high-cholesterol diet, smoking, genetic predisposition |
|
|
arteriosclerosis
|
* disorder characterized by thickening of arterial walls that progresses to hardening as calcium deposits form reducing blood flow to the tissues.
* "hardening of the arteries" * occludes (blocks) arteries and weakens arterial walls * painful and can be life threatening * develops with advanced age, diabetes, high-fat, high-cholesterol diet, hypertension, and smoking * treatment: vasodilator drugs |
|
|
vasodilators
|
* drugs that trigger the smooth muscle of the arterial walls to relax, thus causing the arteries to dilate or widen.
|
|
|
vasoconstrictors
|
* drugs that cause the arteries to constrict, reducing the flow of blood to an area.
|
|
|
great saphenous
|
* the largest and longest superficial vein of the leg
|
|
|
anterior tibial
|
* smaller vein of the leg
|
|
|
thrombus
|
* stationary blood clot
* may eventually cause an embolism if it becomes dislodged. |
|
|
gangrene
|
* necrosis that has progressed to the point of decay
|
|
|
Arterial blood flow:
|
1. pumped from the heart
2. through the arteries 3. arterioles 4. capillaries or capillary beds 5. venules 6. veins |
|
|
aorta
|
* the largest artery in the body
* caries blood out of the left ventricle of the heart |
|
|
venae cavae
|
* both inferior and superior vena cava return blood to the right atrium after the blood has circulated through the body
|
|
|
precapillary sphincters
|
* smooth muscles that guard the entrances to the capillaries and determine how much blood will flow into each capillary bed.
|
|
|
stroke or CVA cerebrovascular accident
|
* results from ischemia of brain tissue caused by an embolism or ruptured aneurysm
* effects can range from hardly noticeable to crippling to fatal depending on the amount of affected tissue. |
|
|
varicose veins
|
* veins in which blood tends to pool rather than continue on toward the heart
* also called varices * most commonly occur in superficial veins near the face of the body * great saphenous vein often becomes varicose in people who stand for long periods. * force of gravity slows the return of venous blood to the heart causing blood engorged veins to dilate. as they dilate the distance between the flaps of venous valves widens, eventually making them incompetent (leaky) * incompetence of valves causes even more pooling in affected veins - a positive feedback phenomenon. * treatment: by supporting the dilated veins from the outside. ie. support stockings. severe cases use surgical removal |
|
|
thrombophlebitis
|
* acute phlebitis caused by clot formation. more likely in veins because venous blood moves more slowly and is under less pressure than arteries
* characterized by pain and discoloration of the surrounding tissue. |
|
|
pulmonary embolism
|
* when an embolus lodges in the circulation of the lung
* can lead to death quickly if too much blood flow is blocked. |
|
|
jugular
|
* vein that returns blood from the head
|
|
|
two main circulatory systems
|
* provides oxygenated blood to the body tissues and cells.
1. Pulmonary circulation consists of the blood vessels that extend between the heart and the lungs and the capillary network, where the actual exchange of gases takes place. 2. Systemic circulation consists of the blood vessels that extend from the left ventricle to the right atrium of the heart. |
|
|
Hepatic portal circulation
|
* refers to blood flows (circulation) through the liver
* process by which nutrients enter the blood by passing through the walls of the intestine and are absorbed through a network of capillaries and veins in the intestines * carries nutrients to the liver for further metabolism * here blood mixes with the arterial blood in the capillaries and is eventually drained from the liver by the hepatic veins that join the inferior vena cava * advantages of this detour of blood from the digestive tract through the liver is that the liver plays such a critical role in metabolism, it needs an easy access to the digestive end products. * this circulation allows excess glucose to be removed from the blood and to be stored as glycogen in the liver before entering the general circulation; therefore blood leaving the liver has a normal blood glucose concentration. * liver cells remove and detoxify various poisonous substances that may be present in the blood. * an example of how "structure follows function" in maintaining homeostasis. * diverted venous blood is sent through a second capillary bed in the liver. once blood exits the liver capillary beds it returns to the systemic blood pathway, returning to the right atrium of the heart. * veins that use the hepatic portal vein and that DO NOT pour their blood directly into the inferior vena cava are spleen, stomach, pancreas, gallbladder, and intestines. |
|
|
Fetal circulation
|
* is circulation through the body of a fetus before birth
* in the fetus, the lungs are collapsed and the digestive organs are still immature and unable to function as needed * there are two umbilical arteries and one umbilical vein * fetal circulation differs from circulation after birth * The foramen ovale shunts blood from the right atrium directly into the left atrium. |
|
|
ductus arteriosus
|
* vessel that allows blood to bypass fetal lungs
* structure that detours blood normally routed to the lungs and lets it flow straight into the aorta and on to the rest of the body. * a small vessel connecting the pulmonary artery with the descending thoracic aorta |
|
|
foramen ovale
|
* structure that shunts blood between the atria in fetus
* shunts blood from the right atrium directly into the left atrium * actually a hole in the middle wall, or septum of the heart which allows blood in the right side to flow through the wall into the left side and out to the rest of the body. * allows blood to bypass the lungs * at birth when baby takes its first breath, increased pressure from the circulatory system results in closure of the foramen ovale and a rapid collapse of the umbilical blood vessels, the ductus venosus, and the ductus arteriosus. * congenital disorders may prevent this shift at birth from happening. |
|
|
ductus venosus
|
* vessel that allows blood to bypass fetal liver
* a continuation of the umbilical vein, serves as a shunt, or bypass which allows most of the blood returning from the placenta to be diverted from the immature liver of the fetus and emptied directly into the inferior vena cava |
|
|
Systemic Circulation
|
* circulation that connects the heart, organs, and tissues and supplies oxygen to them. It also picks up carbon dioxide and other wastes from the cells and returns them to the heart
* blood leaves the heart through the aorta and then travels to all the organs of the body through arteries, returning to the heart through the systemic veins * Arteries, which are usually colored red in diagrams, always carry blood away from the heart. * Veins, which are usually colored blue in diagrams, always carry blood toward the heart. systemic circulation blood flow (step 1) 1. left atrium 2. mitral or bicuspid valve 3. left ventricle 4. aortic semilunar valve 5. aorta 6. arteries of each organ 7. arterioles of each organ 8, capillaries of each organ 9. venules of each organ 10. veins of each organ 11. superior vena cava and inferior vena cava 12. into the right atrium - beginning of pulmonary circulation |
|
|
Pulmonary Circulation
|
* carries blood to and from the lungs, connects the heart and lungs
* venous blood leaves the heart through the pulmonary arteries, goes to the lungs, and then returns to the heart, with oxygen, by means of the pulmonary veins * an exception to the "Veins carry deoxygenated blood and arteries carry oxygenated blood" rule. * After leaving the right ventricle for the lungs, the pulmonary arteries carry deoxygenated blood, which is why they are usually colored blue in diagrams. They must be identified as arteries, however, because they are carrying blood away from the heart. * The pulmonary veins carry oxygenated blood from the lungs and return it to the heart, which is why they are usually colored red in diagrams. Because they are going toward the heart, they are identified as veins. venous blood = deep crimson color arterial blood = scarlet color pulmonary circulation blood flow (step 2): 1. superior vena cava and inferior vena cava 2. right atrium through the tricuspid valve to the 3. right ventricle - then pumped through the pulmonary semilunar valve into the 4. Pulmonary artery 5. lungs 6. capillaries 7. pulmonary veins 8. left atrium |
|
|
Venous blood
|
* is deoxygenated blood which travels from the left ventricle, through the systemic circulation en route to the right atrium.
* Deoxygenated blood is then pumped by the heart to lungs via the pulmonary arteries, one of the few arteries in the body that carries deoxygenated blood (the pulmonary veins likewise return the newly oxygenated blood to the heart). * venous blood = deep crimson color * Venous blood, from the upper portions of the body, drains into the right side of the heart by means of the superior vena cava |
|
|
pulmonary veins
|
* carry oxygenated blood from the lungs and return it to the heart,
* 4 veins - 2 from each lung |
|
|
pulmonary arteries
|
* carry deoxygenated blood from the right ventricle to the lungs.
|
|
|
liver
|
* stores a variety of substances—such as sugars, fats, and vitamins—releases these to the blood as needed
* also filters the blood by removing waste products and toxins. After the blood has crossed the liver cells, veins converge to form the large hepatic vein that joins the inferior vena cava near the right atrium. |
|
|
vena cava
|
* veins that DO NOT pour their blood directly into the inferior vena cava are spleen, stomach, pancreas, gallbladder, and intestines.
|
|
|
placenta
|
* located in the mother's uterus allows the passage of both oxygen and nutrients from the mother's blood through a membrane to the baby's blood.
three vessels that pass oxygen and nutrients from the placenta to the baby and back: 1. umbilical arteries - 2 small arteries - carries oxygen-poor blood away from the heart 2. umbilical vein - single much larger vein - carries oxygenated blood toward the heart 3. umbilical cord * from there if flows through the umbilical vein into the baby. with the lungs collapsed there is no need for the right side of the heart to send blood to the lungs; the blood is already oxygen rich thanks to the placenta. two shortcuts that allow blood to bypass the lungs. 1. ductus arteriosis 2. foramen ovale |
|
|
blood circulation
|
* blood flows through vessels that are arranged in a complete circuit or circular pattern
|
|
|
hepatic portal vein
|
* located between two capillary beds - one located in the digestive organs and the other in the liver.
|
|
|
hole in the heart
|
* when the foramen ovale fails to close or remain closed after birth which allows blood to bypass the pulmonary circulation
* baby's skin might appear bluish because of the lack of oxygen in the systemic arterial blood. |
|
|
cyanosis
|
* condition of bluish tissue coloration
|
|
|
Blood pressure
|
* the force that blood exerts against the walls of the blood vessels as it flows through the circulatory system.
* It is highest in the arteries and lowest in the veins * it is referred to as one of the vital signs * a stronger heartbeat increases blood pressure and a weaker beat decreases it. * normal blood pressure is below 120/80 or 120 mmHg systolic pressure and 80 mmHg diastolic pressure - normal varies by individuals and age |
|
|
Hypotension
|
* low blood pressure, low arterial blood pressure
* prevents adequate blood flow to vital organs and can cause shock. * can cause circulation and life to cease. ie. massive hemorrhage |
|
|
Hypertension (HTN)
|
* high blood pressure or high arterial blood pressure
* can place additional strain on the heart and lungs, damage the kidneys, and create health issues for several other vital organs. * if too high it may cause the rupture of one or more blood vessels * more visits to a physician's office are related to hypertension than any other factor; more than 60 million cases in the US * high considered over 140/90 mmHg * 90% of cases are classified as primary-essential, or idiopathic, with no single known causative etiology. primary HTN * secondary HTN - is caused by kidney disease or hormonal problems or induced by oral contraceptives, pregnancy or other causes. * high-normal range also called prehypertension * risk factors = genetics, men have higher rates at an earlier age than women, african americans have higher rates than caucasions, and age. high stress levels, obesity, calcium deficiencies, high levels of alcohol and caffeine intake, smoking and lack of exercise. * untreated can lead to - ischemic heart disease, heart failure, kidney failure, and stroke. * known as "the silent killer" because it has minimal or no overt signs. * treatment: diuretics - as water is lost from the body, blood volume decreases so blood pressure decreases |
|
|
vital signs
|
1. temperature
2. pulse 3. respirations 4. blood pressure |
|
|
Sphygmomanometer
|
* device used to measure blood pressure
* the cuff is inflated with sufficient air pressure to collapse the artery. |
|
|
systolic
|
* maximum arterial pressure
* first Korotkoff sound is the systolic pressure, sounds will continue to change in tone and loudness until they stop (which is the diastolic pressure) * pressure during ventricular contraction and the maximal arterial pressure during each cardiac cycle. |
|
|
blood pressure gradient
|
* blood pressure hill
* difference between two blood pressures * for the entire systemic system circulation = the difference between the average or mean blood pressure in the aorta and the blood pressure at the termination of the venae cavae where they join the right atrium of the heart. * when a blood pressure gradient is present, blood circulates * when a blood pressure gradient is absent blood does not circulate. * 100 mm represents the average pressure in each part of the circulatory system. |
|
|
central venous (pressure)
|
* pressure within the right atrium that influences the pressure existing in the large peripheral veins
* if the heart beats strongly, the central venous pressure is low as blood enters and leaves the heart chambers efficiently. * if the heart is weakened, central venous pressure increases and the flow of blood into the right atrium is slowed, ie. person suffering heart failure, who is sitting at rest in a chair, often has distended external jugular veins as blood "backs up" in the venous network Five mechanisms help to keep venous blood moving back through the circulatory system and into the right atrium: 1. continued beating of the heart, which pumps blood through the entire circulatory system 2. Adequate blood pressure in the arteries, to push blood to and through the veins 3. Semilunar valves in the veins that ensure continued blood flow in one direction (toward the heart) 4. Contraction of skeletal muscles, which squeeze veins, producing a kind of pumping action. 5. Changing pressures in the chest cavity during breathing that produces a kind of pumping action in the veins in the thorax. |
|
|
diastolic
|
* minimum arterial pressure
* when the Korotkoff sounds completely stop when taking your blood pressure * represents the point which the artery is completely open and blood flows freely. * the pressure that occurs during cardiac relaxation |
|
|
Physiology of Blood Pressure
|
* Blood flows down a hill known as the blood pressure gradient. Since pressure is highest in the arteries, the peak of the hill is highest in the arteries
* The gradient begins to decline in the arteries and continues on to the arterioles, where the pressure lessens. It proceeds into the capillaries, where the pressure becomes even lower. * From the capillaries, the hill continues the descent into venules, then to the small veins, progressing to the large veins and finally into the superior vena cava and inferior vena cava to return to the heart, where it has now reached the lowest pressure on the gradient. * the pressure drop across the arterioles is the greatest |
|
|
Factors Affecting Blood Pressure
|
* blood volume, strength of heart contractions, heart rate, and blood viscosity are just a few of the circumstances that can alter blood pressure
* it is important to monitor blood pressure on a regular basis. |
|
|
Korotkoff sounds
|
* caused by decreased pressure while taking your blood pressure
* represent the first flow of blood through the collapsed artery that can be heard through a stethoscope. * first sound is the systolic pressure |
|
|
volume of blood
|
* the direct cause of blood pressure is the volume of blood in the vessels.
* can effect blood pressure * the larger the volume of blood in the arteries, the more pressure the blood exerts on the walls of the arteries and the higher the arterial blood pressure. * an increase in the rate of the heartbeat increase blood pressure if the blood volume also increase. |
|
|
blood viscosity
|
* refers to the thickness of blood
* can effect blood pressure * if blood becomes less viscous than normal (thinner), blood pressure decreases ie. hemorrhage will dilute blood. * after a hemorrhage, transfusion of whole blood or plasma is preferred to saline because saline is not a viscous (thick) liquid and can't keep blood pressure at a normal level. |
|
|
polycythemia
|
* condition when the number of red blood cells increases beyond normal and thus increases blood viscosity, which increases blood pressure
* can occur when oxygen levels in the air decrease and the body attempts to increase its ability to attract oxygen to the blood - ie. working in high altitude. |
|
|
Pulse
|
* what you feel is an artery that is alternately expanding and recoiling
* caused by ejection of blood from the ventricle and can be felt anywhere an artery is close to the surface and rests against something firm. * easily detected by placing the fingers over a superficial artery and over a bone or other firm base. * The pulse offers valuable information regarding the rate, strength, and rhythm of the heartbeat * Like blood pressure, it is considered a vital sign for healthcare assessment * There are nine body areas where the pulse can be detected with relative ease. These areas are known as pulse points. 1. radial artery - base of thumb or wrist area 2. temporal artery - temple 3. carotid - base of neck 4. facial - bottom left side of face 5. brachial - just above the elbow 6. axillary - bicep 7. popliteal - knee 8. femoral - upper thigh by groin 9. dorsalis - top of foot by ankle 10. posterior tibial - mid calf |
|
|
Circulatory shock
|
* the failure of the circulatory system to adequately deliver oxygen to the tissues
* This results in impairment or ineffective cell function throughout the body * general term for failure of the cardiovascular system to function adequately with resulting cell impairment * untreated, circulatory shock may lead to death. four classifications of circulatory shock: 1. Cardiogenic shock 2. Hypovolemic shock 3. Neurogenic shock 4. Anaphylactic shock 5. septic shock |
|
|
Anaphylactic shock
|
* resulting from an acute allergic reaction called anaphylaxis.
* a type of circulatory shock * anaphylaxis causes the same kind of blood vessel dilation characteristic of neurogenic shock. |
|
|
septic shock
|
* results from infectious agents releasing toxins into the blood; or septicemia
* the toxins often dilate blood vessels, causing shock. made worse by the damaging effects of the toxins on tissues, combined with the increased cell activity caused by the accompanying fever. * a type of circulatory shock ie. toxic shock syndrome - usually results from staphylococcal infections that begin in the vagina of menstruating women and spread to the blood. |
|
|
cardiogenic shock
|
* results from any type of heart failure, ie. myocardial infarction, heart infections
* a type of circulatory shock * because the heart can no longer pump blood effectively, blood flow to the tissues of the body decreases or stops |
|
|
hypovolemic shock
|
* hypovolemia = low blood volume
* results from loss of blood volume in the blood vessels * a type of circulatory shock * results in low blood pressure and reduced flow of blood to tissues * common cause is hemorrhage, or loss of interstitial fluid - causing blood plasma to drain out of the vessels and into the tissue spaces; common in chronic diarrhea or vomiting, dehydration, intestinal blockage, severe or extensive burns |
|
|
neurogenic shock
|
* imbalance in autonomic stimulation of smooth muscle in vessel walls.
* results from widespread dilation of blood vessels caused by an imbalance in autonomic stimulation of smooth muscles in vessel walls * a type of circulatory shock * blood vessels will dilate significantly if sympathetic stimulation is disrupted by an injury to the spinal cord or medulla, depressive drugs, emotional stress, or some other factor. * widespread vasodilation reduces blood pressure, thus reducing blood flow. |
|
|
Reynaud Phenomenon
|
* disorder characterized by sudden decreases in circulation in the digits, often in response to stress or temperature change.
|
|
|
strength of heart contractions
|
* can effect blood pressure
* strength and the rate of the heartbeat affect cardiac output and therefore blood pressure * the stronger each left ventricle contracts the more blood (stroke volume) it pumps into the aorta and arteries and increases blood pressure. * weaker heart beat decreases blood pressure |
|
|
heart rate
|
* an increase in the rate of the heartbeat increases blood pressure
* can effect blood pressure * a decrease in the rate decrease blood pressure * whether a change in the heart rate actually produces a similar change in blood pressure depends on whether the stroke volume also changes and in which direction. |
|
|
resistance to blood flow
|
* can effect blood pressure
* has a huge impact on local blood pressure gradients, and on blood flow is any factor that changes the resistance to blood flow. ie. peripheral resistance |
|
|
peripheral resistance
|
* describe any force that acts against the flow of blood in a blood vessel.
ie. viscosity of blood affects peripheral resistance by influencing the ease with which blood flows through blood vessels. ie. tension in muscles of the blood vessel wall. relaxed = low resistance and blood pressure is low and blood flows easily down its pressure gradient and into the vessel. contracted = resistance increases and so does blood pressure, and the gradient is reduced and blood will not flow so easily into the vessel |
|
|
vasomotor mechanism
|
* the adjustment of muscle tension in vessel walls to control blood pressure, and therefore blood flow
|
|
|
venous blood pressure
|
* very low in the large veins and falls almost to ) by the time blood leaves the venae cavae and enters the right atrium
|

