![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
60 Cards in this Set
- Front
- Back
|
6 ddx's for acute severe chest pain
|
ACS
aortic dissection pericarditis pneumothorax, PE herpes zoster (musculoskeletal, GI reflux, trauma, bronchopneumonia) |
|
|
immediate management of ACS
|
ABCDE! baseline SEWS + IV access
Morphine IV (+anti-emetic) O2 Nitrate (GTN) Aspirin & Clopidogrel (300mg) |
|
|
what's the definitive management/ treatment for STEMI (ACS)
|
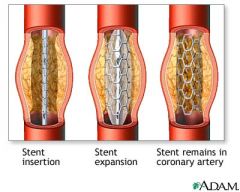
PCI reperfusion
|
|
|
what Ix's is suspect ACS
|
ECG
troponin (12hrs after onset) |
|
|
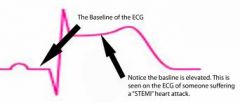
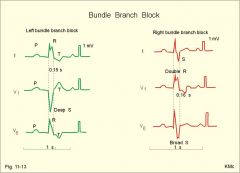
what defines a STEMI on the ECG
|
ST-elevation:
- ≥1mm in 2+ limb leads - ≥2mm in 2+ chest leads new onset BBB (Remember: WiLLiaM & MaRRoW) |
|
|
for a STEMI, if PCI can't be delivered in 90mins, what do you do?
|
THROMBOLYSIS (e.g. tPA, streptokinase)
if no contraindications |
|
|
what are the contraindications of thrombolysis for STEMI which can't receive PCI within 90mins
|
suspect aortic dissection
recent haemorrhage/ CVA/ trauma/ surgery active peptic ulcer uncontrolled HTN aggresive CPR warfarin therapy |
|
|
a pt suffering an acute STEMI has a cardiac arrest in the ambulance for which he required aggressive CPR- how will this effect his type of treatment
|
thrombolysis is contraindicated!
|
|
|
2 main groups of complications following an MI
|
arrhythmic
mechanical (structural) |
|
|
name some arrhythmic complications of an MI
|
AF, atrial flutter
VF/ VT heart block asystole electromechanical dissociation |
|
|
some mechanical (structural) complications of MI
|
LVF
ventricular aneurysm cardiogenic shock pericardial tamponade VSD MR |
|
|
MI secondary prevention includes weight loss. How much is recommended for BMI 25-30
|
5-10% loss
|
|
|
MI secondary prevention includes weight loss. How much is recommended for BMI >30
|
15-20% loss
|
|
|
MI secondary prevention includes exercise. How much is recommended per day and to what intensity?
|
20-30 mins
slight breathlessness |
|
|
post-MI secondary prevention: what diet is recommended
|
Mediterranean-styl
omega-3 (2-4 oily fish/wk) low salt low fat fruit & veg |
|
|
what ECG changes migth be seen in an NSTEMI / unstable angina
|
ST depression
T wave inversion |
|
|
characterise cardiac chest pain
|
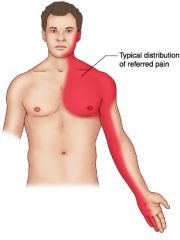
DULL central tight/ heavy/ crushing
radiate - jaw/ arm nausea, sweating, dyspnoea, palpitations |
|
|
differentiate stable angina and ACS (incl unstable angina)
|
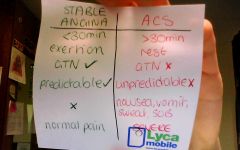
|
|
|
what might cause a rupture of an atherosclerotic plaque
|
iatrogenic (e.g. PCI)
twisting artery (heart beat) ⇈lipid content: thin cap sudden pressure changes |
|
|
2 important prothrombotic factors released by platelets (targeted by antiplatelet therapy)
|

ADP (ADP receptor antagonists- clopidogrel)
TXA2 (aspirin- blocks COX which sythesises it) |
|
|
what tPA
|
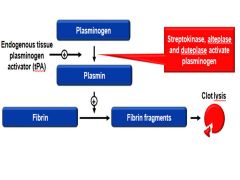
natural fibrinolytic
|
|
|
what's the heart's response to STEMI (occulsion of a vessel)
how does it heal |
ischaemia --> INFARCT
inflam necrosis heal: scar tissue, dilatation |
|
|
LV dilatation can occur after an MI-
What condition does LV dilatation ensue? |

LVF
|
|
|
what's an ECG feature of an old MI
|
T wave inversion
Q waves |
|
|
what 2 blood makers are suggestive on an MI
|
troponin T
CK (non-specific) |
|
|
when does troponin T peak
how long is it raised for |
12-24hrs
1 week |
|
|
aspirin if given immediately for ACS
how does it work |

irreversible blocks COX
COX ⇏ TXA2 ⇏ GPllb/llla receptors for fibrin ⇏ platelet aggregation reduce PLATELET AGREGGATION |
|
|
clopidogrel is given immediately ACS
how does it work |

ADP receptor antagonist (P2Y12 receptor)
⇏ GPllb/llla receptor ⇏ fibrin platelet aggregation |
|
|
prior to undergoing PCI, what drug must pt's take? eG?
how does it work? |

GPllb/llla receptor antagonist (tirofiban)
prevents fibrin aggregating platelets anti-platelet |
|
|
what are the indications for IMMEDIATE reperfusion therapy (PCI via coronary angiography)
|
ST elevation: STEMI
- ≥1mm in 2+ limb leads - ≥2mm in 2+ chest leads new onset BBB (Remember: WiLLiaM & MaRRoW) |
|
|
management of ACS NSTEMI (or unstable angina)
how long for |
MONAC
1) aspirin long term 2) clopidogreal 3 months 3) high risk- coronary ANGIOGRAPHY & revascluarisation (PCI/ CABG) |
|
|
what classifies high risk ACS unstable angina pt's - i.e for angiography & revascularisation
|
ischaemia
high GRACE score |
|
|
what's the worst arrhythmic complication forseeable post-MI
how to treat |
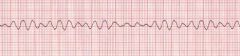
VF
DEFIB!! |
|
|
what's Dressler's syndrome?
when does it occur? clinical signs? |
post-MI/ heart surgery.
auto-ab against ❤ --> recurrent pericarditis, pleural effusion, fever, anaemia chest pain, pleura/ pericardial rub cardiac tamponade |
|
|
treatment of Dressler's syndrome
|
steroids
anti-inflam (autoimmune syndrome) |
|
|
acute pericarditis is a complication post-MI
clinical signs |
central chest pain- worse inspiration/ lying flat
relief SITTING FORWARDS! pericardial friction rub (pericardial effusion/ tamponade) |
|
|
how do you observe/ Ix complications of AMI
|
S&Ss
heart sounds + murmurs creps ECG CXR fluid balance (U&Es, U/O) |
|
|
Starling forces govern fluid movement across capillary wall.
Which 2 forces favour filtration (into interstitial fluid) which end of capillary is this greatest? |
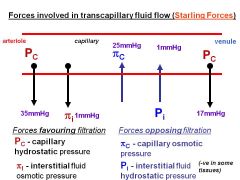
capillary hydrostatic (MAIN)- arteriolar end!
interstitial osmotic |
|
|
Starling forces govern fluid movement across capillary wall.
Which 2 forces oppose filtration (movement back into capillaries?) which end of capillary is this greatest? |
capillary osmotic (MAIN) - venule end!
interstitial hydrostatic |
|
|
how do you calculate the net filtration pressure (NFP) of fluid movement across a capillary wall
|
NFP = (forces favouring capillary HYDROSTATIC p) - (forces opposing capillary ONCOTIC p)
NFP = (cap HYDRO + ISF oncotic) - (cap ONCOTIC + ISF hydro) |
|
|
which 3 starling forces of attraction across a capillary wall remain constant
|
- ONCOTIC p's (capillary & ISF)
- ISF hydrostatic cap hydro fluctuates |
|
|
fluid movement across a capillary wall is greatest at which end for:
- ultrafiltration - reabsorption |
FILT: arteriolar end
REABS: venular end |
|
|
how does po oedema manifest (clinical signs)
|

SOB
bibasal creps didsplaced apex (LVF) CXR: prehilar haziness, po oedema, ↑cardiothoracic ratio |
|
|
2 main physiological causes of systemic/ po oedema? e.gs?
(referring to starling's law of capillary fluid exchange) |
- ↑capillary hydrostatic p (i.e due to RVF/LVF, varicose veins, VTE)
- ↓ capillary oncotic p (malnutrition, protein malabsorption, excess renal excretion, hepatic failure) |
|
|
2 physiological causes systemic/ po oedema ?
other than: - ↑capillary hydrostatic p - ↓ capillary oncotic p |

- lymphatic insufficiency (obstruction, lymph node damage, filariasis)
- change in capillary perm (inflam, histamine)= ↑protein leakage |
|
|
how would you clinically assess for lymphatic insufficiency
|

"NON-PITTING" oedema
|
|
|
post-MI/ ACS medications
|
aspirin
statin BB ACEIs (+GTN for angina) |
|
|
What's HF
|
low CO
S&Ss due to fluid retention / accumulation CCF/ LVF/ RVF |
|
|
3 causes LVF / LHF
|
post-MI
cardiomyopathy (dilated, poorly contracting) valvular disease |
|
|
3 causes RVF/ RHF
|
cor pulmonale
secondary to LVF/ LHF congenital (R more common than L) |
|
|
Symps LVF/ LHF
|
dyspnoea, orthopnoea, PND
nocturnal cough +/- pink frothy sputum (po oedema) wheeze poor exercise tolerance fatigue cold peripheries |
|
|
signs LVF/ LHF
|
tachycardia
fine bibasal creps pleural effusion S3 gallop (accelerated blood filling due to ↑back pressure) LV heave/ displaced apex |
|
|
CXR findings in LVF/ LHF
|
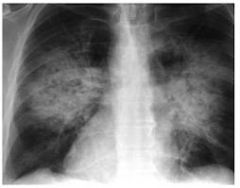
bat wing shadows
kerly B lines po oedema |
|
|
S&Ss RVF/ RHF
|
nausea, anorexia,
periperal oedema ascites hepatomegaly JVP, epistaxis RV heave |
|
|
Ix's HF
|
1) BNP, FBC, U&Es
2) ECG 3) echo (LV dysfunction) CXR |
|
|
treatment of HF depends on cause.
what are the 6 standard pharmacological treatment2 for CCF in prev-MIs & cardiomyopathies (egs) |
DIURETICS (loop- frusemide) +/- Spironolactone
ACEIs (lisinopril) BBs- start low go slow (bisiprolol) ... further: - Digoxin for AF: inotrope - Vasodilators (isosorbide mononitrate) |
|
|
If HF is due to valvular heart disease (normally LVF/ LHF) what's the treatment
|
surgery
|
|
|
If HF is due to cor pulmonale (RVF/ RHF), what's the treatment
|
O2
DIURETICS only!!! |
|
|
lifestyle advice for CCF/ HF/ CHF
|
stop smoking
stop alcohol! optimise weight LOW SALT / ?fluid intake low level reg exercise |
|
|
Implantable devices & surgery for CCF/ CHF/ HF
|
ICD (implantable cardiac defibs)
CRT (cardiac resync therapy) - prolonged QRS new VALVE/s- if that's the cause TRANSPLANT- if young & fit |

