![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
33 Cards in this Set
- Front
- Back
|
Antifungals
Why are antibiotics ineffective in treating fungal diseases? |
-cellular/organelle differences between microbacteria & fungi (e.g., cell wall structural differences; 70S ribsomes in bacteria, 80S ribsomes in fungi)
-SELECTIVE TOXICITY-antibacterial drugs need to be selectively toxic to the microorganisms (but not to the host) -many anti-fungal targets are also found in the hosts (toxicity; life-threatening to host) |
|
|
Antifungals
Dangers of antifungals |
-many anti-fungals are also found in the hosts (--> toxic effects; life-threatening to the host)
|
|
|
Antifungals
Polyene antifungals |
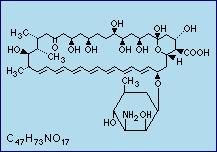
-amphotericin B, nystatin
-amphotericin B= "the gold standard" for anti-fungal agents (used to treat many fungal infections) -rings associated w/ a 7 double bonds chain |
|
|
Antifungals
Amphotericin B (a Polyene antifungal) |
-"the gold standard" for all anti-fungal agents
-used for treating many kinds of fungal infections -toxic |
|
|
Antifungals
Azole antifungals |
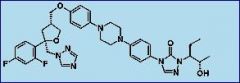
-synthetically produced
-drug names all end in "-azole" -contain many nitrogens |
|
|
Antifungals
Allylamines/Thiocarbamates antifungal drugs |
-Naftitine, Terbinafine, Tolnafate
-cutaneous/externally used antifungal drugs |
|
|
Antifungals
Griseofulvin |
-used against dermatophytes
|
|
|
Antifungals
Cell Wall Synthesis Inhibitor antifungals: Why are they so promising? |
-since the host cells lack cell walls, they can selectively target fungal infections (without affecting the host's cells)
|
|
|
Antifungals
Polyene antifungals: Modes of Action |
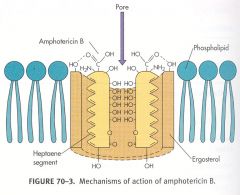
-bind to fungal cell membrane--> produce hole in membrane--> electrolytes (K+) leak out, H20 enters cell--> cell lysis
|
|
|
Antifungals
Amphatericin B (a polyene antifungal; "Gold Standard" for antifungal treatments) |
-very toxic- never given in amounts that exceed the fungal concentration in the patient
-selective toxicity- has higher affinity for ERGOSTEROL, a membrane lipid found in fungi, than for cholesterol, which is found in humans -highly toxic (esp.) to kidneys -can't give them Per Os (b/c polyenes are not soluble and have poor absorption from the gut) -given through IV |
|
|
Antifungals
Liposomes |
-vesicle covered w/ a lipid bilayer (cholesterol)
-can be filled w/ drugs (e.g., Amphotericin B, Nystatin) -can selectively target a certain area/structure -3 types: ABCD-Amphocyl; ABCL; Ambisome-Amphoteracin B (1 AB is surrounded by 9 lipids) -liposomal nystatin is unavailable |
|
|
Antifungals
Liposomes: benefits for treatment |
-spend little time in the plasma
(act quickly) -able to specifically target sites of fungal infection -able to deliver hydrophilic substances across hydrophobic membranes -reduce toxicity to the host |
|
|
Antifungals
Liposomes: drawbacks for treatment |
-v. expensive
|
|
|
Antifungals
Azole antifungals: mode of action |
-inhibit ergosterol synthesis (fungal membrane lipid)
-blocks 14-ALPHA-DEMETHYLASE (= a Cytochrome p450 enzyme) from synthesizing ergosterol |
|
|
Antifungals
Summary of modes of action of Polyenes, Azoles & Allylamines |
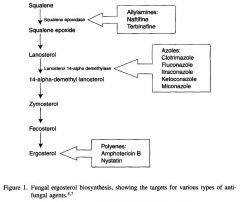
-Azoles (14-alpha-demethylase)= affects cells that are already producing cell walls--> INHIBITS GROWTH
-Polyenes= bind to pre-existing cell wall (ergosterol)--> DECREASED FUNGAL RESISTANCE |
|
|
Antifungals
Allylamine antifungal mode of action |
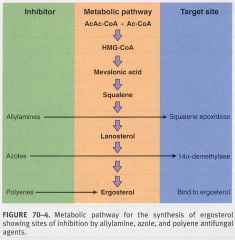
-inhibit SQUALENE EPOXIDASE (which produces lanosterol, a precursor in the ergosterol synthesis pathway)
|
|
|
Antifungals
Terbinafine (an allylamine antifungal) |
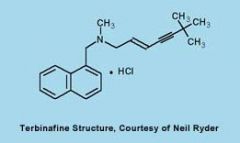
-inhibits ergosterol biosynthesis by inhibiting squalene epoxidase
|
|
|
Antifungals
5'-Fluorocytosine (a Flucytosine antifungal) |
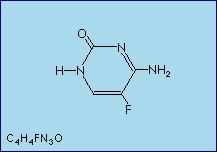
-only antimetabolite drug w/ antifungal activity
-given Per Os |
|
|
Antifungals
5-Fluorocytosine (a flucytosine antifungal) mode of action |
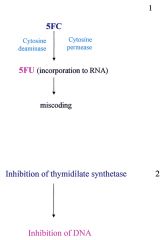
-inhibits fungal protein synthesis/causes RNA miscoding (replaces uracil w/ 5'-fluorouracil in fungal RNA; RNA can't distingsuih b/n 5FU and U)
-5FU enters the cell via CYTOSINE PERMEASE -inhibits fungal DNA synthesis (by inhibiting THYMIDYLATE SYNTHETASE via 5'-fluorodeoxy-uridine monophosphate) -fungistatic (DNA inhibition) |
|
|
Antifungals
Chitin Synthase Inhibitors (cell wall synthesis inhibitors antifungals) |
-polyoxin, nikkomcyins
-inhibit sepatae formation & osmotic lysis -analogs of chitin (the UDP-N-acetylglucosamine substrate) -competitive inhibitors -not used as therapies |
|
|
Antifungals
1,3-beta-Glucan Synthase Inhibitors (cell wall synthesis inhibitors antifungals) |
-Caspofungin, Micafungin, & V-echinocandin (LY303366)
-block fungal cell wall (GLUCAN) synthesis (by inhibiting 1,3-Beta-Glucan Synthase) -effect cells that are undergoing multiplication (NOT pre-existing cells) -EICHINOCANDINS= chemical family to which the antifungals belong |
|
|
Antifungals
Illustration of Cell Wall Inhibitor (1,3-B-glucan synthesis inhibitors) and Azole antifungal modes of action |
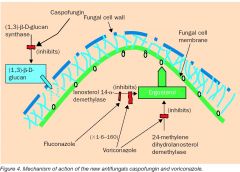
.
|
|
|
Antifungals
Griseofulvin antifungal mode of action |
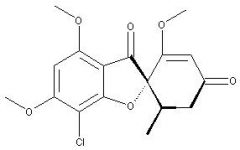
-inhibits fungal mitosis (by disrupting the mitotic spindle)
-disrupts the mitotic spindle through interactions w/ polymerized microtubules |
|
|
Antifungals
Resistance to Antifungals (7 reasons) |
-1) overproduction of target enzyme
-2) drug target is altered (drug can't interact w/ its target) -3) EFFLUX mode of action= drugs is pumped out of the cell by an efflux pump (V. IMPORTANT!!!) -4) entry of the drug into the cell is inhibited at the cell wall/membrane level -5) the cell has a by-pass pathway (the cell stops producing the drug's target & creates a bypass pathway in which the drug doesn't have targets) -6) fungal enzymes that activate "inactive" drugs into their active forms are inhibited -7) enzymes secrete by the cell to the EC space degrade the drugs |
|
|
Antifungals
Resistance to Antifungal Drugs (an illustration) |
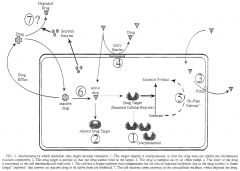
.
|
|
|
Antifungals
Resistance: the example of Cryptococcus neoformans |
-resistant to fluconazole
-fluconazole normally acts against Cryptococcus neoformans (a yeast which causes lots of problems in AIDS patients, including meningitis) -AIDS patients receive flucanozole for months--> resistance (so we give AIDS patients, low doses of flucanozole) |
|
|
Antifungals
Sordarins antifungals |
-selective inhibition of protein synthesis
-target the elongation cycle in yeasts -inhibit EF-2's (elongation factors involved in the elongation cycle) -no pharmacological use for them -fungal EF2's are homologous to mammalian EF2's but are selectively inhibited by Sordarins -EF3's are a 3rd EF that are unique to fungi (don't exist in other organisms) |
|
|
Antifungals
Summary slide |

.
|
|
|
Antifungals
Antifungal Spectrum (definition) |
-range of activity of an antifungal agent against fungi
-broad-spectrum antifungals= act against wide variety of fungi -narrow-sprectrum antifungals= act against small # of fungi |
|
|
Antifungals
Fungastic Activity (definition) |
-the level of anti-fungal activity which inhibits the growth of an organism
-MIC= minimum inhibitory concentration= lowest concentration of the drug that inhibits organism's growth |
|
|
Antifungals
Fungicidal Activity (definition) |
-ability of an antifugnal agent to kill an organism in vitro or in vivo
-MFC= minimum fungicidal concentration= the lowest [drug] that will kill 99.9% of tested organisms |
|
|
Antifungals
Antifungal Concentrations, Antifungal Synergism, Antifungal Antagonism (definitions) |
-combinations of antifungal agents
-ANTIFUNGAL SYNERGISM= combinations of antifungal agents that have enhanced antifungal activity when used together (vs. alone) -ANTIFUNGAL ANTAGONISM= the activity of each agent interferes w/ the activity of the other agent |
|
|
Antifungals
Efflux Pumps |
-families of drug transporters that pump antifungal agents out of fungal cells (decreasing the amount of drug available to interact w/ its target)
-involved in antifungal drug resistance |

