![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
136 Cards in this Set
- Front
- Back
|
Pre-eclamptic woman, BP 170/110, headache, proteinuria 1.2g. Which of the following NOT to use for control of her hypertension: A. Magnesium B. SNP C. GTN D. Hydralazine E. Metoprolol |
A. Magnesium (seizure control not BP control) SNP is last resort |
|
|
Male with a Haemoglobin of 86% and reticulocyte count 10%. Possible diagnosis: A. Untreated pernicious anaemia B. Aplastic anaemia C. Acute leukaemia D. Anaemia of chronic disease E. Hereditary spherocytosis |
E. Hereditary spherocytosis |
|
|
Commonest organism causing meningitis post spinal: A. Staph epidermidis B. Staph salivarius C. Staph aureus D. Strep pneumoniae E. ? |
B. Staph salivarius |
|
|
Exponential decline / definition of time constant (with various options) A. time for exponential process to reach log(e) of its initial value B. Time until exponential process reaches zero C. Time to reach 37% of initial value D. Time to reach half if its initial value E. 69% of half life |
C. Time to reach 37% of initial value |
|
|
Relative humidity – air fully saturated at 20 %. What is the relative humidity at 37 degrees ? A. 20 B. 30 C. 40 D. 50 E. 60% |
C. 40 Fully saturated water content at 37deg = 44g Fully saturated water content at 20deg = 17g RH = 17/44 = 0.39 |
|
|
A 50 year old man with multiple fractures. The BEST parameter to monitor volume resuscitation is: A. Heart rate B. LVEDV C. PCWP D. RVEDV E. Changes in R atrial pressure during inspiration |
B. LVEDV |
|
|
Anaphylaxis to rocuronium. Which is most likely to cause cross-reactivity ? A. Vecuronium B. Pancuronium C. Atracurium D. Cisatracurium E. None of the above - cross reactivity too variable to predict |
?E. None of the above - cross reactivity too variable to predict ?A. Vecuronium |
|
|
Hypotension post propofol induction in elderly patient. More pronounced / profound than in younger patient. Reason? A. Concentric LVH associated with ageing and therefore preload dependent B. Because of increased lean body mass C. Decreased cardiac output with ageing D. Increased sensitivity to all anaesthetic agents, thus relative overdose is common E. Decreased liver blood flow with ageing, decrease drug clearance and increased drug concentration |
D. Increased sensitivity to all anaesthetic agents, thus relative overdose is common ?A (from previous Cram notes) |
|
|
Predictive factors for mortality in elderly patient (except): A. Aortic stenosis B. Diabetes mellitus C. Elevated Creatinine D. Cognitive dysfunction E. Type of surgery |
D. Cognitive dysfunction |
|
|
The best clinical indicator of severe AS: A. Presence of thrill B. Mean Gradient 30mmHg C. Area 1.2 cm2 D. Slow rising pulse and ESM radiating to carotids E. Shortness of breath |
A. Presence of thrill |
|
|
Elderly patient. Indications for pre Femoro-Popliteal Bypass angiogram include all EXCEPT: A. Severe heart failure B. Suspicion of L main disease C. Symptomatic tachyarrhythmia D. Unstable angina E. Stable angina with positive thallium |
? RPA and POW - C RNS - E |
|
|
How do you minimise risk of intravenous cannulation with epidural insertion ? A. Injection saline through epidural needle before catheter insertion B. Lie patient lateral C. Do CSE D. Thread catheter slowly E. |
A and B |
|
|
Timing of peak respiratory depression post intrathecal 300 mcg morphine: A. < 3.5 hours B. 3.5 – 7.5 hours C. 7 - 12.5 hours D. 12.5 -18 hours E. > 18 hours |
B. 3.5 – 7.5 hours (then three hours) |
|
|
Patient with aortic dissection. Blood pressure 150/90. Best drug to control BP: A. Captopril B. Esmolol C. GTN D. Hydralazine E. SNP |
B. Esmolol CEACCP Aortic dissection: "The primary goal is to reduce the force of left ventricular contraction without compromising perfusion, thus reducing shear forces and preventing further extension of the dissection or possible rupture. Beta-blockers (e.g. esmolol, metoprolol) and labetalol (beta- and alpha-blocker) can be used. If further reduction in BP is required, sodium nitroprusside, glyceryl trinitrate, or hydralazine are appropriate. Beta-blockers should be given first before vasodilators, as the reflex catecholamine release due to vasodilatation may increase left ventricular contractions." |
|
|
Type of dissection – which is classically for NON-operative management: A. DeBakey Type I B. DeBakey Type II C. Stanford A D. Stanford B E. Stanford C |
D. Stanford B |
|
|
TURP – patient under spinal. Confused. ABG: Na+ 117 / normal gas exchange. Treatment ? A. 10 ml 20% Saline as fast push IV B. 3% NS 100 ml/h C. Normal saline 200 ml/h D. Frusemide 40 mg IV E. Fluid restrict 500 ml/day |
B. 3% NS 100 ml/h |
|
|
Male undergoing trans-sphenoidal surgery. Now Na+ 155mmol/l and thirsty with polydipsia. Treatment: A. Desmopressin (DDAVP) B. Fluid restrict C. Aldosterone D. E. |
A. Desmopressin (DDAVP) |
|
|
The STRONGEST stimulus for ADH secretion: A. High serum osmolality B. Low serum osmolality C. Hypovolaemia D. High serum Na E. |
C. Hypovolaemia |
|
|
Stellate ganglion block. Needle entry next to SCM muscle at C6. Which direction to advance needle ? A. C3 B. C4 C. C5 D. C6 E. C7 |
D. C6 |
|
|
Thermoneutral zone in 1 month old infant ? A. 26 – 28 degrees Celcius B. 28 – 30 degrees Celcius C. 30 – 32 degrees Celcius D. 32 – 34 degrees Celcius E. 34-46 degrees celcius |
D. 32 – 34 degrees Celcius |
|
|
A 60 year old man describes orthopnoea. On examination: pansystolic murmur (at LSE)/ displaced apex beat. Likely diagnosis ? A. Mitral regurgitation B. ? C. D. E. |
A. MR (alternatives for pansystolic murmur: TR, AS, PS) MR causes displacement of apex beat. |
|
|
A 4 year old child with VSD (repaired when 2 years old) for dental surgery. What antibiotic prophylaxis do the guidelines recommend? A. Amoxycillyn orally B. Amoxycillin IV C. Cephazolin IV D. Amoxycillin / gentamicin E. No antibiotics required |
E. No antibiotics required Only needed if prosthetic material used |
|
|
A 4 year old child with Arthrogrophysis multiplex congenita for dental surgery. Jaw rigidity post induction. Likely cause ? A. Temporomandibular joint involvement/ TMJ rigidity B. Inadequate depth of anaesthesia C. Inadequate muscle relaxation/ inadequate sux D. Masseter spasm E. ? |
A. Temporomandibular joint involvement/ TMJ rigidity |
|
|
A 78 year old man with past difficult intubation for arm surgery. Supraclavicular block with 25 mls 0.5% bupivacaine. Shortly after begins convulsing. INITIAL management? A. Midazolam 5mg B. Intralipid 20% 1.5 ml/kg C. Thiopentone 150mg D. Suxamethonium 50mg E. Propofol 50mg |
A. Midazolam 5mg |
|
|
Advantages of bronchial blockers over double lumen tubes: A. Able to achieve lobar isolation B. Lower cuff pressure C. Quicker deflation of isolated lung D. Pneumonectomy E. Lower incidence of malposition |
A. Able to achieve lobar isolation |
|
|
Patient for pneumonectomy. Pre op FEV1 2.4. (Predicted 4.5L) FVC given as well. For R lower lobectomy. Postoperative predicted FEV1 ? A. 1.3 B. 1.5 C. 1.7 D. 1.9 E. 2.2 |
C. 1.7L 2 ways to calculate. Either 4/5 *2.4 = 1.9 (giving answer D) Or (?more accurately) use right 3/2/5 left 3/2/4 and so (19-5)/19*2.4 = 1.7L (answer C) |
|
|
Post accidental dural puncture with epidural needle. Headache. Which does NOT fit ? A. Epidural blood patch 30-50% effective B. Unlikely to be related to epidural if purely occipital headache C. Caffeine mildly effective in reducing headache D. Subdural haematoma can rarely occur with PDPH E. (?something about photophobia) |
A. Epidural blood patch 30-50% effective |
|
|
Cell saver. Which does NOT get filtered ? A. Foetal cells B. Free Hb C. Platelets D. Clotting factors E. Microaggregates of leukocytes |
A. Foetal cells |
|
|
You are on a humanitarian aid mission in the developing world. Drawover vaporiser apparatus described being used. Given 400 mm tubing, OMV or diamedica vaporiser, 200mm tubing attached to self-inflating bag. Which other ONE piece of equipment is ESSENTIAL to make this system functional? A. Halothane B. In-line Waters' Cannister C. Non-rebreathing valve D. Oxygen source E. Ventilator |
C. Non-rebreathing valve The most simple form of modern drawover system consists of two reservoir tubes, a vapouriser and a non-rebreathing valve:The patient (P) inspires and expires via the non-rebreathing valve (V). Air (A) enters the system from the atmosphere and may be supplemented with oxygen. The tubes provide reservoirs of oxygen (if it is being used) and anesthetic-containing gas. Most systems incorporate a self-inflating bag (e.g. Ambu bag) so that ventilation can be controlled or assisted if necessary. Draw-over systems are most useful in field anesthesia, developing countries and in other situations where supplies of compressed gases are not readily available. They are particularly useful if ether is used, owing to the lack of respiratory depression produced by this agent. http://asevet.com/resources/circuits/drawover.htm |
|
|
Regarding post craniotomy pain: A. Local infiltration proven to reduce long-term pain B. Local more painful than discrete nerve blocks C. Local infiltration more efficacious than discrete nerve blocks D. Local infiltration more efficacious than opioid analgesia E. Local infiltration more efficacious with clonidine included |
A. Local infiltration proven to reduce long-term pain Need to block 6 nerves bilaterally to completely cover: supratrochlear, supraorbital, zygomaticotemporal, great auricular, greater occipital, lesser occipital. http://www.anzca.edu.au/resources/college-publications/pdfs/books-and-publications/Australasian%20Anaesthesia/australasian-anaesthesia-2005/05_Cormack-Costello.pdf |
|
|
A 60 year old female is undergoing hysterectomy. Gabapentin reduces postoperative: A. Nausea B. Vomiting C. Sedation D. Pruritus E. Constipation |
A. Nausea |
|
|
Burns dressings. The following is proven to be of analgesic benefit: A. Morphine gel B. Biosynthetic dressings C. Dexmedetomidine IV D. Lignocaine IV E. Cognitive/Distraction technique |
B. Biosynthetic dressings (from pain book) |
|
|
Subtenon’s block. What is the worst position to insert block? A. Inferonasal B. Inferotemporal C. Superonasal D. Superotemporal E. Medial / canthal |
E. Medial / canthal possibly C. |
|
|
Liposuction. Infiltration of lignocaine with 1:200,000 adrenaline. Peak plasma concentration of lignocaine occurs at: A. 1 hour B. 3 hours C. 18 hours D. 24 hours E. 30 mins |
C. 18 hours |
|
|
Child-Pugh score. Components ? A. Bilirubin / albumin / INR /ascites/ encephalopathy B. Various other options including AST/ALT, GGT, PT C. ? D. ? E. ? |
A Remember as BAPAE: bilirubin, albumin, PT, ascites, encephalopthy. Score A, B, or C. Used to predict post-operative survival. (MELD uses BIC: bilirubin, INR, creatinine. Originally used for prognosis following TIPPS, now used for transplant planning.) |
|
|
Which is NOT a disadvantage of drawover vaporiser versus plenum vaporiser: A. Temperature compensation B. Cannot use sevoflurane C. Small volume reservoir D. Flow compensation E. |
B. Cannot use sevoflurane May need several in series |
|
|
Acute renal failure. Which is not an indication for dialysis ? A. Hyperkalaemia B. Metabolic alkalosis C. Hypernatraemia D. Uraemic pericarditis E. APO |
B. Metabolic alkalosis Indications for dialysis / RRT: UFAKE-TNT - Uraemia - Fluid overload - Acidosis (metabolic) - K > 6 - Extras: ---Toxins ---Na>160 ---Temp control (hyperthermia) |
|
|
Chronic alcohol use. Which is not an associated complication ? A. AF B. hypertriglyceridemia C. Macrocytosis D. Nephrotic syndrome E. Pancreatic Ca |
D. Nephrotic syndrome |
|
|
Chest X-Ray shown of patient post Left pneumonectomy with heart swung to left side. Management: A. Increase PEEP B. Roll onto right side C. Turn on suction to left pleural catheter D. Lung biopsy E. |
B. Roll onto right side |
|
|
Salicylate poisoning: A. Respiratory acidosis B. Metabolic acidosis C. Increased CO2 (production) D. High output renal failure E. Hyperthermia |
B. Metabolic acidosis |
|
|
New onset atrial fibrillation in a 10 week pregnant lady. BP 150/90, HR 160, SaO2 92%. Moderate mitral stenosis on TTE, no thrombus seen. Emergency doctor gave her anticoagulant (not specified what). Most appropriate management: A. Verapamil B. Labetalol 20mg iv to 300mg C. Amiodarone 300mg IV D. Synchronised biphasic cardioversion with 70-100 Joule E. Oral digoxin -1000mcg then 500mcg 6 hrs later |
D. Synchronised biphasic cardioversion with 70-100 Joule or could try B. Labetalol |
|
|
Patient post anterior cervical fusion. Patient in recovery. Confused and combative. Nurse concerned about haematoma Taken to theatre: Most appropriate way of securing airway: A. Gas induction / laryngoscopy / intubate B. Awake tracheostomy C. Awake fibreoptic intubation using minimal sedation D. Thiopentone, suxamethonium, direct laryngoscopy and intubation E. retrograde intubation |
A. Gas induction / laryngoscopy / intubate |
|
|
Young asthmatic male in emergency department. RR 26, pCO2 27, SAO2 92%, struggling talking in sentences. Given nebulised salbutamol, and ipratropium, 200mg IV hydrocortisone. After 30 minutes - no improvement. Further management: A. IV salbutamol B. IV aminophylline C. IV magnesium D. Intubate and ventilate E. ? |
C. IV magnesium |
|
|
Called to emergency department to review a 20 y/o male punched in throat at a party. Some haemoptysis / hoarse / soft voice. Next step in management: A. CT to rule out thyroid cartilage fracture B. XR to rule out fractured hyoid C. Rapid sequence induction / laryngoscopy / intubation D. Awake fibreoptic intubation E. Nasendoscopy by ENT in emergency department |
E. Nasendoscopy by ENT in emergency department |
|
|
How quickly does the CO2 rise in the apnoeic patient ? A. 1 mmHg per min B. 2 mmHg per min C. 3 mmHg per min D. 4 mmHg per min E. 5 or ?8 mmHg per min |
C. 3 mmHg per min |
|
|
Long-standing T6 paraplegia. All present EXCEPT ? A. Flaccid paralysis B. Poikilothermia C. Autonomic hypereflexia D. Labile BP E. Hyperkalaemia with suxamethonium |
A. Flaccid paralysis and E. Hyperkalaemia with suxamethonium Can't use sux from 3 days until 9 months due to risk of hyperkalaemia. T6 paraplegia likely to have autonomic dysfunction and hyperreflexia. Also spasm usually a problem. |
|
|
Young female patient for tonsillectomy with history of bleeding tendency. Which is the most likely cause? A. Factor V Leiden B. Protein C deficiency C. Haemophilia B D. Antithrombin III deficiency E. Lupus anticoagulant |
C. Haemophilia B all others are pro-thrombotic |
|
|
Amniotic fluid embolism. Cause of death in first half hour ? A. Pulmonary hypertension B. Malignant arrhythmia C. Pulmonary oedema D. Hypovolaemic shock E. |
A. Pulmonary hypertension Phase 1: Amniotic fluid and foetal cells enter the maternal circulation resulting in the release of biochemical mediators which cause pulmonary artery vasospasm followed by pulmonary hypertension. This results in elevated right ventricular pressures and right ventricular dysfunction, which will lead to hypoxaemia and hypotension with associated myocardial and capillary damage. Phase 1 may last up to 30 min. Phase 2: This occurs in patients who survive the initial insult. Left ventricular failure and pulmonary oedema occurs. Biochemical mediators trigger DIC leading to massive haemorrhage and uterine atony. CEACCP 2007 http://ceaccp.oxfordjournals.org/content/7/5/152.full |
|
|
Hypocalcaemia – earliest sign: A. Tingling of face and hands B. Chvostek’s sign C. Carpopedal spasm D. E. |
A. Tingling of face and hands |
|
|
Elderly COAD patient. On home oxygen. 24 hours of worsening condition. Various blood gases given: A. paO2 > 50, paCO2 70 HCO3 30 etc… B. C. D. E. |
COPD on home O2, expect: - low PaO2 - high PaCO2 - possibly low normal pH (compensated) - high BE and bicarb (metabolic compensation) |
|
|
Visual loss with pupillary reflexes retained. Likely cause ? A. Retinal detachment B. Occipital mass C. Frontal mass D. Chiasmal mass E. Optic neuritis |
B. Occipital mass |
|
|
Nerve block for anaesthesia over anterior 2/3 of ear? A. C2 B. Mandibular nerve C. Maxillary nerve D. Ophthalmic nerve E. Vagus |
B. Mandibular nerve |
|
|
Complex regional pain syndrome. What proportion of patients have motor involvement ? A. 0 % B. 25 % C. 50 % D. 75 % E. 95 % |
D. 75 % |
|
|
Malignant hyperthermia. The number of people in the community at any given time with a predisposition is called the: A. Prevalence B. Incidence C. Occurrence D. Rate E. Denominator |
A. Prevalence |
|
|
Patient with Hx COAD and suspected pneumonia – clinical findings supporting R pneumonia on examination: A. R Dull percussion note & increased vocal resonance B. R Dull percussion note & decreased vocal resonance C. R Decreased air entry D. Tracheal deviation to left E. Tracheal deviation to right |
A. R Dull percussion note & increased vocal resonance |
|
|
Thallium scan: A. High negative predictive value B. High positive predictive value C. Not as good as a dobutamine stress echocardiography D. E. |
A. High negative predictive value |
|
|
A 50 y/o male diabetic admitted to intensive care with pneumonia. Intubated and ventilated. Extensive results given. BP 80/-, HR 120, CVP 4, PCWP 6, SvO2 69% PaO2 80, BE -4 pH 7.2. Management: A. Blood transfusion B. Bicarbonate infusion C. Fluid resuscitation D. Adrenaline infusion E. Insulin infusion |
C. Fluid resuscitation |
|
|
Young female having cholecystectomy. Venous air embolus: A. Mechanical ventilation and PEEP is part of treatment strategy B. Most likely to occur at initial gas insufflation, but can occur at any time C. Inert gas (argon, xenon) is safer D. E. |
B. Most likely to occur at initial gas insufflation, but can occur at any time |
|
|
LSCS for failure to progress. Spinal is inserted uneventfully. Next day the patient has foot drop. The most likely cause is? A. epidural haematoma B. lumbosacral palsy C. sciatic nerve palsy D. common peroneal palsy E. |
B. lumbosacral palsy |
|
|
Severe pre-eclampsia. WORST treatment option: A. Magnesium B. Nifedipine C. Metoprolol D. SNP E. |
D. SNP SNP - risk of severe hypotension, paradoxical brady + unknown effects of CN on foetus Metoprolol - There are concerns about selective B-blockade in severe PE due to high afterload, hence risk of precipitating APO |
|
|
In pregnancy the dural sac ends at: A. T12 B. L2 C. L4 D. S2 E. S4 |
D. S2 |
|
|
Septic elderly man. Given lots of obs but essentially mixed venous oxygen sat 65%, lactate 4, MAP low. Mx. A. transfuse B. fluid bolus C. Noradrenaline |
B. fluid bolus |
|
|
Another pregnant woman with ?MS. Develops SVT. Try vagal manoeuvres without success. A. Adenosine B. ? C. ? |
A. Adenosine Can use adenosine, CCB, digoxin, DCCV in pregnancy. Avoid amiodarone. |
|
|
Pregnant woman presents with narrow complex tachycardia HR 190, stable BP 100/60. No response to vagal manoeuvres. Management? A. Adenosine 6mg B. DCR C. Amiodarone D. Atenolol E. Magnesium |
A. Adenosine 6mg A then B |
|
|
Which gives the BEST seal? A LMA classic B Proseal C Intubating LMA D. ? E. ? |
B. Proseal |
|
|
Peak plasma lignocaine level after epidural lignocaine. (again various times similar to the tumesent lignocaine one) |
Spinal 90min, epidural 105 min http://www.ncbi.nlm.nih.gov/pubmed/7968331 |
|
|
Lady on citalopram. Which drug is relatively contraindicated? A Tramadol B. Ondansetron C. Metaraminol D. Clonidine |
A Tramadol A - citalo (SSRI) and tramadol (atypical opioid with NA and 5HT effects) triggers for serotonin syndrome |
|
|
A 30yo Male. 5 hour operation. Arms abducted to 60 degrees. Head turned slightly to left side. Post op numb palm/thumb/index finger/middle finger and lateral half of ring finger. Numb ventral forearm. Weak finger grip. Weak elbow flexion. Most likely nerve injured? A. median nerve B. musculocutanous nerve C. upper trunk of brachial plexus D. ?brachial plexus stretch E. |
C. Upper trunk of BP Brachial plexus injury. Terminal nerve affected is median (sensory) plus C5/6 motor. So need BP injury that correlates with this. Upper trunk is C5/6 |
|
|
Diastolic dysfunction is NOT caused by: A. Adrenaline B. Aortic stenosis C. Hypertension D. myocardial fibrosis E. ? |
A. Adrenaline |
|
|
An 18 yo with Fontan circulation undergoing exploratory laparotomy. On ICU vent, sats 70%. Which ventilator parameter would you INCREASE to improve his sats? A. Bilevel pressure B. Expiratory time C. Inspiratory time D. Peak inspiratory pressure E. PEEP |
B. Expiratory time |
|
|
A 7 kg Infant with tetralogy of Fallot, post BT-shunt. Definitive repair at later date. Paralysed and ventilated. Sats 85% baseline, now 70%, best treatment: A. Increase FiO2 from 50 - 100% B. Esmolol 70 mcg C. Phenylephrine 35 mcg D. Morphine 1 mg E. 1/2 NS with 2.5% dex 70 mls |
C. Phenylephrine 35 mcg BT shunt is used to increase pulmonary blood flow. Connects systemic system (usually subclavian artery) to pulmonary artery. ?C as need to force more blood from peripheries through lungs to improve oxygenation. |
|
|
Von Hippel-Lindau disease is associated with: A. increased risk of malignant hyperthermia B. meningiomas C. peripheral neuropathy D. phaeochromocytomas E. poor dentition |
D. phaeochromocytomas Mutation of VHL tumour suppressor gene. S+S: headaches, problems with balance and walking, dizziness, weakness of the limbs, vision problems, and high blood pressure. Associated conditions: angiomatosis, hemangioblastomas, phaeochromocytoma, renal cell carcinoma, pancreatic cysts, endolymphatic sac tumour, and bilateral papillary cystadenomas of the epididymis (men) or broad ligament of the uterus (women) |
|
|
70 year old post TKJR. On sub-cut heparin. Develops clinical DVT and platelets 40 (sounds like HITS type-II). Management A. Enoxaparin B. Fondaparinux C. Heparin by infusion D. Lepirudin E. Warfarin |
D. or B. HITTS: - type 1: benign non-immune condition within 4d - type 2: immune-mediated 5-10d Alternatives to heparin: - direct thrombin inhibitors (e.g. lepirudin, bivalirudin) - factor Xa inhibitors (e.g. danaparoid, fondaparinux) Avoid warfarin in HIT until the platelet count has recovered (risk of thrombosis due to Protein C and S deficiency; risk of skin necrosis) |
|
|
Drug eluting stent 6 months old. On aspirin and Prasugrel 10mg. Elective lap cholecystectomy for biliary colic. A. Do case while taking both. B. Do case while stopping both. C. Stop Prasugrel for 7 days, keep taking aspirin. D. Stop Prasugrel for some other different time E. Postpone for 6 months |
E. Postpone for 6 months Prasugrel is an ADP inhibitor similar to clopidogrel |
|
|
Arterial blood gases (ABGs): pH 7.12, PO2 100, PCO2 65, HCO3 20.3, BE -10. Consistent with? A. Chronic renal failure B. Malignant hyperthermia C. Diabetic ketoacidosis D. End-stage respiratory failure E. Ethylene glycol toxicity |
B. Malignant hyperthermia Metabolic acidosis. Respiratory acidosis. |
|
|
Compared to lignocaine, bupivacaine is A. Twice as potent B. Three times as potent C. Four times as potent D. Five times as potent E. Same potency |
C. four times as potent Relative potency: - procaine 1 - lignocaine 2 - mepivacaine 2 - bupivacaine 8 |
|
|
Aneurysm sugery. Propofol/remifentanil/NMDR. DOA monitoring (Entropy). MAP 70 , HR 70/min, State entropy 50, Response entropy 70. What do you do? A. ? B. Metaraminol C. Check TOF D. Nothing E. Increase TCI. |
C. Check TOF Possible need for repeat NMBD |
|
|
Interscalene block, patient hiccups...where do you redirect your needle? A. Anterior B. Posterior C. Caudal D. Cranial E. Superficial |
B. Posterior ISB nerve twitches: - Correct: pec, deltoid, triceps, biceps, hand, arm - Too anterior = phrenic nerve - Too posterior = scapula (serratus ant m, thoracodorsal n) - Too posterior = trapezius (accessory n) - Caudad = risk of inserting in cervical spinal cord - Blood = carotid artery |
|
|
What is the SVR in a patient with MAP 100mmHg, CVP 5, PCWP 15, CO 5L/min? A. ?0.8 B. ?3 C. 520 D. 1280 E. 1520 dynes.sec/cm-5 |
E. 1520 dynes.sec/cm-5 SVR = (MAP - CVP) / CO = (100-5) / 5 = 19 mmHg ml /min To convert units, multiply by 80. http://www.cvphysiology.com/Blood%20Pressure/BP021.htm |
|
|
Stellate ganglion A. Anterior to scalenus anterior B. ? C. ? D. ? E. ? |
A. Anterior to scalenus anterior |
|
|
The median nerve A. can be blocked at the elbow immediately medial to the brachial artery B. can be blocked at the wrist between palmaris longus and flexor carpi ulnaris C. can be blocked at the wrist medial to flexor carpi ulnaris D. is formed from the lateral, medial, and posterior cords of the brachial plexus E. provides sensation to the ulnar half of the palm |
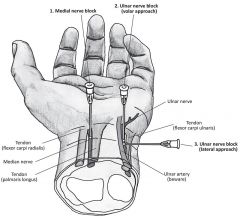
A. can be blocked at the elbow immediately medial to the brachial artery B. No. Median nerve between palmaris longus and flexor carpi radialis. C. No. This is ulnar nerve. D. Formed from lateral and medial cords E. No. Radial Median nerve between palmaris longus and flexor carpi radialis |
|
|
A 75yo male with moderate aortic stenosis (valve area 1.1cm2). Gets mild dyspnoea on exertion but otherwise asymptomatic. Needs hip replacement. A. Continue with surgery B. Beta block then continue C. Get myocardial perfusion scan D. Postpone surgery awaiting AVR E. Postpone surgery awaiting balloon valvotomy |
??A. Continue with surgery NYHA class II (symptomatic with exertion) AHA 2014 treatment algorithm: - step 2 (elective surgery): does the patient have an active cardiac condition (IHD, HF, VHD, arrhythmia)? --> if moderate +, need TTE --> surgical intervention warranted for those who meet std criteria: - "symptomatic pts for elective non-cardiac surgery should have AVR first as they are at risk of sudden death perioperatively (OHA p 63)" --> also need to evaluate for CAD But guidelines also state that "Elevated-risk elective noncardiac surgery with appropriate intraoperative and postoperative haemodynamic monitoring is reasonable to perform in patients with asymptomatic severe aortic stenosis" |
|
|
Baby with tracheo-oesophageal fistula found by bubbling saliva and nasogastric tube coiling on Xray. Best immediate management? A. Bag and mask ventilate B. Intubate and ventilate C. position head up, insert suction catheter in oesophagus D. Place prone, head down to allow contents to drain E. Insert gastrostomy |
C. position head up, insert suction catheter in oesophagus |
|
|
A 60yo man with anterior mediastinal mass, during induction for mediastinoscopy....loses cardiac output, decreased saturations, drop in ETCO2. Management: A. Adrenaline B. CPR C. CPB D. Place prone E. |
D. Place prone Due to compression of SVC |
|
|
The MAIN indication for biventricular pacing is A. complete heart block B. congestive cardiac failure C. VF D. E. |
B. CCF |
|
|
What's the most appropriate mode for neuromuscular monitoring during aneurysm clipping? A. TOF count B. TOF ratio C. Post tetanic count D. ? E. ? |
C. Post tetanic count Aim for TOF of 0 with PTC of 2. A PTC of 2 by palpation suggests no twitch response for about 20-30 minutes; for a PTC of 5, this is about 10-15 minutes. This is clearly the best method for monitoring paralysis for patients in whom you seek to prevent diaphragmatic movement, i.e. micro-neurosurgery; it is best to use infusions of drugs and aim for a PTC of 2. http://www.frca.co.uk/article.aspx?articleid=237 |
|
|
What's the area burnt in the following man? Half of left upper arm, all of left leg and anterior abdomen. A. 27% B. 32% C. 42% D. E. |
Either A or B 0.5 * 0.5 * 9 = 2.25 18 0.5 * 18 = 9 TOTAL = 29.25% If question was actually half of L arm, then answer is B. |
|
|
Torsades, what's not useful? A. Amiodarone B. Isoprenaline C. ? D. E. |
A. Amiodarone Amiodarone prolongs QT - all Ia, Ic, III drugs are out. |
|
|
The intercostobrachial nerve: A. Arises from T2 trunk B. Is usually blocked in brachial plexus block C. Supplies antecubital fossa D. Can be damaged by tourniquet E. Arises from inferior trunk |
D. Can be damaged by tourniquet The intercostobrachial nerve is a lateral cutaneous branch of the second intercostal nerve that supplies sensation to the skin of the axilla. Therefore it is sometimes referred to as the 'tickle' nerve. It leaves the second intercostal space at the midaxillary line and subsequently pierces the serratus anterior muscle to enter the subcutaneous tissues of the axilla. |
|
|
Labour epidurals increase maternal and foetal temperature. This results in neonatal A. Increased sepsis B. Increased investigations for sepsis C. increased non shivering thermogenesis D. Increased need for resuscitation E. Cerebral palsy |
B. Increased investigations for sepsis |
|
|
Maternal cardiac arrest. In making the diagnosis of amniotic fluid embolism, large amount of PMNs surrounding foetal squamous cells are A. Pathognomonic B. Supportive C. Only found at postmortem D. Irrelevant E. Incidental |
B. Supportive |
|
|
Half life of tirofiban: A. 2hrs B. 8hrs C. 12hrs D. 24hrs E. 15 minutes |
A. 2 h Tirofiban is a GP IIb/IIIa inhibitor. Rapid return to baseline function of platelets once infusion ceased. |
|
|
Why is codeine not used in paediatrics? A. Poor taste B. High inter-individual pharmacokinetic variability C. Not licensed for <10 year old D. not as effective as adult when given in ?weight adjusted dose? E. ? |
B. High inter-individual pharmacokinetic variability |
|
|
Best agent to decrease gastric volume AND increase gastric pH before semi-urgent procedure A. Omeprazole B. Cimetidine C. Ranitidine D. Sodium citrate E. |
C. Ranitidine |
|
|
Myaesthenia gravis - features predicting need for post op ventilation EXCEPT A. Prolonged disease B. High dose Rx C. Previous respiratory crisis D. Increased sensitivity to NMBD E. Bulbar dysfunction |
D. Increased sensitivity to NMBD |
|
|
Innervation of larynx A. The internal branch of the superior laryngeal nerve ... B. ? C. D. E. Cuff compression of recurrent laryngeal nerve against thryoid can cause palsy |
E. - Sensory above and inc cords - internal branch superior laryngeal nerve - Sensory below cords - RLN - Motor - RLN to all except cricothyroid + ? interarytenoid, which is ext branch sup laryngeal n |
|
|
The nerve supplying area of skin between greater trochanter and iliac crest: A. subcostal nerve B. ilioinguinal nerve C. genitofemoral nerve D. femoral nerve E. lat cutaneous femoral nerve. |
A. subcostal nerve (ant division T12) LFCN supplies skin distal to GT |
|
|
IV paracetamol: A. late plasma levels around the same as oral B. highly protein bound C. ?30%? renally excreted D. VD 10L/kg E. |
A. late plasma levels around the same as oral |
|
|
Patient with diastolic dysfunction. Is it caused by: A. Restrictive cardiomyopathy B. Dilated cardiomyopathy C. D. E. |
A. Restrictive cardiomyopathy |
|
|
Most likely to result in myocardial infarction: A. intraop myocardial ischaemia B. post op myocardial ischaemia C. D. E. |
B. post op myocardial ischaemia |
|
|
Indication for percutaneous closure of ASD A. Primum < 3cm B. Primum > 3cm C. Secundum < 3 cm D. Secundum > 3cm E. sinus venosus ASD |
C. Secundum < 3 cm CEACCP 2008: "The established indications for atrial septal occlusion are closure of an ostium secundum atrial septal defect (ASD) to prevent shunting of blood from the left to right atrium, and cryptogenic stroke or decompression illness secondary to a patent foramen ovale (PFO). If the defect is very large (>3 cm) or complicated (associated with other abnormalities), or an incomplete rim is detected, referral for surgical closure is indicated. The major types of ASD are the following. 1. Ostium secundum ASD (60–70%) . This is either caused by excessive resorbtion of the thin primum septum or deficient growth of the thicker secundum septum. It manifests after birth as a defect in the fossa ovalis lined by the thin primum septum. 2. Ostium primum ASD (15–20%); a defect of the endocardial cushion, often associated with mitral regurgitation due to an anterior leaflet cleft. 3. Sinus venosus ASD (5–15%) nearly always associated with anomalous pulmonary venous drainage. 4. Unroofed coronary sinus. |
|
|
Respiratory function in quadriplegics is improved by A. abdominal distension B. an increase in chest wall spasticity C. interscalene nerve block D. the upright position E. unilateral compliance reduction |
B. an increase in chest wall spasticity |
|
|
Carbon dioxide is the most common gas used for insufflation for laparoscopy because it A. is cheap and readily available B. is slow to be absorbed from the peritoneum and thus safer C. is not as dangerous as some other gases if inadvertently given intravenously D. provides the best surgical conditions for vision and diathermy E. will not produce any problems with gas emboli as it dissolves rapidly in blood |
C. is not as dangerous as some other gases if inadvertently given intravenously |
|
|
Histamine release in anaphylaxis does NOT cause: A. Tachycardia B. Myocardial depression C. Coronary artery vasodilatation D. Prolonged PR interval E. Decreased impulse conduction |
B. Myocardial depression |
|
|
A device that detects a 10mA difference in active and neutral leads and causes turning off of the circuit within 40 ms. This is a: A. Class 1 device B. Equipotential earthing C. Line isolation monitor D. Residual Current Device E. Fuse |
D. Residual Current Device |
|
|
Which of the following is NOT an absolute contra-indication for MRI? A. cochlear implant B. heart valve prosthesis C. ICD D. pacemaker E. intracranial clips |
B. heart valve prosthesis |
|
|
One lung ventilation and hypoxaemia. After 100% O2 and FOB next step is: A. CPAP 5cm top lung B. CPAP 10cm top lung C. PEEP 5cm bottom lung D. CPAP 5cm top + PEEP 5cm bottom E. ? |
C. PEEP 5cm bottom lung Trial C but variable response. Then do A. |
|
|
Plasma glucose level compared to blood glucose level A. 32% higher B. 14% higher C. Same D. 14%lower E. 32% lower |
B. 14% higher |
|
|
MZ71 With regards to obstructive sleep apnoea (OSA), which of the following statements is INCORRECT? A. hypoxaemia is the main stimulus to arousal B. the main method of treating this syndrome is with Continuous Positive Airway Pressure (CPAP) C. this syndrome is the most likely diagnosis in patients presenting with excessive daytime sleepiness D. this syndrome occurs in up to 5% of adults E. this syndrome rarely has an obstructive component |
E. this syndrome rarely has an obstructive component |
|
|
Management of rhabdomyolysis – best option? A. Haemodialysis B. Bicarbonate C. Frusemide D. IV fluids E. |
D. IV fluids |
|
|
Residual current devices: A. Compare current between active and neutral lines B. C. D. Must be fitted in cardiac protected areas E. Must be fitted in operating theatres |
A. Compare current between active and neutral lines |
|
|
Serotonin syndrome has been reported following SSRI coadministration with: A. Gingko B. Garlic C. Ginger D. St John’s wort E. Vallerian |
D. St John’s wort |
|
|
Child with ?pyloric stenosis and 3 days of vomiting. Which bloods would you expect? A. Na 130 K 4.5 Cl 90 Bic 17 B. Na 130 K 2.5 Cl 87 Bic 24 C. D. E. |
B. Na 130 K 2.5 Cl 87 Bic 24 Pyloric stenosis cause hypochloraemic hypokalaemic metabolic alkalosis |
|
|
Which LMA has highest seal pressure? A. Classic B. Disposable supreme C. Flexible D. Intubating E. Proseal |
E. Proseal |
|
|
Why is tachycardia bad in mitral stenosis? A. B. Increases transvalvular pressure gradient C. D. E. |
B. Increases transvalvular pressure gradient Need low HR to allow diastolic filling of the LV - compromises CO B is true - in a manner of speaking - high HR --> higher LAP (less LV filling) --> higher transvalvular gradient develops to fill the LV --> possible APO |
|
|
You intubate a young male patient for a left thoracotomy with a 39FG Robertshaw tube. When you inflate both cuffs and ventilate the bronchial lumen you get left sided ventilation. When you attempt to ventilate the tracheal lumen the pressures are very high and you get no air entry. Yet when you deflate BRONCHIAL cuff you can ventilate BOTH left and right lungs through the tracheal lumen. The most appropriate step to take next is: A. Change to a 41FG tube B. Change to a 37FG tube C. Deflate both cuffs and insert further cm and recheck D. Deflate both cuffs and withdraw a few cm and recheck E. Pull ETT out and start again. |
C. Deflate both cuffs and insert further cm and recheck Can ventilate bronchial lumen on L --> L-sided OK. Unable to ventilate tracheal lumen --> cuff is herniating over carina. Therefore insert slightly further |
|
|
The average expected depth of insertion of an oral endotracheal tube, from the lip, in a normal newborn infant is A. 7.5 cm B. 8.5 cm C. 9.5 cm D. 10.5 cm E. 11.5 cm |
C. 9.5cm Weight + 6cm |
|
|
What is NOT a feature of high spinal block? A. Hypotension B. C. Hard to speak D. Numb hands E. Tachycardia |
E. Tachycardia |
|
|
Positive predictive value is: A. The proportion of people without disease who are correctly identified as not having the disease. B. The proportion of people with disease who are correctly identified as having the disease. C. The proportion of people with disease who have a positive test result D. The proportion of people without disease who have a positive test result E. etc |
None correct. It is the proportion of people who tested positive who actually have the disease. PPV = TP / (TP+FP) |
|
|
Stellate ganglion block is associated with all EXCEPT: A. Ptosis B. Miosis C. Sweating D. Facial flushing E. Nasal stuffiness |
C. Sweating |
|
|
Recognised clinical associations with dystrophia myotonica include A. development of diabetes mellitus B. abnormal intestinal motility C. cardiomyopathy D. ovarian dysfunction E. all of the above |
E. All of the above Dystrophia myotonica is myotonic dystrophy |
|
|
Left bundle branch block (LBBB) is associated with: A. B. C. D. Relative contraindication to CVL insertion E. |
D. Relative contraindication to CVL insertion
Relative CI to PAC, as RBBB could be serious if LBBB already exists (CHB) |
|
|
When hearing loss occurs following spinal anaesthesia it is usually in which of the following frequency ranges: A. 125 - 1000 Hz B. 1500 - 3000 Hz C. 3500 - 5500 Hz D. 6000 - 10000Hz E. > 11000Hz |
A. 125 - 1000Hz |
|
|
Anaemia in chronic renal failure is characteristically: A. due to haemolysis in the renal vascular bed B. normochromic and microcytic C. due to defective haemoglobin synthesis D. responsive to iron and folate therapy E. associated with increased 2,3-DPG levels in blood cells |
E. associated with increased 2,3-DPG levels in blood cells Anaemia in CKD is typically normocytic, normochromic, and hypoproliferative. Due to lack of EPO. Hb synthesis is normal. May be caused by haemolysis from dialysis. |
|
|
A 12 year old child with hip dislocation at 4pm. Ate something 1 hour after injury. Now 11 pm. Best anaesthetic: A. RSI with ETT B. delay until next day then treat elective C. inhalational induction and continue with face mask D. Reduce immediately with IV sedation E. inhalational induction and continue with face mask |
A. RSI with ETT Emergency procedure to enlocate hip. Treat as unfasted. |
|
|
Central anticholinergic syndrome, which is NOT true: A. Will improve with neostigmine B. Peripheral anticholinergic symptoms C. Caused by anti-Parkinson drugs D. CNS depression E. Associated with agitation, delirium, and hallucinations |
A. Will improve with neostigmine A. Need physostigmine to cross BBB B. Identical symptoms C. Caused by opiates, benzodiazepines, phenothiazines, butyrophenones, ketamine, etomidate, propofol, nitrous oxide, and halogenated inhalation anesthetics as well as by H2-blocking agents such as cimetidine. D. yes E. yes CAS (or central cholinergic blockade) is identical with the central symptoms of atropine intoxication. This behaviour consists of agitation including seizures, restlessness, hallucinations, disorientation or signs of depression such as stupor, coma and respiratory depression. |
|
|
Carcinoid syndrome - finding on examining heart: A. Fine inspiratory crepitations B. Systolic murmur at apex C. Systolic murmur at left sternal edge D. Murmur at apex with opening snap E. Pericardial rub |
C. Systolic murmur at left sternal edge (indicating TR) Carcinoid tumours that invade the liver cause secondary cardiac issues: - due to paraneoplastic effect of vasoactive substances - R heart involved preferentially as substances inactivated by the lungs - endocardial plaques of fibrous tissue cause damage to valves causing stenosis or regurgitation or both |
|
|
Lowering intra-ocular pressure by applying pressure to the globe (e.g. Honan balloon) is typically contraindicated in a patient having A. a revision corneal graft B. a revision trabeculectomy C. an extra-capsular lens extraction D. a redo vitrectomy E. repeat retinal cryotherapy |
B. a revision trabeculectomy |
|
|
Troponin is elevated post-infarct A. 1-2 days B. 2-5 days C. 5-14 days D. 7-21 days E. |
C. 5-14 days |
|
|
Myotome of C6-7 A. Shoulder flexion B. Shoulder extension C. Elbow flexion D. Wrist flexion and extension E. Finger flexion and extension |
D. Wrist flexion and extension |
|
|
Head Trauma patient with unilateral dialated pupil, whats the diagnosis ? A. Global injury B. Optic nerve injury C. Horners syndrome D. Transtentorial herniation E. |
D. Transtentorial herniation |
|
|
The PREDOMINANT pathophysiological effect of restrictive cardiomyopathy is: A. B. Diastolic dysfunction C. D. E. |
B. Diastolic dysfunction |
|
|
When does effect of diclofenac on platelets wear off? A. B. 12 hours C. D. E. |
B. 12 hours |
|
|
Muscle NOT supplied by sciatic nerve: A. B. gluteus maximus C. D. E. |
B. gluteus maximus (supplied by inferior gluteal nerve) |
|
|
Negative predictive value is best described as A. B. Chance of a negative test in people without a disease. C. D. E. |
None correct. NPV = TN / (TN + FN) The proportion of neg test results which are correct (no disease), OR Proportion of subjects with a negative test who are correctly diagnosed. |
|
|
Time to reach peak plasma concentration after injection of 2% lignocaine with adrenaline into epidural space A. 20 min B. 30 min C. 40 min D. 50 min E. 60 min |
B. 30 min ?? Bupivacaine "peak plasma levels following caudal or epidural administration are reached within 30-45 minutes,followed by decline over 3-6 hours" But need lignocaine. http://www.icuadelaide.com.au/files/primary/pharmacology/local_anaesthetics.pdf |

