![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
152 Cards in this Set
- Front
- Back
|
What are the facial bones? |
Mandible, maxilla, zygomatic bone, nasal bone, lacrimal bone, palatine bone, vomer |
|
|
Give the anatomical features of the temporal bone. |
* The thicker part of the bone (the petrous part) houses the middle and inner ear. On the external surface the external auditory (acoustic) meatus and internally a small foramen (hole), the internal auditory meatus, through which 2 cranial nerves pass (the nerve of hearing and balance, the vestibulocochlear nerve CNVIII, and the facial nerve CNVII). * The bar like zygomatic process of the temporal bone forms part of the zygomatic arch – the cheek bone. * The mastoid process is an anchoring site for some neck muscles. The needle like styloid process (often broken off) is an attachment for tongue and pharynx muscles. |
|
|
Give the anatomical features of the sphenoid bone. |
* The sphenoid bones is a butterfly shaped bone. It is a key bone of the cranium because it articulates with all other cranial bones. |
|
|
What is the pterion? |
The pterion (temple) is an important clinical landmark because it marks the position of the anterior branches of the middle meningeal artery. The pterion marks the union of the frontal, parietal temporal and sphenoid bones and the skull is thinnest at this point. Lying in the skull periosteum is a groove in which runs the middle meningeal artery, which supplies the dura and the bone. This artery grooves the bone of the skull and is often implicated inintracranial haemorrhage. |
|
|
Give the anatomical features of the ethmoid bone. |
* The ethmoid bone is very delicate and serves like a sieve through which air can pass. * On the superior surface of the ethmoid bone is the cribiform plate where the olfactory bulbs of the olfactory nerve (the special sensory nerve of smell, CN I) sit. |
|
|
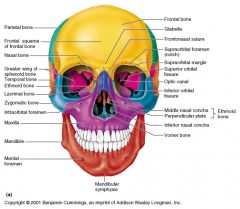
Describe the frontal view of the skull. |
|
|
|
Describe a sagittal section of the skull. |
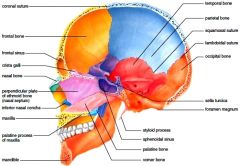
N.B. suture between temporal and occipital = occipitomastoid suture |
|
|
What 3 structures make up the nasal septum? |
Perpendicular plate of ethmoid Vomer Septal cartilage (crest of maxillary and palantine bones) |
|
|
What is the middle meningeal a branch of? |
3rd branch of maxillary artery - branch of external carotid. Runs through foramen spinosum |
|
|
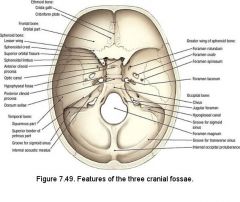
What structures make up the anterior, middle and posterior cranial fossae? |
Anterior - orbital plates of frontal, cribiform plate of ethmoid, small wings and front body of the sphenoid.
Middle - body and greater wing of the sphenoid, parts of temporal, parts of parietal bone
Posterior - parts of occipital bone and mastoid process of temporal bone |
|
|
What parts of the brain do the anterior, middle and posterior cranial fossae hold? |
Anterior - Frontal lobes
Middle - pituitary gland and temporal lobes of the brain
Posterior - Occipital |
|
|
What is a fontanelle? Name them. |
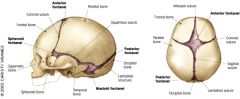
Anatomical feature of an infant skull - soft membranous sutures between cranial bones - allows for rapid stretching and deformation of the neurocranium. |
|
|
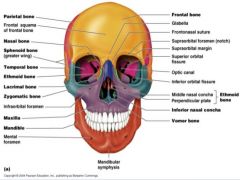
Describe the foramina viewing the skull frontally. |
|
|
|
Describe the foramina of the skull viewing superiorly. |
|
|
|
Describe the foramina of the skull when viewed inferiorly. |
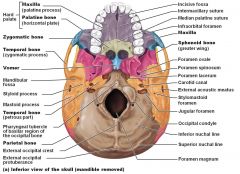
|
|
|
What 3 things do all vertebra have? |
* The body * The vertebral arch forms a vertebral foramen through which the spinal cord passes * The transverse and spinous process is an attachment for the muscles of the back |
|
|
Give some anatomical features of C1 & C2. |
CI The Atlas articulates with occipital condyles of the skull (re: Greek Mythology) C2 The Axis. More similar to a typical vertebra but has a dens process which acts like a pivot, and allows the atlas to pivot around the horizontal axis (ie shaking head to say no) |
|
|
What is the name of the foramen from which spinal nerves exit the vertebral column? |
Intervertebral foramen. |
|
|
What are the: Telencephalon Diencephalon Mesencephalon Metencephalon Myelencephalon? |
* Telencephalon (cerebral hemispheres) * Diencephalon (thalamus, hypothalamus) * Mesencephalon (midbrain) * Metencephalon (pons, cerebellum) * Myelencephalon (medulla oblongata) |
|
|
Which structures constitute the forebrain and the hindbrain? |
Forebrain - prosencephalon - diencephalon + telencephalon
Hindbrain - rhombencephalon - metencephalon + myelencephalon
Separated by midbrain - mesencephalon |
|
|
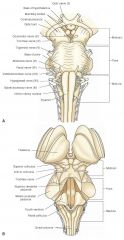
What are features of the ventral surface of the midbrain can you see? |
The midbrain is short and very little of it can be seen in the undissected brain; it is best viewed in a mid-sagittal brain section. Ventrally the cerebral peduncles may be seen. These are massive bundles of nerve fibres descending from the cerebral motor cortex to the brainstem and spinal cord (e.g. corticospinal tract). |
|
|
What are features of the ventral surface of the pons can you see? |
The pons, has a bridge-like appearance and is sharply demarcated both rostrally and caudally from the other parts of the brain stem. Note the transversely ridged appearance of the ventral pons. Four pairs of cranial nerves are associated with the pons (CN V-VIII). |
|
|
What are features of the ventral surface of the medulla can you see? |
The medulla is the rostral continuation of the spinal cord through the foramen magnum. On the ventral surface of the medulla, identify the pyramids. These mark the positions of decussation for the corticospinal tracts.
Lateral to the rostral part of the pyramids are oval swellings that mark the position of the inferior olive, which are functionally associated with the cerebellum. Cranial nerves IX-XII are associated with the medulla. |
|
|
What are features of the dorsal surface of the midbrain? |
The dorsal surface of the midbrain has 2 paired swellings the inferior and superior colliculi (involved in auditory & visual reflexes), is completely buried beneath the overlying cerebral hemispheres. There are two cranial nerves associated with the midbrain (CN III-IV). |
|
|
Where do the gracile and cuneate tubercles lie? |
Either side of the most caudal part of the fourth ventricle, which opens from the central canal about one third of the way up the medulla. This point is the obex. |
|
|
What is the floor of the caudal part of the 4th ventricle? |
The dorsal surface of the medulla.
The 4th ventricle contains CSF that drains into the central canal of the spinal cord inferiorly and into the cerebral aqueduct superiorly. |
|
|
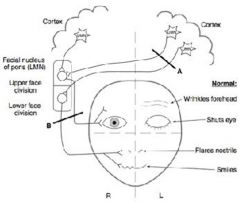
Remember this diagram. |
|
|
|
Describe the anatomy of the olfactory neurones and course of the nerve. |
The olfactory receptor neurons are in the olfactory epithelium (mucosa) in the roof of the nasal cavity. They ascend through the cribiform plate of the ethmoid bone to reach the olfactory bulbs in the anterior cranial fossa. These nerves synapse on neurons in the bulbs. |
|
|
What is associated with anosmia? |
The loss of smell (anosmia) is frequently associated with upper respiratory tract infections, sinus disease and head trauma. Loss of olfactory fibres occurs with aging. Injury to the nasal mucosa or the olfactory bulbs and tracts may also impair smell, i.e. olfactory neurons can be torn away as they pass through a fractured cribiform plate. |
|
|
Describe the course of the optic nerve. |
The optic nerves are surrounded by extensions of the cranial meninges and subarachnoid space, which is filled with CSF. The nerve passes posteromedially in the orbit through the optic canal to enter the middle cranial fossa where it forms the optic chiasm. Here the fibres from the medial (nasal) half of each retina decussate and then join uncrossed fibres from the lateral (nasal) half of the retina to form the optic tract. |
|
|
Recap the different types of blindness at different points of the course of the optic nerve. |

Damage to II anterior to chiasm = ipsilateral anopia Damage to II posterior to chiasm = homonymous left sided hemianopia |
|
|
Describe the course of the occulomotor nerve. |
The oculomor nerves exit the midbrain (medial to cerebral peduncles) and then run anteriorly through the cavernous sinus (on the lateral wall). This nerve divides into superior and inferior branches, which both pass through the superior orbital fissure to innervate the extraocular muscles (excluding lateral rectus and superior oblique) and levator palpebrae superioris. These nerves also send presynaptic parasympathetic fibres to the ciliary ganglion for innervations of the ciliary muscle (accommodation) and sphincter pupillae (constricts pupil). |
|
|
Where can occulomotor lesions come from? |
Pressure from a herniating uncus, a fracture involving the cavernous sinus or from aneurysms. |
|
|
What is the course of the trochlear nerve? |
The trochlear nerve is the smallest cranial nerve, but has the longest intracranial course of the cranial nerves. It arises from the posterior (dorsal) surface of the midbrain (the only cranial nerve to do so), passing anteriorly around the brainstem. The trochlear nerve pierces the dura mater at the margin of the tentorium cerebella and passes on the lateral wall of the cavernous sinus, through the superior orbital fissure to the superior oblique muscle (the only extraocular muscle to use a pulley). |
|
|
What causes damage to the trochlear nerve? What signs are exhibited? |
This nerve is rarely paralysed alone, but may be torn when there are severe head injuries due to its long intracranial course. The characteristic sign of this is double vision (diplopia) when looking down. The superior oblique assists the inferior rectus in depressing the pupil and is the only muscle to do so when the eye is adducted (eg when watching feet when going downstairs). |
|
|
Describe the course of the abducens nerve. |
The abducens nerve emerges from the brainstem, from between the pons and medulla. The nerves then pierce the dura and so have a very long intradural course to the superior orbital fissure. The abducens is somatic motor (general somatic efferent and proprioceptive) to one extraocular muscle, the lateral rectus. |
|
|
What causes damage to the abducensnerve? What signs are exhibited? |
Because of its long intradural course and the sharp bend along the petrosal part of the temporal bone, the abducens can be affected by increased intracranial pressure. Complete paralysis of abducens causes medial deviation due to the unopposed action of medial rectus.
Diplopia is present in all ranges of movement, except when looking away from the lesion. Other than increased intracranial pressure, paralysis of abducens can result from: * pressure from atherosclerotic plaque in internal carotid artery (plaques particularly build up at bends in arteries)* cerebral aneurysm of the circle of Willis (85% occur in this region) * septic thrombosis of the sinus subsequent to infection in the nasal cavities or paranasal air sinuses (the facial vein makes important connections to the cavernous sinus via the ophthalmic vein) |
|
|
Summarise the trigeminal nerve. |
CN V is the somatic sensory and motor to derivatives of the first pharyngeal arch. The trigeminal nerve arises from the lateral aspect of the pons. It has a large sensory root and a smaller motor root. The roots of CN V are comparable to the dorsal and ventral roots of spinal nerves, i.e. the trigeminal ganglion is comparable to the dorsal root ganglion of spinal nerve
The motor root passes inferior to the trigeminal ganglion (just as the ventral roots of spinal nerves do not pass through the DRG). The fibres join the mandibluar division and supply the muscles of mastication. |
|
|
Describe the innervation of the different sensory dermatomes of the face. |
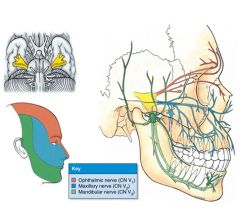
|
|
|
What is the function of the opthalmic nerve? |
CNV1 Opthalmic Nerve – sensory to cornea, upper conjunctiva, upper nasal mucosa, frontal and ethmoidal sinus, anterior dura, superior eyelid and forehead/scalp. The ophthalmic nerve passes anteriorly through the lateral wall of the cavernous sinus and passes through the superior orbital fissure. Note how the ophthalmic nerve divides into the frontal nerve, the nasociliary and the lacrimal nerve. |
|
|
What are the divisions of the frontal nerve? What is the function and exit foramen of the supraorbital nerve? |
Supraorbital and supratrochlear
Supraorbital - palpebral filaments to the upper eyelid, + conjunctiva of the eye, frontal sinus, and the skin from the forehead to the middle of the scalp. Exits via the supraorbital foramen. |
|
|
What is the function of the maxillary nerve? |
Sensory to dura middle cranial fossa, inferior conjunctiva, upper dentition and skin and mucous membranes associated with upper jaw. The maxillary branch exits the middle cranial fossa through the foramen rotundum.
The superior alveolar nerves are not accessible to dentists and so anaesthesia is achieved by injecting the agent into tissues surrounding the root of the tooth and allowing the solution to infiltrate to the terminal branches. |
|
|
What is the function of the mandibular nerve? |
Sensory to oral mucosa and anterior 2/3 of the tongue, lower teeth and jaw, temporal regions of face and external ear. Motor to muscles of mastication. The mandibular nerve leaves the middle cranial fossa through the foramen ovale. |
|
|
What are the branches of the mandibular nerve? Which nerve 'hitches' a lift with one of these branches? |
The lingual nerve and the inferior alveolar nerve.
Chorda tympani = special sensory + presynaptic parasympathetic to submandibular ganglion -> secretomotor innervation to submandibular and sublingual + symp and parasymp fibres
|
|
|
Through which foramina does the inf alveolar nerve enter and leave the mandible? |
Enters via mandibular foramen Leaves via the mental foramen |
|
|
What are the 4 muscles of mastication? |
Masseter Temporalis Medial pterygoid Lateral pterygoid |
|
|
How can CN V be injured, how could you test both the motor and sensory components of CN V? |
CNV can be injured by trauma, tumors, aneurysms or meningeal infections. The sensory and motor nuclei in the pons and medulla may be destroyed by intramedullary tumors or vascular lesions.
Motor: palpate massester and temporalis during function
Sensory: cotton wool touch each division |
|
|
What reflexes are mediated by the trigeminal nerve? |
Corneal
Jaw jerk |
|
|
Describe the course of the facial nerve. |
The facial nerve emerges from pontine medullary junction lateral to abducens, and has 2 divisions, a larger motor root and a smaller intermediate nerve which carries taste and parasympathetic fibres. CN VII exits the posterior cranial fossa through the internal auditory meatus. The nerve then courses through the temporal bone close to the tympanic cavity. While coursing through the temporal bone, the facial nerve gives rise to * parasympathetic to lacrimal gland* nerve to stapedius (a muscle that dampens vibrations of the stapes) * special sensory (taste) to anterior 2/3 tongue * parasympathetic to submandibular ganglion (submandibular & sublingual gland) The facial nerve then exits the temporal bone through the stylomastoid foramen. The nerve then enters the parotid gland and gives rise to the terminal motor branches. |
|
|
How is CN VII damaged? |
CNVII is the most frequently paralysed of all the cranial nerves. Depending on location this can cause paralysis of facial muscles with or without loss of taste or altered secretion from the lacrimal or salivary glands. Because the motor branches of VII are superficial they can easily be damaged through cuts, birth injury or to a fractured temporal bone. Also during parotid or submandibular surgery care must be taken to preserve the branches. Bell's palsy is a unilateral facial paralysis of sudden onset resulting from a lesion of CNVII. A lesion of VII near its origin will result in paralysis of facial muscles on the ipsilateral side. A central lesion (upper motor lesion, UML) results in paralysis on the contralateral inferior face. |
|
|
In what instance would you get forehead sparing? Is this the case in Bell's palsy or stroke? |
Bell's = LMN Stroke = UMN - sparing |
|
|
What is the course of CN VIII? |
The nerve originates from the pontine medullary junction and exits the posterior cranial fossa through the internal auditory (acoustic) meatus. The nerve divides into the cochlear and vestibular components. The cochlear nerve is sensory to the spiral organ for hearing, and the vestibular nerve is sensory to the semicircular ducts for the sense of equilibration. Although the vestibular and cochlear nerves are independent, peripheral lesions often produce concurrent clinical effects. |
|
|
What are symptoms of CN VIII damage? How does this nerve get damaged? |
Hearing loss, vertigo, dysequilibrium, nystagmus.
Acoustic neuroma, vestibular neuritis |
|
|
How does CN VIII exit the inner skull, with which nerve does it do this with? |
Internal acoustic meatus
w/ facial nerve. |
|
|
What are the medullary nuclei of CNIX? |
Four nuclei in the medulla send or receive fibres via IX, 2 motor (nucleus ambiguus and inferior salivatory nucleus) and 2 sensory (sensory of trigeminal nerve and the solitary tract). The three nuclei (in bold) are shared with CNX – Vagus. The sensory fibres from IX join fibres from the X in the pharyngeal plexus. |
|
|
What is the course of IX? |
The glossopharyngeal nerve exits the posterior cranial fossa through the jugular foramen. The nerve follows stylopharyngeus (which it innervates) and passes between the superior and the middle pharyngeal constrictors. The parasympathetic fibres innervate the parotid gland (via the otic ganglion). The somatic sensory fibres and special sensory fibres are afferent to the posterior 1/3 of the tongue and the oropharynx (hence the name glossopharyngeal). There is also an important branch called the carotid sinus nerve. This nerve supplies the carotid sinus (baroreceptor) and the carotid body (chemoreceptor) sensitive to blood gas. |
|
|
Describe injuries to IX? |
Injuries of IX in isolation are rare, as they are usually accompanied by signs of involvement in IX, X and XI as all of these nerves pass through the jugular foramen. A tumour in this area creates multiple cranial nerve palsies, called jugular foramen syndrome. |
|
|
What is jugular foramen syndrome? |
Vernet's sydnrome - paresis of 9th-11th CN Dysphonia/hoarse, deviation of uvula, dysphagia, loss sensory function posterior 1/3 tongue, decrease parotid secretion, loss gag reflex, SCM/trapezius paresis
Cause - glomus tumours, meningiomas, schwannomas/acoustic neuroma |
|
|
What are the function of the vagus nerve? |
The vagus nerve is * somatic sensory to laryngopharynx and larynx* visceral sensory from the thoracic and abdominal organs * somatic motor to palate, pharynx and larynx * visceral motor (parasympathetic) to thoracic and abdominal organs
In the neck the vagus gives rise to the pharyngeal branch (to pharyngeal plexus) and the superior laryngeal nerve. All the muscles of the pharynx and palate (except tensor veli palatini) are supplied by vagus via the pharyngeal plexus and so injury to the pharyngeal branches of vagus results in dysphagia. |
|
|
What is the course of the vagus nerve? |
The vagus arises from a series of rootlets from the lateral surface of the medulla, and exits the posterior cranial fossa through the jugular foramen. The vagus nerve descends through the neck in the carotid sheath to the root of the neck. It lies between the internal jujular vein (laterally) and the common carotid artery (medially). |
|
|
What is the function and course of the spinal accessory nerve? |
A somatic motor nerve to trapezius and sternocleidomastoid. The spinal accessory nerve is so called because it arises from a column of anterior horn motor neurons C1 to C5/6 of the spinal cord. They emerge as a series of rootlets and ascend into the cranial cavity via the foramen magnum and then exit through the jugular foramen (temporarily joining vagus). The accessory nerve then descends in the carotid sheath which it pierces to innervate sternocleidomastoid (SCM). It emerges from the posterior border of SCM and crosses over the posterior triangle of the neck and passes deep to trapezius which it also innervates. |
|
|
When is XI subject to damage and what happens upon damage? |
The accessory nerve is susceptible to injury during some surgical procedures due to its superficial course through the posterior triangle.
No shrugging - trapezius No head turning - SCM |
|
|
Describe the function and course of XII? |
The hypoglossal nerve is somatic motor to the intrinsic and extrinsic muscles of the tongue. The hypoglossal nerve exits the cranium via the hypoglossal canal. It spirals behind vagus to emerge between the internal carotid artery and the internal jugular vein. It lies on the carotid sheath deep to the muscles which attach to the styloid process (including the posterior belly of digastric). |
|
|
What occurs upon injury to XII? Which side does the tongue deviate upon protrusion? |
Injury to XII paralyses the ipsilateral half of the tongue. After some time the tongue may appear shrunken and wrinkled.
Tongue deviates to damaged side as muscles on that side are paralysed. |
|
|
Through which foramen and bone does the internal carotid enter the skull? |
Carotid canal through the temporal bone |
|
|
Which functional areas are supplied from the anterior, middle, and posterior arteries? |
Anterior - foot and leg, gait,
Middle - broca's wernicke's, primary motor cortex, auditory cortex
Posterior - visual cortex, pain and temperature, facial, occulomotor |
|
|
Describe the venous anatomy of the brain. |
Cerebral drainage is by superficial and deep veins and dural sinuses that ultimately drain into the internal jugular veins. The superficial veins in the arachnoid space and the deep veins from the centre of the brain eventually all drain into the dural sinuses. The confluence of the sinuses is the junction of the straight, superior sagittal and transverse sinuses. Each transverse sinus makes an S-shaped turn as the sigmoid sinuses, which are continuous with the internal jugular veins. |
|
|
What structures exit the skull via the jugular foramen? |
Internal jugular v, IX, X, XI |
|
|
Which meningeal layers are the dural venous sinuses found? |
Inner (meningeal layer) and outer (periosteal layer) of the dura mater. |
|
|
What are some features of the surface anatomy of the brain? |
The lobes are subdivided into fissures (deep grooves), gyri (elevated folds) and sulci (shallow grooves between folds). Their function is to increase the surface area. The pattern of sulci and gyri is extremely variable and defining even these relatively major sulci and gyri is not always easy. The sulci provide landmarks for identifying lobes and functional areas of the brain. In general, each lobe can be divided into 3 gyri by 2 sulci. |
|
|
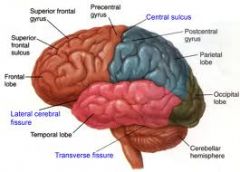
Describe the lateral view of the brain in terms of sulci and fissures. |
|
|
|
What are the functions of: Air sinuses Basal ganglia Blood sinuses Cerebellum Cingulate cortex Corpus callosum Fornix Hippocampus Hypothalamus Internal capsule Medulla oblangata Pituitary gland Pons Thalamus? |
Air sinuses - vocal resonance Basal ganglia - execution of voluntary motor control, routine behaviours Blood sinuses - venous drainage Cerebellum - motor control (balance & coordination) & language Cingulate cortex - memory relay Corpus callosum - communication between both hemispheres Fornix - memory storage Hippocampus - memory formation Hypothalamus - controls body temperature, hunger, thirst, circadian cycles & link between nervous and endocrine system Internal capsule - white matter containing ascending and descending axons Medulla oblangata - Involuntary functions (breathing, heart rate, blood pressure) Pituitary gland - endocrine gland Pons - controls respiration and contains nuclei for CNV-VIII (control of their function) Thalamus - relay station for sensory & motor info to cortex (conscious perception) |
|
|
What is the limbic system? |
The limbic system is a group of structures located on the medial aspect of each cerebral hemisphere and diencephalon. Its cerebral structures encircle (limbus=ring) the upper part of the brain stem. The limbic system is our emotional, or affective (feelings) brain. Two parts seem especially important in emotions, the amygdale and the anterior part of the cingulated gyrus. |
|
|
What are the roles of the amygdala and the cingulate gyrus? |
The amygdale recognizes angry and fearful facial expressions, assesses anger and elicits the fear response. The cingulated gyrus plays a role in expressing our emotions through gestures and in resolving mental conflicts when we are frustrated. |
|
|
Revise the anatomy of the limbic system. |
|
|
|
Describe the anatomy of the reticular formation. |
The reticular formation extends through the central core of the medulla oblongata, pons and midbrain. It is composed of loosely clusters of neurons that form three broad columns along the length of the brain stem. The outstanding feature of reticular neurons is their far flung axonal connections, making them ideal for governing the arousal of the brain. |
|
|
How does the reticular formation communicate with the cortex? |
Certain reticular neurons, unless inhibited by other brain areas, send a continuous stream of impulses (via thalamic relays) to the cortex, which keeps the cortex alert and conscious and enhances its excitability. This system also acts like a filter for a flood of sensory inputs. Repetitive, familiar, or weak signals are filtered out, but unusual, significant or strong impulses do reach consciousness. |
|
|
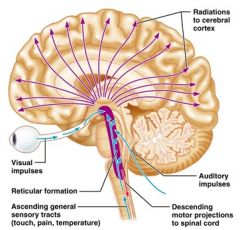
Remember this image for the relay of the reticular formation. |
|
|
|
What are some other features of the reticular formation? |
This system is also inhibited by sleep centres, depressed by alcohol, sleep inducing drugs and tranquilizers. Severe injury to this system results in permanent unconsciousness. Some of the nuclei in the reticular formation project to motor neurons in the spinal cord (reticular spinal tract) and help control skeletal muscles during coarse limb movements. Other reticular motor nuclei, such as vasomotor, cardiac and respiratory centres of the medulla oblongata are autonomic centres that regulate visceral motor functions. |
|
|
What is the basal ganglia? |
The basal ganglia is a subcortical structure and the definition of the precise structures forming the basal nuclei is controversial. Most anatomists agree that the caudate nucleus, putamen and globus pallidus constitute most of the mass of each group of basal nuclei. The basal nuclei are functionally associated with the subthalamic nuclei of the diencephalon and the substantia nigra of the midbrain. |
|
|
What is the role of the basal nuclei? |
The role of basal nuclei in motor control is complex and there is evidence they play a part in regulating attention and cognition as well. The striatum receives input from the entire cerebral cortex, as well as other subcortical areas. The basal nuclei project back to the cortex (premotor and prefrontal cortices) via relay through the thalamus. The basal ganglia exert an inhibitory influence on a number of motor systems. |
|
|
What are the putamen and the globus pallidus collectively called?
What are the putamen and the caudate nucleus collectively called? |
Lentiform nucleus
Striatum |
|
|
What occurs upon release of dopamine from the substantia nigra? |
When dopamine is released from the substantia nigra, there is a release of this inhibition that permits a motor system to become active. The "behaviour switching" that takes place within the basal ganglia is influenced by signals from many parts of the brain, including the prefrontal cortex, which plays a key role in executive functions. |
|
|
What is the role of the basal ganglia with respect to the control of the cortex? |
The basal nuclei are particularly important in starting, stopping and monitoring the intensity of movements executed by the cortex, especially those that are relatively slow or stereotyped (e.g. arm-swinging during walking). Additionally, they inhibit antagonistic or unnecessary movements, thus their input seems necessary to our ability to perform several activities at once. Disorders of the basal ganglia result in either too little or too much movement as exemplified by Parkinson’s disease and Huntington’s chorea, respectively. |
|
|
What is the blood supply to the BG? When can this be impaired? |
MCA - lenticulostriate branch, can be impaired during lacunar infarcts (LACIs) - small infarcts in the deeper parts of the brain, with deep penetrating arteries implicated |
|
|
What is the role and function of the cerebellum? |
The cerebellum (‘small brain’) accounts for about 11% of total brain mass. By processing inputs received from cerebral motor cortex, various brain stem nuclei and sensory receptors, the cerebellum provides the precise timing and appropriate patterns of skeletal muscle contractions for smooth, coordinated movement and agility. Cerebellar activity occurs without our awareness of its functioning. The cerebellum also appears to play a role in cognition. The cerebellum recognizes and predicts sequences of complex movements of the limb. Some non-motor functions include word association and puzzle solving. |
|
|
Describe the gross anatomy of the cerebellum. |
The cerebellum is bilaterally symmetrical, and its two cerebellar hemispheres are connected by a worm-like vermis. Deep fissures subdivide each hemisphere into anterior, posterior and flocculonodular lobe. The latter is situated deep to the vermis and cannot be seen in a surface view. Like the cerebrum, the cerebellum has outer cortex of gray matter, internal white matter and small deeply situated, paired masses of gray matter, the most familiar of which are the dentate nuclei. The distinctive pattern of white matter in the cerebellum resembles a branching tree, called arbour vitae (‘tree of life’). |
|
|
What are the roles of the different areas of the cerebellum? |
The anterior and posterior lobe of the cerebellum, which coordinate body movements, have completely overlapping sensory and motor maps of the entire bodies. The medial portions influence the motor activities of the trunk, whereas the intermediate pats of each hemisphere are concerned with more distal parts of the limbs in skilled movements. The flocculonodular lobe receives inputs from the inner ear to adjust posture and balance. |
|
|
What are the cerebellar peduncles? |
There are 3 pairs of fibre tracts connecting the cerebellum to the brain stem. Virtually all fibres entering and leaving the cerebellum are ipsilateral. The superior cerebellar peduncles connect the cerebellum to the midbrain and carry outputs from the cerebellum to the cerebral cortex via relay in the thalamus (there are no direct connections to the cortex). The middle cerebellar peduncles carry input to the cerebellum from the pons, advising the cerebellum of voluntary motor activities initiated by the cortex (relayed in the pons). The inferior cerebellar peduncle carry input to the cerebellum from the medulla oblongata conveying sensory information to the cerebellum from muscle proprioceptors of the body (What is the name of this tract? SC) and sensory information concerned with equilibrium and balance from the inner ear via brain stem relays. |
|
|
What is the functional scheme of cerebellar processing for motor activity? |
1. The motor areas of the cortex notify the cerebellum of their intent to initiate voluntary muscle contraction. What is the name of this tract? Corticopontinecerebellar tract - pyramidal fibres 2. At the same time, the cerebellum receives information from proprioceptors throughout the body. This information enables the cerebellum to evaluate body position and momentum. 3. The cerebellum calculates the best way to coordinate the force, direction and extend of muscle contraction to prevent overshoot, maintain posture and ensure smooth, coordinated movement. 4. Then via the superior peduncles (output), the cerebellum dispatches to the cerebral motor cortex its ‘blueprint’ for coordinating movement. The cerebellum also sends fibres to neurons in the brain stem that influence motor neurons in the spinal cord. |
|
|
What are cerebellar tonsils? What happens upon elongation? |
The cerebellar tonsil is analogous to a rounded lobule on the undersurface of each cerebellar hemisphere, continuous medially with the uvula of the cerebellar vermis and superiorly by the flocculonodular lobe.
Elongation of the cerebellar tonsils can, due to pressure, lead to this portion of the cerebellum to slip or be pushed through the foramen magnum of the skull resulting is tonsillar herniation. This is a life-threatening condition as it causes increased pressure on the medulla oblongata which contains respiratory and cardiac control centres. |
|
|
What are the symptoms of cerebellar injury? DANISH |
Dysdiadochokinesis - is the impaired ability to perform rapid, alternating movements |
|
|
What is the diencephalon? |
Forming the central core of the forebrain and surrounded by the cerebral hemisphere, the diencephalon consists largely of three structures: the thalamus - lateral to 3rd ventricle, hypothalamus - anterior to 3rd ventricle and the epithalamus - posterior to 3rd ventricle (pineal gland). They collectively enclose the 3rd ventricle. |
|
|
Describe the gross anatomy of the thalamus. |
The thalamus (Greek meaning ‘inner room’) consists of bilateral egg-shaped masses. These masses are connected at the midline by the interthalamic adhesion. The thalamus contains a large number of nuclei, most named according to their relative location, and each has a functional modality and projects to or receives fibres from the cerebral cortex. |
|
|
What is the general function of the thalamus? |
Afferents from all senses and all parts of the body converge in the thalamus and synapse with at least one of its nuclei. Within the thalamus, information is sorted and ‘edited’, thus the thalamus plays a key role in mediating sensation, motor activities, cortical arousal, learning and memory. It is the gateway to the cerebral cortex (to consciousness). |
|
|
What are the functions of: * Lateral geniculate nucleus (LGN)* Medial geniculate nucleus * Ventral posterior lateral nucleus * Anterior nucleus * Ventral lateral nucleus * Ventral anterior nucleus? |
* Lateral geniculate nucleus (LGN) - visual pathway, sensory information from retina and connects optic nerve to occipital lobe * Medial geniculate nucleus - auditory part of the thalamus - represents thalamic relay between inferior colliculus and auditory cortex * Ventral posterior lateral nucleus - touch pain and pressure from neospinothalamic (fast ad) + medial lemniscus * Anterior nucleus - alertness, learning, memory * Ventral lateral nucleus - motor input from basal ganglia and cerebellum * Ventral anterior nucleus - motor input from basal ganglia |
|
|
What is the function of the epithalamus? |
The epithalamus consists of the pineal gland, which secretes melatonin, which together with the hypothalamus regulates the sleep and wake cycle. |
|
|
What are the characteristics of CSF? |
Cerebrospinal fluid (CSF) is found in and around the brain and spinal cord, forms a liquid cushion and gives buoyancy to the brain. By floating the brain, the CSF effectively reduces brain weight by about 97% and prevents the brain from crushing under its own weight (1.3 kg). It also protects the brain and spinal cord from blows and other trauma. Additionally, although the brain has rich blood supply, the CSF helps nourish the brain, and there is evidence of it carrying chemical signals (such as hormones) from one part of the brain to another. CSF is similar in composition to blood plasma, from which it is formed, but it contains fewer proteins and its ion concentrations are different. In adults, the total CSF volume of about 150ml is replaced every 8h, hence about 500ml of CSF are formed daily. |
|
|
Where is CSF formed? |
Ependymal cells of the choroid plexus - 2/3rs of CSF = venous plexus in all 4 ventricles of the brain. |
|
|
Describe the anatomy of the brain ventricles. |
|
|
|
Describe the flow of CSF in the brain. |
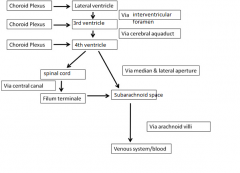
|
|
|
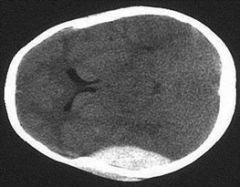
CSF is produced and drained in a constant rate. If something such as a tumour, however, obstructs its circulation or drainage, it accumulates and exerts pressure on the brain. What is this condition called? |
Hydrocephalus: increased ICP - noncommunicating and communicating
In new born babies, this condition causes the head to enlarge, this is possible because the skull bones are not fused. In adults, however, brain damage will occur more rapidly because the skull is rigid and hard, and accumulating fluid compresses blood vessels serving the brain and crushes the soft nervous tissue. |
|
|
What are the 5 layers of the scalp? |
* Skin: thin, has many sweat & sebaceous glands, abundant arterial supply & venous drainage
* Connective tissue: thick and richly vascularised and is also well supplied with nerves * Aponeurosis: strong tendinous sheet between muscle bellies of frontalis and occiptalis * Loose connective tissue: sponge like has potential to distend with many spaces; allows free movement of scalp * Pericranium: dense connective tissue, periosteum of the calvaria (Skull bones) |
|
|
Describe the anatomy of the orbit. |
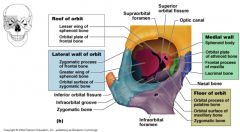
|
|
|
Describe the anatomy of the dura mater. |
The dura mater is the outermost layer of the meninges and is a dense fibrous membrane composed of a tough external layer and an inner meningeal layer. This inner layer draws away from the outer layer to form dural folds (septa) that separate different brain regions from each other. The largest of these septa is the cerebral falx. |
|
|
What is the anatomical function of cerebral falx? |
It separates the 2 cerebral hemispheres. The falx becomes continuous with the cerebellum tentorium in the midline. |
|
|
What is the cerebellum tentorium? |
The cerebellum tentorium separates the cerebellum from the occipital lobe of the cortex. It covers the posterior fossa structures (hindbrain) and supports the temporal and occipital lobes.
It contains a gap – the tentorial notch – through which the brainstem and blood vessels pass to enter the middle cranial fossa. Tumours that occupy this space raise the intracranial pressure and may cause herniation of the temporal lobe (uncus) through this space. |
|
|
What is the anatomy of the two inner meningeal layers? |
The pia is microscopically thin and follows the contours of the brain tissue, while the arachnoid surrounds the brain more loosely. The subarachnoid space contains a network of connective tissue strands, blood vessels and nerves and CSF. The arachnoid is on either side of the longitudinal fissure between the hemispheres on a real brain, the arachnoid granulations appear as numerous whitish nodules along a line parallel with the fissure. These are sites of return of CSF to the venous circulation, e.g. the superior sagittal sinus. |
|
|
Describe the anatomy of the cranial meninges. |
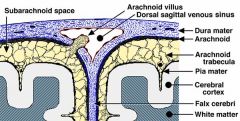
|
|
|
What are the features of Xray cerebral imaging? |
X-rays utilise the differential absorption of x-rays. They provide the contrast to the image. Structures like the brain and spinal cord are mostly water, so they do not absorb enough x-rays and are largely invisible by this technique. Bone absorbs much x-ray energy, so it is easily seen. |
|
|
What are the features of cerebral MRI imaging? |
Magnetic resonance imaging(MRI) utilises the magnetic properties of hydrogen nuclei. This method is particularly sensitive for distinguishing CNS tissue. It is particularly sensitive for imaging areas of demyelination, spinal cord lesions and brain lesions. It is the best method of choice to study the spinal cord, nerve roots and disc spaces. |
|
|
What is the difference between T1 and T2 weighted MRIs? |
In T1-weighted images, CSF, bone, air and blood emit almost no signal and are rendered black whereas fat and bone marrow have a high signal and appear white. Brain tissue is intermediate between these and gray matter appears slightly darker than white matter. In T2-weighted images the reverse occurs. T1 images are most often used to reveal soft tissue damage whereas T2 is used for visualising damage involving fluid containing structures. |
|
|
What can be used to enhance MRI contrast? |
Gadolinium (Gd) contrast is used to enhance contrast. Gd does not cross the blood brain barrier (BBB) and any lesion that disrupts the BBB displays increased signal intensity. |
|
|
How do CT scans work? What is it particularly sensitive to? |
Computed Tomography (CT) uses x-rays to convert the differential absorption of x-rays into an electrical signal which is then converted into an image by a computer. It is a quick imaging method that provides good resolution and contrast of anatomical features; however, images can only be obtained in 1 plane at a time making 3-d reconstruction of lesions difficult. CT is used as the first line in diagnostic imaging where stroke is suspected.
It is particularly sensitive to haemorrhagic stroke, and its role here is usually to eliminate a bleed as this profoundly affects the aims of treatment. If stroke is clinically suspected but not seen, further investigation with contrast scans, or MRI may be indicated. |
|
|
Which arteries are contrasts injected into in angiograms? |
R & L Internal carotids |
|
|
What MCA infarct would cause aphasia? |
Dominant hemisphere - usually left sided damage = aphasia Non-dominant hemisphere - usually right sided damage = contralateral neglect syndrome. |
|
|
What functional deficits result from MCA occlusion? |
1. PARLAYSIS(/weakness) of contralateral face/arm 2. SENSORY loss of contralateral face/arm 3. aphasia/neglect 4. Visual disorders - Déviation conjuguée 5. Ataxia - faciobrachial > lower limb |
|
|
What are possible causes for enlarged brain ventricles? |
Obstruction to CSF flow through ventricular system/subarachnoid space - stenosis cerebral aqueduct, obstruction interventricular formaina - tumours, haemorrhages, infection, congenital malformation
Overproduction CSF - choroid plexus papilloma/villous hypertrophy |
|
|
Where are arachnoid granulations located? |
Superior sagittal sinus |
|
|
What are signs and symptoms of hydrocephalus? |
Headaches, vomiting, nausea, papilloedema, sleepiness, coma. Elevated ICP - uncal/cerebellar tonsilar herniation - BS compression |
|
|
How is hydrocephalus treated? |
Cerebral shunting; cerebral ventricular catheterisation - VP shunting! Also Vatrial and Vpleural. |
|
|
What is the epidemiology of head injury? For every 100 survivors, what types of recoveries do they all make? |
Head injury accounts for around 1% of deaths in developed countries, a third of trauma deaths and up to half of road traffic accident deaths. In the UK, for every 100 survivors, 60% make a good recovery, 20% have minor psychiatric/psychological problems, 15% are severely disabled and 5% remain in a persistent vegetative state. |
|
|
What are the most usual neuropathological causes of long term disability after head injury? |
Damage to axons and hypoxic-ischaemic damage, sustained at the time of injury. |
|
|
What are the 2 factors that determine brain damage? |
Impact to the head
Movement of the brain |
|
|
What 2 classifications are there for head injury? |
Clinically, the most useful is as focal or diffuse injury. The term ‘focal’ indicates pathology that can be seen on a CT or MRI scan – and which may be neurosurgically treatable. ‘Diffuse’ brain injury refers to microscopic damage which cannot be demonstrated by any of the current imaging techniques, but which the clinicians diagnose because they have an unconscious patient whose scan shows very little obvious damage. |
|
|
What are the 4 types of skull fractures? |
The type of fracture is partly determined by the nature of the object involved. A depressed fracture, in which an area of skull is driven inwards, needs to be repaired by a neurosurgeon. Infection is a possible consequence of compound skull fractures, in which the scalp is torn, and also of skull base fractures where there is communication with the nasal sinuses. Linear closed fractures of the vault (in which the skin is not broken) do not usually require treatment. |
|
|
What are 'blow out' fractures? |
Blows around the eye region may fracture the orbit. The medial and inferior walls are paper-thin and indirect injuries that displace the orbital walls produce “blow-out fractures”. These fractures may involve damage to the air sinuses. Orbital fractures often produce intraorbital bleeding producing pressure on the eyeball and “black eyes” as the blood accumulates in the soft tissues around the eye. |
|
|
What occurs upon zygomatic bone fracture? |
If the zygomatic bone is fractured, double vision often results either due to damage of the suspensory ligament, which no longer holds the eye in the horizontal plane or because a bone fragments/ obstructs the recti muscles. Orbital fractures can be difficult to see on X-rays but are readily identifiable in CT scans. |
|
|
What are the consequences of orbital fractures? |
Orbital fractures may damage the cavernous sinus and thus the blood/nerve supply to the eye. The abducens nerve and internal carotid artery run in its substance and the oculomotor, trochlear, ophthalmic and maxillary nerves run in its lateral wall. Infection can spread to the cavernous sinus via the ophthalmic vein as a result of such fractures |
|
|
What are the features of mengingeal bleeds? |
Bleeding in the spaces around the brain is a common feature of head injury. In trauma, meningeal bleeding may be extradural, subdural, or subarachnoid. Extradural and subdural haemorrhages usually need to be evacuated neurosurgically, and if left untreated are important causes of death, because they act as mass lesions. |
|
|
What are the effects of mass lesions on the skull? |
The cranial cavity is subdivided by the relatively rigid tentorium and falx cerebri into three compartments with limited capacity to accommodate accumulations of blood or swelling due to oedema without an increase in pressure. Differences in pressure between two adjacent intracranial compartments, or between an intracranial compartment and the spinal canal cause the brain to be displaced into the lower pressure compartment (i.e. internal herniation).Raised intracranial pressure (ICP) can also lead to external herniation of brain tissue through a skull fracture or craniotomy. |
|
|
What are the 3 types of cerebral herniation? |
Subfalcine - most common; displacement of the brain usually cingulate gyrus beneath the free edge of the falx cerebri to the contralateral hemisphere
Uncal/transtentorial - herniation of medial temporal lobe from the middle of the posterior fossa across the tentorial opening - gap between the midbrain and the edge of the tentorium - compresses ipsilateral III & PCA.
Cerebellar tonsilar - pons against clivus and cerebellar tonsils into foramen magnum |
|
|
What is the falx cerebri? |
The falx cerebri is a double-fold of dura mater that descends through the interhemispheric fissure in the midline of the brain to separate the cerebral hemispheres. |
|
|
What is extradural haemorrhage? |
Extradural haemorrhage occurs in approximately 10% of severe head injuries and up to 15% of fatal head injuries. It is important to understand the anatomy and natural history of EDHs, because if an EDH is not diagnosed and treated, it will kill the patient. Extradural haemorrhage is an impact phenomenon. It occurs when a blood vessel running between the skull and the dura is torn, in association with a skull fracture. The vessel damaged is either an artery or one of the large venous sinuses; in many cases, it is the middle meningeal artery that is torn. |
|
|
What is the pathophysiology of EDHs? |
EDHs accumulate slowly, usually over a period of hours, because in most cases the dura is strongly adhered to the inner aspect of the calvaria, and the enlarging clot slowly strips the dura from the skull. The patient may appear to be relatively normal after the injury and only becomes unconscious as the haemorrhage enlarges, and begins to press on the brain. Because there is so little reserve volume inside the skull, haematomas of >75 ml are usually fatal. If an EDH is not diagnosed and treated, death is caused by a combination of mass effect and raised intracranial pressure. |
|
|
What are subdural haemorrhages? |

Acute SDH is completely different from EDH. It is principally caused by movement of the brain, not by impact. The movement responsible is acceleration, with or without deceleration. When the head is accelerated, the inertia of the brain causes its movement to lag behind that of the skull. This leads to traction on bridging veins running between brain and dura mater, which get torn. |
|
|
What is the pathophys of SDHs? |
Blood from the ruptured vessels spreads freely through the subdural space and can envelop the entire hemisphere. Because of the forces involved in producing a subdural haemorrhage, there is very often damage to axons in the underlying brain as well. This is in contrast to an EDH, where the underlying brain tissue is not usually severely damaged. |
|
|
What is the clivus? |
The clivus (Latin for "slope") is a part of the cranium, a shallow depression behind the dorsum sellæ that slopes obliquely backward. It forms a gradual sloping process at the anterior most portion of the basilar occipital bone at its junction with the sphenoid bone
The pons sits on the clivus. |
|
|
What is a subarachnoid haemorrhage? |
Subarachnoid bleeding in trauma is almost always insignificant, seen on the surface of the hemispheres in relation to fracture sites or contusions. Occasionally, if a vessel at the base of the brain is damaged, a large amount of blood collects in the subarachnoid space over the base of the brain. |
|
|
What are the types of SAH? |
Spontaneous subarachnoid haemorrhage is quite different from traumatic subarachnoid haemorrhage, resulting from rupture of an aneurysm on a vessel of the circle of Willis (e.g. a Berry aneurysm). This latter type of subarachnoid haemorrhage is a form of haemorrhagic stroke. |
|
|
What are brain contusions? |
These are foci of superficial bruising of the brain. Contusions occur on the crests of gyri, particularly where the brain moves over the roughened floor of the skull, namely: * Inferior surface of the frontal lobes* Lateral and inferior surfaces of the temporal lobes * Region adjacent to the lateral fissures * Orbital poles |
|
|
What is a laceration? |
The term ‘laceration’ is used when the arachnoid and brain are damaged, usually at the site of a fracture, a contusion or a large intracerebral haematoma. |
|
|
What is diffuse axonal injury? |
Diffuse axonal injury (‘DAI’) is the term given to widespread damage to axons, caused by acceleration of the head, with or without deceleration. As with subdural haemorrhage, this is primarly a non-impact phenomenon. The patient with DAI is unconscious from the time of injury, remains in prolonged coma, and is severely disabled or vegetative until death, which is usually caused by bronchopneumonia or other infection. |
|
|
How do brain tumours cause brain damage? |
Mass effect & raised ICP can also be caused by brain tumours which slowly expand. The clinical presentation may develop over several months. Epileptic seizures may occur and neurological examination may reveal focal deficits. Many brain tumours are due to abnormal proliferation in glial cells e.g. astrocyotoma’s and ependymoma’s (lining the 4th ventricle). Others may affect the meninges and some affect the cerebellum such as medulloblastomas. Brainstem tumours have a particularly poor prognosis. |
|
|
What are the positive and negative signs seen in basal ganglia abnormalities? |
1. Negative signs are actions patient wants to perform but cannot because the cells no longer elicit activity. They often result in hypokinetic disorders e.g. Parkinson’s disease.
2. Positive signs are actions patient does not want to perform but cannot prevent because of a loss of control over the cells or due to release (disinhibition) of other parts of the motor system. They often result in hyperkinetic disorders e.g. Huntington’s disease (chorea) or hemiballismus. |
|
|
What is Huntington's? |
This is a genetically inherited disease due to a single gene defect in chromosome 4, which leads to a progressive loss of cholinergic and GABAergic cells in the striatum. It produces continuous dance-like movements of the face and limbs. |
|
|
What are the 2 types of motor injury after cerebellar injury? |
1. HYPOTONIA –manifests as muscle weakness and loss of motor tone. It results in a floppy, loose-jointed, rag-doll like appearance with pendular reflexes and the patient appears “drunk”. 2. ATAXIA - which manifests as “errors in the rate, range or force of movement” |
|
|
What drug is the cerebellum particularly susceptible to? |
ALCOHOL. If you get drunk, you show many of the symptoms of mild cerebellar damage! e.g. slurred or incoherent speech, incoordination, ataxic gait, clumsiness, double vision, are all signs of cerebellar damage. These disorders reflect the role of the cerebellum in the co-ordination of skilled movements. |
|
|
What happens upon lesions of the cerebellum? |
Different parts of the cerebellum coordinate movement in different parts of the body. Focal lesions of the cerebellum produce deficits on the same side of the body as the lesion. Remember that movements are not initiated in the cerebellum. Lesions of the cerebellum also result in disequilibrium (loss of balance) characterized by gait & truncal ataxia. |
|
|
What are the types of cerebellar tumour? |
1. Astrocytoma (30%). Most frequently located in the cerebellar hemisphere. Can be surgically removed with good morbidity. 2. Medulloblastoma (20%) Malignant and arise from granular layer of cerebellar cortex. Invade 4th ventricle and can block CSF flow. 3. Ependymoma (15%) Occur in 4th ventricle and obstruct CSF flow. |
|
|
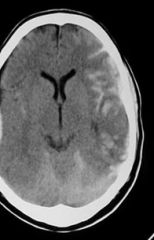
What is MS? |
Multiple Sclerosis attacks the central nervous system. The destruction of the myelin sheath of CNS axons by the immune cells leads to impaired communication between nerve cells and neurological symptoms such as abnormal sensations, vision problems, and weakness. Immune system T cells normally in the bloodstream become activated against components of the brain myelin. They cause local inflammation in scattered regions of the brain and spinal cord once they cross the barrier between the bloodstream and CNS. Astrocytes form scars (plaques) where myelin formerly existed. Inflammation, loss of myelin, and nerve fibres, and the following scarring result in reduced transmission of nerve signals within the CNS. Nerves can regain myelin, but process is not fast enough to avoid the functional deterioration that occurs in MS. Remyelinated axons are thinner with shorter internode regions than intact axons. Types of symptoms and severity vary widely due to the location of the scar tissue and extent of demyelination. |
|
|
Look at this image of an MS lesion. |

n.b. dawson's fingers |

