![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
15 Cards in this Set
- Front
- Back
|
What are the dietary sources of fructose and how is dietary fructose absorbed?
|
From:
Sucrose: digested by intestinal sucrase Fruits and Honey High fructose Corn Syrup Sorbitol (can form fructose by sorbitol dehydrogenase) It is absorbed by GLUT-5 via facilitated diffusion. |
|
|
What are the two enzymes in the liver needed for metabolism of dietary fructose?
|
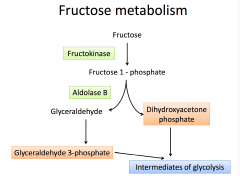
Fructokinase and Aldolase B
|
|
|
What is high fructose corn syrup (HFCS)?
|

It is commonly used as a sucrose substitute in beverages and one of the reasons for obesity.
Limiting it is highly recommended. Hypoglycemia occurs following consumption of hypoglycemia (no fasting state) |
|
|
What is Benign Fructosuria (essential)?
|
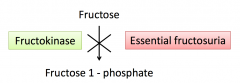
Is the deficiency of enzyme fructokinase in liver.
Fructose is not metabolized and accumulates in liver, does not contain toxic metabolites so no symptoms. Must test urine for a reducing sugar, that is not glucose or galactose. |
|
|
What is Hereditary Fructose Intolerance and what are the affects and why?
|
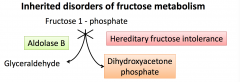
Is the deficiency of Aldosa B in liver.
Fructose is phosphorylated to Fructose 1-P but cannot be further metabolized. This is a toxic metabolite. This is results in trapping of Pi from (ATP), this will inhibit gluconeogenesis and also inhibits glycogenolysis (glycogen phosphorylase needs ATP)----> Results in hypoglycemia due to low sugar, following indigestion of sucrose - NOT FASTING. Back flow of Fructose results in reducing sugar in liver. Difference is symptoms of drowsy and apathetic. |
|
|
Why should individuals with fructose disorders not be given sorbitol?
|
Sorbitol can be converted to fructose via sorbitol dehydrogenase. Hence they should also avoid sorbitol.
No need to avoid glucose - only fructose and sorbitol |
|
|
What is aldose reductase?
|
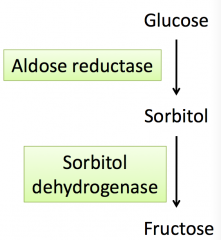
It is rich in lens, retina and peripheral nerves and seminal vesicles. It converts glucose to sorbitol when blood glucose is high.
Also converts galactose to galactitol. |
|
|
What is the correlation of diabetis mellitus and polyl pathway?
|
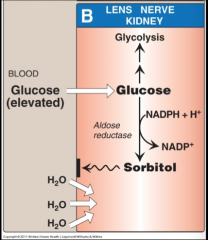
High glucose levels results in lens converting glucose to sorbitol (via aldose reductase).
Sorbitol increased water content in the lines and results in cataract. |
|
|
What is galactosemia?
|
Elevated galactose in the blood results in entry of galactose into the lens where it is converted to galactitol by aldose reductase. This also increase water content in lens and causes cataracts.
|
|
|
How is galactose metabolism?
|
Galactose is monosaccharide in lactose (milk) β1→4 linkage).
Lactose is hydrolyzed by lactase to form galactose and glucose. Galactose is absorbed into the intestinal mucosal cell by SGLT-1 (sodium dependent glucose transporter-1) It is then metabolized in the liver via 3 enzymes: 1) Galactokinase 2) Galactose 1-phosphate uridyl transferase 3) Epimerase These actions result in production of glucose used for glycogen synthesis. |
|
|
What is classical galactosemia and what are the symptoms?
|
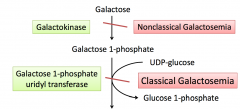
Is a deficiency of GALT (galactose 1-phosphate uridyl transferase).
This results in accumulation of galactose of 1-phosphate, this causes back flow and accumulation of galactose in blood. This will results in loss of galactose in the urine. Accumulation of galactose 1-phosphate in liver results in trapping of Pi, which means there is low ATP for gluconeogensis and glycogenolysis. This will show as hypoglycemia immediately following feeding of galactose or lactose (milk) The accumulation of galactose 1-P and galactitol (formed by polyl) - which are toxic to liver resulting in damage and hepatomegaly - causing jaundice. Will find galactose in urine. |
|
|
What is the affect of galactitol in classical galactosemia?
|
It can accumulate in the lens due to galactosemia and cause cataracts. It is made via galactose by aldose reductase.
It also can accumulate in brain and cause neurological damage and learning disability in children. |
|
|
How is galactosemia managed?
|
Dietary exclusion - lactose free milk
Levels of galactose 1-phosphate is monitored In females galactosemia results on delayed puberty. |
|
|
What is non-classical galactosemia?
|
Is the deficiency of galactokinase. This results in accumulation of galactose but no toxic metabolites (galactose 1-P) like classical.
Manifestation are less severe and main symptom is cataract formation (from galactitol) Urine will be positive for reducing sugar. |
|
|
How does lactose synthesis occur?
|

It takes place in the lactating mammary gland during lactation.
α-lactalbumin (protein B) synthesis is stimulated by prolactin (secreted during lactation) to form lactase synthase - used to make lacate from galactose and glucose. |

