![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
25 Cards in this Set
- Front
- Back
|
Cellulitis
|

destructive infective condition confined to the skin
loss of outer skin layers (destructive process) - behaves like amojor burn - sharp demarkating edge |
|
|
2ndary Cellulits
|

bugs that cause this
- olecranonoe bursitiis - secondary infection into the skin and then get a true cellulitis |
|
|
erysipelas
|
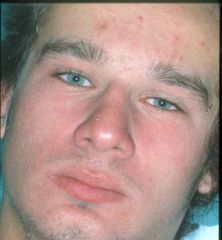
basically celluiltus in the face
|
|
|
Recognising the diagnosis
|
Limited to skin
True infection of dermis Skin oedema Painful Sharply demarcated from normal skin May be associated with a nidus of infection esp non-streptococcal cellulitis Spread via normal routes Direct/ contiguous structures (Venous and) esp lymphatic channels |
|
|
Culprit pathogens
|
S pyogenes
Able to dissect tissue planes(elastase/ hyaluronidase) (Aeromonas hydrophila; Vibrio vulnificans) (clostridia) S aureus Not v good at rapid spread (more pyogenic) The most common pathogen on the skin |
|
|
DDx Pathogens
|
dominant gram +ve pathogens:
Staph aurea Staph Epidermis Strep: tend to be able to discete skin layers S.pneumonia; can cause lobar pneumonia (stops at the anatomical boundary, because it disects the areas) S.pyogenes; same mech. and so it can spread through skin and local S.aureas is necortising and causes boils, and necortising stuff... |
|
|
Aggressive Cellulitis
|

aggressive fascitis
- Strep. Pyogens infection spreading along the tissue planes and necrosis and bleeing resulting - spreading fascitis (below the fat layer and so the inflammatory process picks off the small BV throughout the skin and thus mixed infection it creates an aneraobic envirnoemtn and so other microbes thrive in it (synergistic gangreen) CATASTROPHIC MEDICAL EMERGENCY: fatal outcome. - need to debulk all the infective areas and use penicillin - castrophic skin loss, and can masively mutliply - can spread really quick |
|
|
strep. toxic shock
|
- boggy underneath the skin adn the skin on top is stip red and good
- then need immunoglobuin in early |
|
|
Opportunists
|
Water (Aeromonas, Vibrio) – consider carbapenems/quinolones
Aeromonas hydrophila: ciproflox/ TMP-SMX/ carbapenem Vibrio vulnificus: doxi + ceftriaxone/ (quinolones)/ carbapenem Bites – consider Augmentin Human: Augmentin/ TZP/ (clindamycin + cipro if PNC allergic) Dog (5% get infected): (Pasteurella)/ Stpah/ bacteroides Augmentin/ (clinda/ quinolones) Cat (80% get infected): Pasteurella/ Staph: Augmentin/ PNC/ quinolones (diclox/ceph 1 no good for P multocida) Abscess/ therapeutic devices Wounds/ ulcers (Staph and Gram negs eg Pseudomomas) Penetrating injuries and/or ischaemia (staph/ clostridia) |
|
|
soil (gut contents from herbivores)
which bug? |
Clostridia
|
|
|
moist envirnoments (eg from shoes, flower pots... so eg pentrating injury from shoe)
|
P.ariginousa
|
|

|
skin loss
- skin infection (meets criteria for localised cellulitis) - sharp demarcation - medial edge of the thigh signs of oedema, and red flare is diffuse - thus the top wound is the pentration point of the femoral aa. of a catherter the second wound is from cellulits - BUT REALLY under hear is a large infected haemotoma and not just a trivial cellulits so the oedema and the diffuse distal part of the redness gives this away |
|
|
Diabetic foot
|
Host context
Immune compromise Neuropathy: predisposition to injury Wound or ulcer-related Usual suspects: S. aureus>S pyogenes Gram negatives P aeruginosa “wet place” bugs - enterics Ischaemic element anaerobes |
|

|
sharp edge
- probably gram +ve bag of exudate - and discharge - tinea that has been super-infected with Stap. Aureus (capable of causing some cellulitis..) |
|
|
Diabetic foot assessment
|
Typically ball of foot (pressure necrosis
and/ or unrecognised direct injury) Neuropathy (vibration sense/ pinprick) Vasculopathy Microvasculature: capillary return <2 sec Macrovasculature: post tibial/ dorsalis pedis |
|
|
Home IV Therapy for Cellulitis
|
clinically stable with cellulitis severe enough to warrant IV therapy.
Patients requiring IV therapy include those: Unsuitable for oral Rx (severe illness or GI problems). with hypotension, or vital signs suggesting septicaemia. with rapidly progressing or extensive cellulitis. progression despite oral Rx nb may represent evolution of inflammation rather than Rx failure Patients requiring hospital admission because immobile Patients consent to home therapy and meet eligibility criteria Region/ number of visits/ suitable drugs IV access Home support |
|
|
Before Hospitial Discharge with HOME IV
|
before hospital discharge
first dose of IV antibiotic administered in hospital. medication chart and supply of the IV antibiotic. script for oral antibiotics for continuing therapy. script for analgesia as needed. Follow up arrangements. Letter to GP. |
|
|
Management of cellulitis
|
Baseline FBC, EUC, LFT, blood glucose.
blood culture if > 38o C or vital signs abnormal. swab skin defect, ulcer or bullae, for culture. border of the cellulitis should be marked at beginning of therapy. rest and elevate cellulitis of the foot/leg. saline dressings for weeping areas. analgesia as needed. IV 72 hours or until the patient afebrile and cellulitis stable (no progression for 24 hours) |
|
|
Inpatient therapy
|
Extremities
S. pyogenes>>S aureus PNC/ CTX Cephazolin (better S. aureus cover) Consider S aureus: clinda/ vanc Facial (erysipelas) cellulitis S. pyogenes>S aureus Clindamycin/ PNC Vancomycin/ daptomycin/ linezolid |
|
|
Home IV Drugs
|
Cephazolin 2g twice daily in hospital.
Cefazolin 2g once daily with oral probenecid 1.0 grams daily for home therapy. (probenecis delays renal Cl of the drug BUT not as good as bd dosing) Di/flucloaxacillin (and penicillin) are less suitable for home IV therapy dosage schedules. Allergy: mild delayed rash after PNC = Cephazolin. Immediate/severe = vancomycin. |
|
|
Avoiding catastrophe
|
Misdiagnosis of the rash
Eg meningococcus/ toxic shock Failure to debride adequately Failure to recognise extension Eg Necrotising fasciitis/ gangrene Failure to recognise ischaemia Pressure (eg hand/ lat compartment syndrome) Underlying vascular disease |
|

|
tissue infection (mairne)
vibrio inocculation rare but aggressive - extensive necrosis and bleeding |
|
|
Gas Gangrene (Clostridium perfringens)
|

clostridial infection cant hatch spores in viable tissue thus needs really low redox (thus need anerobic infection; crush wounds or vascualr wounds)
|
|

|
schoulding leg syndrome
- superantigen mediated: bypass the MHC and stuff, thus activate 10% of lymphocytes and causes toxic shock syndrome - and leave u with schaulded skin syndrome and causes desmosomal split in the skin - followed by a skock syndrome - this was all due to contamiated tampons (the ladies then died of toxic shock) |
|

|
petichial rash (wont blanch under ingers)
meningoccocal sepesis - can cause patches of skin necrosis - infant can lose limbs |

