![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
250 Cards in this Set
- Front
- Back

|
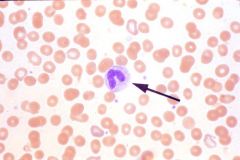
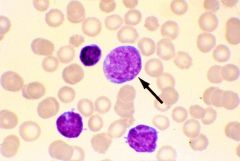
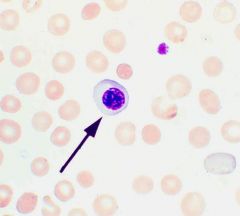
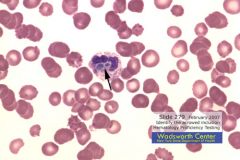
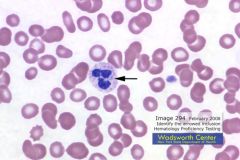
Plasma Cell. Plasma cells have an eccentric nucleus with coarse chromatin, which is often arranged in a cart-wheel-like pattern. The cytoplasm is abundant and is pale blue-gray to deeply basophilic. There is often an area of paranuclear clearing or “hof”. Plasma cells are rarely seen in normal blood films. However, they may be found in the peripheral blood in bacterial, viral or protozoal infections, chronic liver disease, autoimmune and collagen vascular disorders, various malignancies – particularly in multiple myeloma, and hypersensitivity reactions.
|
|
|
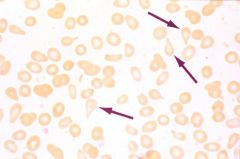
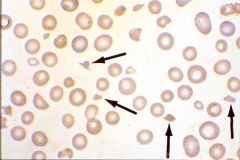
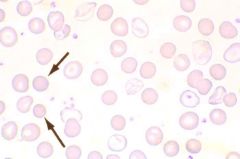
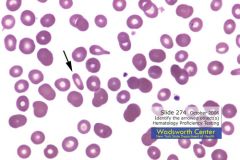
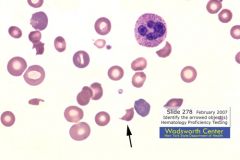
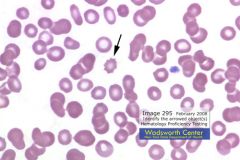
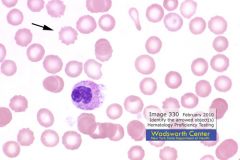
Tear Drop Cells or Dacryocytes. They are most commonly associated with an abnormal spleen or bone marrow, where the erythrocytes must stretch in order to move through the circulation. These cells are most often found in cases of myelofibrosis, pernicious anemia, thalassemia, myeloid metaplasia, and some hemolytic anemias. Teardrop cells may also be artifactual due to an improperly made smear. It is usually obvious since there are many teardrops with their tails lined up, pointing in the same direction.
|
|
|
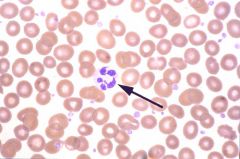
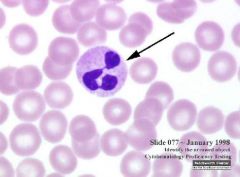
Hypersegmented Neutrophil. More than five lobes in more than 5% of neutrophils is one of the first signs of pernicious anemia.
|
|
|
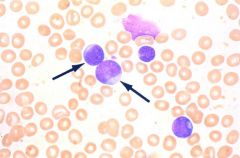
Myeloblast. 15-20 um. Small amount of dark blue cytoplasm, usually without granules. Nucleus has delicate chromatin with nucleoli. Blast cell not identified can be an acceptable answer until further testing.
|
|
|
Band Neutrophil. In granulocytic maturation, a cell is considered a band when nuclear indentation is more than half.
|
|
|
Blast Cell.
|
|
|
Giant Platelet.
|
|
|
Schistocyte. RBC Fragments, helmets, triangular cells. Seen with disseminated intravascular coagulation (DIC), hemolysis, artificial heart valves, burns, microangiopathic hemolytic anemia.
|
|
|
Target Cells or Codocytes. Seen in hemoglobinopathies, thalessemia, alcholism, post-splenectomy. May be an artifact if observed in only one part of a smear.
|
|
|
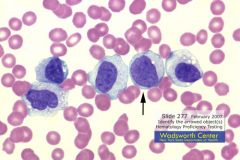
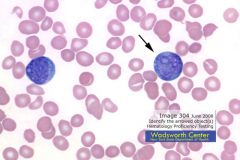
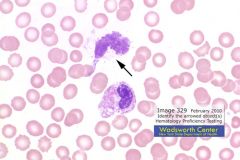
Atypical or Reactive Lymphocytes. One or more of the following: large size, elongated or indented nucleus, immature chromatin, increased parachromatin, nucleoli, increased cytoplasm, dark blue or very pale cytoplasm, peripheral basophilia, scalloped edges due to cytoplasm being indented by adjacent RBCs, frothy appearance, many azurophilic granules. Seen in viral infections like infectious mononucleosis, CMV.
|
|
|
Target Cells or Codocytes. Seen in hemoglobinopathies, thalessemia, alcholism, post-splenectomy. May be an artifact if observed in only one part of a smear.
|
|
|
Metamyelocyte.
|
|
|
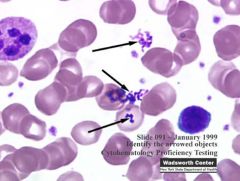
Platelet satellitosis.
|
|
|
Spherocytes. Small, dark-staining RBCs without central pallor. Often as a result of damaged RBC membrane via hereditary spherocytosis, autoantibodies, burns, hemoglobinopathies, hemolysis, ABO hemolytic disease of the newborn, incompatible blood transfusion, transfusion of stored blood. A few are normal due to aging of RBCs.
|
|
|
Smudge/Basket Cell.
|
|

|
Basophil. 10-14 um. Nucleus is usually difficult to see because of overlying granules, which are dark purple. Relative Adult Count (Ref Range): 0-1%; Absolute Adult Ref Range: 0-0.1x10^9/L
|
|
|
Band neutrophil with toxic granulation and Dohle bodies. Döhle bodies represent denatured aggregates of free ribosomes or rough endoplasmic reticulum containing RNA. They are found in infections, poisoning, burns, and following chemotherapy.
|
|
|
Elliptocytes/Ovalcytes. Seen in hereditary ovalocytosis or various anemias.
|
|
|
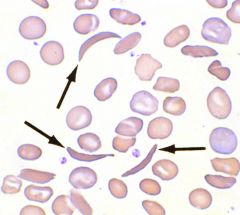
Sickle cells or drepanocytes. Sickle-cell anemia.
|
|
|
Nucleated RBC.
|
|

|
Eosinophil. 12-16 um. Nucleus: Band-shaped or segmented into two lobes. Cytoplasm: Large, red granules. Adult Reference Range (Relative): 1-3%; Adult Reference Range (Absolute): 0.05-0.30x10^9/L.
|
|

|
Monocyte.
|
|

|
Platelet.
|
|

|
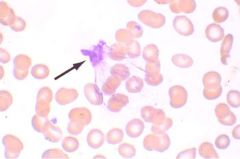
Parasite.
|
|

|
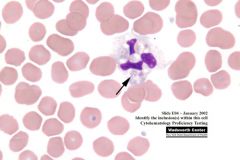
Auer Rods within a Myeoblast. Auer rods are red or purplish needles in the cytoplasm of leukemic myeloblasts and monoblasts. They are indicative of nonlymphocytic leukemia.
|
|

|
Pelger-Huet. Anomaly in which most neutrophils have round or bilobed nuclei. Inherited disorder with no clinical effect. May be misinterpreted as a shift to the left.
|
|
|
Monocyte.
|
|
|
Yeast.
|
|

|
Bacteria.
|
|
|
Hairy Cells. Leukemic reticuloendotheliosis, or hairy cell leukemia, is a rare malignant disorder accounting for 2% all leukemias. Hairy cells are thought to be of lymphocytic origin and show characteristics of B-lymphocytes. Hairy cells have reniform to oval nuclei with finely granular chromatin and delicate grey cytoplasm with projections (filipodia), which give the cells their "hairy" appearance.
|
|
|
Hypersegmented Neutrophil.
|
|
|
Giant Platelet.
|
|

|
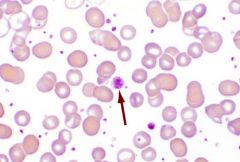
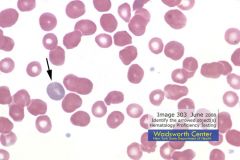
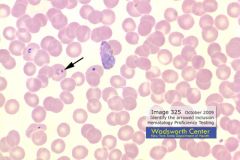
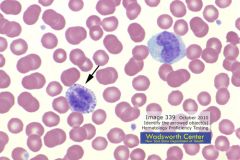
Howell-Jolly Bodies. Round, purple 1-2 um in diameter. Usually only one per cell. Nuclear remnants (DNA) and seen in accelerated/abnormal erythropoiesis. Seen in postsplenectomy, thalassemia, hemolytic/megaloblastic anemias, sickle cell anemia. Wright's and new methylene blue stain.
|
|
|
Atypical Lymphocytes.
|
|
|
Smudge (Basket) Cell.
|
|
|
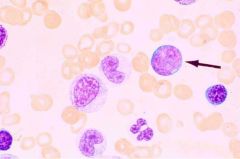
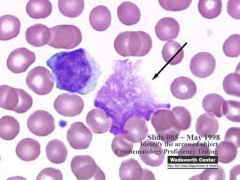
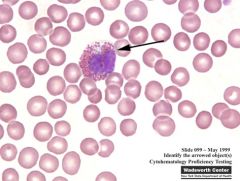
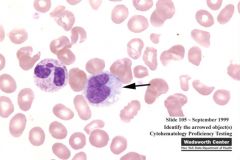
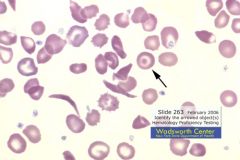
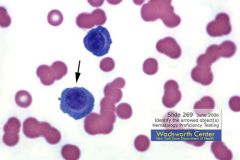
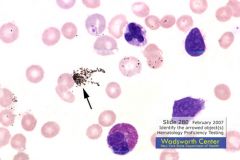
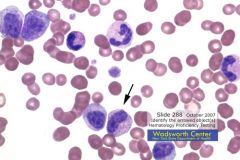
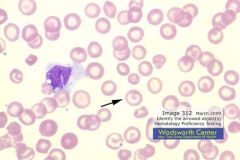
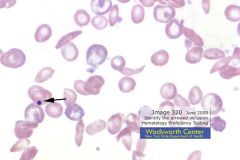
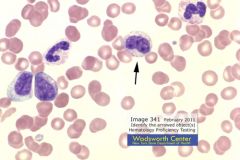
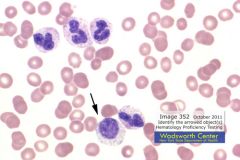
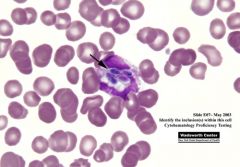
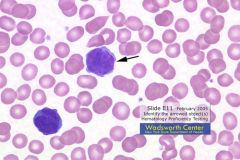
The cell indicated by the arrow is a myeloblast. The myeloblast is the first stage of the granulocytic series that is identifiable by light microscopy. Two to five distinct nucleoli are usually present. One prominent nucleolus is present on this photographic transparency. The nucleus is slightly indented and the cytoplasm is scant and basophilic. The nucleus is composed of very fine non-aggregated chromatin that stains light blue to reddish-purple with Wright's stain. The nucleus is often bordered at one side by a distinct light perinuclear zone. A slight perinuclear halo is present on this photographic transparency. A myeloblast can be distinguished from a promyelocyte by its lack of cytoplasmic granulation. It may be difficult to distinguish myeloblasts from other blasts in the peripheral blood unless one uses special stains or infers their identity from the presence of other immature cells of the same line. Since there are no Auer rods present and no cytochemical data given, the response of blast not otherwise specified was an acceptable response.
|
|

|
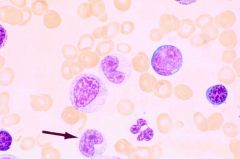
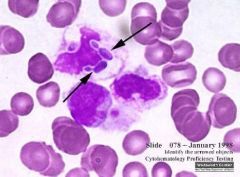
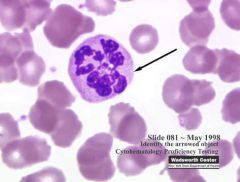
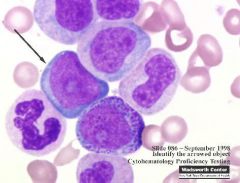
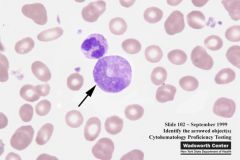
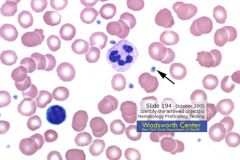
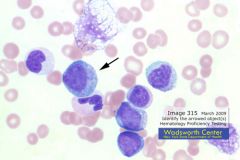
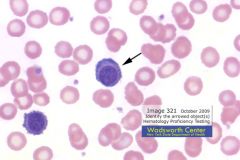
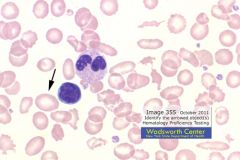
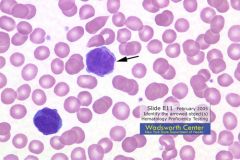
This cell is a promyelocyte. The cell size, 12 to 20 µm, is the same as that of a myeloblast. A nucleolus is still visible. Promyelocytes are the second stage in the granulocytic series. The large, reddish-purple granules that characterize promyelocytes are nonspecific in that they are shared by the other granulocytes (eosinophils and basophils). These granules are peroxidase positive, and a lipid component reacts with Sudan black stain, providing a second cytochemical reaction for the identification of large mononuclear cells in blood and bone marrow smears. The nucleus to cytoplasm ratio is less, usually from 3:1 to 2:1. The chromatin is still fine, but some aggregation is evident. Seven laboratories (1.5%) called this cell a myelocyte. Myelocytes are usually smaller than promyelocytes and their nucleus to cytoplasm ratio decreases to 1:1. The nucleus may be round to oval with a flattened side. The nuclear chromatin shows clumping, and nucleoli are usually no longer visible.
|
|

|
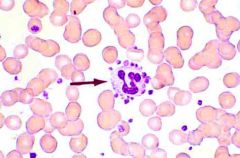
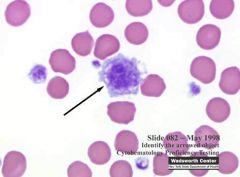
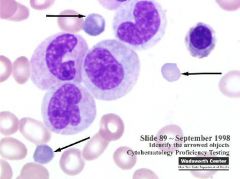
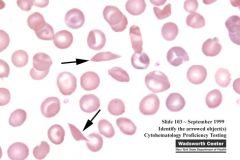
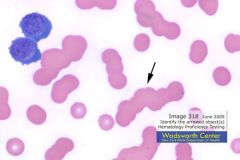
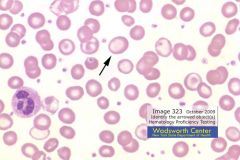
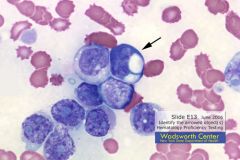
Metamyelocyte. The major morphological change between a metamyelocyte and a band neutrophil involves nuclear shape, and considerable debate exists as to the criteria for assigning neutrophils to metamyelocyte, band and segmented neutrophil. A band can be defined as a cell whose nucleus has indented to a point between uniform thickness and one half of the thickness of the arms of the 'U'. The indentation must have proceeded to at least the center of the nucleus or the cell would be classified as a metamyelocyte. Metamyelocytes have a cell diameter from 10 to 18 µm, and the nucleus to cytoplasm ratio is 1:1. Indentation of the nucleus begins at this stage, forming an outline that varies from slightly kidney shaped, to that of a broad V shape.
|
|
|
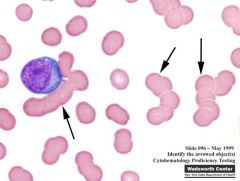
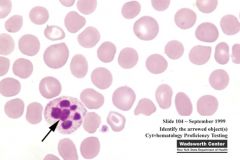
Polychromatiphilic RBCs. Bluish-gray color. Young RBCs. Reticulocytes with supravital stain. Sign of active erythropoiesis. 1-2% in normal adult. Increased with acute blood loss, hemolytic anemia and following treatment for iron deficient/pernicious anemia.
|
|
|
Basophilic Stippling. RBC Inclusion. Multiple, irregular purple inclusions evenly distributed throughout the cell. Result of an aggregation of RNA (ribosomes.) Coarse: Exposure to lead. Fine: Young RBC. May be seen in accelerated or abnormal hemoglobin synthesis or thalassemia. Wright's and new methylene blue stain.
|
|
|
Stain Precipitate.
|
|

|
Parasite. (Babesia)
|
|

|
Smudge (Basket) Cell.
|
|
|
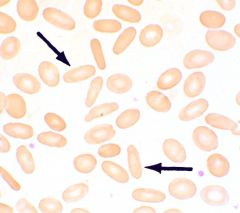
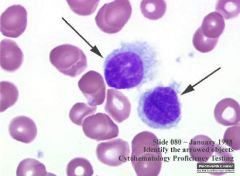
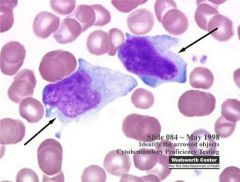
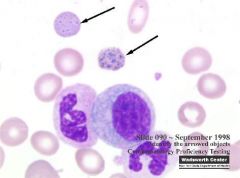
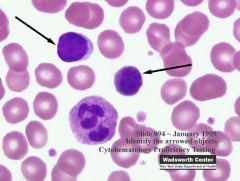
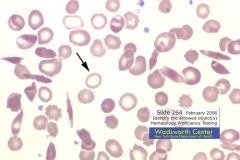
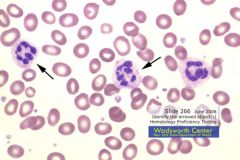
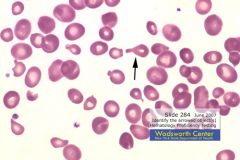
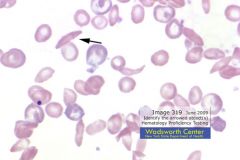
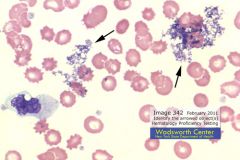
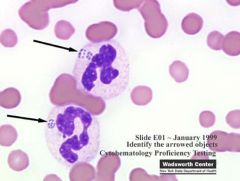
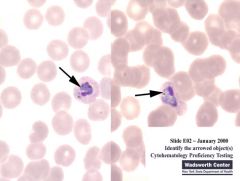
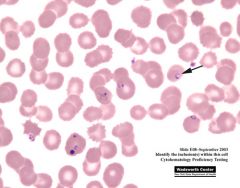
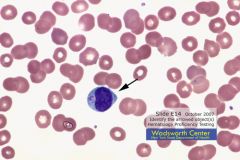
Lymphocytes. Both of the arrowed cells in this photograph are normal, small lymphocytes. They are approximately the same size as the red blood cells within the same field. The nucleus is round and the chromatin is dense and clumped. No nucleoli are visible. The cytoplasm forms a thin rim around the nucleus and is a moderate dark blue in color.
|
|

|
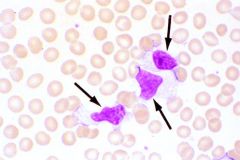
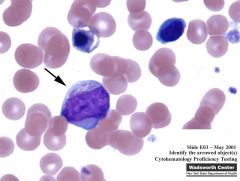
Plasma Cells. Plasma cells have an eccentric nucleus with coarse chromatin, which is often arranged in a cart-wheel-like pattern. The cytoplasm is abundant and is pale blue-gray to deeply basophilic. There is often an area of paranuclear clearing or “hof”. Plasma cells are rarely seen in normal blood films. However, they may be found in the peripheral blood in bacterial, viral or protozoal infections, chronic liver disease, autoimmune and collagen vascular disorders, various malignancies – particularly in multiple myeloma, and hypersensitivity reactions.
|
|
|
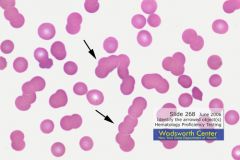
Rouleaux. RBCs resemble a stack of coins. Result of a serum protein abnormality; e.g., increased globulins or fibrinogen. Seen in multiple myeloma and macroglobulinemia. May be artifact due to delay in spreading drop of blood or smear that is too thick.
|
|
|
Acanthocytes. Shrunken cells with irregular, spiny projections. Result of damage to the RBC membrane, alcoholic cirrhosis, post-splenectomy, abetalipproteinemia. The mechanical damage to the red blood cells, caused by the formation of platelet thrombi in capillaries and arterioles throughout the body, is evident in the photograph. Acanthocytes are smaller than normal red cells. In contrast to echinocytes/ burr cells, acanthocytes have irregularly spaced projections, which are usually fewer in number, and lack a central pallor.
|
|

|
Target Cells. The formation of target cells in thalassemia usually results from an abnormal ratio of membrane to internal contents caused by decreased hemoglobin. Other morphologic signs of thalassemia in this slide include anisocytosis, microcytes and spherocytes.
|
|
|
Eosinophil. Circulating eosinophils are typically bilobed, although segmented forms having three lobes or more are occasionally seen. The characteristic bright color of eosinophilic granules makes these mature cells easy to identify on well-stained blood smears. The uniform, coarse nature of eosinophilic granules is characteristic and differs from the smaller, finer granules of neutrophilic cells or the unevenly distributed deep purple/black staining, irregularly shaped granules of basophils.
|
|

|
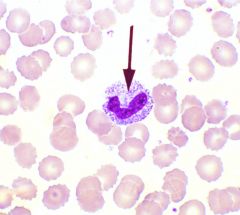
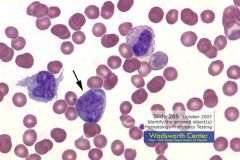
Monocyte. Prominent nuclear folding and indentation, as well as the presence of irregular cell outlines and numerous vacuoles are typical of a monocyte.
|
|

|
Nucleated RBC. The blue-purple nucleus displays pyknotic degeneration with condensed homogeneous chromatin.
|
|
|
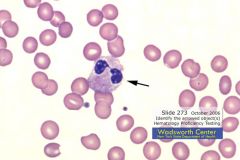
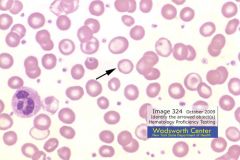
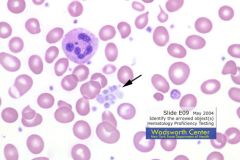
Metamyelocyte. While the nuclear:chromatin ratio is close, the nucleus is indented to less than half the nuclear width. The cytoplasm contains primary as well as specific granules. The cell is large in comparison to the adjacent segmented neutrophil.
|
|
|
Sickle Cell. The helmet cell form of schistocytes can appear similar to a sickle cell, also having pointed ends, but -unlike a sickle cell - does not usually elongate beyond the circumference of a normal sized red blood cell. The central diameter of a sickle cell is usually narrower than that of a schistocyte.
|
|
|
Hypersegmented Neutrophil.
|
|
|
Monocyte. 12-22 um. Nucleus: Round, horseshoe-shaped or lobulated; convoluted; loose strands of chromatin. Cytoplasm: Gray-blue with indistinct pink granules, vacuoles and occasional pseudopods. Adult Reference Range (Relative Count): 2-8%; Adult Reference Range (Absolute Count): 0.1-0.8 x 10^9/L
|
|

|
Parasite. Normochromic cells favor parasitic distinction over Cabot Rings, since Cabot Rings are seen in anemias with more disrupted cellular structures.
|
|

|
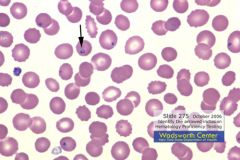
Normal Erythrocyte.
|
|

|
Auer Rod. Auer rods are rod-like bodies representing primary granules that stain a reddish purple. They are found in the cytoplasm of myeloblasts, monoblasts, and promyelocytes in acute monocytic or acute myelogenous leukemia.
|
|

|
Target Cells. The formation of target cells in thalassemia usually results from an abnormal ratio of membrane to internal contents caused by decreased hemoglobin. Other morphologic signs of thalassemia in this slide include anisocytosis, microcytes and spherocytes.
|
|

|
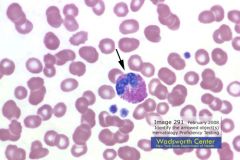
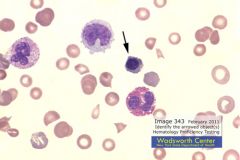
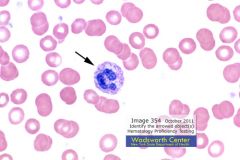
Atypical Lymphocyte. The nucleus is elongated and irregular, with mature coarse, red-purple nuclear chromatin. Abundant cytoplasm partially surrounds adjacent red cells, producing irregular borders, with darker staining margins.
|
|

|
Eosinophil.
|
|

|
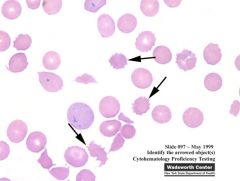
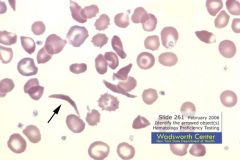
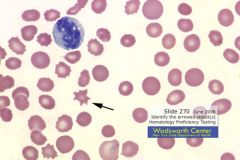
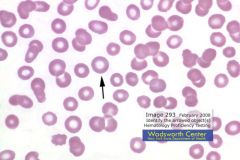
Tear Drop Cell or Dacrocyte. Teardrop cells should not be confused with oval macrocytes, ovalocytes, fragmented cells, or sickle cells. The tip is never short and pointed (an artifactual change), but rather elongated with a blunt or round tip. They are most commonly associated with an abnormal spleen or bone marrow, where the erythrocytes must stretch in order to move through the circulation. These cells are most often found in cases of myelofibrosis, pernicious anemia, thalassemia, myeloid metaplasia, and some hemolytic anemias. Teardrop cells may also be artifactual due to an improperly made smear. It is usually obvious since there are many teardrops with their tails lined up, pointing in the same direction.
|
|

|
Platelet.
|
|

|
Myeloblast. 15-20 um. Small amount of dark blue cytoplasm. Usually no granules. Nucleus has delicate chromatin with nucleoli. A myeloblast can be distinguished from a promyelocyte by its lack of cytoplasmic granulation. The nucleus is composed of very fine nonaggregated chromatin that stains light blue to reddish-purple with Wright's stain. Two to five distinct nucleoli are usually present. The nucleus is often bordered at one side by a distinct perinuclear zone. An Auer rod is evident in the myeloblast at approximately 8 o’clock. Auer rods are rod-like bodies found in 1- 10% of myeloblasts, monoblasts, and promyelocytes in approximately one third of acute myelogenous leukemia cases, as well as acute monocytic leukemia and erythroleukemia. Demonstration of one or several Auer rods is generally considered diagnostic of acute non-lymphocytic leukemia.
|
|

|
Elliptocyte/Ovalocyte. Oval or pencil-shaped RBCs. Observed in hereditary ovalocytosis and various anemias.
|
|

|
Plasma Cell.
|
|

|
Nucleated RBC.
|
|

|
Basophil.
|
|

|
Segmented Neutrophil.
|
|

|
Schistocyte.
|
|

|
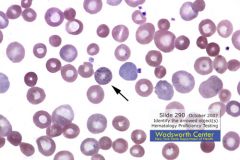
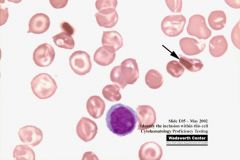
Howell-Jolly Body. Howell-Jolly bodies are round blue-black inclusions in red cells seen on Wright-stained smears. They are nuclear fragments of condensed DNA, normally removed by the spleen, but appearing in severe hemolytic anemias, in patients with dysfunctional spleen, or after splenectomy.
|
|

|
Spherocyte.
|
|

|
Segmented Neutrophil with Toxic Granulation.
|
|

|
Band Neutrophil.
|
|

|
Eosinophil.
|
|

|
Basophilic Stippling. Basophilic stippling appears as round, dark-blue granules in red blood cells on smears stained with supravital stains such as brilliant cresyl blue. They may be observed in lead poisoning, exposure to some drugs, severe burns, anemias, or septicemia. The granules are precipitated ribosomes and mitochondria.
|
|

|
Macrocytic RBC. RBCs greater than 9 um. Often seen in: Vitamin B12 Deficiency, Folic Acid Deficiency, Pernicious Anemia, Hemolytic Anemia, Cirrhosis, Alcoholism. Normal in newborns.
|
|

|
Giant Platelet.
|
|

|
Target Cell.
|
|

|
Metamyelocyte. A neutrophilic metamyelocye has a slightly indented nucleus and small, pinkish-blue granules. As a class, these cells are slightly smaller than myelocytes and have relatively smaller nuclei and less well defined chromatin stucture. Neutrophilic metamyelocytes are rarely seen in normal peripheral blood but are often found in conditions in which there is myelocytic hyperplasia. As the neutrophilic metamyelocyte matures, the nuclear indentation becomes more marked until a stage is reached in which the indentation is greater than half the width of the hypothetical round nucleus.
|
|

|
Promyelocyte. Promyelocytes are the second stage in the granulocytic series. A cell ceases to be a myeloblast and becomes a promyelocyte when it develops distinct granules. The nucleus is round or oval and relatively large in relation to the cytoplasm. The chromatin structure is slightly coarser, and the strands of chromatin are bluer and not as red as in the myeloblast. Nucleoli may be visible but are usually indistinct. The cytoplasmic margins are smooth, and the cell does not indent nor is it compressed by neighboring cells. Since some early granulocytes are still capable of reproduction, the size may be quite variable, depending on the stage of a given cell in the mitotic cycle. A promyelocyte becomes a myelocyte when the granules differentiate to such a degree that one can identify the granules as basophilic, eosinophilic, or neutrophilic.
|
|

|
Sickle Cell.
|
|

|
Platelet Satellitosis. Blood drawn in EDTA as anticoagulant sometimes undergoes a phenomenon known as platelet satellitosis. Platelets surround or adhere to the neutrophils and can produce an artificially low platelet count by automated instruments. The low count should prompt a review of the blood smear for platelet clumps and/or satellitosis.
|
|

|
Hairy Cell. On peripheral blood films, hairy cells are one to two times the size of small lymphocytes and have round, oval, or kidney-shaped nuclei. The chromatin patterns are stippled, and nuclei usually are single, small, and inconspicuous. The cytoplasm is moderate to abundant and pale blue and has poorly defined borders or projections.
|
|

|
Monocyte. The three most characteristic features of the monocyte, and the most helpful in diagnosis, are the dull gray-blue color of the cytoplasm, the blunt pseudopods, and the brain-like convolutions of the nucleus. (Note vacuolization.)
|
|

|
Eosinophil.
|
|

|
Cabot Ring. Reddish purple rings or figure eights. May be part of mitotic spindle, remnant of microtubules or fragment of nuclear membrane. Usually seen with rapid blood regeneration or abnormal erythropoiesis. Observed in pernicious anemia, thalassemia, post-splenectomy, and lead poisoning.
|
|

|
Blast Cell. (Lymphoblast.) The cell is large with a high nucleus to cytoplasm ratio. The cytoplasm is deeply basophilic without visible granules. The chromatin strands are thin, evenly stained and reddish purple. Two nucleoli are visible. A marked heterogeneity in the size of these early cell types is evident.
|
|

|
Nucleated RBC.
|
|

|
Dohle Bodies.
|
|

|
Band Neutrophil.
|
|

|
Echinocytes (Crenated) or Burr Cells.
|
|

|
Giant Platelet.
|
|

|
Polychromatophilic RBC. Polychromatophilia may be defined as increased numbers of immature peripheral red blood cells that have a blue-gray tint on Wright-stained smears, indicating the presence of cytoplasmic RNA. These polychromatophilic red blood cells are usually larger than normal. Many of these cells prove to be reticulocytes when stained with supravital stains such as brilliant cresyl blue. They appear under conditions of accelerated red cell production.
|
|

|
Spherocyte.
|
|

|
Segmented Neutrophil.
|
|

|
Basophil.
|
|

|
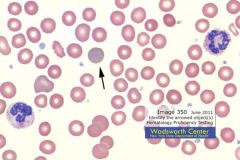
Lymphocyte. The lymphocyte is slightly larger than the surrounding red blood cells, with a round, compact, coarse chromatin and scant cytoplasm.
|
|

|
Sickle cell.
|
|

|
Acanthocyte.
|
|

|
Pelger-Huet.
|
|

|
Reactive or Atypical Lymphocyte.
|
|

|
Hypersegmented Neutrophil.
|
|

|
Plasma Cell. The round to ovoid nucleus is eccentrically located and a moderate to abundant amount of grey-blue cytoplasm is present. A key distinguishing feature of the plasma cell is a perinuclear zone as seen on this image. This zone represents the presence of a very active Golgi apparatus in the production of large amounts of immunoglobulins.
|
|

|
Target Cell.
|
|

|
Band Neutrophil.
|
|

|
Cabot Ring. Reddish purple rings or figure eights. May be part of mitotic spindle, remnant of microtubules or fragment of nuclear membrane. Usually seen with rapid blood regeneration or abnormal erythropoiesis. Observed in pernicious anemia, thalassemia, post-splenectomy, and lead poisoning.
|
|

|
Rouleaux.
|
|

|
Ovalocyte/Elliptocyte.
|
|

|
Howell-Jolly Body.
|
|

|
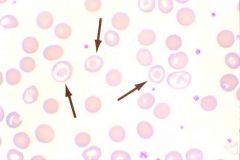
Hypochromic RBC. Central pallor greater than one-third cell diameter. Seen in iron-deficient anemia and thalassemia.
|
|

|
Metamyelocyte. Nucleus begins to indent.
|
|

|
Hairy Cell. Hairy cells can sometimes be confused with monocytes or promonocytes. Hairy cells are slightly smaller and contain less abundant cytoplasm. Monocytes and promonocytes contain frequent vacuoles and fine azurophilic granules with more irregular nuclear shapes.
|
|

|
Myeloblast.
|
|

|
Segmented Neutrophil.
|
|

|
Smudge or Basket Cell.
|
|

|
Basophilic Stippling.
|
|

|
Schistocyte.
|
|

|
Basophil.
|
|

|
Monocyte.
|
|

|
Tear Drop Cell.
|
|

|
Macrocyte.
|
|

|
Acanthocyte.
|
|

|
Stomatocyte. RBCs with a slit-like central pallor. Seen in hereditary stomatocytosis, hereditary spherocytosis, thalassemia, alcoholic cirrhosis, Rh null disease. May be an artifact in parts of the smear that are too thin or too thick.
|
|

|
Normal RBC.
|
|

|
Lymphoblast.
|
|

|
Myelocyte.
|
|

|
Spherocyte.
|
|

|
Echinocyte (Crenated) or Burr Cell.
|
|

|
Polychromatophilic RBC.
|
|

|
Blast Cell.
|
|

|
Giant Platelet. Most normal sized platelets are 1.5 to 3 µm in diameter. Large platelets are 4 to 7 µm. Giant platelets are larger than 7 µm and usually 10 to 20 µm. The term giant platelet is used when the platelet is larger than the size of the average red cell in the field, assuming a normal MCV. Giant platelets may be seen in Bernard-Soulier syndrome and in myeloproliferative disorders (chronic myelogenous leukemia (CML), polycythemia vera, essential (primary) thrombocythemia, and agnogenic myeloid metaplasia).
|
|

|
Myelocyte or Promyelocyte.
|
|

|
Normal Lymphocyte.
|
|

|
Eosinophil.
|
|

|
Blast Cell. (Most likely Prolymphoblast.)
|
|

|
Normal Lymphocyte.
|
|

|
Nucleated RBC.
|
|

|
Hairy Cell. Hairy cells can sometimes be confused with monocytes or promonocytes. Hairy cells are slightly smaller and contain less abundant cytoplasm. Monocytes and promonocytes contain frequent vacuoles and fine azurophilic granules with more irregular nuclear shapes.
|
|

|
Segmented Neutrophil with Toxic Granulation.
|
|

|
Auer Rods.
|
|
|
Platelet.
|
|

|
Bacteria.
|
|
|
Sickle cell.
|
|
|
Howell-Jolly Body.
|
|
|
Target Cell.
|
|
|
Hypochromic RBC.
|
|

|
Band Neutrophil.
|
|
|
Hypersegmented Neutrophil.
|
|

|
Dohle Body. Döhle bodies are associated with infection, trauma and burns. They are remnants of rough endoplasmic reticulum that appear smooth and oblong staining pale blue with Wright-Giemsa, most commonly found in the periphery of neutrophils. They can also occur in eosinophils, basophils, monocytes, and lymphocytes. Döhle bodies are also a prominent finding in May-Hegglin disorder. The May-Hegglin anomaly is a rare autosomal dominant disorder characterized by (1) large abnormal Döhle bodies in granulocytic cells including monocytes, (2) poorly granulated ‘giant' platelets, and (3) variable thrombocytopenia that may cause purpura.
|
|
|
Rouleaux.
|
|
|
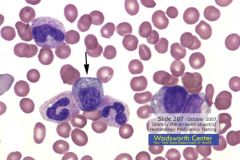
Plasma Cell. he distinctive plasma cell contains a round to ovoid eccentrically located nucleus with moderate to abundant grey-blue cytoplasm. A key distinguishing feature of the plasma cell is a perinuclear zone as seen on this image. This zone represents the presence of a very active Golgi apparatus involved in the production of large amounts of immunoglobulins.
|
|
|
Acanthocyte. Acanthocytes are dense red cells (lack central pallor) with irregular projections of the cell membrane formed as the result of alterations in the cell membrane lipid bilayer content often due to an increased cholestrol:lecithin ratio. Few acanthocytes are commonly observed in cases of post splenectomy although their presence in myeloproliferative disorders and neonates would not be unexpected.
Echinocytes differ from acanthocytes, as the spicules are shorter, blunter and evenly spaced over the entire cell surface |
|

|
Hairy Cell.
|
|

|
Lymphoblast.
|
|
|
Pelger-Huet Anomaly.
|
|
|
Ovalocyte/Elliptocyte.
|
|
|
Parasite.
|
|

|
Monocyte.
|
|
|
Blast Cell.
|
|
|
Schistocyte.
|
|
|
Fungus.
|
|
|
Stain Precipitate.
|
|

|
Basket or Smudge Cell.
|
|

|
Spherocyte.
|
|

|
Stomatocyte.
|
|
|
Tear Drop.
|
|

|
Lymphoma/Sezary Cell.
|
|
|
Blast Cell.
|
|
|
Myelocyte.
|
|
|
Atypical or Reactive Lymphocyte.
|
|

|
Normal RBC.
|
|
|
Basophilic Stippling.
|
|
|
Eosinophil.
|
|

|
Giant Platelet.
|
|
|
RBC. Could be ID'd as: Normal, Hypochromic or Macrocytic.
|
|
|
Dohle Body.
|
|
|
Echinocyte or Burr Cell. (Crenated.)
|
|

|
Band Neutrophil.
|
|

|
Segmented Neutrophil with Toxic Granulation.
|
|
|
Polychromatophilic RBC.
|
|
|
Blast Cell.
|
|

|
Normal Lymphocyte.
|
|

|
Blast Cell.
|
|

|
Nucleated RBC.
|
|

|
Basophil.
|
|

|
Plasma Cell. he distinctive plasma cell contains a round to ovoid eccentrically located nucleus with moderate to abundant grey-blue cytoplasm. A key distinguishing feature of the plasma cell is a perinuclear zone as seen on this image. This zone represents the presence of a very active Golgi apparatus involved in the production of large amounts of immunoglobulins.
|
|

|
Platelet.
|
|

|
Acanthocyte. The thorn-like cell membrane projections and no visible central pallor favor ID as an acanthocyte and a more uniform shape and distribution of the cell membrane projections favor the ID as an echinocyte. Acanthocyte is usually smaller than an RBC and echinocyte is usually the same size or slightly smaller, blunt projections and central pallor. Acanthocytes prevalent in abetalipoproteinemia and advanced liver disease and some myeloproliferative disorders and post-splenectomy. Echinocytes usually from improperly prepared smeans, rare causes (renal disease, E def, pyruvate kinase deficiency.)
|
|
|
Target Cell.
|
|

|
Auer Rod.
|
|

|
Bacteria.
|
|
|
Promyelocyte or Myelocyte. (May be transitioning.)
|
|

|
Hairy Cell.
|
|

|
Segmented Neutrophil.
|
|
|
Rouleaux.
|
|
|
Sickle Cell.
|
|
|
Howell-Jolly Body.
|
|
|
Plasma Cell. Mature plasma cells are often oval or fan shaped, measuring 8-15 µm. The nucleus to cytoplasm ratio is typically 2:1 to 1:1. The nucleus may be bilobed or multilobed, especially in patients with lymphoid blood dyscrasias. Nuclear chromatin is condensed and very patchy. The cytoplasm stains deep blue to gray blue, depending on the stain and the ribosomal content of the individual cell.
|
|

|
Hypersegmented Neutrophil.
|
|
|
RBC: Macrocytic, Hypochromic, and slightly Elliptocytic.
|
|
|
Hypochromic RBC.
|
|
|
Spherocyte.
|
|

|
Pelger-Huet.
|
|

|
Transitioning between a Metamyelocyte and Band Neutrophil.
|
|

|
Normal RBC.
|
|
|
Smudge or Basket Cell.
|
|
|
Echinocyte or Crenated (Burr) Cell.
|
|

|
Myeloblast.
|
|

|
Schistocyte.
|
|

|
Stomatocyte.
|
|

|
Monocyte.
|
|

|
Basophilic Stippling.
|
|

|
Spherocyte.
|
|

|
Platelet.
|
|

|
Atypical or Reactive Lymphocyte.
|
|
|
Basophil.
|
|

|
Eosinophil.
|
|
|
Echinocyte or Burr Cell. (Crenated.)
|
|
|
Stain Precipitate.
|
|
|
Nucleated RBC.
|
|

|
Tear Drop Cell.
|
|

|
Blast Cell. (Most likely a Monoblast.)
|
|

|
Giant Platelet.
|
|

|
Normal Lymphocyte.
|
|

|
Segmented Neutrophil.
|
|

|
Macrocytic RBC.
|
|
|
Polychromatophilic RBC.
|
|

|
Dohle Body.
|
|
|
Myelocyte.
|
|

|
Blast Cell.
|
|
|
Segmented/Band Neutrophil with Toxic Granulation.
|
|
|
RBC: Macrocytic, Hypochromic and Ovalocytic.
|
|
***
|
Bacteria. HGE Inclusions w/i Neutrophils.
|
|
***
|
Auer Rod.
|
|
***
|
Myeloblast/Auer Rods. (Multiple, stacked Auer Rods are known as ****** Cells.)
|
|
***
|
Phagocytized Platelet within Segmented Neutrophil.
|
|
***
|
Hemoglobic C Crystal. Blunt, six-sided, dark staining projection. "Bar of gold" or "Washington monument." Seen in Hemoglobin C disease.
|
|
***
|
Yeast.
|
|
***
|
Parasite. (Babesia.)
|
|
***
|
Platelet Clumping.
|
|
***
|
Cabot Ring. Cabot rings are red-purple staining threadlike filaments in the shape of a ring or figure 8 in the red blood cell, often in association with basophilic stippling. They may also appear as granules in a linear array rather than as complete rings. Cabot rings are thought to be microtubules from a mitotic spindle or remnants of the nuclear membrane. Cabot rings are seen in severe anemia including megaloblastic anemia, leukemia and lead poisoning. They are distinguished from the ring forms of Plasmodium by their larger size and by the absence of a red chromatin mass.
|
|
***
|
Lymphoma/Sezary Cells. Lymphoma/ Sézary cells are found in patients with mycosis fungoides, a cutaneous T cell lymphoma. Cutaneous T cell lymphomas are a group of mature T lymphoproliferative lesions that involve the skin. Sézary syndrome refers to the stage of the disease characterized by extensive skin involvement. It is a disease of older adults associated with clinical symptoms. The skin and lymph nodes involved in this syndrome are infiltrated with a mixture of small and large lymphoid cells. These cells are dark staining, contain folded or cerebriform nuclei and scant cytoplasm. Neoplastic infiltrates often involve other organs later in the course of the disease; once there is organ involvement the average survival is only several months.
|
|
***
|
Micromegakaryocyte.
|
|
***
|
Blast Cell with Vacuole.
|
|
|
Lymphocyte with Snapper-Schneid Granules.
|
|

|
Cell in Mitosis.
|
|

+++
|
Blister Cell. RBCs with one or more vacuoles. Seen in microangiopathic hemolytic anemia and pulmonary emboli in sickle cell anemia.
|
|

|
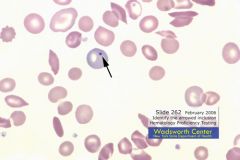
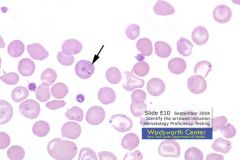
This case was not malaria and certain findings favor the identification of the inclusion as a Cabot ring. Namely, the presence of target cells, sickle cells,
polychromatophilic red cells, nucleated red cells, the lack of the diagnostic chromatin mass of a malarial parasite and the knowledge that most individuals with malaria inclusions are normochromic/ normocytic. |
|

|
Pappenheimer Bodies. Blue-purple inclusions, irregular in shape and located on the periphery. Formed as the result of red cell discharges its abnormal iron-containing mitochondria. Seen in sideroblastic anemias, post-splenectomy, thalassemia, sickle cell anemia and hemochromatosis. Wright's Stain.
|

