![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
37 Cards in this Set
- Front
- Back
|
T or F about Risk of Colon Cancer: Sporadic Cases> FAP Familiar Risks> Lynch Syndrome >Hamartomatous Polyposis |
False: Sporadic Cases> Familiar Risks> Lynch Syndrome> FAP >Hamartomatous Polyposis |
|
|
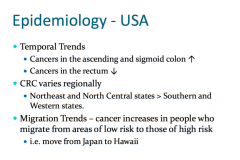
Colorectal Cancer:Temporal vs Migratory Trends |
|
|
|
Colorectal Cancer: Risk Factors |
- Age - IBD -Personal history of polyps - Hereditary Colorectal Cancer syndromes - Prior abdominal radiation - AfricanAmerican >Caucasian - Men > Women - Acromegaly - Patients on immunosuppression (renal transplant its) - Obesity - Diabetics - Alcohol - Cigarette smoking - Cholecystectomy (right sided colon cancers) - red meat |
|
|
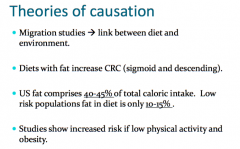
Colorectal Cancer: Theory of Causation |
|
|
|
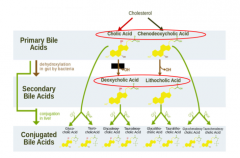
Colorectal Cancer: Primary, Secondary, ad Conjugated Bile Acids |
|
|
|
Colorectal Cancer: Bile acid Effect on Arachidonic Acid |
bile acids stimulate this process (increase PGEs, TXAs) As a resutlt these increase angiogenesis (tumor has more BV) and decease apoptosis and increase cellular proliferation NSAIDS and Aspirin can block this pathway, high dose NSAIDS may be a tx |
|
|
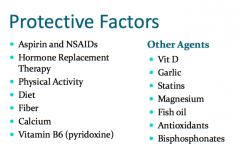
Colorectal Cancer: Protective Factors |
|
|
|
Colorectal Cancer: Possible Protective Mechanisms |
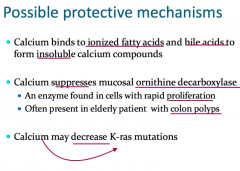
High fiber diet: Dilutes carcinogens, Minimizes duration ofcontact with mucosa, and May decrease harmfulbacterial enzymes andare fermented by fecalflora to short chain fattyacids (lowers pH whichinhibits carcinogenesis). |
|
|
Colorectal Cancer: Symptoms and Location |
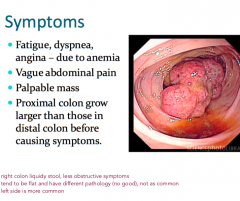
Symptom Prevalence by location: - Ascending colon (25%) - Transverse colon (15% ) -Descending (5% ) - Sigmoid colon (35%) - Rectum (20%) Right Colon – Anemia Left Colon – Rectal Bleeding |
|
|
Colorectal Cancer: Diagnostic Studies |
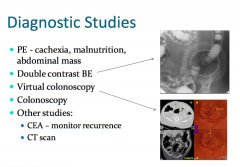
|
|
|
Colorectal Cancer: Colonoscopy |
Very Important in Screening and Prevention |
|
|
Colorectal Cancer: Biology |
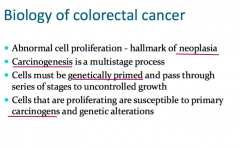
Abnormal Proliferation: stem cell can mutate (monoclonal mutation to a cancer cell) because of the properties of uncontrolled growth, becomes cancerous. |
|
|
Types of Polyps |
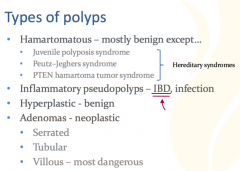
|
|
|
Colorectal Cancer Pathogenesis : Adenoma-Carcinoma Sequence |

|
|
|
Colorectal Cancer: Multistep Carcinogenesis |
1. Normal Epithelium 2. Hyper proliferative Epithelium (from loss of APC) 4. Early Adenoma 4. Intermediate Adenoma (from Activation of Kras) 5. Late Adenoma (From loss of 18q) 6. Carcinoma (from loss of p53) 7. Metastasis |
|
|
Molecular Genetics of Colorectal Cancer |
Alterations in genetic mechanisms may lead todisruption of the normal cell cycle and cellproliferation. - Germline mutations(e.g. familial polyposis) - Somatic mutations (environmental, diet, etc) Three major classes of genetic changesleading to CRC: - Alteration in oncogenes - Loss of tumor suppressor genes - Abnormal DNA mismatch repair |
|
|
Colorectal Cancer: Alteration in oncogenes |
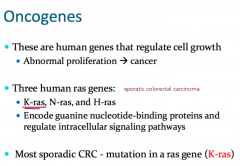
|
|
|
Colorectal Cancer: Loss of tumor suppressor gene ( affect cell adhesion) |
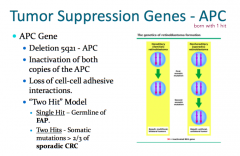
|
|
|
Colorectal Cancer: Loss of tumor suppressor gene (affect cell cycle) |
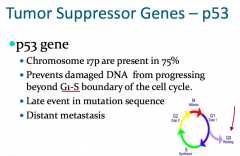
|
|
|
Colorectal Cancer: Loss of tumor suppressor gene (regulated cell adhesion) |
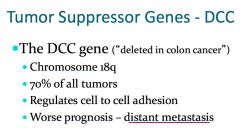
|
|
|
Colorectal Cancer: Loss of tumor suppressor gene (Abnormal DNA mismatch repair ) |
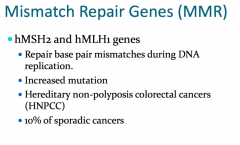
|
|
|
Genes altered in sporadic colorectal cancer |
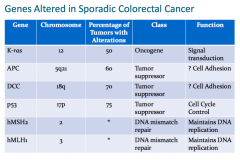
|
|
|
Major Hereditary Colon CancerSyndromes |
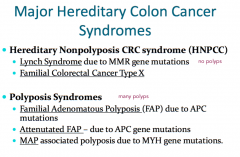
|
|
|
Clinical features of Lynch Syndrome |
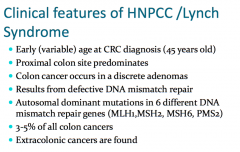
Commonly Mutinous and poor differentiated, Dx around 40s Often Proximal Hypermutable/ Replication aError Phenotype |
|
|
Lynch Syndrome: Lifetime Cancer Risks |
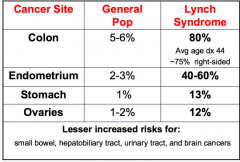
|
|
|
Amsterdam and Bethesda Criteria |
Amsterdam Criteria (3, 2, 1 rule) - at least 3 family members - cases must span 2 generations - one must be a first degree Bethesda Criteria: - < 50yo - HPNCC associated tumors - MSI-H Histology |
|
|
Microsatallite Instability (MSI) |
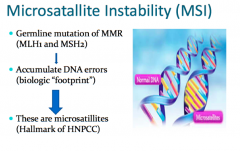
MSI – changes in sizes of repetitive stretches of DNAdue to insertion or deletion of repeated units. Mismatch repair genes (MLH1 and MSH2) ‐ germline >somatic. 90% of HNPCC/Lynch 15% of sporadic colon cancers |
|
|
Muir-Torre Syndrome |
Variant of Lynch Syndrome Associated with MSH2 or MLH1 Typical Features of HNPCC and: - Sebaceous gland tumors (cysts) - keratoacanthomas |
|
|
Recommendations for Individuals with lynch Syndrome |
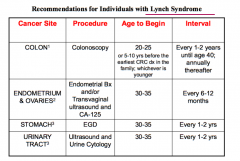
|
|
|
Familial Adenomatous Polyposis (FAP) |
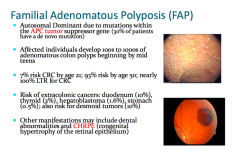
|
|
|
Familial Adenomatous Polyposis (FAP) Surveillance |
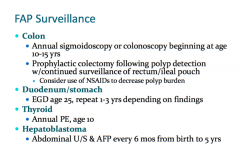
|
|
|
Gardner Syndrome |
A Variant of FAP Features of FAP and Extraintestinal lessons - demoed tumors - osteomas - supernumerary teeth - CHRPE - Soft tissue skin tumors |
|
|
Turcot Syndrome |
A Variant of FAP or Lynch Syndrome Rare hereditary syndrome of multiple colorectal adenomas and primary bring tumors 2 Distinct subtypes: - APC mutations associated with medulloblastoms - PMS2/MLH1 mutations associated with glioblastoma Genetic Testing may clarify diagnosis |
|
|
Peutz-Jeghers Syndrome |
- Autosomal Dominant - STK11 gene on chromosome 19 - GI hamartoma - Characteristic pigmentation - 93% overall cancer risk by age 65 years - cancers include colon, breast, pancreas, stomach, ovaries, and others |
|
|
Colon Cancer Pathology, Staging, and Prognosis |
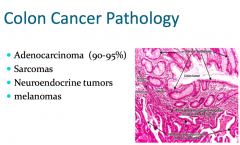
Duke Classification: ABDC (based on bowel wall penetration, LN, and metastasis)
TMN Classification: Stage 0 to 4 Prognosis- 5yr survival: 0 (100%) 1 (100-80%) 2 (30-70%) 3 (30-60%) 4 (3-30%) |
|
|
Hereditary Pancreatic Cancer Genes and Associated Conditions |
Genes: PRSS1, SPINK1 Associated Diseases: - HNPCC: Risk of PC is 3‐4% - Peutz‐Jeghers Syndrome: Risk of PC of 11‐36% - FAP: Risk unknown |
|
|
Hereditary Gastric Cancer |
Other hereditary syndromes have increased risk ofgastric cancer including:Col - HNPCC - FAP - Peutz‐Jegher |

