![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
45 Cards in this Set
- Front
- Back
|
Corynebacterium spp morphology |
-small, pleomorphic, gram + -in stained smears appear Chinese letter characters -relatively slow growth in lab media |
|
|
Differentiating factors of corynebacterium spp |
-most are catalase +, oxidase -, -non spore forming -pathogenic bacteria are non motile -cause pyogenic infections |
|

|
chinese letter characters of corynebacterium spp |
|
|
corynebacteriu spp pathogenesis and pathogenicity |
-opportunistic pathogens -pyrogenic organisms(with the exception of C. Bovis which can be isolated from teat canal of healthy cattle) |
|
|
C. presudotuberculosis can surviv and replicate in |
phagocytes |
|
|
virulence in C. presudotuberculosis is linked to |
-cell wall lipid and an exotoxin(phospholipase D(PLD)) and Corynebacteial secreted protease 40(CP40)
|
|
|
what may enhance survival and multiplication of corynebacterium spp |
PLD |
|
|
CP40 induces |
strong immune response which may provide protection |
|
|
What do C. pseudotuberculosis and C. ulcerans produce |
diphtheria-toxin which the presence of in milk may have public implications |
|
|
C.renale group are |
-urinary tract pathogens and produce urease -also posses fimbriae for attachment to urogenital mucosa |
|
|
Diagnositc procedures of Corynebacterium spp |
-animals species affected and clinical signs may suggest a specific infection -suitable specimens for the lab: pus, exudate, affected tissue, midstream urine -direct examination of gram stained smears may reveal corynebacteria -culture media: blood agar, McConkey and CNA incubated up to 5 days at 37C
|
|
|
Corynebacterium spp identifying diagnostic procedures |
-colonial characteristics - presence of hemolysis -absence of growth in McConkey, presences of growth in BAP and CNA -typical corynebacterium polymorphism on gram stain -biochemical tests |
|
|
Caseous lymphadenitis is |
a chronic suppurative condition of sheep, goat, and rarely cattle caused by C. pseudotuberculosis with organisms surviving in the environment for several months |
|
|
Caseous lymphadenitis transmission route |
-skin wounds, arthropod bites, or dips -ruptured abscesses -hematogenous spread causes abscesses in internal lymph nodes |
|
|
caseous lymphadenitis clinical signs |
-abscessation and enlargement of superficial and internal lymph nodes -goats usually develop superficial, subcutaneous abscesses usually in the head and neck -ill-thrift and pneumonia may be present -visceral form may not be detected antemortem |
|

|
caseous lymphadenitis |
|
|
incubation period of caseous lymphadenitis |
around 3 months |
|
|
Caseous lymphadenitis diagnosis |
-clinical (or postmortem) findings -smears from lesions by gram stain -isolation and identification of bacteria via submitted swabs to lab -serological diagnosis:ELISA (individual and flock screen) -interferon-gamma test as flock screen |
|
|
Caseous lymphadenitis: Tx |
susceptible to many antimicrobials but therapy is usually ineffective due to intracellular survival ability of bacteria and inability of drugs to penetrate into abscesses |
|
|
caseous lymphadenitis: control |
-import animals from countries/states/flocks free of caseous lymphadenitis -animals should be subjected to pre-importation screening tests such as ELISA -imported animals should be quarantines up to 3 months -infected animals should be slaughtered -contaminated buildings and equipment should be disinfected -vaccines available |
|
|
ulcerative lymphangitis is/caused by |
- slow and chronic either lymphangitis of lower limbs or abscessation of pectoral region(also called pigeon fever) -C. pseudotuberculosis in horses and rarely in cattle -prevalent in fall and early winter |
|
|
ulcerative lymphangitis is transmited by |
skin wounds, arthropod bites or contact of infected animals |
|

|
ulcerative lymphangitis |
|

|
ulcerative lymphangitis |
|
|
ulcerative lymphangitis clinical signs |
-lymphatic vessels swollen and firm with nodules forming along their length -edema develops in affected limbs and ulcerated nodules exude a thick odorless, greenish blood-tinged pus |
|
|
ulcerative lymphangitis diagnosis |
based on isolation and identification in the lab |
|
|
Tx and control of ulcerative lymphangitis |
-systemic antimicrobials may be combined with topical Tx - affected animals should be isolated and contaminated areas disinfected |
|
|
Bovine pyelonephritis causative agent |
C. renale- which may be isolated from healthy cattle vulva, vagina and prepuce
|
|
|
Bovine pyelonephritis acquired by |
stress of parturition and short urethra in cow may predispose to infection |
|
|
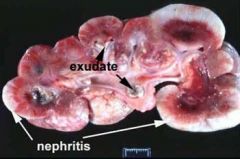
Bovine pyelonephritis -ascending infection from bladder to ureters can result in pyelonephritis with chronic infections possibly leading to extensive renal damage |
|
|
Bovine pyelonephritis: clinical signs |
-fever, anorexia and decreased milk production -restlessness and kicking in the abdomen may indicate renal pain -dysuria and blood tinged urine are present -clinical signs may suggest UTI -red blood cells and protein are present in the urine - thickened ureter and enlarged kidneys may be detected by renal palpation and or ultrasonography: unilateral -culture of C. renale frome urine is confirmatory |
|
|
Bovine pyelonephritis: Tx |
-antimicrobial tx based on susceptibility test, should start early for at least 3 weeks -penicillin is usually good choice for high excretion in urine |
|
|
Ulcerative balanoposthitis |
-caused by C. renale -characterized by ulceration around prepucial orifice with a brownish crust developing over the lesion -similar lesion may happen on the vulva of ewes -castrated sheep more prone -untreated cases may progress to total occlusion of preputial orifice |
|
|
C. renale may cause mucosal irritation and ulceration by |
hydrolyizing urea into ammonia |
|
|
predisposing factor of Ulverative balanoposthitis |
high urea level in the urine due to high protein intake |
|

|
ulcerative balanoposthitis |
|
|
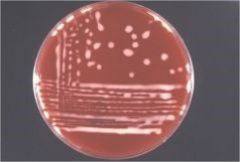
rhodococcus equi morphology |
-gram positive rods or cocci -salmon-pink, mucoid, non-hemolytic colonies -aerobic, non motile -CAMP test positive -major respiratory pathogen of foals |
|
|
Rhodococcus equi |
|
|
Rhodococcus equi- suppurative bronchopneumonia epidemiology |
-one of the most common causes of pneumonia in folas -generally acquired by inhalation of dust -may be present in high number in horse feces -environmental influences-dry weather, poorgrass coverage -high foal density -only young foals susceptible |
|
|
Rhodococcus equi- suppurative bronchopneumonia pathogenesis |
-ability to survive and multiply in macrophage -virulence is principally associated with a large??(not on slide) -encodes several proteins most important VapA -only equine isolates have VapA gene -capsular polysaccharides, mycolic acids and exoenzymes |
|
|
Rhodococcus equi- suppurative bronchopneumonia clinical signs |
-usually less than 4 weeks old foals -sudden onset of fever -anorexia -signs of bronchopneumonia -could be insidious in 2-4 month old foals -coughing, dyspnea, weight loss, exercise intolerance -loud, moist rales on auscultation |
|

|
Rhodococcus equi- suppurative bronchopneumonia |
|
|
Rhodococcus equi- suppurative bronchopneumonia: diagnosis |
-differentiating lower respiratory trac infections problematic -WBC, fibronegen, radiography, ultrasonography, -bacterial culture from tracheobronchial aspirate -salmon color mucoid colonies on BAP, CAMP test -PCR tests |
|
|
Rhodococcus equi- suppurative bronchopneumonia: Tx |
-combination of oral rifampin and a macrolide for up to 10 weeks -severely affected foals have poor prognosis -response to therapy monitored by radiography/ultrsonagrophy and plasma fibrinogen -supportive therapy: rehydration and bronchodilatotory agents or expectorants |
|
|
Rhodococcus equi- suppurative bronchopneumonia: control |
-vaccines not aailable -screening of foals twice a week clinical examination -prevention of dust ihalation -limit the foal density -limited time spent indoor -foaling at pasture may reduce the occurence -passive immunization-hyperimmune plasma -chemoprophylaxis-conflicting evidence and danger or resistance -development of active immunization highly needed(aka vaccine) |

