![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
90 Cards in this Set
- Front
- Back
|
What kind of heart failure is associated with primary abnormalities of contractility?
|
Cardiomyopathies: dilated, restricted, hypertrophic
|
|
|
What kind of heart failure is associated with secondary (d/t decompensation) abnormalities of contractility?
|
- Ischemic heart disease
- Valvular heart disease - Systemic HTN |
|
|
What causes cardiac remodeling?
|
- Diastolic wall stress
- Volume overload - Increased preload |
|
|
What are the effects of increased afterload on the heart?
|
- ↑ Systolic wall stress (have to push against increased afterload)
- LV hypertrophy and concentric remodeling (parallel sarcomeres) - Leads to diastolic heart failure (harder to fill chambers w/ hypertrophy) |
|
|
What are the effects of increased preload on the heart?
|
- ↑ Diastolic wall stress (more filling in same chamber)
- LV dilation and eccentric remodeling (sarcomeres in series) - Leads to systolic heart failure (harder to push out extra volume) |
|
|
What is the LaPlace's Law?
|
Wall Tension = (Pressure x Radius) / (2 * Wall Thickness)
|
|
|
How does a change in radius of a ventricular lumen affect wall tension?
|
↑ Wall Tension
Wall Tension = (Pressure x Radius) / (2 * Wall Thickness) |
|
|
How does a change in pressure in the ventricular lumen affect wall tension?
|
↑ Wall Tension
Wall Tension = (Pressure x Radius) / (2 * Wall Thickness) |
|
|
How does a change in wall thickness of a ventricle affect wall tension?
|
↓ Wall Tension
|
|
|
What is a way for the heart to compensate for increased wall tension?
|
Increase wall thickness / hypertrophy (decreases wall tension)
Wall Tension = (Pressure x Radius) / (2 * Wall Thickness) |
|
|
What are the possible cellular mechanisms of heart failure?
|
Abnormalities in:
- Myofilament protein - Calcium regulation - Mitochondria and metabolism - Cytoskeletal protein - Apoptosis - Nuclear membrane protein |
|
|
Abnormalities in what aspect of myofilament proteins can cause heart failure (non-ischemic cardiomyopathy)?
|
- Changes in activation or relaxation of sarcomere (Ca2+ sensitivity)
- Changes in cross-bridge kinetics - Changes in mechano-transduction (sensing and transmission) and passive stiffness |
|
|
Abnormalities in what aspect of calcium regulation can cause heart failure (non-ischemic cardiomyopathy)?
|
- Calcium influx
- E-coupling - Relaxation |
|
|
Abnormalities in what aspect of mitochondria and metabolism can cause heart failure (non-ischemic cardiomyopathy)?
|
- Metabolic substrate use
- O2/ATP ratio |
|
|
Abnormalities in what aspect of cytoskeletal proteins can cause heart failure (non-ischemic cardiomyopathy)?
|
Changes in mechano-transduction (sensing and passive stiffness)
|
|
|
Abnormalities in what aspect of apoptosis can cause heart failure (non-ischemic cardiomyopathy)?
|
Drop out of cardiac myocytes
|
|
|
Abnormalities in what aspect of nuclear membrane proteins can cause heart failure (non-ischemic cardiomyopathy)?
|
Uncoupling of mechano-transduction to transcriptional regulation
|
|
|
How are inherited mutations causing cardiomyopathies inherited? What kind of mutations?
|
- Autosomal dominant
- Commonly missense mutations - >400 mutations possible in 13 sarcomeric proteins (different mutations in same gene can cause different phenotypes) |
|
|
What are the three types of cardiomyopathy?
|
- Hypertrophic
- Dilated - Restrictive |
|
|
What is the leading cause of sudden cardiac death in young people in the US?
|
Hypertrophic Cardiomyopathy
|
|
|
How common is Hypertrophic Cardiomyopathy? Who is most likely to get it? How is it most commonly obtained?
|
- 1:500 individuals
- Men 2x more than women - SCD commonly in athletes - Most common cause of SCD in young people in US - Autosomal dominant in >50% of patients |
|
|
What is the most prevalent form of Cardiomyopathy?
|
Dilated Cardiomyopathy
|
|
|
How common is Dilated Cardiomyopathy? How is it most commonly obtained?
|
- 1:2500 individuals
- Most prevalent form of cardiomyopathy - Common clinical outcome of many prolonged cardiac insults |
|
|
What is the least prevalent form of Cardiomyopathy?
|
Restrictive Cardiomyopathy
|
|
|
What is the most lethal form of Cardiomyopathy?
|
Restrictive Cardiomyopathy
|
|
|
How common is Restrictive Cardiomyopathy? How is it most commonly obtained?
|
- Least common
- Causes extremely variable, includes induced and genetic initiators as well as idiopathic (in absence of other pathology) - Idiopathic may be associated w/ skeletal myopathies - Injury by radiation, scarring after heart surgery, infection, or diseases such as amyloidosis can also cause it |
|
|
If a young athlete suddenly dies of a sudden cardiac event, what should you suspect they have?
|
Hypertrophic Cardiomyopathy (autosomal dominant mutation in >50% of patients)
|
|
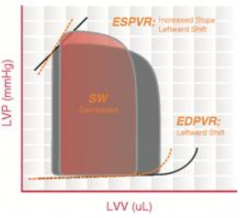
What cardiomyopathy is characterized by this pressure-volume loop?
|
Hypertrophic Cardiomyopathy
- Thickening of the ventricular muscle → ↓ chamber compliance and ↑ LV pressures - ↓ EDV and ↑ ESV → ↓ SV → ↓ CO Exceptions: - Healthy (athletes and healthy elderly) may have ↑ EDV and ↑ SV - Moderate hypertrophy allows for a ↓ HR, ↑ EDV, and thus ↑ SV |
|
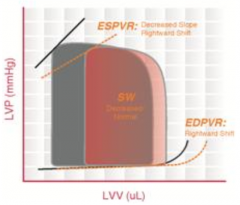
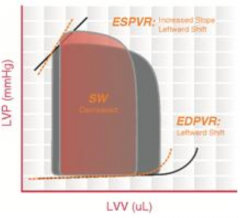
What cardiomyopathy is characterized by this pressure-volume loop?
|

Dilated Cardiomyopathy
- Dilated ventricle without compensatory thickening of the wall - LV unable to pump enough blood to meet metabolic demands - ↑ ESV and ↑ EDV; pressures remain relatively unchanged - ESPVR and EDPVR curves are shifted to the right - Not always a diminished ejection fraction |
|
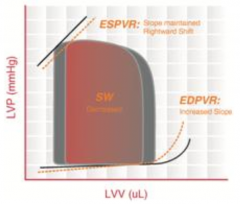
What cardiomyopathy is characterized by this pressure-volume loop?
|
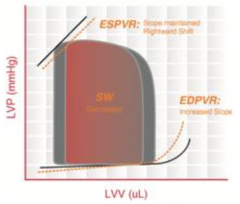
Restrictive Cardiomyopathy
- Walls of the ventricles become stiff (but not necessarily thickened) and resist normal filling - Occurs when heart muscle is gradually infiltrated or replaced by scar tissue or when abnormal substances accumulate in the heart muscle. - Ventricular systolic pressure remains normal - ↑ Diastolic pressure - ↓ SV → ↓ CO |
|
|
What are the consequences of LV remodeling?
|
- Move up on PV curve to higher volume at higher pressures, ↑EDV → ↑EDP → Pulmonary Edema
- ↑ Wall tension (LaPlace relationship) - Compensatory hypertrophy - ↑ O2 demand |
|
|
What are the main determinants of myocardial O2 demand?
|
- HR
- Ventricular wall tension |
|
|
What factors determine the ventricular wall tension?
|
- Pressure
- Wall thickness - Radius La Place Equation: Wall Tension = (Pressure x Radius) / (2 * Wall Thickness) |
|
|
Why does pressure increase ventricular wall tension? How does this affect O2 demand?
|
- ↑Pressure requires more force to contract ventricle
- ↑Contractility will ↑O2 demand La Place Equation: Wall Tension = (Pressure x Radius) / (2 * Wall Thickness) |
|
|
Why does wall thickness increase ventricular wall tension? How does this affect O2 demand?
|
- Total force is distributed across width of ventricle, thinner ventricle wall leads to greater force per unit of thickness (↑tension)
- Hypertrophy therefore will ↓tension - Thick walled ventricle will also have more muscle mass and will have ↑O2 demand La Place Equation: Wall Tension = (Pressure x Radius) / (2 * Wall Thickness) |
|
|
Why does radius increase ventricular wall tension? How does this affect O2 demand?
|
- As volume increases, the bigger the radius is
- There will be more work required to shrink it - ↑ Preload → ↑ Volume → ↑ Wall Tension → ↑O2 Demand |
|
|
How do cardiomyopathies compare to heart failure?
|
Cardiomyopathy:
- Structural heart disease w/ abnormality of myocardium Heart Failure: - Syndrome defined by constellation of signs and symptoms - Relaxation abnormality (diastolic dysfunction) or contractility abnormality (systolic dysfunction) - Involve LV or RV |
|
|
What are the possible etiologies of Dilated Cardiomyopathy?
|
- Alcohol
- Coxsackie B virus (and other enteroviruses - Pregnancy (late in gestation or up to several months postpartum) - Toxins (doxorubicin = chemo) - Idiopathic - Genetic: 20-50% of cases, primarily autosomal dominant |
|
|
What are the common genetic causes of Dilated Cardiomyopathy?
|
- 20-50% of cases
- Predominantly autosomal dominant: cytoskeletal proteins (eg, actin, desmin, nuclear lamins A and C) - X-linked: dystrophin - Mitochondrial: ox. phos. or FA β-ox |
|
|
What are the possible etiologies of Restrictive Cardiomyopathy?
|
- Amyloidosis
- Hematochromatosis |
|
|
What are the possible etiologies of Hypertrophic Cardiomyopathy?
|
Myosin gene mutation
|
|
|
Which Cardiomyopathy is associated with a virus? Which virus?
|
Dilated CM - Coxsackie Virus (and other Enteroviruses); may be able to detect nucleic acids in heart muscle
|
|
|
Which Cardiomyopathy is associated with amyloidosis or hematochromatosis?
|
Restrictive CM
|
|
|
Which Cardiomyopathy is associated with a myosin gene mutation?
|
Hypertrophic CM
|
|
|
Which Cardiomyopathy is associated with pregnancy?
|
Dilated CM - multifactorial (pregnancy assoc. HTN, volume overload, gestational diabetes, immunologic responses)
|
|
|
Which Cardiomyopathy is associated with alcohol?
|
Dilated CM - direct toxic effect on myocardium; also associated with thiamine deficiency (lends to beriberi heart disease)
|
|
|
What are the respiratory symptoms of heart failure?
|
- Dyspnea (at rest or w/ activity)
- Orthopnea (difficulty breathing w/o extra pillows) - Paroxysmal Nocturia Dyspnea (waking up at night w/ difficulty breathing) |
|
|
What are the non-respiratory symptoms of heart failure?
|
- Edema (lower extremity swelling)
- Anorexia (decreased appetite) |
|
|
What are the classifications of heart failure? How are they defined?
|
- I: no symptoms w/ ordinary activity
- II: symptoms w/ moderate exertion - III: marked limitation of activity but comfortable at rest - IV: symptoms at rest |
|
|
Which New York Heart Association classification of heart failure is associated with symptoms at rest?
|
Class IV
|
|
|
What are the signs of elevated LV filling pressures?
|
- Pulmonary Congestion
- Systemic Congestion |
|
|
What are the signs of pulmonary congestion seen with elevated LV filling pressures?
|
Signs:
- Rales (crackles) - Decreased breath sounds (d/t pleural effusion) Symptoms: - Orthopnea - Shortness of breath - Dyspnea on exertion - Decreased exertional tolerance |
|
|
What are the signs of systemic congestion seen with elevated LV filling pressures?
|
- Dependent edema
- Jugular venous distension - Hepatomegaly and splenomegaly - Ascites - Anorexia - Lethargy |
|
|
What are the effects of reduced stroke volume?
|
- Ventricular dilation (dilates ring/opening of AV valves)
- Reduced CO (causes fatigue, weakness, poor exertional tolerance) |
|
|
What are two outcomes of ventricular dilation d/t reduced stroke volume? Why?
|
Dilates annuli of AV valves:
- Mitral regurgitation - Tricuspid regurgitation Occurs because leaflets get pulled away from annulus, when they try to squeeze down, they can't contact how they used to, leads to regurgitation |
|
|
How does the body try to compensate for a decreased stroke volume?
|
Causes decreased renal perfusion, which leads to:
- ↑ Renin secretion - ↑ AngII and Aldosterone production - ↑ Na+ / H2O retention - ↑ Blood volume - ↑ Preload |
|
|
What happens to the PV curve when there is vasoconstriction?
|
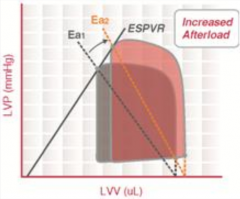
- Increased afterload and preload causes fluid retention in heart
- ↑Afterload → ↑ESV - ↑Preload → ↑EDV |
|
|
What happens when there is an increase in capillary pressure?
|
Net force tends to cause filtration of fluid into tissue space (edema)
|
|
|
What is the effect of diuretics on heart failure?
|
- ↓ Preload → ↓ SV → ↓ CO
|
|
|
What are the morphologic characteristics of hypertrophic cardiomyopathy? What is not a cause of this?
|
- LV hypertrophy
- Myocyte hypertrophy - Abnormal diastolic filling (restriction of ventricular filling) - Dynamic LV outflow obstruction (1/3 of cases) - Not caused by chronic pressure overload such as HTN or aortic stenosis |
|
|
What are the outcomes of the myocyte hypertrophy in Hypertrophic Cardiomyopathy?
|
- Myofibers in disarray → Ventricular arrhythmias → Syncope or Sudden Death
- LV Hypertrophy → Impaired relaxation → ↑LV EDP (increased preload) → Dyspnea - LV Hypertrophy → ↑MVO2 → Angina |
|
|
What are the outcomes of dynamic LV outflow obstruction in Hypertrophic Cardiomyopathy?
|
- ↑Systolic Pressure → ↑MVO2 → Angina
- Mitral regurgitation → Dyspnea - Failure to ↑CO w/ exertion → Syncope |
|
|
How should you treat Hypertrophic Cardiomyopathy depending on the symptoms?
|
If no symptoms: no tx
If heart failure symptoms: - Non-obstructive: try drug therapy → transplant - Obstructive: try drug therapy → septal reduction If high risk for sudden death: implantable cardioverter-defibrillator (ICD) |
|
|
What surgical procedure is sometimes used for Hypertrophic Cardiomyopathy? When?
|
If heart failure symptoms:
- Non-obstructive: transplant - Obstructive: septal reduction / myectomy (cut out obstructive part of septum) |
|
|
What are the causes of restrictive cardiomyopathy?
|
- Idiopathic
- Endomyocardial fibrosis (carcinoid syndrome or hyper-eosinophilic syndrome) - Infiltrative disorders (amyloidosis or sarcoidosis) - Rare metabolic disorders / storage disorders (Gaucher's dz, Mucopolysaccharidoses, Fabry's dz, Hemochromatosis) - Radiation |
|
|
What are the outcomes of the rigid myocardium in restrictive cardiomyopathy?
|
- ↑ Diastolic ventricular pressure → Venous congestion → Jugular vein distension, hepatomegaly and ascites, peripheral edema
- ↓ Ventricular filling → ↓ CO → Weakness and Fatigue |
|
|
What kind of CM is caused by sarcoidosis? How do you treat it?
|
- Restrictive cardiomyopathy
- Glucocorticoids |
|
|
What kind of CM is caused by Gaucher's disease or Mucopolysaccharidoses or Fabry's disease (storage diseases)? How do you treat it?
|
- Restrictive cardiomyopathy
- Enzyme replacement |
|
|
What kind of CM is caused by Hemachromatosis? How do you treat it?
|
- Restrictive cardiomyopathy
- Maintenance phlebotomy, chelation therapy |
|
|
What kind of CM is caused by radiation?
|
Restrictive cardiomyopathy
|
|
|
What kind of CM is caused by Hyper-eosinophilic Syndrome? How do you treat it?
|
- Restrictive cardiomyopathy
- Glucocorticoids, tyrosine kinase inhibitor (imatinib) |
|
|
What kind of CM is caused by Amyloidosis? How do you treat it?
|
- Restrictive cardiomyopathy
- Chemotherapy (melphalan) and bone marrow transplant |
|
|
What are some other cardiomyopathies that don't fit into the classical categories?
|
- Stress-induced CM / Takotsubo CM (broken heart syndrome - heart looks like octopus trap)
- LV Non-Compaction (altered myocardial wall d/t intrauterine arrest of compaction) - Cirrhotic CM (patients w/ cardiac dysfunction w/ cirrhosis independent of alcohol exposure) - Arrhythmogenic RV CM (ARVD) - risk for ventricular arrhythmias |
|
|
What kind of CM is associated w/ fibro-fatty replacement of the RV free wall? Why does this happen?
|
- Arrhythmogenic RV cardiomyopathy (ARVD)
- Familial sometimes (autosomal dominant d/t mutations in desmosomal junctional proteins) |
|
|
How do you diagnose a Cardiomyopathy?
|
Endomyocardial Biopsy
|
|
|
What are the morphological characteristics of Dilated CM?
|
- Cardiomegaly (2-3x bigger)
- Globular appearance - Four chamber dilatation, flabby walls - Mural thrombi - Valves normal but may have mitral or tricuspid regurgitation d/t dilation of chamber |
|
|
What are the histological characteristics of Dilated CM?
|
- Not specific for CDM (except for iron overload - stainable)
- Some fibers may appear stretched or irregular; no necrosis - Hypertrophy and fibrosis are ususal |
|
|
Case: 20-50 yo patient w/ SOB, easily fatigued, poor exertional capacity, low EF, global hypokinesia on echo.
Type of CM? Prognosis? Tx? |
- Dilated CM
- 50% die w/in 2 yrs, 25% survive longer than 5 years - Death d/t cardiac failure, arrhythmia, or thromboembolic complications - Tx: cardiac transplantation |
|
|
What are the morphological characteristics of Arrhythmogenic RV CM?
|
- Thin and dilated RV wall
** Fatty infiltration of RV wall (essential feature) - Interstitial fibrosis of RV wall |
|
|
Case: Young adult w/ arrhythmias (ventricular tachycardia) and sudden death. RV failure.
Type of CM? |
Arrhythmogenic RV Cardiomyopathy / Dysplasia
|
|
|
Which CM is associated with a banana shape subaortic region?
|
Hypertrophic CM - disproportionate thickening of setpum
|
|
|
What are the morphological characteristics of Hypertrophic CM?
|
- Massive myocardial hypertrophy (disproportionate thickening of septum, especially in subaortic region causing a "banana shape")
- No ventricular dilation (ventricle is compressed) - Atrium enlarged (d/t decreased ventricular compliance) - Endocardial thickening and mural plaques in outflow tract (d/t valve contacting septum during contraction) |
|
|
What are the histological characteristics of Hypertrophic CM?
|
- Marked hypertrophy (>40 µm, normal 15 µm)
- Interstitial fibrosis * Myofiber disarray |
|
|
What is the pathogenesis/causes of Hypertrophic CM?
|
- Mutations increase myofilament activation resulting in myocyte hyper-contractility
- Most are familial mutations in genes encoding sarcomeric proteins (>400 mutations) - Autosomal dominant w/ variable expression - Most commonly: β myosin heavy chain mutation → results in defects in direct sarcomere function or defect in transfer of energy to sarcomere |
|
|
Case: patient presents after puberty, may be asymptomatic, have exertional dyspnea (limited CO), syncope (LV outflow obstruction), sudden death in young athletes, atrial fibrillation w/ mural thrombus formation.
Type of CM? Tx? |
- Hypertrophic CM
- Tx: surgical excision, ventricular relaxing drugs |
|
|
What are the morphological characteristics of Restrictive CM?
|
- Normal ventricles (size, wall thickness)
- Bi-atrial dilation - Firm to rubbery myocardium and interstitial fibrosis |
|
|
What are the histological characteristics of Hypertrophic CM?
|
* Interstitial deposition of amyloid
- Patchy or diffuse interstitial fibrosis and disease specific changes - Birefringence under polarized light (congo red stain) - bright apple green spots = amyloid |
|
|
What is the most common amyloidosis of the heart? Cause? Common presentation?
|
Senile Cardiac Amyloidosis
- Cause: transthyretin (pre-albumin) deposits in ventricles and atria (gene mutation in 4%, autosomal dominant) - 60 yo, African-American:Caucasians (4:1) |
|
|
Case: CHF (R and L side), severe pulmonary congestion, hepatic congestion, similar s/s to constrictive pericarditis.
Type of CM? |
Restrictive CM
|
|
|
What are some rare causes of Restrictive CM?
|
- Endomyocardial fibrosis (tropical) - disease of children and young adults in Africa - fibrosis of ventricular endocardium and subendocardium → ↓volume and compliance → restrictive; mural thrombi
- Loeffler eosinophilic endomyocarditis |

