![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
15 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
what is the MOA, pharmacokinetics, side effects and toxicity of the loop diuretics
|
MOA-secreated into PCT then acts on the thick ascending loop to inhibit the Na, K, 2 Cl Co-transporter so these ions are excreated in the urine. ( AKA NKCC inhibitor) along with more water. Also increases renal blood flow ( by inducing synthesis of renal PG) this Also makes it a systemic venodilator esp when given IV. It is a high ceiling drug so as the dose increases the efficacy ( max effect) will increase more so than other low ceiling diuretics. They also have a high potency.
pharmacokinetics - rappid onset of action ( 10-20 mins when given IV or 1-1.5 hrs if oral). Well Ab orally and will last for 4-6 hrs. ( note according to the VMD furosemide is only in tablet form). side effects - dehydration esp in cats, pre renal azotaemia, disturbance of electrolites ( esp K, Na and Mg) , at Very high doses or when used with aminoglycosides it will cause ototoxicity ( ear). |
MOA- loation, inhibits transporter, also affects blood flow and if given IV does...... potency and efficacy
pharmacokinetics- onset and duration side effets - ear think of a loop around the ear!), cats, azotaemia, electrolytes. |
|
|
what do diuretics cause
|
1.INCREASED URINE FLOW (DIURESIS) 2.INCREASED Na+ EXCRETION (NATRIURESIS)
|
2 things
|
|
|
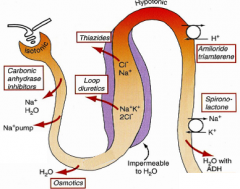
what are the classes of diuretics and which one is used most
|
.Loop diuretics ( furosemide is used the most)
.Thiazides K+-sparing Carbonic anhydrase inhibitors Osmotics (Xanthines, e.g. theophylline) - more as positive inotropes or bronchodilators |
|
|
|
describe how the dose of diuretic effects the efficacy in loop diuretics, low dose thiazides and K sparing diuretics
|
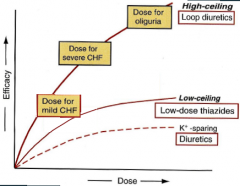
|
|
|
|
what is the MOA, pharmacokinetics, side effects and toxicity of the Thiazides
|
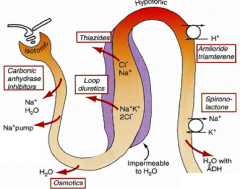
MOA- Again secreated into the PCT acting on the DCT to block Na and Cl reabsorption- ( AKA NC inhibitors) this causes loss of Na, Cl, K, Mg and acid. It depends on renal PG production because it is ineffective when renal blood flow is low. It is normally only used as an add on as its potency is only 1/3 of furosemides. slower onset and longer acting then furosemide.
pharmacokinetics - like the loop diuretics they are well Ab orally side effects -As for any diuretic -dehydration esp in cats, pre renal azotaemia, disturbance of electrolites ( esp K, Na and Mg) , Also Alkalosis and Insulin resistance. -usually at a lower does so dont see side effects- NOT LICENSED |
MOA-location, similar to loop diuretics, potency, onset and duration different though.
pharmaokinetics - well Ab orally side effets - |
|
|
what is the MOA, pharmacokinetics, side effects and toxicity of the K sparing diuretics
|
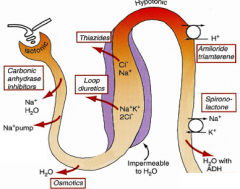
MOA- depends on the drug - Amiloride inhibits the Na- acid exchanger which reduces loss of K indirectly whereas Spironolactone is a competative aldosterone antagonist so is direct acting. weak diuretics so used in combination to reduce hypokalaemia.
pharmacokinetics - / side effects - No apparent adverse effects in dogs except reversible prostatic atrophy. skin reaction in cats. used for ascites due to hepatic disease, used in combination to reduce low K, or to reduce the systemic effects of aldosterone. spironolactone is licenced for use in dogs for valvular heart disease. |
MOA- 2 possibilities
pamaokinetics- none!! side effects- only on prostate/ skin reation in..... use- .......... |
|
|
what are the 'rare use ' diuretics
|
Carbonic anhydrase inhibitors
Osmotics (Xanthines, e.g. theophylline) - more as positive inotropes or bronchodilators |
|
|
|
what is the MOA, of the carbonic anhydrase inhibitors and the osmotic diuretics what are they commonly used for other than being diuretics and are there any countraindications.
|
MOA of CAI-Secreted into PCT- Inhibit tubular production of H+ for Na+/H+ exchange leading to increased NaHCO3 & water (& K+) excretion- Causes acidosis.-
osmotics -Filtered & effective mainly in PCT +loop use- topical CAI are often used for treating glycoma in cats and dogs. use of osmotics - cerebral oedema/increased intra-cranial pressure (moves fluid>plasma, +?)/oiguric renal failure (must re-hydrate)/topically for glaucoma - not commonly/Contra-indicated in congestive heart failure & other generalised oedema as increases plasma volume. ??? |
|
|
|
which diuretics are licensed and for what
|
furosemide for use in SAs in tablet form for oedema and in SAs, cattle and horses not intended for human consumption in injectable form.
spirolactone ( k sparing diuretic ) - dogs for valvular heart disease in tablet form. |
furosemide and spironolatone
|
|
|
what is the most common use for diuretics and list some others.
|
Treatment & control of systemic oedema -to decrease systemic oedema in congestive HF ( ALL PATIENTS SHOULD GET A DIURETIC) as blood pressure may increase as much as 30 %. ( most common use). Also to decrease systemic oedema from hepatic and renal disease.
.Management of localised oedema -Glaucoma: topical CAIs (or other classes of drugs)/Cerebral oedema: mannitol i/v/Non-bacterial udder oedema (heifers) occasionally treated with furosemide .Maintain urine flow (acute renal failure) -usually furosemide (also mannitol & dopamine) after re-hydration. Treatment of certain endocrinopathies -hypercalcaemia - i/v furosemide & saline/diabetes insipidus - thiazides/hyperaldosteronism - spironolactone Exercise-induced pulmonary haemorrhage in horses (esp. in USA) - i/v furosemide (UK-not if competing!) Hypertension: thiazide diuretics are first line treatment in humans but vasodilators are used in animals |
systemic oedema- congestive HF
localised furosemide treatment of hypocalcaemia, diabetes insipidus, hyperthyroidism an exercising horse problem ... hypertension in humans |
|
|
when would CHF NOT require a diuretic
|
the only exception to the use of diuretics in CHF is cardiac tamponade due to pericardial effusion - here pericardiocentesis is essential.
|
|
|
|
give an example of the combined use of diuretics
|
furosemide is the first line diuretic, may be used with spironolactone, or with a thiazide/thiazide+amiloride combination
|
use the loop 1st !!!
|
|
|
what are the possible side effects of all diuretics and in which sp are they more of an issue
|
All diuretics may potentially cause dehydration, pre-renal azotaemia & electrolyte disturbances, especially hypo-K+........-More often a problem in cats, where lower doses/frequencies of administration should be employed: species & behaviour
Hyponatraemia in severe CHF may be due to over-diuresis, or to excessive ADH secretion.???? Hypomagnesaemia - rare ( excreated with others) Incontinence can be a problem, esp. in older patients & neutered bitches!Increased thirst/urination to be expected Treating CHF + CRF is a problem! as there will already be azotaemia |
all - pre renal azotaemia, obviously dehydration, electrolite disturbances esp.... a group esp to prevent this.
low Na low Mg incontinence esp in .... CHF and CRF... |
|
|
how are these side effects avoided or controled
|
Reduce problems by:Use ACE inhibitors ± spironolactone with diuretics/Use appropriate doses/frequencies/routes of admin.- avoid iv as it causes more electrolyte disturbances /Ensure cardiac function/rhythm adequately treated.
Not usually a problem in dogs & cats, esp. with furosemide, if eating & drinking normally & if moderate doses are used (“enough but not too much”!) Where higher doses needed, if patient well, mild dehydration & azotaemia (urea <30mmol/l) can usually be tolerated/may be unavoidable! |
|
|
|
describe how resistance to diuretics may arise and how might this be overcome
|
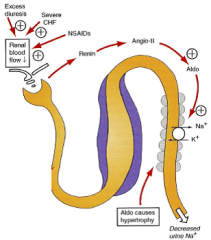
hypertrophy of the DC tubular cells will increase their ion transport capacity
Efficacy of diuretics may be improved by: Increasing the dose/frequency (esp. furosemide) Giving by i/v bolus or continuous rate infusion (increases bioavailability/duration of action) Improving cardiac function & controlling arrhythmias/excessive heart rates Adding ACE inhibitors ± spironolactone Use “sequential nephron blockade” Ensure compliance; ?salt restriction |
|

