![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
18 Cards in this Set
- Front
- Back
|
4 Factors Affecting Rumenoreticular Contractions |
1. Feeding - increases frequency and amplitude of contractions 2. Diet composition - more grain or smaller particles decreases rate and amplitude of contractions 3. VFAs - decrease primary contractions 4. Metabolic Disorders - decrease primary contractions (ie: hardware disease, hypocalcemia) |
|
|
What are the 3 receptors involved with regulating rumenoreticular motility? |
1. Epithelial receptors located on the basement membrane of the RR detect chemical and mechanical stimuli (light tactile) 2. Mucosal receptors located on the mucosa of the abomasum and intestine detect mechanical and chemical (acid/hyperosmolality) stimuli 3. Tension receptors in the muscle of the reticulum, cranial rumen sac, abomasum and intestines detect mechanical tension (physical distension and drug induced contractions) |
|
|
What are the three mechanisms of rumenoreticular motility regulation? |
Neural: 1. Vago-vagal 2. Splanchnic Hormonal: 3. Cholecystokinin |
|
|
Describe the stimulation mechanism of RR motility |
Through neural and hormonal signals: - Moderate RR distension activates medullary gastric and salivation centres to increase salivation, rumination and RR motility. - Abomasal mucosal receptor activation from acid leads to increased RR motility
|
|
|
Describe the inhibitory mechanism of RR motility |
Through neural and hormonal signals: - Severe RR distension inhibits medullary gastric and salivation centres, which decreases salivation, rumination and RR motility - Tension receptors in the abomasum and duodenum leads to decreased motility (to limit emptying) |
|
|
How much gas production occurs? Where does it end up? |
12-27L/min of gas is made at peak (postfeeding). 1-2L/min is average.
CO2: 25-35% absorbed in blood (and removed by lungs); the rest lost through mouth Methane: 20% in blood, 80% mouth |
|
|
What can inhibit eructation? |
1. Presence of digest near the cardia and lower esophageal sphincter 2. Epinephrine and histamine *Note that this will cause the animal to bloat! |
|
|
What is the stimulus for eructation? |
Gaseous distension of the reticulum and rumen causes an increase in secondary contractions, which moves gas from the dorsal sac to the cardia. The ruminoreticular fold and cranial pillar create a digesta barrier so the cardia is free of fluid. This allows the gas to leave through the esophagus through reverse peristalsis. |
|
|
Why does bloat cause death? |
As the rumen expands, there is pressure on the diaphragm which inhibits respiration, causing death. |
|
|
What is free gas bloat? |
- Caused by physical obstruction of the esophagus or cardia, such as from feed, vagus nerve damage (i.e. from chronic pneumonia or hardware disease) or irregular feed intake (i.e. changes in diet, uneven water/feed intervals) - Rapid onset
|
|
|
What is frothy bloat? |
- Also known as pasture/alfalfa bloat - Often occurs with high grain or fresh alfalfa diets - Increased mucopolysaccharide production from S. Bovis combined with cell lysis (which releases soluble proteins) increases the rumen fluid viscosity, which traps gas bubbles and makes a froth - Individual variability (ie Holsteins more at risk than beef breeds) |
|
|
How can you measure GI motility? |
1. Gastric Emptying Scintigraphy: use known amount of radioactive substance 2. Stable isotope breath tests: use 13C and see how much leaves lungs as CO2 3. MRI 4. Functional Ultrasonography: for gastric volume and emptying, and antropyloric contractions 5. Absorbable markers: paracetamol or acetominophen 6. Non absorbable markers: phenol red, methycellulose, wireless pH or motility capsules |
|
|
How can you measure gastric capacity and accommodation? |
1. Balloon measurements (Barostat) 2. Single photon emission computed tomography: requires CT of stomach after IVing a chemical |
|
|
What are the functional regions of the stomach? |
1. The Gastric Pump (antrum, part of corpus) - phasic contractions 2. The Gastric Reservoir (most of corpus, fundus) - tonic contractions |
|
|
What are the 3 phases of the gastric pump? |
1. Phase of propulsion: Proximal antral contraction causes liquid to rapidly move toward pylorus. Large particles then also flow toward pylorus. 2. Phase of emptying: A middle antral contraction allows small particles to empty through pylorus, but large particles are retained. 3. Phase of retropulsion: A distal antral contraction - large particles are cleared from the terminal antrum. |
|
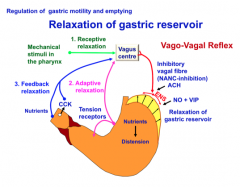
Describe relaxation of the gastric reservoir. (What does this flowchart mean?) |
- Receptive relaxation during chewing and swallowing due to a vago-vagal reflex from mechanical stimuli in the pharynx (picked up in the vagus centre). - Adaptive relaxation triggered by digesta in the stomach (mediated through both the vagus centre and the gastrogastric reflex btw the gastric reservoir and antral pump) - Feedback regulation triggered by nutrients (and CCK?) in the small intestine through vagus centre (known as the duodenal, jejunal or ileal brake) - The vagus centre communicates back to the stomach through a NANC inhibitory vagal fiber, where Ach activates the ENS, which then releases NO, PACAP, VIP and ATP --> relax muscle |
|
|
Will hay or grain produce a greater receptive relaxation phase in horses? |
Hay. Maybe because it requires more chewing. |
|
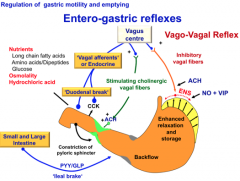
Describe the entero-gastric reflexes |
- Sensory vagal afferent fibers are activated by intestinal nutrients, osmolality, acid, and hormones; then are integrated in the vagal centre/DMV. - Vagal efferents can cause relaxation in the proximal stomach [via NO, VIP] or increase contractions of the pyloric sphincter [via Ach] - Gastrointestinal hormones can feed back to inhibit or stimulate gastric motility - The duodenal brake (CCK), ileal brake (GLP,PYY), secretin and GIP will inhibit gastric motility - Ghrelin, neurotensin and gastrin will stimulate gastric motility |

