![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
124 Cards in this Set
- Front
- Back
|
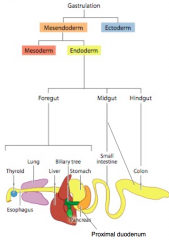
During what stage does formation of the GI tract begin?
|
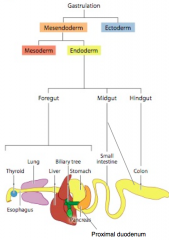
During gastrulation (week 3)
|
|
|
What is the first step information of the GI tract?
|
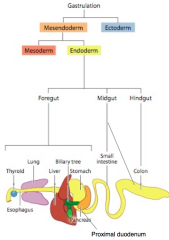
Formation of the three germ layers
- Endoderm - Mesoderm - Ectoderm |
|
|
What does the endoderm form in the GI tract?
|
Epithelial components of the gut
|
|
|
What does the mesoderm form in the GI tract?
|
Splanchnic Mesenchyme → Muscle, CT, and other layers of the wall of the gut
|
|
|
What does the ectoderm form in the GI tract?
|
Ectoderm-Derived Neural Crest → Enteric Nervous System
|
|
|
What happens following gastrulation to the GI precursors?
|
Small indentations develop first in the anterior and then in the posterior of the embryo
|
|
|
What does the anterior indentation in the GI of the embryo form?
|
Foregut diverticulum (anterior intestinal portal)
|
|
|
What does the posterior indentation in the GI of the embryo form?
|
Hindgut diverticulum (caudal intestinal portal)
|
|
|
Does the foregut or hindgut diverticulum form first?
|
Foregut diverticulum (anterior intestinal portal) forms before the hindgut diverticulum (posterior intestinal portal)
|
|
|
What do the foregut and hindgut diverticulum form? How?
|
They elongate to form to tubes that fuse into a single, straight tube consisting of the foregut, midgut, and hindgut
|
|
|
What does the foregut give rise to?
|
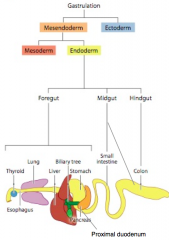
Epithelium of:
- Esophagus - Stomach - Proximal duodenum (Also the Thyroid, Lung, Liver, and Pancreas) |
|
|
What does the midgut give rise to?
|
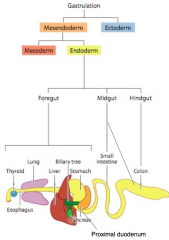
Epithelium of the small intestine
- Distal duodenum - Jejunem - Ileum Contributes to the epithelium of the large intestine - Cecum - Appendix - Ascending colon - First 1/3-1/2 of the transverse colon |
|
|
What does the hindgut give rise to?
|
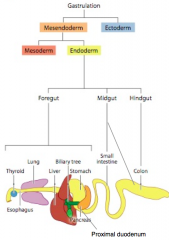
Contributes to the epithelium of the large intestine:
- Remaining 1/2-2/3 of the transverse colon - Descending colon - Sigmoid colon - Rectum - Superior part of anal canal |
|
|
What is the general organization of the wall of the GI tract?
|
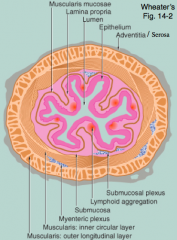
Four tunics / layers:
- Mucosa (innermost) - Submucosa - Muscularis Externa - Adventitia or Serosa |
|
|
What is the innermost layer of the GI tract? What is it composed of?
|
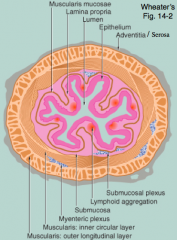
Mucosa
- Epithelium - Lamina propria - Muscularis mucosa |
|
|
What is the second layer of the GI tract? What is it composed of?
|
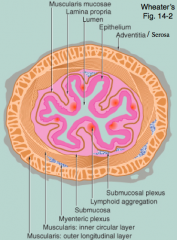
Submucosa
- Loose collagenous and adipose supporting tissues - Large vessels and lymphatics - Innervated by submucosal / Meissner's plexus |
|
|
What is the third layer of the GI tract? What is it composed of?
|
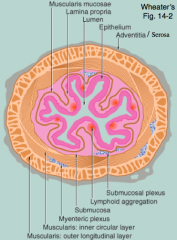
Muscularis Externa
- Inner circular layer of smooth muscle - Outer longitudinal layer of smooth muscle - Innervated by myenteric / Auerbach's plexus |
|
|
What is the outermost layer of the GI tract? What is it composed of?
|
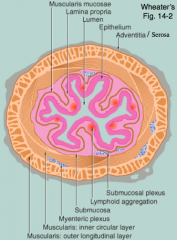
Adventitia / Serosa
- Outer layer of tissue that surrounds the entire tube |
|
|
What are the plexuses that innervate the GI tract? Which layer do they innervate?
|
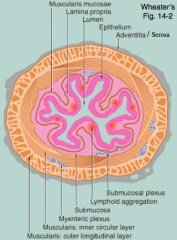
- Meissner's / Submucosal Plexus - innervates submucosa
- Auerbach's / Myenteric Plexus - innervates the Muscularis Externa |
|
|
What happens to food in the stomach?
|
Mechanical and chemical digestion → forms chyme
- Strong churning action breaks down solid food - Chemical breakdown is accomplished by gastric juices secreted by mucosal epithelial glands |
|
|
What is formed in the stomach?
|
Chyme
|
|
|
Where are the gastric juices released from in the stomach?
|
Mucosal epithelial glands
|
|
|
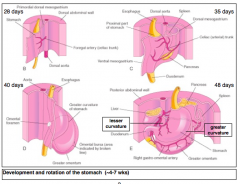
What does the stomach form from? How?
|
- Forms from the foregut
- "Fusiform" or "spindle-shaped" dilation of foregut around week 4 |
|
|
What is the stomach attached to?
|
- Between the esophagus and intestine
- Attached to the body wall by dorsal and ventral mesenteries |
|
|
What nerves are on the left and right sides of the stomach?
|
L and R Vagus nerves
|
|
|
Along what axis does the primordial stomach enlarge along?
|
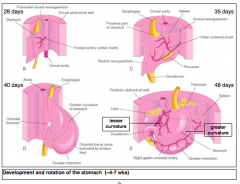
Dorsal-ventral axis
|
|
|
What part of the stomach expands more quickly? More slowly? Implications?
|
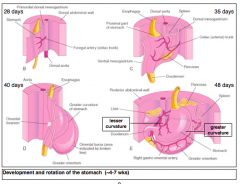
- Dorsal wall of stomach expands more quickly → Greater Curvature of Stomach
- Ventral wall of stomach expands more slowly → Lesser Curvature of Stomach |
|
|
What happens after formation of the greater and lesser curvatures?
|
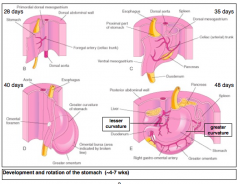
- Stomach rotates 90 degrees clockwise around its longitudinal axis
- This places the long axis of the stomach almost transverse to the long axis of the body - Lesser curvature faces right side of body |
|
|
What are the implications of the rotation of the stomach by 90 degrees?
|
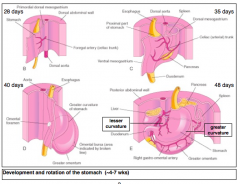
- Left vagus nerve supplies the anterior wall of the mature stomach
- Right vagus nerve supplies the posterior wall of the mature stomach - Produces a space behind the stomach referred to as the lesser sac or omental bursa - Pulls the stomach and duodenum upward |
|
|
Which nerve supplies the anterior wall of the mature stomach? Why?
|
Left Vagus Nerve (renamed anterior vagal trunk nerve) d/t the 90 degree rotation
|
|
|
Which nerve supplies the posterior wall of the mature stomach? Why?
|
Right Vagus Nerve (renamed posterior vagal trunk nerve) d/t the 90 degree rotation
|
|
|
What is the greater omentum formed from?
|
Dorsal mesentery extends from greater curvature to form the greater omentum
|
|
|
What is the lesser omentum formed from?
|
Ventral mesentery attaches to the developing liver and lesser curvature to form the lesser omentum
|
|
|
What is the space formed posterior to the stomach?
|
Lesser sac / omental bursa
|
|
|
What is the space formed anterior and inferior to the stomach?
|
Greater sac
|
|
|
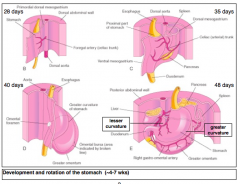
What kind of cells form the epithelium of the mature stomach? What do they arise from?
|
- Simple columnar cells
- Arise from the foregut endoderm |
|
|
What do the smooth muscle and connective tissue components of the stomach derive from?
|
Splanchnic Mesenchyme
|
|
|
What components form the duodenum?
|
- Foregut and midgut endoderm
- Splanchnic mesenchyme - Neural crest |
|
|
What kind of cells do the foregut and midgut endoderm form in the duodenum?
|
- Simple columnar epithelium that covers the villi
- Crypts of Lieberkuhn |
|
|
What does the splanchnic mesenchyme form in the duodenum?
|
Smooth muscle and connective tissue components of duodenum
|
|
|
What does the neural crest form in the duodenum?
|
Neurons that innervate the gut (enteric nervous system)
|
|
|
What is the location of the junction between the foregut and midgut endoderm?
|
Distal to the bile duct
|
|
|
What is the shape of the duodenum? What happens as it expands?
|
Transforms from a straight tube to a "C" shaped tube
|
|
|
What happens to the duodenum as the developing stomach rotates?
|
The duodenum also rotates to the right
|
|
|
What happens to the lumen of the esophagus and the duodenum during development?
|
The epithelial cells derived from the endoderm proliferate to occlude the lumen of the gut tube
|
|
|
What locations in the GI tract have occlusion of the lumen during development?
|
- Esophagus
- Duodenum |
|
|
How do you restore the lumen in the esophagus and duodenum?
|
Re-canalization
|
|
|
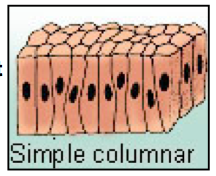
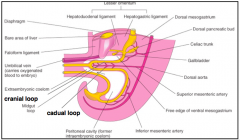
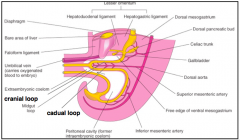
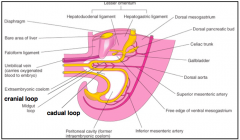
What happens to the midgut as it elongates?
|
Forms a ventral U-shaped tube termed the midgut loop or primary intestinal loop
|
|
|
What are the components of the midgut U-shaped loop?
|
- Cranial Loop
- Caudal Loop |
|
|
What connects the Cranial and Caudal Loops of the Midgut Loop?
|
Omphaloenteric duct (aka Vitelline duct, Omphalomesenteric duct, or Yolk Stalk)
|
|
|
What does the Cranial Loop of the Midgut Loop give rise to?
|
Gives rise to the bulk of the small intestine (distal duodenum, jejunum, and most of the ileum)
|
|
|
What does the Caudal Loop of the Midgut Loop give rise to?
|
Distal ileum, cecum, appendix, and parts of the colon (ascending colon and part of the proximal transverse colon)
|
|
|
What happens to the midgut loop as it develops into the organs? Why?
|
The organs expand more quickly than the body cavity expands, so the midgut loop herniates through the umbilicus into the umbilical cord forming a Physiological Umbilical Hernia
|
|
|
What happens after the Midgut Loop herniates into the umbilicus?
|
The midgut loop rotates 90 degrees counterclockwise around the axis of the superior mesenteric artery (as viewed from the front of the embryo)
|
|
|
What are the implications of the Midgut Loop rotating 90 degrees clockwise after herniating into the umbilicus?
|
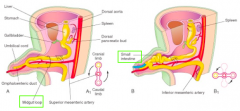
- Positions the cranial limb on the right
- Positions the caudal limb on the left |
|
|
What happens to the cranial limb of the Midgut Loop after it has rotated 90 degrees counterclockwise?
|
Cranial limb undergoes looping to form the primordial jejunum and ileum
|
|
|
What happens to the caudal limb of the Midgut Loop after it has rotated 90 degrees counterclockwise?
|
Caudal limb develops the cecal bud, which ultimately forms the cecum
|
|
|
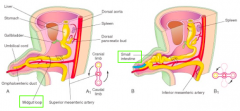
What happens at 10 weeks, once the body cavity has grown sufficiently?
|
- The midgut loop retracts into the body cavity (out of the umbilicus)
- Cranial limb retracts before the caudal limb - Midgut undergoes another 180 degree rotation counterclockwise around the axis of the SMA |
|
|
Where do the cranial and caudal limbs of the Midgut loop go once the body cavity expands sufficiently?
|
- Cranial loop returns into the left side of the body cavity
- Caudal loop returns to the right side of the body cavity - Transverse colon rests in front of the duodenum - Initially, cecum and short ascending colon rest under the liver |
|
|
What happens to the cecum and short ascending colon after it returns into the body cavity?
|
- Initially the cecum and short ascending colon rest underneath the liver
- As the ascending colon grows and elongates, the cecum descends, placing the cecum and appendix in the RLQ of the body |
|
|
What happens to the vitelline duct during the fetal period?
|
It regresses and disappears
|
|
|
What marks the division between the midgut-derived and hindgut-derived ascending colon?
|
Transition of the blood supply from the superior mesenteric artery (to the midgut) to the inferior mesenteric artery (to the hindgut)
|
|
|
What is the term for the expanded terminal region of the hindgut?
|
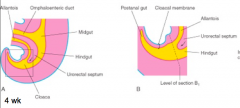
Cloaca
|
|
|
What partitions the cloaca?
|
Urorectal septum - mesenchyme grows and expands to separate the cloaca
|
|
|
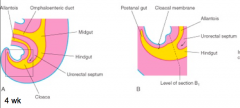
How does the urorectal septum form? Function?
|
- Septum develops at an angle between the allantois and hindgut
- As it grows toward the cloacal membrane, it extends fork-like projections that result in infolding of the lateral walls of the cloaca - As the infolds grow toward each other and fuse, leading to a partition of the cloaca |
|
|
What forms after the urorectal septum partitions the cloaca?
|
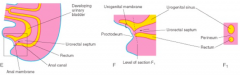
- Dorsal side produces the rectum and part of the anal canal
- Ventral side produces the urogenital sinus |
|
|
What does the urorectal septum fuse with?
|
Fuses with the cloacal membrane to divide it into a dorsal anal membrane and a ventral urogenital membrane
|
|
|
What does the urorectal septum partition the cloacal sphincter into?
|
External anal sphincter (posterior part) and multiple muscles (superficial transverse perineal, bulbospongiosus, and ischiocavernosus) (anterior part)
|
|
|
What muscles are separated from the cloacal sphincter by the urorectal septum? How are they related?
|
- Superficial transverse perineal
- Bulbospongiosus - Ischiovavernosus - They are all innervated by the pudendal nerve |
|
|
What forms the anal canal?
|
- Superior - from hindgut
- Inferior - from proctodeum (ectodermally-derived) |
|
|
What do the liver, gallbladder, and biliary duct system develop from?
|
Outgrowth of the ventral foregut endoderm
|
|
|
What happens in the first phase of the liver bud (hepatic diverticulum) formation?
|
- The foregut endoderm, composed of polarized columnar epithelial cells, protrudes into the surrounding septum transversum mesenchyme
- Apical surface faces the gut lumen and basal surfaces contact laminin-rich basement membrane |
|
|
What is the septum transversum mesenchyme derived from?
|
Splanchnic mesoderm between heart and midgut
|
|
|
What happens in the second phase of the liver bud (hepatic diverticulum) formation, after the foregut endoderm protrudes into the septum transversum mesenchyme?
|
Simple columnar epithelium transforms into a pseudostratified epithelium encased in basement membrane
|
|
|
What happens in the third phase of the liver bud (hepatic diverticulum) formation, after the epithelium transforms to a pseudostratified epithelium encased by BM?
|
- BM is degraded, and bipotential hepatoblasts delaminate and migrate into the septum transversum mesenchyme
- This forms cords of hepatic cells within the mesenchyme - Hepatoblasts have potential to differentiate into hepatocytes, the epithelial cells of the liver parenchyma, or into cholangiocytes, the epithelial cells of the biliary system |
|
|
What are the epithelial cells of the liver parenchyma?
|
Hepatocytes
|
|
|
What are the epithelial cells of the biliary system?
|
Cholangiocytes
|
|
|
What do the hepatoblasts have the potential to differentiate into during formation of the liver bud?
|
- Hepatocytes (epithelial cells of the liver parenchyma)
- Cholangiocytes (epithelial cells of the biliary system) |
|
|
What growth factors are secreted from the heart and the septum transversum? Function?
|
- FGFs and BMPs
- Essential for proper specification and outgrowth of the primordial liver bud |
|
|
What surrounds the pseudostratified liver bud? Function?
|
- Necklace of endothelial cells
- Required for delamination and expansion of the liver |
|
|
What is the fetal liver an important site for?
|
Hematopoiesis - remains the key site of hematopoiesis prior to the onset of BM hematopoiesis
|
|
|
Why is the liver characteristically bright red?
|
Hematopoiesis
|
|
|
What are the sinusoids of the liver? What are they derived from?
|
- Blood vessels residing at the basal surface of polarized hepatocytes
- Derived from vessels resident in the septum transversum mesenchyme via angiogenesis |
|
|
What does the gall bladder originate from?
|
Small caudal region of the liver bud
|
|
|
What does the cystic duct originate from?
|
Stalk of the liver bud
|
|
|
What does the stalk connecting the hepatic and cystic ducts to the duodenum become?
|
Bile duct
|
|
|
What does the bile duct connect to?
|
- Initially attaches to the ventral aspect of the duodenal loop
- As the duodenum grows and undergoes rotation, the bile duct is carried to the dorsal aspect of the duodenum |
|
|
What does the pancreas originate from?
|
Two buds emanating form the dorsal and ventral foregut endoderm
|
|
|
What does the dorsal and ventral endoderm give rise to?
|
Exocrine and endocrine epithelial cells of the pancreatic parenchyma
|
|
|
How does the rotation of the duodenum to form a "C" shape affect the developing pancreas buds?
|
Ventral pancreatic bud is carried dorsally to lie posterior to the dorsal pancreatic bud, the buds eventually fuse
|
|
|
Which pancreatic bud emerges first? What does it give rise to?
|
- Dorsal pancreatic bud
- Gives rise to the majority of the mature pancreas |
|
|
What signals are important for the development of the dorsal pancreatic bud?
|
- Signals received from the notochord, which resides above the endoderm fated to form the pancreas
- Notochord secretes FGF2 and Activin to inhibit SHH, promoting pancreatic development instead of intestinal development |
|
|
What happens to the notochord during development that impacts the formation of the dorsal pancreatic bud?
|
- Notochord is displaced by the fusing dorsal aorta
- Endodermal cells of the dorsal pancreatic bud now receive signals from the aorta to promote bud expansion and endocrine cell differentiation |
|
|
What induces exocrine cell differentiation of the dorsal pancreatic bud?
|
Caused by mesenchyme comes between the aorta and dorsal pancreas
|
|
|
How does SHH affect the development of the pancreas?
|
- Dorsal pancreatic bud: SHH is inhibited by FGF2 and Activin from the notochord, which promotes pancreatic development instead of intestinal development
- Ventral pancreatic bud: SHH is not involved |
|
|
What signals are important for the development of the ventral pancreatic bud?
|
- It is automatically fated to become pancreatic, but can become fated to become hepatic by instructive factors like FGFs and BMPs
- SHH is not involved in the signaling |
|
|
What is the affect of FGF and BMP on the ventral pancreatic bud? Where do these signals come from?
|
- FGF and BMP are secreted from the closely associated cardiac and septum transversum mesenchyme tissues
- They cause the pancreatic fated tissues to a adopt a hepatic fate |
|
|
What does the ventral pancreatic bud require for its development?
|
- Splanchnic mesoderm
- Signals from the vasculature, namely the vitelline veins, for expansion and differentiation of the endocrine and exocrine cell lineages |
|
|
What are the possible defects in duodenal development?
|
- Duodenal atresia - failure to recanalize, complete occlusion
- Duodenal stenosis - failure to completely recanalize, partial occlusion |
|
|
What are the implications of blockage of the duodenum (duodenal atresia and stenosis)?
|
- Vomiting of the stomach contents as well as bile
- Often associated with other congenital anomalies - Polyhydramnios occurs w/ duodenual atresia because the blockage prevents proper intestinal absorption of the swallowed amniotic fluid |
|
|
What is Polyhydramnios? When does it occur?
|
Occurs w/ duodenual atresia because the blockage prevents proper intestinal absorption of the swallowed amniotic fluid
|
|
|
What is the most serious anomaly of extrahepatic biliary system development?
|
Extrahepatic Biliary Atresia
|
|
|
What is the most common cause of Extrahepatic Biliary Atresia?
|
Obliteration of bile ducts (85% of cases)
|
|
|
What are the symptoms of Extrahepatic Biliary Atresia? Prognosis?
|
- Jaundice occurs soon after birth
- Stools are acholic (clay colored) - If unable to repair ducts surgically, biliary atresia will be fatal without a liver transplant |
|
|
What causes Gastroschisis?
|
- Defect lateral to the median plane of the anterior abdominal wall
- Poorly understood etiology, thought to be multifactorial (vascular events and/or environmental factors may contribute by impacting abdominal wall development) |
|
|
What happens if there is a defect lateral to the median plane of the anterior abdominal wall?
|
Gastroschisis
- Abdominal viscera are extruded through the wall (does not involve the umbilical cord) - Protruding viscera are bathed in amniotic fluid, which causes Serositis |
|
|
Where does Gastroschisis occur?
|
Most commonly on the right side lateral to the umbilicus
|
|
|
What is Gastroschisis categorized as?
|
- Not a hernia because it is not covered in a sac
- It is an evisceration |
|
|
What is the term for herniation of the abdominal contents into the proximal umbilicus?
|
Omphalocele
|
|
|
What happens in Omphalocele?
|
- Herniation of the abdominal contents (small and large intestine, liver, stomach, and gonads) into the proximal umbilicus
- Failure of the intestine to return to the abdomen during development |
|
|
How does Gastroschisis compare to Omphalocele?
|
Gastroschisis
- Evisceration (not a hernia) - Not associated with other congenital anomalies Omphalocele - Hernia into proximal umbilicus - Commonly associated with other congenital anomalies (including cardiac and urogenital defects) |
|
|
What commonly causes congenital anomalies of the small intestine?
|
Defects in gut rotation including non-rotation or mal-rotation, also reverse rotation (rare)
|
|
|
What are the impacts of defects in gut rotation on the intestines?
|
- Leads to misplacement of the intestines within the body cavities
- Improperly positioned and fixed intestines can lead to twisting of the midgut = Volvulus |
|
|
What is the term for twisting of the midgut d/t a fixed intestine?
|
Volvulus
|
|
|
What are the implications of Volvulus?
|
Intestinal:
- Obstruction - Infarction - Gangrene |
|
|
What direction does the gut normally rotate during development? What direction can it turn rarely, called "reverse rotation"?
|
- Normal: counterclockwise
- Reverse: clockwise |
|
|
What is the term for an out-pocketing of the ileum?
|
Meckel Diverticulum
|
|
|
What is one of the most common anomalies of the GI tract?
|
Meckel Diverticulum
|
|
|
What is a Meckel Diverticulum a remnant of? What is it?
|
- Remnant of the Omphaloenteric duct
- It is an outpocketing of the Ileum |
|
|
What are the symptoms of Meckel Diverticulum?
|
- Can become inflamed
- Mimics appendicitis - Can lead to ulceration and bleeding because of secretion of gastric acid and gastric and pancreatic enzymes |
|
|
What is the anatomical organization of a Meckel Diverticulum?
|
Wall of the diverticulum contains all layers of the ileum and may also contain gastric and pancreatic tissues
|
|
|
What can cause ulceration and bleeding in Meckel Diverticulum?
|
Secretion of gastric acid and gastric and pancreatic enzymes
|
|
|
What is the disease that presents as a "mega-colon" (enlarged colon)?
|
Hirschsprung disease
|
|
|
What causes Hirschsprung disease?
|
Aganglionosis - enlarged, dilated region contains normal ganglion cells but the affected tissue lacks ganglion cells and fails to relax, thus preventing movement of bowel contents
|

