![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
102 Cards in this Set
- Front
- Back
|
What are the four secretory salivary glands and what is their secretions? |
Parotid: serous/watery secretion Mandibular/submaxillary: serous and mucous Sublingual: serous and mucous Buccal: mucous |
|
|
Where is saliva initially secreted by? And where is it modified? |
Secreted by acinar
Modified by the ducts (Na & HCO3 absorption, K secretion) |
|
|
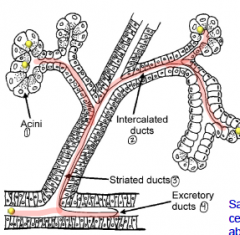
What is the pathway for saliva excretion? |
Acini -> Intercalated ducts -> Striated ducts -> Excretory ducts |
|
|
Regardless of how much saliva is produced, the saliva is also _______ with the blood in ruminants. |
Isotonic |
|
|
What two components of saliva are unique in Ruminants? |
Bicarbonate and Phoshate |
|
|
What are the four components of saliva? |
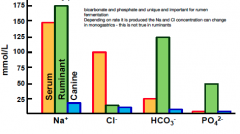
Na+, Cl-, HCO^3-, PO4^2- |
|
|
The quantity and composition of saliva depends on what two factors? |
Species Level of chewing activity |
|
|
What is the flow rate of ruminants and non ruminants? |
Ruminants - isotonic, with a high flow rate = increasing HCO3 and decreasing HPO4
Non Ruminants - low flow rate = increasing K and high flow rate = increasing HCO3 |
|
|
Secretion levels for cattle, horses, sheep, and birds |
Cattle 60-160 L/d Horse 10-12 L/d Sheep 6-16 L/d Birds 0.007-0.03 L/d |
|
|
Functions of saliva in ruminants? |
-fluid for fermentation (no secretory glands in the reticulo-rumen) -increase alkaline saliva (HCO3-, HPO4-) to buffer rumen pH -Recycle PO4- and Urea |
|
|
Functions of salivary secretions in dogs and cats? |
-evaporative cooling -salivary amylase (not cats) - lipase |
|
|
Function of saliva in pigs |
-increasing salivary amylase: function in proximal stomach but inactivated at low gastric pH
|
|
|
Function of salivary secretions in horses? |
-no salivary digestion enzymes -'latherin' - protein secreted from salivary glands (mastication) and skin (evaporative cooling) |
|
|
Functions of salivary glands in birds? |
-lubricate ingesta (mucous secreting cells) -salivary amylase -'pigeon milk' (fat cells from crop) for feeding in young |
|
|
How is the salivary secretion regulated by the sympathetic? |
By the sympathetic -NE-induced contraction of 'basket' myoepithelial cells -expel stored saliva rich in protein and mucin
|
|
|
How is the salivary secretion regulated by the parasympathetic? |
By the parasympathetic -Ach excites the acing cells = increased saliva low in protein -salivary reflexes: coordinated by 'salivary enters' in the hindbrain |
|
|
Distribution of gastric mucosa in a dog? |
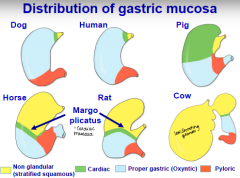
Majority proper gastric (oxyntic) and pyloric -small cardiac and non glandular |
|
|
Gastric mucosa distribution in the pig? |
Mostly cardiac and proper gastric -some non glandular and some pyloric |
|
|
Distribution of gastric mucosa in horses and rats? |
Mostly non glandular and proper gastric -some pyloric and cardiac
**margo placates between non glandular and gastric |
|
|
Distribution of gastric mucosa for cow? |
Mostly all non glandular Some proper gastric and pyloric Little cardiac |
|
|
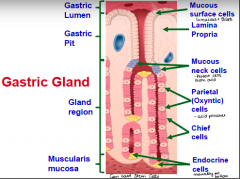
What are the 4 gastric glands and their secretions? |
Neck cells - secrete mucous, HCO3, trefoil peptides (repair/damage/protective cells) Parietal/oxyntic cells - secrete HCL, intrinsic factor (vit B12 absorption) Chief or peptic cells - secrete pepsinogen, gastric lipase Endocrine cells - secrete gastrin, somatostatin, histamine, and GRP (proventriculous) |
|
|
What is the Cardiac gland and what does it secrete? |
Branched tubular glands - secrete mucous, HCO3 |
|
|
What are the pyloric glands and what do they secrete? (lack parietal cells) |
Neck - secrete mucous Chief cells - secrete pepsinogen (few) Endocrine cells - secrete gastrin, somatostatin, histamine, and GRP (proventriculous) |
|
|
Gastric Gland (image) |
|
|
|
What are the 2 gastric cell types that are in the proventriculus? |
Simple mucous glands = mucous
Compounds submucosal glands = mucous, H=, pepsinogen |
|
|
What is the function of the following... Surface cells Neck cells Simple mucous glands (proventriculus) Parietal Cells Chief Cells Compounds submucosal glands (proventriculus) Endocrine cells |
Surface cells/Neck cells - Lubrication, Protection Simple mucous glands (proventriculus) - Lubrication (birds mucous) Parietal Cells - Protein digestion, binding of B12 Chief Cells - Digestion protein and fats Compounds submucosal glands (proventriculus) - Protein digestion Endocrine cells - Regulation of acid secretion |
|
|
What are the 3 phases of gastric acid secretion? |
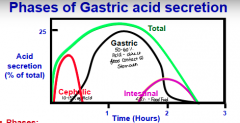
1. Cephalic 2. Gastric 3. Intestinal |
|
|
What is the cephalic phase of gastric acid secretion? |
-part of the response due to the anticipation, sight, smell, auditory, taste sensations -mechanism = VAGAL! 10-15% of acid |
|
|
What is the Gastric phase of gastric acid secretion? |
-part of the response is due to stimulation from meal in the stomach -mechanism = VAGAL, LOCAL, GASTRIN 50-60% of acid
|
|
|
What is the Intestinal phase of gastric acid secretion? |
part of the response due to stimulation from chyme in intestines -Mechanisms = VAGAL, HORMONAL <5% acid |
|
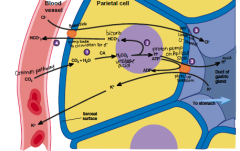
How does a parietal cell secrete acid? |
1. Carbonic anhydrase catalyzes the conversion of CO2 + H20 to make carbonic acid 2. Carbonic acid dissociates to H+ + HCO3- 3. Proton (H+) pump: H-K ATPase (lumen) pumps H against gradient into lumen, exchange K+ 4. HCO3- is secreted into blood in exchange for CL- (Alkaline tide) 5.Cl- digress from cell via Cl- conductance pathway on lumen membrane |
|
|
What is an alkaline tide? |
Alkaline tide happens during intense acid secretion -increased HCO3- secreted into blood (normally reversed when HCO3- is secreted via pancreatic juice to neutralize acid in the intestine) |
|
|
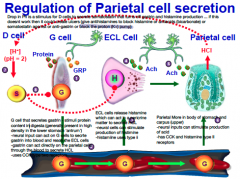
Regulation of the Parietal Cell Secretion - what controls it? |
-Neurocrine -paracrine -humoral (endocrine) |
|
|
Regulation of the Parietal Cell Secretion - what is the neuronal release and what does it stimulate? |
-Releases gastrin releasing peptide
-Stimulates gastrin from G-cells |
|
|
Regulation of the Parietal Cell Secretion - What does gastrin do? |
Endocrine -it activates the parietal cell -stimulates the release of histamine form the enterochromaffin-like cell (ECL) |
|
|
Regulation of the Parietal Cell Secretion - what does the neuronal release of Ach do? |
-directly activates the parietal cell -stimulates histamine release from the ECL cells |
|
|
Regulation of the Parietal Cell Secretion - what does histamine do? |
activates the parietal cell via a paracrine pathway |
|
|
Regulation of the Parietal Cell Secretion - accumulation of HCL (low pH=2) stimulates what? |
-the secretion of somatostatin from the D-cell |
|
|
Regulation of the Parietal Cell Secretion - what does the D-cell secretion of somatostatin do? |
-inhibits gastrin and histamine (turns off)
**if this doesn't happen might have ulcers |
|
|
What are the 3 major secretagogues (agonists) of parietal cell HACL secretion (synergism)? |
1.Gastrin acting though a CCL2 receptor 2. Histamine acting through a histamine H2 - receptor 3. Acetylcholine acting though a muscarinic 2 (M2) receptor |
|
|
Regulation of Parietal Cell Secretion (image) |
|
|
|
Acid secretion is influenced by what 3 factors? |
pH, good buffering and gastric emptying |
|
|
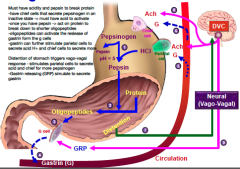
Regulation of Gastric secretions - what is the gastric phase of acid and pepsinogen secretion stimulated by? |
-intraluminal oligopeptides -distention of stomach |
|
|
Regulation of Gastric secretions - pepsinogen secreted by chief cells is activated to form what and by what? |
-to pepsin -by HCl secreted from parietal cells |
|
|
Regulation of Gastric secretions - pepsin breaks down the protein to release what? Which then stimulate what? |
-oligopeptides -stimulate gastrin release form G-cell in antrum |
|
|
Regulation of Gastric secretions - what does gastrin do? |
Acts as a endocrine transmitter to further stimulate... -HCl secretion from parietal cells -Pepsinogen from chief cells |
|
|
Regulation of Gastric secretions - How does gastric distention activate the vago-vagal reflex? |
1. Vagal afferent input activates dorsal vagal complex
2. vagal efferent outflow stimulates HCl and pepsinogen secretion
3. vagal efferents (via Ach) activate enteric neutrons and ECL cells (histamine) to stimulate pepsinogen and acid secretion
4. Vagal efferents stimulate secretomotor neurons to release GRP (gastrin releasing peptide) -> realeases gastrin |
|
|
Regulation of Gastric secretions (image) |
|
|
|
Why doesn't the stomach autosuggest? |
-Parietal and chief cells: apical barriers are impermeable to NH3, NH4, CO2, HCO3- -Presence of gastric mucosal barrier |
|
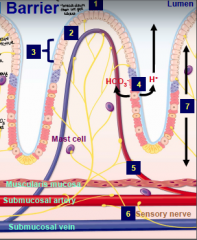
What are the layers of the gastric mucosal barrier? |
1. Unstirred layer 2. Surface epithelial cells 3. Cell renewal (restitution) 4. Alkaline tide 5. Microcirculation 6. Sensory nerves 7. Prostaglandins (PGE2, PGl2) and NO |
|
|
Gastric Mucosal Barrier - unstirred layer? |
- mucous and HCO3 (physical barrier) |
|
|
Gastric Mucosal Barrier - surface epithelial cells |
-secrete mucous, HCO3, PGs, HSP, trefoil peptides, antimibrobials |
|
|
Gastric Mucosal Barrier - Cell Renewal (restitution) from what and stimulated by? |
-from the mucosal progenitor cells -stimulated by growth factors |
|
|
Gastric Mucosal Barrier - Alkaline tide |
-exchange H+ out for HCO3- in |
|
|
Gastric Mucosal Barrier - Microcirculation - maintained by? and do what? |
-maintained by PG, NO, H2S -Protect endothelial cells form injury and prevent platelet and leukocyte aggregation |
|
|
Gastric Mucosal Barrier - Sensory nerves go where? |
-blood -lamina propria -mucosa |
|
|
Gastric Mucosal Barrier - Prostaglandins and NO do what? |
maintain/enhance all mucosal defines mechanisms |
|
|
What region of the Equine stomach is most prone to gastric ulcers? Why? |
Non glandular region = 80% -lacks mucous and bicarbonate layers
Glandular region = 20% -highly vascular and rapid restitution and mucous bicarbonate protection (heals rapidly)
|
|
|
What is the ontogeny of the stomach of a calf? |
Birth - 3ws = pre-ruminant phase (80% abomasum) 3-8 wks = Transition phase (50% abo) 2-4 months = pre/post weaning (25% abo) Mature = <10% abomasum |
|
|
GI ontogeny: Functional adaptations of cow stomach = 0-24 hrs |
-Colostrum (Ig, Vit A,D,E, lactose, Ca, Mg) -No acid/pepsinogen in abomasum -No gastric digestion (Ig protected and absorbed)
**Joint/naval ill, scours, hypothermia, hypoglycaemia, insulin sensitive
|
|
|
GI ontogeny: Functional adaptations of cow stomach = 1d to 3wks (pre-ruminant) |
-Milk based = salivary esterase (lipid hydrolysis) -Reflex closure of reticular groove (by sucking) -Rennin and milk = curd + whey (curdles in stomach) -No maltase = starch is indigestible
**scours, steatorrhea |
|
|
GI ontogeny: Functional adaptations of cow stomach = 3-8wks (transitional) |
- Milk and Grain and roughage -Grain -> VFA -> butyrate = stimulates RR papillae development -Less insulin sensitive |
|
|
GI ontogeny: Functional adaptations of cow stomach = 2-4 months and adult (pre/post weaning) |
-pepsinogen in ABOMASUM -RR motility, eructation, alkaline saliva - METABOLISM - VFA based and less insulin sensitive |
|
|
What are the 4 types of abomasa ulcers in calves?
**typically in the pylorus |
Type-1: non perforating Type-2: non perforating and blood loss Type-3: Perforating and local peritonitis Type-4: Perforating and diffuse pertonitis |
|
|
What are the 3 common etiologies of abomasa ulcers in calves? |
1. Alkalization of the pyloric antrum by bile reflux and duodenum 2. Mechanical trauma - hair balls (trichobenxoars) = abrasive action on mucosa 3. Stress: cortisone and corticotrophin = decreased gastric mucous secretion and cell renewal |
|
|
What are the 5 gastric ulcer therapies? |
1. Mucosal protectants 2. Proton pump inhibitors 3. H2 receptor antagonists 4. synthetic hormones - Prostaglandin analogues (increase mucosal flow) & somatostatin analogues (decrease gastrin secretion) 5. prokinetics (small animals and horses) |
|
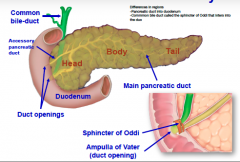
General anatomy of the pancreas.... |
-Common bile duct -Accessory pancreatic duct -Duct openings -Body, head, tail -Sphincter of oddi (common bile duct into duodenum) -Ampulla of vater (duct opening) |
|
|
What are the main endocrine cells in the pancreas? |
Islet of Langerhans (1-2% of the total mass of the pancreas)
|
|
|
What do the Islet of longerhans cells secrete? |
-Glugagon (a-cell; 10%) -Insulin (B-cell; 75%) -Somatostatin (δ-cell; 5%) -Pancreatic polypeptide (F or PP-cell) -Amylin (Amylin cell) |
|
|
What are the 3 functions of the exocrine secretions in the pancreas? |
1. Neutralization of duodenal pH 2. Optimize environment for bile action 3. Optimize fermentation in cecum and colon (horses) |
|
|
Explain 'neutralization of the duodenal pH' |
1. Inactivate pepsin - prevent acid-pepsin damage to duodenal mucosa 2. Optimize pH for pancreatic and brush border enzyme activity (pancreatic juice pH ~8.2-9.6) |
|
|
Explain 'optimize environment for bile action' |
Increase fatty acid and bile acid solubility |
|
|
Explain 'optimize fermentation in cecum and colon' |
continuous flow of juice in HCO3- buffer (low in enzymes) |
|
|
What are the two exocrine secretions of the pancreas? |
1. Enzymes - Trypsinogen, chymotrypsinogen, procarboxypeptidase, pancreatic amylase, pancreatic lipase, deoxyribonucleases and ribonucleases
2. Electrolytes- alkaline solution of electrolyse to neutralize stomach acid for optimum function of digestive enzymes (H2O, HCO3-, Cl-, Na+, K+, Mg2+, Ca2+) |
|

What are these 3 components? |
Top to bottom -Acinar cells (enzymes) -Centro-acinar cells (HCO3-) -Duct Cells (HCO3-/Cl- exchange) |
|
|
What are the 4 exocrine secretory proenzymes and enzymes secreted by the acing cells? |
1. Peptidases (90%) 2. Amylases (7%) 3. Lipases (2%) 4. Nucleases (<1%) |
|
|
What is secreted from the centro-acinar cells? |
Water and electrolytes (bicarb) |
|
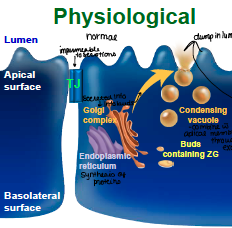
How does the acinar cell secrete enzymes? |
-Buds coming from the Zymogen Granules (ZG) from golgi coalesce to form vacuoles that -Exocytosis of ZG restricted to apical membrane (Basolateral exit blocked) to enter into the lumen -Tight Junction complex restricts paracellular movement of proteins/ions |
|
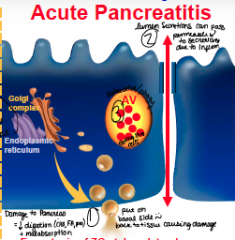
How does the acinar cell secrete enzymes with acute pancreatitis? |
-excytosis of zymogen granules at basolateral membrane (which is usually blocked) and the apical exit decreased -INCREASED paracellular permeability -DECREASED secretion and autophagy (AV; activation of digestive enzymes within cell)
**this causes damage to the pancreas = decrease in digestion and absorption |
|
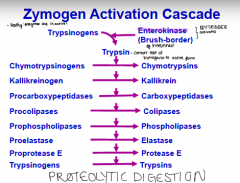
What is the zymogen Activation Cascade? |
Trypsinogen's are converted to trypsin by ENTEROKINASE (brush border) -trypsin causes a cascade and changes other zymogens to their active form (including trypsinogen) |
|
|
Trypsin -Zymogen -Activator -Action |
Trypsinogen Enterokinase Endopeptidase: cleaves internal bonds |
|
|
Chymotrypsin -Zymogen -Activator -Action |
Chymotrypsinogen Trypsin Endopeptidase |
|
|
Elastase -Zymogen -Activator -Action |
Proelastase Trypsin Endopeptidase
|
|
|
Carboxypeptidase -Zymogen -Activator -Action |
Procarboxypeptidase Trypsin Exopeptidase: cleaves last AA from the c-terminal polypeptide
|
|
|
Phospholipase -Zymogen -Activator -Action |
Prophospholipase Trypsin Cleaves FA from phospholipids (lecthin) |
|
|
Lipase -Zymogen -Activator -Action |
None None Cleaves FA from glycerol
|
|
|
Amylase -Zymogen -Activator -Action |
None None Digest starch to maltose and glucose
|
|
|
Cholesterolesterase -Zymogen -Activator -Action |
none none Releases cholesterol from other molecules
|
|
|
Ribonuclease -Zymogen -Activator -Action |
None None Cleaves RNA
|
|
|
Deoxyribonuclease -Zymogen -Activator -Action |
None none cleaves DNA |
|
|
What are the 4 reasons why the pancreas doesn't auto-digest? |
1. Synthesis of enzymes as inactive zymogens 2. Segregation of enzymes in membrane bound components (vacuoles) 3. Trypsin inhibitor packaged in zymogen granules 4. enterokinases on the intestine |
|
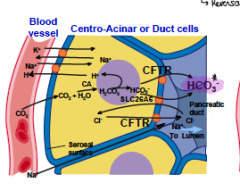
How does the Pancreas secrete HCO3-? (sorry for the length) |
1. Carbonic anhydrase catalyzes the conversion of CO2+H2O to form carbonic acid 2. Carbonic acid dissociate to H+ + HCO3- 3. Na+ H+ exchanger at basolateral membrane extrudes H+ 4. HCO3- Cl- exchanger (apical) secretes HCO3- in exchange for Cl- 5. Cl- efflux leads to K efflux (basolateral) to maintain neutrality and Na+ transport (Na,K ATPase replenishes K and maintains Na) 6. HCO3- and Na+ ions into lumen causes osmotic gradient and water moves from blood to pancreas!
|
|
|
What is the HCO3- Cl- exchanger controlled and regulated by? |
Cl- efflux though the Cl-s channel that is regulated by SECRETIN! |
|
|
What are the 3 phases of pancreatic secretion? |
Cephalic Gastric Intestinal |
|
|
Cephalic phase -Stimulant? -Regulatory pathway ? -Enzyme Secretion (%max) ? |
-Anticipation, sight, smell, mastication, taste -Vagal -25% |
|
|
Gastric phase... -Stimulant? -Regulatory pathway ? -Enzyme Secretion (%max) ? |
Distension Vagal 10-20% |
|
|
Intestinal Phase... -Stimulant? -Regulatory pathway ? -Enzyme Secretion (%max) ? |
-Oligopeptides, essential AA, FA, gastric acid -Vagal, enteropancreatic reflexes, CCK, Enzyme secretion -50-80% |
|
|
Regulation of Pancreatic secretion.... (steps) |
1. Intestinal phase (major contributor) stimulated by intraluminal acidity, oligopeptides, AA, & FA 2. S cells release Secretin & I cells release CCK 3. CCK and Secretin mediate pancreatic secretion
|
|
|
How does CCK and Secretin mediate pancreatic secretions? |
1. Vago-Vagal reflex -vagal afferent activates dorsal vagal complex -vagal efferents (Ach) activate enteric neutrons releasing Ach, VIP, GRP = pancreatic exocrine secretion of CCK (acinar cells) & secretin (ducts) 2. Endocrine (hormonal) : blood to brain then vagal efferents to pancreas 3. Endocrine (hormonal) : blood to pancreas |
|
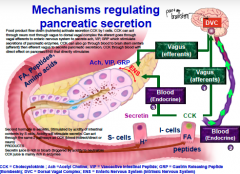
Mechanisms regulating pancreatic secretions... (steps) |
1. Food product activates secretion of CCK by I cells (FA, peptides) and Secretin by S cells (H+) 2. CCK and Secretin act on... -neuro roots to stimulate release of Ach, VIP, GRP -go through blood to brain then vagus -go though blood straight to pancreas (ENS) to release pancreatic enzymes
|
|
|
What are the clinical signs for Exocrine pancreatic Insufficiency?
**common in german shepherds and rough coated collies |
-Yellowish/grey, loose feces -increased fecal volume and frequency -weight loss -flatulence - increase appetite -occasional coprophagia |
|
|
What are the pancreatic function tests? |
-Serum trypsin like immunoreactivity -Decrease fecal proteolytic activity -Decreased elastase activity
|

