![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
24 Cards in this Set
- Front
- Back
|
Your patient is a 40-year-old woman with a severe attack of diarrhea that began on the airplane while she was returning from a vacation in the Middle East. She had had multiple episodes of watery, nonbloody diarrhea and little vomiting. She is afebrile. A stool culture reveals only lactose-fermenting colonies on EMB agar. Of the following, which one is the MOST likely cause?
A. Shigella sonnei B. Helicobacter pylori C. Escherichia coli D. Pseudomonas aeruginosa |

C. Escherichia coli
*Only one that ferments lactose *Test aids in the identification of pathogens among normal flora. *Most enteric bacteria ferment lactose including E. coli--> show up red. *Primary enteric pathogens (i.e Shigella, Salmonella, and Yersinia) are unable to ferment lactose. *Employs Eosin-methylene blue (EMB) or MacConkey’s agar |
|
|
Your patient is a 70-year-old man who underwent bowel surgery for colon cancer 3 days ago. He now has a fever and abdominal pain. You are concerned that he may have peritonitis. Which one of the following pairs of organisms is MOST likely to be the cause?
A. Bacteroides fragilis and Klebsiella pneumoniae B. Bordetella pertussis and Salmonella enteritidis C. Actinomyces israelii and Campylobacter jejuni D. Clostridium botulinum and Shigella dysenteriae |
A. Bacteroides fragilis and Klebsiella pneumoniae
*Both normal inhabitants of normal flora; if colon is perforated, they can cause opportunistic infection --> sepsis, abscesses, polymicrobial infections. Anaerobic. |
|
|
Hand washing is an important means of interrupting the chain of transmission from one person to another. Infection by which one of the following bacteria is most likely to be interrupted by hand washing?
A. Legionella pneumophila B. Staphylococcus aureus C. Streptococcus agalactiae (Group B streptococcus) D. Treponema pallidum (syphilis) |
B. Staphylococcus aureus
|
|
|
A 25-year-old man with abdominal pain was diagnosed with acute appendicitis. He then had a sudden rise in temperature to 39°C and a sudden fall in blood pressure. Which one of the following is the most likely cause of the fever and hypotension?
A. An exotoxin that ADP-ribosylates elongation factor-2 B. An exotoxin that stimulates production of large amounts of cyclic AMP C. An endotoxin that causes release of tumor necrosis factor D. An endotoxin that binds to class I MHC protein E. An exoenzyme that cleaves hyaluronic acid |
C. An endotoxin that causes release of tumor necrosis factor
*A PRO-inflammatory cytokine. |
|
|
A 24-year-old man, an automobile accident victim, was brought to the hospital with a compound fracture of the distal left tibia and fibula. Within 6 hours of the accident, the patient was taken to surgery where the wound was debrided, the leg was immobilized, and therapy was begun (cephalothin sodium IV, 1 g/4 hr). The patient was afebrile.. He did well until the fourth postoperative day when he was noted to have a temperature of 38.3°C orally, a tachycardia rate of 120 bpm, a painful left leg, and a sense of impending doom. The cast was opened and the entire lower leg was found to be swollen and reddish-brown, and was exuding a serosanguineous foul-smelling discharge. Crepitations were palpable over the anterior tibial and entire gastrocnemius areas. His blood pressure became unstable and then dropped to 70/20 mm Hg. Gram stain of an aspirate from the gastrocnemius demonstrated both Gram-negative and Gram-positive rods, but no spores were seen. At this time, the hematocrit reading had decreased to 35%, and WBC count was 12,000/mm3, with 85% polymorphonuclear leukocytes. Therapy was begun with IV penicillin G aqueous, 5 million units every 6 hours. The man was taken to surgery, where an above-knee amputation was performed. Cultures of the necrotic muscle grew Escherichia coli and Clostridium perfringens. Within 3 hours after amputation, the patient had a sense of well-being, and complete recovery followed. The injury in the tissue is produced by which of the following:
A. ADP-ribosylating toxin B. Lecithinase -toxin C. Pore-forming -toxin D. Enterotoxin E. Spores |
B. Lecithinase -toxin
*Could be the alpha toxin of c. perfringens; it produces at least a dozen exotoxins. |
|
|
Unique pathogenic factors for pseudomonas?
|
-Secrete multiple pigments
-Can live with minimal nutritional requirements |
|
|
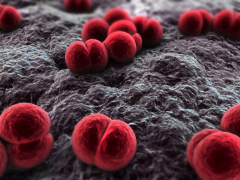
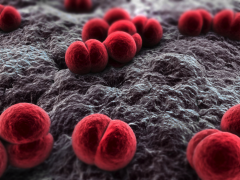
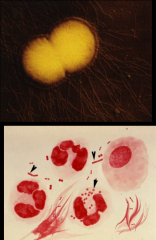
Neisseriaceae. *Aerobic, Gram-negative diplococci.
|
|
|
Key points about Neisseriaceae:
|
*Aerobic, Gram-negative diplococci.
*Pathogenic species: Neisseria meningitidis Neisseria gonorrhoeae *Outer membrane contains Lipooligosaccharide (LOS)– a variant of LPS. This is an important virulence factor. *Oxidase positive and grow on chocolate agar. |
|
|
Neisseriaceae. *Aerobic, Gram-negative diplococci.
|
|
|
Describe the role of chocolate agar in Neisseriaceae:
|

-Must be grown on Thayer-Martin plates. It's a selective media and is necessary to select for Neisseria. Contains antimicrobials that kill everything else but Neisseria.
|
|
|
How does Neisseria get inside us and enter the bloodstream?
|

1. Attach (pili and OMPs)
2. Endocytosed and multiply in cytoplasm. 3. Both are transcytosed through the cell into subepithelial space to establish infection. 4. Gonococcus remains localized; meningococcus enters bloodstream. *TNF-a is secreted and promotes inflammation--> symptoms. Acute inflammatory response. *gonorrhea enters in the urethra; stays localized *meningitidis enters in the resp. tract.; spreads (has capsule and is resistant to phagocytosis) |
|
|
Describe the encounter and entry of Neisseria gonorrhoeae as well as its virulence factors:
|
*Encounter and Entry
-Obligate human pathogens; all are sexually acquired. -Pili and Opa proteins mediate attachment to nonciliated mucosal epithelial cells of distal urethra (males) or cervix (female), eye, rectum, and throat. *Virulence factors -IgA protease -Serum resistance through LOS sialylation -Catalase production (deals with ROS generated by neutrophils) -Antigenic variation (on pili) |
|
|
Types of antigenic variation in Neisseria gonorrhea:
|
1. Phase Variation
2. Gene Conversion |
|
|
Describe phase variation and gene conversion in neisseria gonorrhea:
|
*Phase Variation: gene is moved into a locus where translational reading frame is shifted; genes get turned “on” and “off”. Pilin and Opa protein genes undergo phase variation.
*Slipped strand mispairing *Gene Conversion: most evident in pilin genes. Allows pili to be expressed (pilE) or silent (pilS) because they lack transcriptional promoter elements. By shuffling and recombining chromosomal regions of these genes, a single strain can at different times express multiple pilins that are antigenically variant. |
|
|
Describe the damage that occurs in neisseria gonorrhea:
|
*Tend to remain localized to genital structures.
*Damage is immune mediated by inflammatory response and release of TNF-a. - Responsible for local symptoms such as dysuria and urethral discharge of pus (copious, thick, and greenish yellow, with intense pain). *95% of infected men have acute symptoms; complications are rare but can include epididymitis, prostitis, and periurethral abscesses. *Women with gonococcal cervicitis are more often asymptomatic, but can experience dysuria, painful intercourse, abdominal pain and vaginal discharge. |
|
|
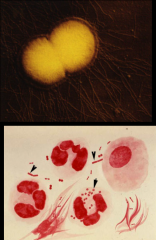
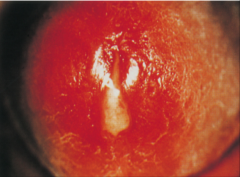
*Neisseria gonorrhoeae
*Purulent urethral discharge in man with urethritis |
|
|
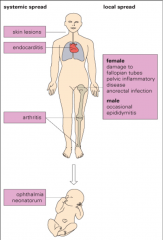
Describe Local Spread, Chronic Infection, and Systemic Illness in neisseria gonorrhea:
|
*Local Spread: Important in women; infection of fallopian tubes, i.e. salpingitis. Occurs in > 15% of untreated cases. Organism is non-motile but may be able to attach to sperm. Local spread may also be due to reflux of menstrual blood, urethral or uterine contractions.
*Chronic Infection: Can lead to scarring, PID. Common cause of infertility and ectopic pregnancy. Early treatment critical. *Systemic Illness: 1-3% suffer bacteremia; breaches epithelial barrier and then becomes exocytosed into subepithelial layer; gains access to blood, can then spread to skin and joints. |
|
|
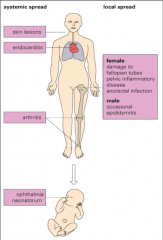
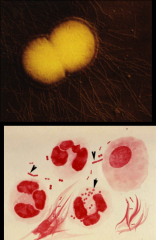
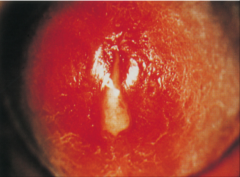
*Systemic spread from n. gonorrhea
*Not good! Could be key to diagnosis |
|
|
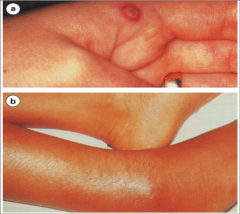
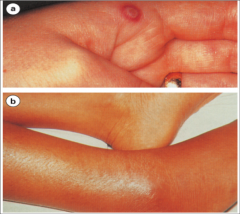
a. Skin lesions of disseminated gonoccocal infection with a necrotic, grayish central lesion on an erythematous base.
b. Purulent arthritis |
|

|

Gonococcal ophthalmia neonatorum. Lid edema, erythema, and marked purulent discharge are seen. A Gram-stained smear would reveal abundant organisms and inflammatory cells.
|
|
|
Key points about n. meningitidis:
|
*Causes meningitis and septicemia.
*Carried asymptomatically in nasopharyngeal flora of 10% of healthy individuals and serve as a source of infection to others. Organisms are transmitted by airborne droplets. *From the nasopharynx, the organism can enter the bloodstream and spread to specific sites, such as the meninges or joints, or be disseminated throughout the body (meningococcemia). *Can be heavily encapsulated, which allows them to multiply and disseminate in the bloodstream. *Can be prevented with vaccines containing capsular polysaccharide (EXCEPT FOR group B strains; group B strains aren't antigenic). |
|
|
Key virulence factors for n. meningitidis:
|
*A polysaccharide capsule that enables the organism to resist phagocytosis by neutrophils.
*Endotoxin, which causes fever, shock, and other pathophysiologic changes. *An IgA protease helps the bacteria attach to the membranes of the upper respiratory tract by cleaving secretory IgA. |
|
|
The most important manifestations of disease in n. meningitidis:
|
*Meningococcemia
*Meningitis. *The most severe form of meningococcemia is Waterhouse-Friderichsen syndrome --> DIC, septic sx. |
|

|

*Meningococcemia. Note purpuric lesions on leg caused by endotoxin-mediated disseminated intravascular coagulation (DIC)
|

