![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
106 Cards in this Set
- Front
- Back
|
What structures pass through the obturator canal? |
Obturator membrane forms the canal. Obturator nerve, artery, vein. |
|
|
Which structures pass through the greater sciatic foramen? |
* Sciatic Nerve:
* Superior Gluteal Nerve: * Inferior Gluteal Nerve: * Pudendal Nerve: * Posterior Femoral Cutaneous Nerve * Nerve to Quadratus Femoris * Nerve to Obturator Internus * Superior Gluteal Artery & Vein * Inferior Gluteal Artery & vein * Internal Pudendal Artery & vein * Piriformis |
|
|
Which structures pass through the lesser sciatic foramen? |
* the tendon of the Obturator internus
* internal pudendal vessels * pudendal nerve * nerve to the obturator internus |
|
|
What form the walls of the pelvis? |
Anterior Wall Shallow and formed by the pubic bones and the pubic symphysis
Lateral Wall The sacrospinous ligament covered by the coccygeus muscle and the obturator internus muscle. This is a lateral rotator of the thigh which originate from around the internal aspect of the obturator foramen and passes to the greater trochanter of the femur
Posterior Wall Formed by the sacrum, the coccyx and by the piriformis muscles and their covering of fascia. |
|
|
Give features of the piriformis muscle? |
The piriformis muscle originates from the anterior (front) part of the sacrum, the part of the spine in the gluteal region, and from the superior margin of the greater sciatic notch (as well as the sacroiliac joint capsule and the sacrotuberous ligament). It exits the pelvis through the greater sciatic foramen to insert on the greater trochanter of the femur. Its tendonoften joins with the tendons of the superior gemellus, inferior gemellus, and obturator internus muscles prior to insertion. |
|
|
What form the pevlic part of the sympathetic trunk? |
The pelvic part of sympathetic trunk runs behind the rectum on the anterior surface of the sacrum, medial to the sacral foramina. Its branches are i. Gray rami communicantes (which join spinal nerves and are distributed to the periphery ii. Fibres the join the hypogastric plexus |
|
|
Where do preganglionic parasympathetic fibres originate in the pelvis? |
Pelvic splanchnic nerves arise from S2-4 Emerge from anterior rami of sacral spinal nerves
From there, they contribute to the innervation of the pelvic and genital organs. The nerves regulate the emptying of the urinary bladder, control opening and closing of the internal urethral sphincter, influence motility in therectum as well as sexual functions like erection
They contain both preganglionic parasympathetic fibers as well as visceral afferent fibers. |
|
|
Describe the superior and inferior hypogastric plexi. |
Some of the fibres ascend through both the inferior and then the superior hypogastric plexus to the inferior mesenteric plexus →hindgut. * The superior hypogastric plexus is anterior to the sacral promontory. It is a continuation of the aortic plexux and L3 and L4 sympathetic ganglia. It contains sympathetic, sacral parasympathetic (ascending) and visceral afferent fibres. The hypogastric plexus divides inferiorly to form the right and left hypogastric nerves.* The inferior hypogastric plexuses lie on either side of the rectum. Each plexus is formed by a hypogastric nerve (from the superior plexus) and from the pelvic splanchnic nerves. |
|
|
What is the hindgut? |
it includes the distal third of the transverse colon and the splenic flexure, the descending colon, sigmoid colon (sigmoid arteries of IMA) and rectum.
The lymph travels to nodes along the course of the inferior mesenteric artery (inferior mesenteric nodes). The nerve supply is autonomic from the hypogastric plexus. |
|
|
What is volvulus? |
Volvulus: Because of its mobility, the sigmoid colon can rotate around its mesentery. This may correct itself spontaneously, or the rotation may continue until the blood supply to the sigmoid colon is completely shut off. The rotation commonly occurs clockwise and is referred to as a volvulus. |
|
|
What are features of the sigmoid colon? |
The sigmoid colon shows a great variation in length and may measure as much as 91cm. In a young child (because the pelvis is small), this segment of the colon may lie mainly in the abdomen. The sigmoid colon is a common site for cancer of the large bowel. Because the lymphatic vessels drain to inferior mesenteric nodes, an extensive resection of the gut and its associated lymphatics is necessary. The colon is removed from the left colic flexure to the distal end of the sigmoid colon, and the transverse colon is anastomosed with the rectum. |
|
|
Describe the position of the rectum? |
The rectum is about 13cm long and begins anterior to the 3rd sacral vertebra as a continuation of the sigmoid colon. It passes inferiorly, following the curve of the sacrum and coccyx, and ends at the tip of the coccyx by piercing the pelvic diaphragm and becoming continuous with the anal canal. The lower part of the rectum is dilated to form the rectal ampulla. The peritoneum covers the anterior and lateral surfaces of the first third of the rectum, and only the anterior surface of the middle third, leaving the lower third devoid of peritoneum. |
|
|
What are the 3 arteries that supply the rectum? |
* The superior rectal artery is a direct continuation of the inferior mesenteric artery.
* The middle rectal artery is a small branch from the internal iliac artery. * The inferior rectal artery is a branch of the pudendal artery. It anastomoses with the middle rectal artery at the anorectal junction. |
|
|
What are the branches of the anterior and posterior divisions of the internal iliac artery? |
Anterior division → Umbillical →artery to vas deferens (male), superior vesical artery Obturator Inferior vesical Middle rectal Inferior gluteal Uterine (female) Vaginal (female)
Posterior Division → Iliolumbar lateral sacral superior gluteal |
|
|
Label the branches of the internal iliac. |
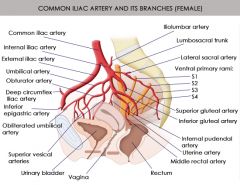
|
|
|
What 2 main muscles make up the pelvic floor? |
levator ani, the coccygeus muscle |
|
|
Which muscles make up the levator ani muscle? |
* Iliococcygeus muscle
* Pubococcygeus muscle * Puborectalis muscle |
|
|
Describe a sagittal view of the pelvic floor? |
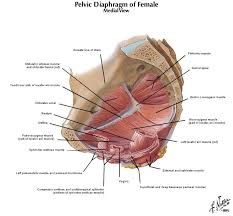
|
|
|
What is involved in involuntary losses of urine after increases in intra-abdo pressure? |
Involuntary loss of urine after an increase in intra-abdominal pressure is often associated with weakening of supporting structures involving the uterus and bladder including: * Medial and lateral pubovesical ligaments* Pubovesical fascia at the ureterovesical junction * Levator ani * Functional integrity of the urethral sphincter |
|
|
What forms the recto vaginal septum? |
* anterior pelvi wall (pubocervical ligament)
* lateral pelvic wall (transverse cervical or cardinal ligament) * posterior pelvic wall (uterosacral ligament) |
|
|
Describe the apex and base of the bladder. |
The apex of the bladder is directed towards the top of the pubic symphysis, a structure known as the median umbilical ligament (a remnant of the embryological urachus), and continues from it superiorly up the anterior abdominal wall to the umbilicus.
The base of the bladder is shaped like an inverted triangle and faces posteroinferiorly. The two ureters enter the bladder at each of the upper corners of the base and the urethra drains inferiorly from the lower corner of the base. Inside, the mucosal lining on the base of the bladder is smooth and firmly attached to the underlying smooth muscle coat of the wall- unlike elsewhere in the bladder where the mucosa is folded and loosely attached to the wall. The smooth triangular area between the openings of the ureters and urethra on the inside of the bladder is known as trigone. |
|
|
Describe the inferolateral and neck of the bladder. |
The inferolateral surfaces of the bladder are cradled between the levator ani muscles of the pelvic diaphragm and the adjacent obturator internus muscle.
The neck of the bladder surrounds the origin of the urethra. The neck is the most inferior part of the bladder and also the most ‘fixed’ part. It is anchored into position by a pair of tough fibromuscular bands (in women= pubovesicular ligaments), which connect the neck and the pelvic part of the urethra to the posteroinferior aspect of each pubic bone. Together with the perineal membrane and associated muscles, the levator ani muscles and the pubic bones, these ligaments help support the bladder. |
|
|
Describe the position of the bladder. |
Although the bladder is considered to be pelvic in the adult, it has a higher position in children. At birth, the bladder is almost entirely abdominal. |
|
|
Describe the sacral innervation of the perineum. |
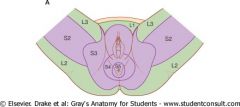
Most of the skeletal muscles contained in the perineum and pelvic floor, including the external anal sphincter and external urethral sphincter, are innervated by spinal cord levels S2-S4. Much of the somatic motor and sensory innervation of the perineum is provided by the pudendal nerve from spinal cord levels S2-S4. The ischial spine can be palpated transvaginally in women and is the landmark for administrating a pudendal nerve block. |
|
|
Describe the lymphatic drainage of the pelvis. |
Lymphatics from most pelvic viscera drain mainly into lymph nodes distributed along the internal iliac artery and their associated branches, which drain into nodes associated with common iliac arteries and then into the lateral aortic and lumbar nodes associated with the lateral surfaces of the abdominal aorta. These lateral aortic and lumbar nodes drain into lumbar trunks and continue to form the origin of the thoracic duct at the level to T12.
Lymphatics for the ovaries and uterine tubes leave the pelvic cavity superiorly and drain, via vessels that accompany the ovarian arteries, directly into the lateral aortic and lumbar nodes, unlike the rest of the pelvic viscera.
A few lymph vessels follow the round ligament of the uterus through the inguinal canal and drain to the superficial inguinal nodes. |
|
|
Describe the female pelvic floor inferiorly. |
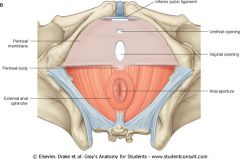
|
|
|
What does the deep perineal pouch contain? |
The deep perineal pouch contains: * Proximal part of the urethra* A mass of smooth muscle (in place of deep transverse perineal muscle in men) * Dorsal neurovasculature of the clitoris |
|
|
What does the superficial perineal pouch contain? |
* Clitoris and associated muscle (ischiocavernosis)
* Bulbs of the vestibule and surrounding muscle (bulbospongiosis) * Greater vestibular glands * Deep perineal branch of internal pudendal vessels and nerve * Superfiscial transverse perineal muscle The perineal body marks the posterior border of the urogenital triangle and is an ill-defined but important connective tissue structure into which muscles of the pelvic floor and the perineum attach. It is posterior in the midline along the posterior border of the perineal membrane, to which it attaches. The deep transverse perineal muscles intersect at the perineal body. |
|
|
Describe the vagina and clitoris. |
The internal end of the canal is enlarged to form a region called the vaginal vault. The urethra is fused with the anterior wall of the vagina, and posteriorly the vagina is related to the rectum. The vaginal wall is normally collapsed so that the anterior wall is in contact with the posterior wall. The vaginal fornix is the recess of the margin of the cervix and the vaginal wall.
The clitoris is composed to two corpora cavernosa and the glans clitoris. The attached part is formed by the root of the clitoris and technically consists only of the two crura. The body of the clitoris is formed by an unattached part of the two corpora cavernosa, angles posteriorly and is embedded in the connective tissue of the perineum. The bulbs of the vestibule are attached to the glans clitoris by thin bands of erectile tissue. |
|
|
Describe the nervous innervation to the vagina and clitoris |
Stimulation of parasympathetic fibres carried by splanchnic nerves from the anterior rami (S2-S4, which enter the inferior hypogastric plexus) cause specific arteries in the corpora cavernosa to relax, allowing blood filling and clitoral erection. Arteries supplying the clitoris are branches of the internal pudendal artery, and general sensory information is carried by the pudendal nerve (S2-S4). |
|
|
Describe the female reproductive glands. |
Posterior to the bulb of the vestibule lie small, pea-shaped mucous glands on each side of the vaginal opening. These glands (the greater vestibular glands) are homologues of the bulbourethral glands in men. In women, however, they are located in the superficial perineal pouch. Like the bulbourethral gland in men, the greater vestibular gland produces secretion during sexual arousal. The duct of each greater vestibular gland opens into the vestibule of the perineum along the posterolateral margin of the vaginal opening. |
|
|
How are the female genitalia examined? |
Careful examination of the external genitalia (vulva) is first. The labia majora and minora are separated and the area inspected for anatomical anomalies, discharge and genital warts. A speculum is then carefully inserted into the vagina with the handle at 6 or 9 o’clock. As the speculum is inserted it is rotated 90 degrees and the blades are parted. Once the speculum has been fully inserted it allows good visualisation of the cervix, vaginal fornices and the external os of the uterus. |
|
|
How are pap smears carried out? |
A ‘pap’ smear tests for pre-malignant cervical lesions. This has been a successful screening program in the UK which is offered to all ladies between the ages of 25 and 64. Human papillomavirus is the cause of cervical cancer in almost all cases.Once all swabs and smears have been taken the speculum is removed slowly, inspecting the walls of the vagina for evidence of prolapse from either anterior (cysto or urethrocele) or posterior (recto- or enterocele). |
|
|
How is a bimanual technique employed? |
A bimanual technique can employed to examine the uterus and adnexae. Firstly the index and middle finger are placed in the posterior fornix of the vagina. Gentle anterior pressure is then placed on the cervix and with the other hand the fundus of the uterus is palpated in the suprapubic region. The right and left iliac fossae are then palpated to feel for the ovaries however they are impalpable unless pathological. |
|
|
What are fibroids? |
Fibroids are the most common benign tumours in women. They are benign tumours of uterine smooth muscle (myometrium) and also of the surrounding connective tissue. They are largely asymptomatic, however, they can grow to be large causing dysmennorhoea, mennorhagia, painful sexual intercourse, urinary frequency and urgency. |
|
|
Where do fibroids occur? |
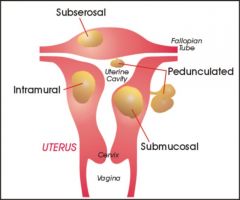
|
|
|
What is the risk of fibroid malignancy? |
Uterine fibroids have a very low risk of malignant transformation, approximately 1 in 1000, and there is no consensus between pathologists as to which is more likely to transform. Fibroids tend to be slow growing, however, continued or rapid growth particularly after menopause is a suspicious symptom. |
|
|
What are features of uterine prolapse? |
Occurring in women of all ages, it is more common as women age, particularly in those who have delivered large babies or had exceedingly long pushing phases of labour. Prolapse is more likely to occur with age as the supporting structures of the pelvic organs in females are less strong post-menopause as levels of oestrogen are lower. Smoking, obesity, connective tissue disorders, upper respiratory disorders and repetitive strain injuries can all increase prolapse risk. Why do you think constipation, smoking, obesity and respiratory tract infections increase the risk of prolapse? |
|
|
What are the 6 types of uterine prolapse? |
There are many types of prolapse 1. Uterine prolapsed2. Cystocele – bladder into vagina 3. Rectocele – rectum into vagina 4. Enterocele – small bowel into vagina 5. Urethrocele – urethra into vagina 6. Vaginal vault – post hysterectomy |
|
|
What are the stages of uterine prolapse? |
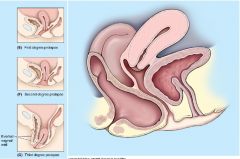
|
|
|
How is uterine prolapse sensed and treated? |
Females often feel a sense of ‘dragging’ or pressure within the vagina, or pain during intercourse. However, thereafter symptoms vary depending on the severity of the prolapse and the organ prolapsed. Difficulty passing stool, constipation and even faecal incontinence are symptoms of a rectocele. Incomplete emptying of the bladder and stress incontinence are symptoms of cysto- and uretroceles.
Treatment varies with symptom severity, degree of prolapse and suitability of the patient for surgery. Often patients require no treatment, however, ring pessaries (some of which secrete oestrogen) are an option for moderate symptom severity, and surgery is reserved for more severe prolapses or symptoms. |
|
|
What is stress incontinence? |
Stress incontinence is the loss of small volumes of urine during coughing, laughing, straining or exercising. Any activity that increases intra-abdominal pressure results in pressure being transmitted downwards onto the bladder. During sudden increases in intra-abdominal pressure the pelvic floor muscles and external sphincter contract to prevent urine leakage. Physical changes from pregnancy, childbirth and menopause all contribute to weakened pelvic floor muscles and thus increase risk of urine leakage.
Treatment ranges from lifestyle changes to surgery. Weight loss and pelvic floor exercises are first line treatments. Pessaries act to elevate the bladder neck and compress the urethra against the posterior aspect of the pubic symphisis. Surgery varies, but all aim to restore normal pressure transmission during periods of increased intra-abdominal pressure. |
|
|
What is the spermatic cord? |
The spermatic cord is the tube-shaped connection between the pouch in the scrotum and the abdominal wall. The sides and anterior aspects of the testis are covered by a closed sac of peritoneum (tunica vaginalis), which originally connected to the abdominal cavity. Normally after testicular descent, the connection closes, leaving a fibrous remnant. Each testis is composed of seminiferous tubules and interstitial tissue surrounded by a thick connective capsule (tunica albuginea). |
|
|
Where are spermatozoa made? |
Spermatozoa are produced by the highly coiled seminiferous tubules. These tubules become straight tubules and connect to a collection chamber (rete testis), projecting from the capsule into the posterior aspect of the gonad. Approximately 12-20 efferent ductules originate from the upper end of the rete testis, penetrate the capsule and connect with the epididymis. |
|
|
Where is testicular pain referred to? |
Abdomen and inguinal canal |
|
|
What is the vertebral level of the origin of the testicular artery? |
L2 |
|
|
Name the plexus of veins which is adjacent to the testes.
How is this plexus involved in regulating the testicular temperature?
Which vein drains the testis? Into which vessels do the testicular veins drain? |
Pampiniform venous plexus - union of multiple spermatic veins from the back of testis and tributaries
Heat exchanger - cools blood in adjacent arteries.
Enlargement = varicocele
Drains into testicular vein, which drains to IVC (R) and left renal vein (L)
|
|
|
What is the epididymis? |
The epididymis is a single, long coiled duct that courses along the posterolateral side of the testis, and consists of: * The efferent ductules (head of epididymus)* The true epididymus (body and tail of epididymus) During passage through the epididymus, spermatozoa acquire the ability to move and fertilize an egg, and are stored here until ejaculation. The end of the epididymus is continuous with the vas deferens. |
|
|
What is the ductus deferens |
The ductus deferens is a long muscular duct that transports spermatozoa from the tail of the epididymus in the scrotum to the ejaculatory duct in the pelvic cavity/prostate. It ascends as a component of the spermatic cord and passes through the inguinal canal in the anterior abdominal wall over and behind the bladder to the prostate. |
|
|
What are the 3 layers of the abdominal wall? |
Before the descent of the testis and ovaries from their initial position high in the posterior abdominal wall, a peritoneal outpouching (the processus vaginalis) forms, passing through the various layers of the anterior abdominal wall and acquiring coverings from each layer: * The transversalis fascia (deepest covering)* Musculature of the internal oblique (second covering) * Aponerosis of the external oblique (most superfiscial covering) |
|
|
How is the inguinal canal formed? |
As a result the processus vaginalis is transformed into a tubular structure, forming the inguinal canal. The final event of this development is the descent of the testes into the scrotum (or ovaries into the pelvic cavity). This process depends on the development of the gubernaculums, which extends from the inferior border of the developing gonads to the labioscrotal swellings. |
|
|
Describe the descent of the testes? |
As the testes descend, the testes and their accompanying vessels, ducts and nerves pass through the inguinal canal and are therefore surrounded by the same fascial layers of the abdominal wall. Testicular descend completes the formation of the spermatic cord in men. The development sequence is concluded in both sexes when the processus vaginalis obliterates. If this does not occur, a potential weakness exists and an inguinal hernia may develop. |
|
|
What are the structures in the spermatic cord? |
* The ductus deferens
* The artery to ductus referens * The testicular artery * The testicular veins (pampiniform plexus of veins) * The cremasteric artery and vein * The genital branch of the genitofemoral nerve (to cremaster muscle) * Sympathetic and visceral afferent nerve fibres * Lymphatics * The remnants of the processus vaginalis * |
|
|
Describe the anatomy of the spermatic cord. |

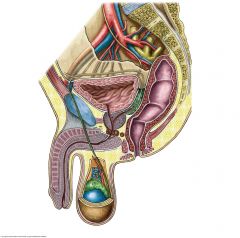
|
|
|
What is the function of the sympathetic fibres in the spermatic cord (why are there no parasympathetic fibres in the spermatic cord)? |
??? |
|
|
Describe the inguinal canal. |
The inguinal canal is a slit-like passage that extends downwards and medially, above and parallel to the inguinal ligament. It begins at the deep inguinal ring and continues for 4 cm, ending at the superficial ring. Besides the spermatic cord, part of the canal is also occupied by the ilio-inguinal nerve from the lumbar plexus. |
|
|
What does the fascia enclosing the content of the spermatic cord include? |
The fascia enclosing the content of the spermatic cord below the superficial ring include: * Internal spermatic fascia (deepest layer arising from the transversalis fascia, and its margins are attached to the deep inguinal ring)* Cremasteric fascia with the associated cremasteric muscle (arising from the internal oblique muscle) * External spermatic fascia (most superficial layer covering the spermatic cord, arising from the aponerosis of the external oblique, and attached to the margins of the superficial inguinal ring) |
|
|
Which arteries lie medial to the deep inguinal ring? |
Inferior epigastric arteres |
|
|
What structures of the abdominal wall are associated with the superficial inguinal ring and the deep inguinal ring? |
Superficial - within the aponeurosis of the external oblique.
|
|
|
What is an indirect hernia? |
An inguinal hernia is a protrusion or passage of a peritoneal sac, with or without abdominal contents, through a weakening of the abdominal wall in the groin. It occurs because the peritoneal sac enters the inguinal canal either: * Indirectly, through the deep inguinal ring (already existing weakness)* Directly, through the posterior wall of the inguinal canal (new opening) Indirect inguinal hernias occur because some part, or all, of the embryonic processus vaginalis remains open or patent (congenital in origin), and is therefore more common in men than in women. Protruding peritoneal sac enter the deep inguinal ring, therefore LATERAL to the inferior epigastric artery. Its protrusion depends on the amount of the processus vaginalis that remains patent. |
|
|
Where does a direct inguinal hernia enter? |
A direct inguinal hernia enters the medial end of the canal (MEDIAL to the inferior epigastric artery). It is usually described as acquired (in mature men), because it develops when abdominal musculature has been weakened. It is defined by the Hesselbach triangle |
|
|
What are the boundaries of the Hesselbach triangle? |
* Medial border: Lateral margin of the rectus sheath, also called linea semilunaris
* Superolateral border: Inferior epigastric vessels * Inferior border: Inguinal ligament, sometimes referred to as Poupart's ligament |
|
|
Define the following terms: 1. Varicocele2. Hydrocele 3. Hematocele 4. Testicular Torsions |
1. A varicocele is an abnormal enlargement of the pampiniform venous plexus in the scrotum. This plexus of veins drains the testicles. The testicular blood vessels originate in the abdomen and course down through the inguinal canal as part of the spermatic cord on their way to the testis. Upward flow of blood in the veins is ensured by small one-way valves that prevent backflow.
2. A hydrocele testis is the accumulation of fluids around a testicle, and is fairly common. It is often caused by fluid secreted from a remnant piece of peritoneum wrapped around the testicle, called the tunica vaginalis.
3. A hematocele is a collection of blood in a body cavity. The term is generally used to refer to the collection of blood in the tunica vaginalis around thetesticle. Hematoceles are often more painful than ahydrocele
4.Testicular torsion occurs when the spermatic cord(from which the testicle is suspended) twists, cutting off the testicle's blood supply, a condition calledischemia. The principal symptom is rapid onset oftesticular pain. The most common underlying cause is a congenital malformation known as a "bell-clapper deformity" wherein the testis is inadequately affixed to the scrotum allowing it to move freely on its axis and susceptible to induced twisting of the cord and its vessels. |
|
|
What is a vasectomy? |
The common method of sterilizing males is deferentectomy, popularily called a vasectomy. During this procedure, part of the ductus deferens is ligated and/or excised through an incision in the superior part of the scrotum. Hence the ejaculatory fluid from the seminal glands, prostate and bulbourethral glands contains no sperm. |
|
|
Why are indirect hernias more common in baby boys? |
Patent processus vaginalis more common right side later descent right testes |
|
|
Finish this sentence: The vas deferens begins at the tail of the epididymis, at the ………………….. pole of the testis. It ascends to the testis medial to the epididymis. It then becomes the primary component of the spermatic cord and then enters the abdominal cavity via the …………………….... canal. The vas then crosses the ………………. iliac vessels, passing around the lateral wall of the pelvis and then between the ……………………….. and bladder. At the posterior aspect of the bladder it lies ………….....……….. to the seminal vesicles and joins the duct from the seminal vesicle to form the ejaculatory duct. The arterial supply of the vas deferens usually arises from the superior vesical artery. |
|
|
|
The superior vesicular artery is a branch of which main artery? |
Umbilical artery/ anterior trunk of internal iliac
|
|
|
Describe the seminal vesicles |
The seminal vesicle glands are two elongated structures approximately 5cm long that lie between the bladder and rectum. They are obliquely placed superior to the prostate and secrete a thick alkaline fluid. The fluid contains high levels of fructose, that provide energy for sperm, and also a coagulation agent which mixes with the sperms as they pass into the ejaculatory ducts of the urethra. The arterial supply of the seminal vesicles arises from the inferior vesical and middle rectal arteries. |
|
|
What is the prostate? |
The prostate gland is a walnut-sized gland and is the largest accessory gland of the male reproductive system. It is divided into glandular part, making up two-thirds of the prostate, and a fibromuscular part. It has a dense fibrous capsule which contains the plexuses of prostatic nerves and veins. Its surfaces and relations are as follows: * Base: neck of the bladder * Apex: fascia on the superior surface of the urethral sphincter and deep perineal muscles * Muscular anterior surface: retropubic space and pubic symphisis * Posterior: ampulla of the rectum * Inferolateral: levator ani |
|
|
Where do the ejaculatory and prostate ducts open? |
The ejaculatory ducts pass anteroinferiorly through the glandular part of the prostate. They open into the prostatic urethra through two slit like openings either side of the prostatic utricle. The prostatic ducts (20 to 30) open through prostatic sinuses which lie lateral to the seminal colliculus. Prostatic fluid accounts for approximately 20% of the volume of semen. |
|
|
What are the divisions of the male urethra?
|
Pre-prostatic 0.5-1.5cm Vertical through the neck of the bladder Surrounded by internal urethral sphincter. Prostatic 3-4cm Descends through anterior prostate Widest and most dilatable, ejaculatory ducts, prostatic utricle and prostatic sinuses open into. Membranous (Intermediate) 1-1.5cm Through deep perineal pouch Surrounded by circular fibres of external urethral sphincter and the bulbourethral glands. Spongy ~15cm Courses through the corpus spongiosum Longest and most mobile. Bulbourethral gland opens onto proximal part. |
|
|
How is BPH treated? TRANSITIONAL ZONE |
BPH is first treated with alpha-blockers (α1) such as tamsulozin. Additionally 5α reductase inhibitors such as finasteride inhibit dihydortestosterone a hormone responsible for enlarging the prostate.
Trans-urethral resection of the prostate (TURP) is still considered the gold standard of prostate interventions for patients that require a procedure. This involves removing (part of) the prostate through the urethra. |
|
|
What are the features of prostate cancer? PERIPHERAL ZONE |
Prostate cancer is the most common cause of cancer found in men. Most tend to be slow growing; however, some can be aggressive. More than 80% of men will develop prostate cancer by the age of 80. However, in the majority of cases, it will be slow-growing and harmless. Symptoms are similar to that of BPH, however men may also experience dysuria and haematuria. Prostate cancer is most likely to spread to bone and therefore bone pain and symptoms of hypercalcaemia (bones, groans, stones, thrones, and psychiatric overtones). Examination of the prostate at digital rectal examination provides different findings from that of a BPH prostate. |
|
|
What are the treatment options for prostate cancer? |
Treatment is variable depending on both patient factors (such as grade and stage) and also tumour factors (such as grade and stage). Many men diagnosed with low-risk prostate cancer are eligible for active surveillance. Active surveillance involves monitoring the tumor for signs of growth or the appearance of symptoms. The monitoring process may involve serial PSA, physical examination of the prostate, and/or repeated biopsies. The goal of surveillance is to avoid overtreatment and the sometimes serious, permanent side effects of treatment for a slow-growing or self-limited tumor that would never cause any problems for the patient. Treatment for aggressive prostate cancers involves surgery (i.e. radical prostatectomy), radiation therapy including brachytherapy (prostate brachytherapy) and external beam radiation therapy, high-intensity focused ultrasound (HIFU), chemotherapy, oral chemotherapeutic drugs (Temozolomide/TMZ), cryosurgery, hormonal therapy, or some combination. |
|
|
Describe the course of the urethra in the penis. Within what structure does the urethra lie? |
Corpus spongiosum |
|
|
Name the arteries that supply the penis. From which artery do they branch? |
The penile artery (also known as the common penile artery) is the artery that serves blood to the penis. It subdivides into three arteries, the bulbourethral artery, the dorsal artery of the penis and the cavernosal artery.
Branches off the internal pudendal |
|
|
Name the muscle which contributes towards erection. |
Ischiocavernosus |
|
|
Which feature makes the scrotal skin corrugated? |
Dartos fascia of scrotum - consists mainly of smooth muscle - responsible for the rugged appearance |
|
|
Name the muscles involved in the temperature regulation of the testes. |
Cremasteric muscle part of spermatic cord - contracts to warm. Pubococcygeus somatic control |
|
|
To which nodes do the lymphatic vessels of the scrotum drain? How does this differ from the lymphatic drainage of the testes? |
Scrotum - inguinal lymph |
|
|
What is the homologue of the scrotum in women? |
Labiam majora |
|
|
Which nerve supplies the dartos fascia and cremaster muscles? |
Genital branch of genitofemoral nerve |
|
|
Describe the nervous innervation of the pelvis and perineum. |
Two hypogastric nerves on each side enter the pelvis, which are formed by the separation of the fibres in the superior hypogastric plexus at L5 (ascending parasympathetic and descending sympathetic). Pelvic parts of the plexus carry sympathetic, parasympathetic and visceral afferent fibres and are associated with innervations of pelvic viscera and erectile tissues of the perineum. |
|
|
What forms the inferior hypogastric plexus? |
The inferior hypogastric plexus is formed in part by pelvic splanchnic nerves (parasympathetic nerves leaving the anterio rami of the sacral spinal nerves) from S2 to S4. Parasympathetic nerves derived from these plexuses penetrate the pelvic floor to innervate erectile tissue in both sexes. Terminal branches from this plexus pass through the deep perineal pouch and innervate erectile tissue. In men, these nerves (also known as cavernous nerves) are extensions from the prostatic plexus. |
|
|
What are features of parasympathetic nerves entering the pelvis? |
The parasympathetic fibres that enter the pelvic plexus: * Are generally vasodilatory* Stimulate bladder contraction (detrusor muscle & internal urethral sphincter) * Stimulate erection * (Modulate activity of the enteric nervous system) * Stimulation of parasympathetic nerves causes specific arteries in erectile tissues to relax, allowing blood to fill these tissues (corpora cavernosa and corpus spongiosum), causing the penis (and clitoris in women) to become erect. Arteries of the penis are branches of the internal pudendal artery. |
|
|
What are features of the sympathetic innervation of the perineum? |
Sympathetic fibres enter the plexus from the upper sacral parts of the sympathetic trunk. Ultimately, these fibres are derived from preganglionic fibres that leave the spinal cord in the anterior roots, mainly T10 to L2. These fibres: * Innervate blood vessels* Cause contraction of smooth muscle in the internal urethral sphincter in men and internal anal sphincter in both sexes * Cause smooth muscle contraction associated with the reproductive tract and with the accessory glands of the reproductive system * Move semen and secretion from the epididymus and associated glands into the urethra during ejaculation |
|
|
What are the divisions of the pudendal nerve? |
he major somatic nerve of the perineum is the pudendal nerve, originating from the sacral plexus (S2 to S4). It leaves the pelvic cavity through the greater sciatic foramen inferior to the piriformis muscle, passes around the sacrospinous ligament and then enters the anal triangle of the perineum by passing medially through the lesser sciatic foramen. The pudendal nerve has 3 major terminal branches: * Motor: external sphincter muscle, levator ani muscle* Sensory: anal triangle * Perineal nerve * Motor: urogenital triangle, superficial and deep perineal pouch * Sensory: urogenital triangle, posterior scrotal nerve (posterior labial nerve in women) * Sensory to glans of penis (or clitoris) |
|
|
Which nerves supply the scrotal skin? Specify their root values. |
Genital part of genitofemoral - L1-L2 |
|
|
What are features of ED? |
Erectile dysfunction (ED) is the inability to get and maintain an erection that is sufficient for satisfactory sexual intercourse. The Latin term impotentia coeundi describes simple inability to insert the penis into the vagina. ED is also known as impotence. Normal erection occurs when a sexual stimulus causes the release of nitric oxide from nerve endings, causing the relaxation of endothelial cells of the corpus cavernosum , increasing blood flow, thereby compressing veins and engorging erectile tissue. It is estimated that half of men between 40 and 70 have some degree of ED. ED is often an early sign that your blood vessels are narrowing, as blood vessels to the penis are a lot smaller than elsewhere in the body. |
|
|
What is the treatment of ED? |
A vacuum pump is a treatment method for ED. It consists of a clear plastic tube that is connected to a pump, which is either hand or battery operated. This creates a vacuum that causes the blood to fill the penis, then a rubber ring is placed around the base of the penis in order to keep the blood in place, allowing the maintenance of an erection for around 30 minutes. Simple drugs aid corpus smooth muscle relaxation. PDE-5 inhibitors (e.g. sildenafil [Viagra], tadalafil, vardenafil) work to relax smooth muscles for various durations and are triggered by sexual stimulation. In men who did not respond to PDE-5 inhibitors, alprostadil intracavernosous injections are successful in 85%. Alprostadil is a synthetic hormone that helps to stimulate blood flow to the penis and can be injection directly into the penis (intracavernosal injection) or placement of a small pellet into the urethra. In the past, surgery was used if there was clear evidence of a blockage to the blood supply of the penis (e.g. due to trauma), unblocking the vessels to restore a normal blood supply. Long-term results of this type of surgery are poor, however, so it is unlikely to be used. Penile implants are a type of surgery that may be considered for trauma patients. These can be semi-rigid implants or inflatable implants (which consist of two or three parts that can be inflated to give a more natural erection). |
|
|
What are the boundaries of the anal triangle? |
The anal triangle can be defined either by its vertices or its sides. * one vertex at the coccyx bone* the two ischial tuberosities of the pelvic bone * perineal membrane (posterior border of perineal membrane forms anterior border of anal triangle) * the two sacrotuberous ligaments |
|
|
What are the contents of the anal triangle? |
* Ischioanal fossa
* Anococcygeal body * Sacrotuberous ligament * Sacrospinous ligament * Pudendal nerve * Internal pudendal artery and Internal pudendal vein * Anal canal * Sphincter ani externus muscle * Gluteus maximus muscle * Obturator internus muscle * Levator ani muscle * Coccygeus muscle |
|
|
Describe the main function of the ischio-anal fossa.
Name the structures contained within the ischio-anal fossa. |
The ischioanal fossa (formerly called ischiorectal fossa) is the fat-filled space located lateral to the anal canal and inferior to the pelvic diaphragm. The fossa is filled with fat as its function is to allow movement and provide structural support to the pelvic diaphragm and anal canal during defecation.
The contents include: * internal pudendal artery* internal pudendal vein * pudendal nerve * inferior rectal artery * inferior rectal veins * inferior anal nerves * fatty tissue across which numerous fibrous bands extend from side to side |
|
|
Name the structures contained within the pudendal canal. |
The pudendal canal is formed by the obturator internus fascia. It encloses the following: * Internal pudendal artery* Internal pudendal veins * Pudendal nerve These vessels and nerve cross the pelvic surface of the obturator internus. |
|
|
What are features of the upper 2/3rd of the anal canal? |
The mucous membrane of the upper half of the anal canal (2/3s) is derived from hindgut endoderm. It has the following features * lined by columnar epithelium* vertical folds – anal columns joined together inferiorly by semilunar folds – the anal valves * nerve supply same as rectal mucosa * arterial supply and venous drainage same as hindgut (inf mesenteric) * lymphatic drainage along superior rectal artery to inf. mesenteric nodes |
|
|
What are features of the lower 1/3rd of the anal canal? |
The mucous membrane of the lower half of the anal canal (1/3s) is derived from ectoderm (proctodeum). It has the following features * lined by stratified squamous epithelium – merges with skin of anus* no anal columns * nerve supply somatic – inferior rectal branch of pudendal * arterial supply and venous - inferior rectal – branch of pudendal – internal illiac * lymphatic drainage down to superficial inguinal nodes |
|
|
The anal cushions also bulge into the anal canal? Describe the main function of the anal cushions. |
Anal columns (of Morgagni) are 5-10 longitudinal (vertical) mucosal folds in the upper part of the anal canal. At the bottom of these columns are anal crypts, or sinuses, into which open the anal glands and anal papillae. Infection of the anal glands is likely the initial event in causation of perianal abscess and fistula-in-ano. Three of these columns (left lateral, right posterior, and right anterior, at 3, 7, and 11 o’clock position in supine position) are prominent; they are called anal cushions and contain branches and tributaries of superior rectal (hemorrhoidal) artery and vein. When prominent, veins in these cushions form the internal hemorrhoids. |
|
|
What are features of the pectinate line? |
The dentate line (also called the pectinate line) is the site of fusion of the proctodeum below and the postallantoic gut above. It is a wavy demarcation formed by the anal valves (transverse folds of mucosa) at the inferior-most ends of the anal columns. Anal glands open above the anal valves into the anal crypts. The dentate line is not seen on inspection in clinical practice, but under anesthesia the anal canal descends down, and the dentate line can be seen on slight retraction of the anal canal skin. |
|
|
What are features of the anal sphincter + anorectal ring? |
The anal canal has an involunatary sphincter the internal anal sphincter and a voluntary external sphincter. The puborectalis fibres of the levator ani blend with the deep fibres of the external sphincter. At the junction of the rectum and the anal canal, the internal sphincter, the deep part of the external sphincter and the puborectalis muscles form a distinct ring, called the anorectal ring, which can be felt on rectal examination |
|
|
How do you treat haemorrhoids? |
The simplest treatment is to increase the amount of fibre (e.g. fruits, vegetables, breads and cereals) and fluids in the diet, avoid straining or spending a long time on the toilet. This avoids constipation and reduces the pressure in the anal canal. If the pile is uncomfortable sitting in a bath of warm water for 10 minutes or so may give some relief. If haemorrhoids are particularly troubling a variety of procedures can be performed as an outpatient. * Rubber band ligation* Injection sclerotherapy * Hemorrhoidectomy * Stapled haemorrhoidopexy |
|
|
What are perianal haematomas? |
Patients may suddenly develop a small painful lump at the edge of the anus. This often happens after passing stool and represents a ruptured blood vessel at the edge of the anal canal. It is not sinister and often resolves itself, often by discharging a small amount of blood as the clot bursts. Avoiding constipation and using simple painkillers is often all that is required. Sitting in warm water for about 10 minutes may also help and the pain usually subsides in a few days. If the pain is severe or persistent the blood clot can be evacuated using a small incision under local anaesthesia as an outpatient to provide relief. |
|
|
What are peri-anal abscesses? |
Patients with an abscess around the anal canal present with severe pain often associated with fever and feeling generally unwell. An abscess forms when one of the glands which surround the anal canal becomes blocked and infected with bacteria. Some groups of patients such as those with Crohn’s disease are more prone to develop these abscesses. In those with diabetes or who have a reduced immunity peri-anal abscesses may be very dangerous and should be treated immediately. The treatment for these abscesses is by surgery. |
|
|
What is a fistula in ano? |
An anal fistula is a connection, or tunnel, between the inside of the anal canal and the skin around it. It is the result of a previous abscess which develops when the anal glands become blocked and subsequently infected. Fistulas present about 4-6 weeks after an abscess has been treated but may become obvious months or years later. A fistula leads to persistent discharge of pus or fluid around the anus leading to soiling of underwear and skin irritation. Occasionally the fistula may appear to have healed only for a recurrent abscess to form. Patients with Crohn’s disease are particularly prone to the development of anal fistulas. |
|
|
What is an anal fissure? |
An anal fissure is a small tear in the skin that lines the anus. They present with pain on defecation and bright fresh rectal bleeding usually o the toilet paper. The pain associated with a fissure may be so severe that patients avoid going to the bathroom, this leads to constipation and even more pain. Often patients will not allow their doctor to examine their anus since the pain is unbearable, this is almost diagnostic of a fissure. Fissures typically occur following trauma to the lining of the anal canal, this is commonly due to passing hard dry stool such as with constipation. They may also be associated with inflammatory conditions such as Crohn’s disease. Fissures are divided into acute, which are of new onset, and chronic which have been present for over 6 weeks or are recurrent. Chronic fissures are usually associated with a small skin tag at the anal margin known as a sentinel pile. |
|
|
How are anal fissures treated? |
Although some favour the use of GTN ointment, which has the same effect as diltiazem, this may not be tolerated by some people due to the development of headaches. If creams fail, injecting Botox (botulinum toxin) directly into the sphincter muscle can be attempted and may lead to healing in up to 75% of patients. If these treatments fail consideration should be given to surgery. This usually consists of an operation to cut a small portion of the internal anal sphincter muscle (a lateral sphincterotomy). This is a highly effective treatment for a fissure with complete healing occurring in a few weeks. There is however, a small risk of minor incontinence following this procedure and the benefits and risks should be discussed with the surgeon. |
|
|
What are features of anal cancer? |
Anal cancers usually arise from the skin cells (squamous cells) around the anal opening and are known as squamous cell carcinomas. Anal cancer is relatively uncommon accounting for 1% of all gastrointestinal cancers with colorectal cancer being around 40 times more common. Some patients develop pre-cancerous cells, which require regular surveillance, these are known as carcinoma-in-situ. The symptoms of anal cancer are similar to those of many anal canal lesions such as itching, bleeding, pain, feeling a lump, an alteration in bowel habit and even swollen glands in the groin. Since the anal canal is an area easily accessible to doctors, making an early diagnosis should be possible with rectal examination and simple biopsy under anaesthetic. Risk factors for developing anal cancer include; age, the presence of anal warts and infection with the human papilloma virus (HPV), anal sex, HIV infection, smoking, impaired immunity and previous pelvic irradiation. |

