![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
63 Cards in this Set
- Front
- Back
|
local interactions
|
- effect of material on host tissues
- effect of environment on materials |
|
|
effect of material on host tissues
|
- blood material interactions
- toxicity - modification of healing - inflammation - infection - tumorgenesis |
|
|
effect of environment on material
|
- wear
- fatigue - corrosion - stress-corrosion cracking - absorption of tissue constituents by implant - enzymatic degradation - calcification |
|
|
systemic interactions
|
- embolization
- hypersensitivity - elevation of implant elements in blood - lymphatic particle transport |
|
|
device-associated complications
|
- thrombosis/thromboembolism
- infection - exuberant or defective healing - biomaterials failure - adverse local tissue reaction - adverse systemic effect |
|
|
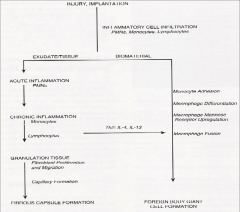
sequence of host reactions following implantation devices
|
- injury from an implantation process
- blood-material interactions - acute inflammation = short duration that may last minutes to days - chronic inflammation = may last for weeks to months or even longer if not treated - granulation tissue - foreign body reaction = immune system response - fibrosis/fibrous capsule development |
|
|
injury implantation
|
|
|
|
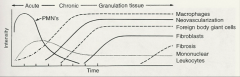
acute inflammation
|
- granulocyte, leukocyte, macrophage
- acute process last from minutes to few days depending on injury - engulfment and degradation of biomaterials may or may not occur - disparity between the size of biomaterial and cells may lead to frustrated phagocytosis |
|
|
granulocyte
|
- any blood cell containing specific granules
- neutrophils, eosinophils, basophils |
|
|
leukocyte
|
- a colorless blood cell capable of ameboid movement
- lymphocytes, monocytes, granulocytes |
|
|
macrophage
|
- large phagocytic mononuclear cell
|
|
|
neutrophils
|
- most common one
- segmented nuclei connected by thin strands of chromatin - first cells to appear at injury site - cells become sticky - stick to capillary endothelium - penetrate between endothelial cells - move into surrounding damaged tissue - emigration begins minutes to hours after insult and may continue for as long as 24 hours - activates when engages foreign particles - predominate during first several days |
|
|
eosinophils
|
- bi-lobed nucleus
|
|
|
basophils
|
- least common one
- large cytoplasmic granules which obscure nucleus - very rare |
|
|
monocytes
|
- largest one
- deeply indented of U-shaped nucleus - replace neutrophils as predominant cell type - short lived = 24 - 48 hours - emigration is limited - chemotactic factors for emigration are not active during latter stages of inflammation - emigration continue to be at injury for days to weeks - chemotactic factors activated over longer periods of time - differentiate into macrophages which are very long lived = months |
|
|
acute inflammation response
|
- caused by tissue damage from traumatic wound, pathogenic microorganism, or implantation
- delivery of effector molecules and cells to site of infection - formation of physical barrier to spread of tissue damage or infection - wound healing and tissue repair |
|
|
four clinical signs of acute inflammation response
|
- rubor = redness
- tumor = swelling - calor = heat - dolor = pain |
|
|
swelling
|
- due to presence of difference between capillary and external tissue bed increase
- low permeability in normal condition - greater permeability in inflammation - increased fluid influx not promptly balanced by lymphatic system |
|
|
low permeability
|
- endothelium = fluid flow and small molecules permeate
- lymphatic vessels drain away this fluid maintaining constant tissue volume |
|
|
greater permeability
|
- larger molecules move into the tissue at greater rate
|
|
|
rubor
|
- redness
- erythrocytes rush to injury area and accumulating there |
|
|
tumor
|
- swelling
- local edema |
|
|
calor
|
- heat
- increased cellular metabolic activity - possible generation of pyrogens (fever induced substance) which are known to cause systemic fever - local disturbance of fluid flow |
|
|
dolor
|
- pain
- from edema and kinins - local edema may activate local deep pain receptors - throbbing pain associated with peaks of systolic pressure - kinins act directly on nerve ends to produce pain sensation |
|
|
phase of phagocytosis
|
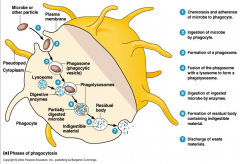
- chemostasis and adherence of microbe to phagocyte
- ingestion of microbe by phagocyte - formation of a phagosome - fusion of phagosome with a lysosome to form a phagolysosome - digestion of ingested microbe by enzymes - formation of residual body containing indigestible material - discharge of waste materials |
|
|
response to acute inflammation
|
- reduction in local tissue mass and fluid = edema
- dead cells removed by neutrophils and macrophages |
|
|
frustrated phagocytosis
|
- caused by disparity between size of biomaterial and cells
- leukocyte products are released extracellularly in an attempt to degrade the biomaterial |
|
|
chronic inflammation
|
- follow acute inflammation
- persistent inflammatory stimuli - confined to implant site |
|
|
persistent stimuli
|
- chemical and physical properties of biomaterial
- motion in implant site |
|
|
characterization of chronic inflammation
|
- presence of macrophages, monocytes, lymphocytes
- proliferation of blood vessels and connective tissue - no exudates |
|
|
macrophages
|
- produce great number of biologically active products
- proteases to degrade molecules - chemotactic factors - growth promoting factors - coagulation factors - cytokines |
|
|
growth factors
|
- growth of fibroblasts and blood vessels
- regeneration of endothelial cells - stimulate production of a wide variety of cells - initiate cell migration and differentiation - tissue remodeling and wound healing |
|
|
granulation tissue
|
- hallmark of healing inflammation
- neovascularization or angiogenesis - wound healing dependent on extent of injury |
|
|
healing inflammation
|
- pink, soft granular appearance on surface of healing wounds
- seen as early as 3-5 days of following implantation |
|
|
neovascularization or angiogenesis
|
- proliferation, maturation, and organization of endothelial cells into capillary tubes
- budding or sprouting of pre existing vessels - formation of new small blood vessels |
|
|
wound healing response
|
- primary union = first intention
- secondary union = second intention |
|
|
primary union
|
- wound edges approximated by surgical sutures
- without significant bacterial contamination - clean surgical incisions - minimal loss of tissue |
|
|
secondary union
|
- large tissue defect
- extensive loss of cells and tissue - original architecture not reconstituted - large amounts of granulation tissue formed - larger areas of fibrosis or sear formation |
|
|
foreign body reaction
|
- macrophages
- multi nucleated foreign body giant cells that form upon coalescence of macrophages - fibroblasts - capillaries - these cells persist at tissue implant interface - if implant has smooth and flat surfaces = FBR composed of layer of macrophages one to two cells in thickness - if implant has relatively rough surface = FBR composed of multiple layers of macrophages and foreign body giant cells at surface - if implant has rough surface = FBR composed of macrophages and foreign body giant cells with varying degrees of granulation tissue |
|
|
fibrosis and fibrous encapsulation
|
- occur at end stage of healing response
- usually it takes four or more weeks after implantation - presence of neutrophils = persisting inflammatory challenge - presence of foreign body giant cells = production of small particles by corrosion, depolymerization, dissolution or wear - thickness of encapsulation depends on chemical activity of material - capsules thickness increases with increase in relative motion between implant and tissue - shape of implant: capsule will be thicker over sharp edges |
|
|
type of infections
|
- delayed infection
- late infection - delayed and late infections are rarely seen in total joint replacement or heart valve implantation - infections difficult to treat once established in or around implant |
|
|
delayed infection
|
- happens within 3 months
- slow development of intraoperative bacterial contamination |
|
|
late infection
|
- month to years after surgery in sites of no prior history of infection
- believed to be caused by transport and seeding of blood-borne bacteria from an established infection at a remote site - tooth root abscess - urinary tract infection |
|
|
mechanisms for interactions
|
- biomaterials release toxic substances: unpolymerized monomer of bone cement
- biomaterials that are non-toxic but are reabsored: synthetic absorbable sutures, TCP screws - biomaterial that are non-toxic and non absorbable are encapsulated - biomaterial non-toxic but stimulates inflammation or enhances infection: any material that can be resorbed - biomaterial with highly interactive bonding to tissues: natural materials |
|
|
local host reaction
|
- blood-biomaterial interactions: protein adsorption, coagulation, fibrinolysis, platelet activation, leukocyte adhesion, hemolysis
- modification of normal healing: encapsulation, foreign body reaction, pannus formation - infection = defense against foreign microorganisms - edema - tumorgenesis |
|
|
systemic host reaction
|
- hypersensitivity and sensitization
- thrombus, embolization - fever - pain |
|
|
undesired material selection
|
- irritation = feeling of discomfort, sore, and mild to moderate pain
- itching = surface phenomenon, chemical or physical incompatibility - inflammation = process of defensive response, much more severe response than irritation, redness, heat, swelling, and pain - necrosis = tissue death - pyrogenicity = tendency to trigger fever - sensitization = delay reaction, immunologically mediated allergies - mutagenicity = tendency to produce genetic mutation - plasticizers, carcinogenicity, tumorgenesis |
|
|
effects of host on implant
|
- mechanical physical effects
- biological effects - inflammation |
|
|
mechanical physical effects
|
- fatigue
- corrosion - abrasive wear - micro-cracking - degeneration - dissolution |
|
|
biological effects
|
- absorption of substances from tissues
- enzymatic degradation - calcification |
|
|
inflammation
|
- acute and chronic response
|
|
|
major physiological events during an inflammatory response
|
- immediate vasoconstriction of blood vessels leading away from site
- increased volume of blood flow to site = vasodilation - decreased velocity of blood flow to site = leucocytes are able to slow down and adhere to vascular endothelium - increased expression of vascular endothelial adhesion molecules = leucocytes are able to attach to vascular endothelium - increased vascular permeability = fluid enters tissue - influx of phagocytic cells in to tissues = may be due to increased margination and extravasation |
|
|
inflammation response
|
- phagocytic cells are first main types of leucocytes to emigrate = first neutrophils then macrophages
- later, lymphocytes (B & T cells) may also enter site - margination - phagocytic cells accumulate at responded site |
|
|
margination
|
- adherence fo cells to endothelial wall
- diapediesis/extravasation = migration between capillary endothelial cells into tissue - chemotaxis = chemically directed migration through tissue to the site of inflammatory response |
|
|
phagocytic cells
|
- release lytic enzymes and damage nearby cells
- pus forms which is accumulation of dead cells, digested materials, fluid |
|
|
histamine
|
- released by different cell types following tissue injury
- stimulate vasodilation and increase capillary permeability |
|
|
sequence of local events following implantation
|
- injury
- acute inflammation - chronic inflammation - granulation tissue - foreign body reaction - fibrous encapsulation |
|
|
arachidoinc pathway
|
- leads to production of leukotrienes and prostaglandins
|
|
|
secondary pathway
|
- leads to production of platelet aggregating factor
|
|
|
cells and components of vascularized connective tissue
|
- extracellular matrix components = collagen, proteoglycans, elastin, fibronectin, laminin
- intracellular fluid (blood cells) = erythrocytes, neutrophils, monocytes, eosinophils, lymphocytes, plasma cells, basophils, and platelets - connective tissue cells = mast cells, fibroblasts, macrophages, lymphocytes |
|
|
prosthetic valve complication
|
- thrombosis on aortic valve prosthesis
- prosthetic valve endocarditic with large ring abscess - thromboembolic infarct of small bowel - strut fracture of Bjork-Shiley valve - structural valve dysfunction |
|
|
inflammatory chemicals
|
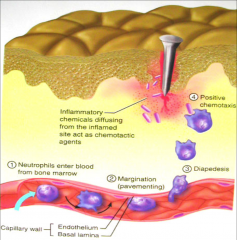
- diffuse from inflamed site
- act as chemotactic agents - neutrophils enter blood from bone marrow - margination - diapedesis - positive chemotaxis |
|
|
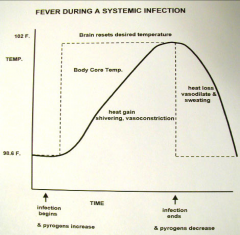
fever temperatures
|
|

