![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
93 Cards in this Set
- Front
- Back
|
Describe the quadrant subdivision of the abdomen. Which organs are located in each quadrant?
|
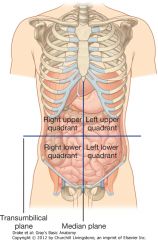
Quadrants are formed from the median plane that runs vertically along the line of the vertebral column and the transumbilical line that runs horizontally through the umbilicus
Right upper quadrant: ---Liver ---Gallbladder Left upper quadrant: ---Spleen ---Stomach Right lower quadrant: ---Cecum ---Appendix Left lower quadrant: ---Descending colon ---Sigmoid colon |
|
|
Describe the nine region subdivision of the abdomen. Which organs are located in each region?
|
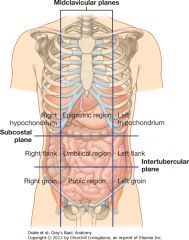
The regions are formed by the two midclavicular lines running vertically, the subcostal plane, the superior horizontal plane, that is just inferior to the costal margins and the inferior horizontal plane, the intertubercular plane, that crosses between the tubercles of the iliac crests
Right hypochondrium: ---Liver, Gallbladder, Kidney Epigastric region: ---Liver, Stomach, Pylorus, Duodenum, Kidney/Adrenal gland, Pancreas Left hypogastric: ---Spleen, Kidney, Pancreas, Descending colon Right lumbar/flank: ---Ascending colon, Kidney Umbilical region: ---Duodenum, Stomach Left lumbar/flank: ---Kidney, Descending colon Right inguinal/groin: ---tail end of cecum Hypogastric/pubic region: ---Appendix, Rectum, Sigmoid colon Left inguinal/groin: ---Descending colon Referred pain: ---Foregut pain refers to epigastric region ---Midgut pain refers to umbilical region ---Hindgut pain refers to inguinal/pubic region |
|
|
Describe the fascial and muscular components of the anterior abdominal wall.
|
Fascia:
Superficial fascia: ---superficial layer: fatty (camper's fascia); in men, continues over penis, loses its fat, fusing with deep layer and forms specialized fascia containing smooth muscle in scrotum (dartos fascia) ---deep layer: membranous, thin with little fat (scarpa's fascia); fuses with fascia lata; forms superficial perineal fascia (colles' fascia); in men, forms fundiform ligament of the penis, on sides/inferiorly Transversalis fascia: ---deep to transverse abdominis, continuous layer of deep fascia that lines the abdominal cavity and into pelvic cavity Rectus sheath: aponeurotic tendinous sheath surrounding rectus abdominis formed by layering of aponeuroses of obliques; arcuate line marks end of sheath Extraperitoneal fascia: deep to transervsalis fascia, separating it from peritoneum Muscles: ---external obliques: immediately deep to fascia on sides, fibers running inferomedially; lower portion of aponeurosis forms inguinal ligament ---internal obliques: deep to external, smaller and thinner, fibers run superomedial ---transverse abdominis: deep to internal, fibers run horizontally towards midline ---rectus abdominis: long, flat, separated in midline by linea alba; transected by tendinous intersections ---pyramidalis: small, triangular anterior to rectus abdominis attaching near pubis and linea alba Peritoneum: ---deep to extraperitoneal fascia; thin serous membrane that lines abdominal walls ------parietal peritoneum: lines walls ------visceral peritoneum: covers organs |
|
|
Describe the innervation of the abdominal wall.
|
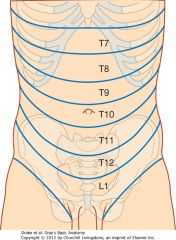
Innervation:
---skin, muscles, parietal peritoneum: T7-L1 spinal nerves (anterior rami), pass around body, end as cutaneous branches ------intercostal nerves (T7-T11) leave intercostal space and continue into abdomen between internal oblique and transversus abdominis ------subcostal nerve (T12) follows intercostals' course ------Ilio-hypogastric and Ilio-inguinal (branches of L1) originate from lumbar plexus, follow initial course but end differently Dermatomes indicate skin innervation |
|
|
Describe the vascular supply of the anterior abdominal wall.
|
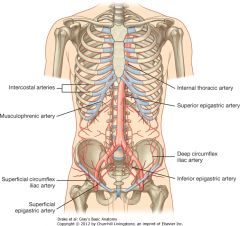
Arterial:
superficially: ---superior: musculophrenic (terminal branch of internal thoracic) ----inferior: (medial) superficial epigastric; (lateral) superficial circumflex iliac, branches of femoral artery deeply: ---superior: superior epigastric (terminal branch of internal thoracic) ---lateral: branches of 10/11 intercostal arteries and subcostal artery ---inferior: inferior epigastric, deep circumflex iliac artery, branches of external iliac artery ***superior/inferior epigastric anastomose*** Veins: ---follow arteries |
|
|
Describe the inguinal canal.
|
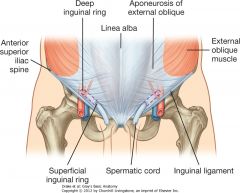
Parallels the inguinal ligament superiorly; contains the genital branch of the genitofemoral nerve, the spermatic cord (men) and round ligament (women) and ilio-inguinal nerve
Walls: ---anterior: aponeurosis of external oblique, lower fibers of internal oblique (laterally) to cover deep inguinal ring (form cremasteric muscle) ---posterior: transversalis fascia, conjoint tendon (medially) formed by intersection of transverse abdominis and internal oblique ---roof: arching fibers from transverse abdominis and internal oblique ---floor: inguinal ligament ---Deep inguinal ring: beginning of canal, midpoint between ASIS and pubic symphysis; formed from beginning of tubular evagination of transersalis fascia covering of spermatic cord/round ligament ---Superficial inguinal ring: external ring, opening of aponeurosis of external oblique, with medial/lateral crus on each side; beginning of tubular evagination of aponeurosis |
|
|
Why is the inguinal region considered a weak area of the abdominal wall?
|
The wall is weakened from changes that occur during development of the gonads (processus vaginalis: peritoneal outpouching)
|
|
|
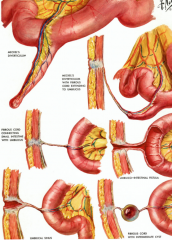
Describe direct and indirect inguinal hernias.
|
Direct: enters medial end of inguinal canal through weaken abdominal musculature
---covering of hernia: transversalis fascia, cremasteric muscle, parietal peritoneum, extraperitoneal fascia (all coverings of spermatic cord/round ligament) and external spermatic fascia Indirect: most common, usually because processus vaginalis remains open; enters inguinal canal through deep inguinal ring, lateral to inferior epigastric vessels and exits through superficial inguinal ring More common in men because the spermatic cord causes a weakness in the abdominal wall. |
|
|
What are the major subdivisions of the peritoneal cavity and how are they related?
|
Greater sac:
---most of space in cavity, beginning superior to diaphragm and continuing to pelvic cavity, deep to the parietal peritoneum Lesser sac (omental bursa): ---smaller, posterior to stomach and liver; continuous with greater sac through omental foramen |
|
|
Describe parietal and visceral peritoneum and their innervations.
|
Parietal peritoneum:
---lines walls of cavity; innervated by somatic afferents carried by branches of associated spinal nerves, sensitive to well-localized pain Visceral peritoneum: ---covers viscera; innervated by visceral afferents that accompany sympathetic/parasympathetic nerves back to CNS leading to referred pain (poorly localized sensation of discomfort) and reflex visceral motor activity |
|
|
Describe the omenta in the peritoneal cavity, its function and the two different ones found in the cavity.
|
Omenta: consists of two layers of peritoneum, from stomach and duodenum to other viscera
---Greater omentum: (derived from dorsal mesentary) large, apron-like attached to greater curvature of stomach, drapes inferiorly over transverse colon, jejunum and ileum and attaches to posterior abdominal wall near transverse mesocolon ------thin membrane that contains fat, and right/left gastro-omental arteries/veins ---Lesser omentum: (derived from ventral mesentary) two-layer peritoneum extending from lesser curvature of stomach and first part of duodenum to liver; contains left/right gastric vessels ------forms into: hepatogastric ligament (medial) passing between stomach and liver; hepatoduodenal ligament (lateral) passing between liver and duodenum - forms omental foramen |
|
|
Describe mesenteries of the peritoneal cavity, its function and the different ones found in the cavity.
|
Mesenteries: peritoneal folds that attach viscera to posterior abdominal wall; allow some movement, provide conduit for vessels, nerves, lymphatics
---mesentery: large, fan-shaped double layer fold connecting jejunum and ileum to the posterior abdominal wall; starts superiorly at duodenojejunal flexure and ends at ileocecal flexure (vessels, nerves, lymphatics lie between the two peritoneal layers) ---transverse mesocolon: connects transverse colon to posterior wall; double layers contain vessels, nerves, lymphatics; anterior layer is adherent to posterior greater omentum ---sigmoid mesocolon: attaches sigmoid colon to abdominal wall; shaped like inverted V, ends near division of left common iliac artery into internal/external branches; sigmoid/superior rectal vessels, associated nerves and lymphatics pass through fold |
|
|
Describe ligaments in the peritoneal cavity, their function and give examples.
|
Ligaments: consist of two layers of peritoneum that connect two organs to each other, or an organ to the body wall (can form part of omentum)
Examples: ---splenorenal ligament: left kidney to spleen ---gastrophrenic ligament: stomach to diaphragm ---hepatogastric ligament: stomach to liver |
|
|
Describe the location of spaces and gutters in the peritoneal cavity and explain their clinical significance.
|
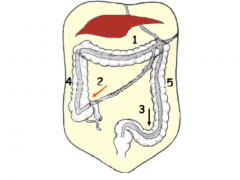
1. supramesocolic/inframesocolic spaces: divisions of the abdominal cavity formed by the transverse colon
2. Right and 3. Left infracolic spaces: small bowl mesentery forms division; right terminates at ileocecal flexure and left opens into pelvis to right and restricted from continuity by sigmoid mesocolon 4. Right and 5. Left paracolic gutters: lateral to attachments of peritoneal reflections of ascending/descending colon; represent communication between lower abdomen and pelvis with supramesocolic space ---gutters are significant because allow passage of infectious fluids between different compartments of abdomen and pelvis |
|
|
Name the organs that are retroperitoneal.
|
SAD PUCKER:
S-suprarenal (adrenal gland) A-aorta D-duodenum (2nd, 3rd, 4th parts) P-pancreas U-ureters C-colon (ascending/descending K-kidneys E-esophagus (lower 2/3) R-rectum and inferior vena cava, common iliac artery (internal/external branches), inferior bladder and uterus |
|
|
Name the organs that are intraperitoneal.
|
Liver, stomach, spleen, 1st part of duodenum, jejunum, ileum, cecum, transverse colon, sigmoid colon, rectum, superior bladder and uterus (fallopian tubes/ovaries)
|
|
|
Describe the foregut, its derivatives and neurovascular supply.
|
Organs: esophagus*, stomach, proximal duodenum, liver, gall bladder, pancreas*, spleen
Blood supply: branches of celiac trunk Innervation: T5-T9 ---sympathetic: preganglionic - greater splanchnic nerves; postgangilonic - celiac plexus via celiac ganglia (pain referred to epigastric region) ------decreased motility and secretion, contraction of sphincters, visceral afferents refer pain sensations ---parasympathetic: preganglionic - vagus nerve ------increased motility and secretion, relaxation of sphincters, visceral afferents transmit visceral reflexes |
|
|
Describe the derivatives of the midgut and its neurovascular supply.
|
Organs: distal duodenum*, jejunum, ileum, cecum, appendix, ascending colon*, proximal 2/3 of transverse colon
Blood supply: branches of superior mesenteric artery Innervation: T5-T9/T10-T11 ---sympathetic: preganglionic - greater (T5-T9) and lesser splanchnic (T10-T11) nerves; postganglionic - superior mesenteric plexus via superior mesenteric ganglia (pain referred to umbilical region) ------decrease motility and secretion, contraction of sphincters, visceral afferents refer pain ---parasympathetic: preganglionic - vagus nerve ------increased motility and secretion, relaxation of sphincters, visceral afferents transmit visceral reflexes |
|
|
Describe the derivatives of the hindgut and its neurovascular supply.
|
Organs: distal 1/3 of transverse colon, descending colon*, sigmoid colon, rectum*, anal canal*
Blood supply: branches of inferior mesenteric artery Innervation: L1-L2 ---sympathetic: preganglionic - lumbar and sacral splanchnic nerves; postganglionic - inferior mesenteric plexus via inferior mesenteric ganglia (pain referred to pubic region) ------decreased motility and secretion, contraction of sphincters, visceral afferents refer pain ---parasympathetic: preganglionic - pelvic splanchnic nerves (S2-S4) ------increased motility and secretion, relaxation of sphincters, visceral afferents transmit visceral reflexes |
|
|
Describe the anatomical features of the stomach, its neurovascular supply and lymphatic drainage.
|
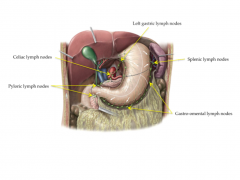
It is the most dilated portion of GI tract, has a J shape and lies in the epigastric, umbilical and left hypogastric regions
Divides into four regions: ---cardia: area around opening of esophagus into stomach ---fundus: area superior to cardial orifice ---body: largest main portion of stomach ---pylorus: distal end of stomach, contains pyloric sphincter between stomach and duodenum ---Greater curvature of stomach: forms outside/inferior curve ---Lesser curvature of stomach: forms inner/superior curve Blood supply: ---arterial: gastric arteries follow the lesser curvature (right from proper hepatic artery and left from celiac trunk); gastro-omental arteries follow the greater curvature (right from gastroduodenal artery and left from splenic artery) ------short gastric arteries from gastric and gastro-omental arteries project inwards to body of stomach Innervation: T5-T9 ---sympathetic: greater splanchnic/superior mesenteric ---parasympathetic: vagus nerve Lymph: drains to thoracic duct ---regional: splenic, gastric, gastro-omental, pyloric ---regional drain into celiac nodes ---celiac nodes drain into cisterna chyli and thoracic duct |
|
|
Describe the anatomical structure of the small intestine, its neurovascular supply and lymphatic drainage.
|
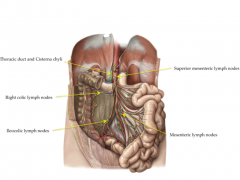
Longest part of GI tract, extends from pyloric orifice of stomach to ileocecal flexure; hollow tube 6/7 m long with narrowing diameter from beginning to end
Duodenum: c-shaped, retroperitoneal except for first part; connected to liver by hepatoduodenal ligament, ends at duodenoejejunal flexure ---four parts: superior, descending (contains major/minor duodenal papilla - entrance for bile/pancreatic ducts), inferior, ascending Blood supply: ---branches from gastroduodenal artery ---supraduodenal artery from gastroduodenal artery ---duodenal branches from anterior/posterior superior and inferior pancreaticoduodenal arteries (from gastroduodenal artery/superior mesenteric artery) Jejunum: proximal 2/5 of end sections of small intestine; larger diameter, thicker wall than ileum; inner mucosal lining has plicae circularis (circular folds in lumen) and longer vasa recta (arterial branches) Blood supply: jejunal arteries from superior mesenteric artery Ileum: distal 3/5; thinner walls, fewer plicae circularis, shorter vasa recta, more mesenteric fat; form flaps at ileocecal flexure that prevent reflux from cecum to ileum and regulate passage of contents into cecum Blood supply: ileal arteries from superior mesenteric artery; ileal branch from ileocecal artery Innervation: T5-T9/T10-T11 ---proximal duodenum receives greater splanchnic/celiac plexus and vagus ---all other small intestin receives greater and lesser splanchnic/superior mesenteric and vagus Lymph: all goes to thoracic duct ---regional: mesenteric, ileocolic, right colic, middle colic, paracolic, sigmoid and superior rectal ---regional drain into superior/inferior mesenteric nodes ---superior/inferior mesenteric drain into cisterna chyli and thoracic duct |
|
|
Describe the anatomical structure of the large intestine, its neurovascular supply and lymphatic drainage.
|
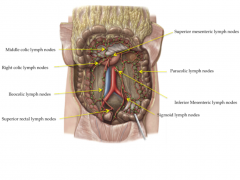
It extends from ileum to anus, ~1.5 m; absorbs fluids/salts from gut contents, forming feces; larger diameter, longitudinal muscle in walls form three bands (taenia coli), and sacculations (haustra)
Cecum/appendix: inferior to ileocecal opening, continuous with ascending colon, intraperitoneal; appendix attaches to inferior portion of cecum ---blood supply: anterior/posterior cecal arteries and appendicular artery from ileocecal artery (from superior mesenteric artery) Colon: (ascending*, transverse, descending* and sigmoid) ---transition of ascending to transverse to descending is marked by right/left colic flexures Blood supply: ---ascending: colic branch, anterior/posterior cecal arteries from ileocecal artery (from superior mesenteric artery) and right colic artery from superior mesenteric artery ---transverse: right colic artery, middle colic artery (from superior mesenteric artery) and left colic artery (from inferior mesenteric artery) ---descending: left colic artery (inferior mesenteric artery) ---sigmoid: sigmoidal arteries (inferior mesenteric artery) Rectum/anal canal: retroperitoneal, at end of sigmoid mesocolon ---blood supply: superior rectal artery (inferior mesenteric artery), middle rectal artery (internal iliac artery and inferior rectal artery from internal pudendal (internal iliac artery) Innervation: L1-L2 ---sympathetic: lumbar and sacral splanchnic/inferior mesenteric plexus ---parasympathetic: pelvic splanchnic nerves Lymph: all goes to thoracic duct ---regional: middle colic, right colic, paracolic, ileocolic, superior rectal, sigmoidal ---regional drain into superior/inferior mesenteric nodes ---superior/inferior mesenteric drain into cisterna chyli and thoracic duct |
|
|
Describe the anatomical structure of the liver and its neurovascular supply.
|
It is the largest visceral organ in the body; it is divided into left/right lobes by the falciform ligament (attaches to anterior abdominal wall); porta hepatis is the entry point for the hepatic arteries, portal vein and exit for hepatic ducts
---quadrate lobe: on the anterior/right side, next to gall bladder and ligamentum teres (functions are related to left lobe) ---cuadate lobe: on posterior/right side, near inferior vena cava and ligamentum venosum (functions separately from right/left lobes) Blood supply: right and left hepatic artery from proper hepatic artery (branch of common hepatic artery from celiac trunk) Innervation: T5-T9 ---sympathetic: greater splanchnic/celiac plexus ---parasympathetic: vagus nerve |
|
|
Describe the anatomical structure of the gall bladder, and its neurovascular supply.
|
It is a pear-shaped sac lying on visceral surface of right lobe of liver; receives, concentrates and stores bile from liver
Fundus: top, rounded end Body: major portion lying in fossa of liver Neck: narrowing near cystic duct Blood supply: cystic artery from right hepatic artery (branch of proper hepatic artery) Innervation: T5-T9 ---sympathetic: greater splanchnic/celiac trunk ---parasympathetic: vagus nerve |
|
|
Describe the anatomical structure of the pancreas, and its neurovascular supply.
|
It lies posterior to the stomach, from duodenum to spleen; secondarily retroperitoneal
Head: lies in C-shaped concavity of duodenum Uncinate process: projects from lower part of hear to superior mesenteric vessels Neck: narrowing before body Body: elongated portion Tail: passes between splenorenal ligament ---pancreatic duct: begins in tail, joins with bile duct to form the hepatopancreatic ampulla (surrounding by sphincter of Oddi) which enters the duodenum (2nd part) through major duodenal papilla ---accessory pancreatic duct: empties into duodenum above major papilla through minor papilla Blood supply: gastroduodenal artery (common hepatic), anterior/posterior superior pancreaticoduodenal arteries from gastroduodenal artery, dorsal and great pancreatic arteries (branches of splenic artery) and anterior/posterior inferior pancreaticoduodenal arteries (from branch of superior mesenteric artery) Innervation: T5-T9 ---sympathetic: greater splanchnic/celiac trunk ---parasympathetic: vagus nerve |
|
|
Describe the lymphatic drainage for the liver, gall bladder, pancreas and proximal duodenum.
|
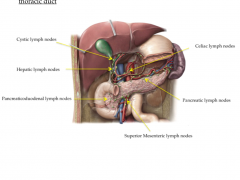
All eventually drain into thoracic duct
---regional: cystic, hepatic, pancreaticoduodenal, or pancreatic ---regional drain into celiac and superior mesenteric nodes ---celiac and superior mesenteric nodes drain into cisterna chyli and thoracic duct |
|
|
Describe the pathway of bile from liver to duodenum. What are some consequences of blockage?
|
Ducts coalesce in liver until right and left hepatic ducts are formed, draining their respective lobes; these combine to form the common hepatic duct (forms part of hepatic triad); as it descends it is joined by the cystic duct (from gall bladder), forming the bile duct; the bile duct continues to descend until it enters the duodenum at the major papilla
Blockages: gall bladder can form gall stones ---blocks in neck of gall bladder: can't empty, contractions cause pain, no jaundice ---block of sphincter of Oddi: obstructs flow of bile into duodenum, leads to jaundice (excess bile in plasma leads to yellow discoloration) |
|
|
Describe the course of the exocrine pancreatic secretions from source into duodenum.
|
Start in tail, continue through body
---pancreatic duct joins bile duct forming hepatopancreatic ampulla and enters duodenum through the major papilla ---accessory pancreatic duct empties into duodenum above major papilla through minor papilla; also branches (connects to pancreatic duct/descends into uncinate process) |
|
|
Describe the portal venous system and the systemic venous system. What are their anastomoses and how do they relate to portal hypertension?
|
Portal vein: is final common pathway for transport of venous blood from:
---spleen, pancreas, gall bladder and abdominal portion of GI tract Formed by union of splenic and superior mesenteric veins ---tributaries to portal: right/left gastric veins, cystic vein, para-umbilical veins ---tributaries to splenic: short gastric veins, left gastro-omental vein, pancreatic veins, inferior mesenteric vein ---tributaries to superior mesenteric: right gastro-omental vein, anterior/posterior inferior pancreaticoduodenal veins Systemic: drains anterior abdominal wall veins, esophageal veins, and middle/inferior rectal veins into femoral veins/iliac veins to inferior vena cava or azygos to superior vena cava Anastomoses: ---left gastric vein with azygos veins/esophageal veins: create esophageal varices during hypertension ---superior rectal vein with middle/inferior rectal veins: create hemorrhoids during hypertension ---para-umbilical veins with veins of anterior abdominal wall: create caput Medusa during hyptertension |
|
|
Describe the function and structure of the enteric nervous system.
|

It is a collection of neurons in the GI tract that acts as "brain of gut" and can function independently from CNS; extends from esophagus to anus
---primarily controls motility and secretion with input from sympathetic/parasympathetic nervous systems Consists of two plexuses of neurons embedded in wall of GI tract: ---myenteric/Auerbach's plexus: located in layers of muscle in muscularis externa; controls primarily motility ---submucosal/Meissner's plexus: located in submucosa; controls epithelial secretion (in areas where no secretion occurs, plexus little/absent) Local reflex system: formed from sensory, interneurons, motor and secretory neurons ---sensory: monitor changes in luminal activity (distension, chemistry, mechanical stimulation) ---interneurons: activated by sensory neurons/extrinsic inputs (sympathetic/parasympathetic) and relay signals to stimulatory/inhibitory motor neurons ---motor and secretomotor: stimulate/inhibit wide range of effector cells (smooth muscle in muscularis externa, epithelial cells that secrete/absorb fluid and submucosal blood vessels) Peristaltic activity in GI tract involves coordinated contraction proximal to mechanical stimulation from bolus and relaxation distal to stimulation |
|
|
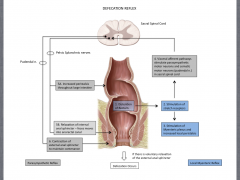
Describe the defecation reflex in regards to the parasympathetic reflex and the local myenteric reflex.
|
|
|
|
Describe the anatomical structure of the diaphragm, its neurovascular supply and the structures that pass through it.
|
It is a musculotendinous sheath that separates the thoracic cavity from the abdominal cavity; has a central tendinous part around which the muscle fibers attach
---anchored to lumbar vertebrae by crura (right/left), which are connected together by the median arcuate ligament Blood supply: ---superiorly: musculophrenic and pericardiacophrenic arteries (branches of internal thoracic), superior phrenic artery (branch of thoracic aorta) ---inferiorly: inferior phrenic arteries (branches of abdominal aorta) Innervation: phrenic nerves (C3-C5) Structures passing through: ---aorta: between crura; thoracic duct and azygos vein: accompany aorta; esophagus: through musculature to left of aortic hiatus; anterior/posterior vagal trunks, esophageal branches of left gastric vein, lymphatics: pass with esophagus; inferior vena cava: through central tendinous part; right phrenic nerve: accompanies IVC; left phrenic nerve: pass through musculature; greater/lesser splanchnic nerves; hemiazygos vein, sympathetic trunks/least splanchnic nerves; superior epigastric vessels; other vessels, nerves |
|
|
Describe the kidney's location in the body, their gross internal structure and their neurovascular supply.
|
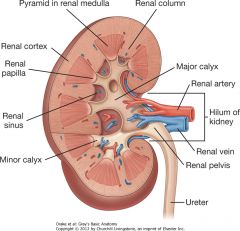
They are retroperitoneal, immediately lateral to the vertebral column from T12 to L3.
Structure: has smooth anterior/posterior outer surface covered by fibrous capsule ---Renal cortex: outer layer, with projections (renal columns) into the inner layer; continuous band of pale tissue ---Renal medulla: inner layer, divided into renal pyramids by outer layer ---Renal sinus: inner core (entrance/exit), apex of renal pyramids point in towards it, forming renal papilla ---Minor calyx: surround the renal papilla; receive urine; are proximal parts of tube that becomes ureter ---Major calyx: groups of minor calyx that merged together ---Renal pelvis: where major calyx come together, forming superior end of ureters Blood supply: ---Arteries: single large renal artery (branch of abdominal aorta); left usually higher than right, right longer; each divide into anterior/posterior branches; can also have accessory renal arteries (extrahilar) ---Veins: multiple veins contribute to left/right real veins (anterior to arteries); left is longer, passing anterior to aorta/posterior to superior mesenteric artery Innervation: ---sympathetic: (T10-T11/T12) preganglionic - lesser splanchnic and least splanchnic; postganglionic - renal plexus (from aorticorenal ganglia) ---parasympathetic: vagus nerve |
|
|
Describe the structure and neurovasculature of the ureters. Trace their path from kidney to bladder.
|
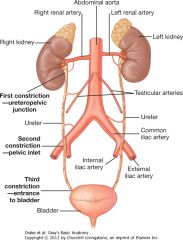
They are muscular tubes that are continuous with the renal pelvis
Blood supply: ---Arteries: receive arterial branches from adjacent vessels (renal arteries; abdominal aorta/common iliac arteries; internal iliac arteries); all form longitudinal anastomoses Innervation: from renal, aortic, superior/inferior hypogastric plexuses through nerves that follow blood vessels; visceral afferents follow sympathetic nerves back to T11 to L2 (pain is felt at these cutaneous levels) Pathway: ---renal pelvis exits kidney through hilum, becomes continuous with uterer at ureteropelvic junction and descends retroperitoneally on medial aspect of psoas major ---at pelvic brim, cross common iliac/external iliac arteries to enter pelvic cavity and continue to bladder ---Have three constriction points: 1. ureteropelvic junction 2. crossing of common iliac vessels at pelvic brim 3. where ureters enter wall of bladder |
|
|
Describe the major branches of the abdominal aorta and its course through the abdomen.
|
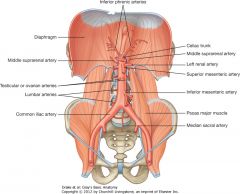
It begins at aortic hiatus in the diaphragm and ends when it splits into the left/right common iliac arteries at L4
Three types of branches: 1. visceral: supply organs (paired/Unpaired) ---Celiac trunk: supplies foregut ---Superior mesenteric artery: supplies midgut ---Inferior mesenteric artery: supplies hindgut ---middle suprarenal arteries: small, lateral, arise above renal arteries; supply adrenal glands ---renal arteries: lateral, arise inferior to superior mesenteric artery; supply kidneys ---testicular/ovarian arteries: anterior, arise inferior to renal arteries, pass lateral on psoas major 2. posterior: supplies diaphragm or body wall ---inferior phrenic arteries: arise inferior to aortic hiatus, ascend to supply portion of suprarenal glands and inferior surface of diaphragm ---lumbar arteries: four pairs, arise on posterior, pass around vertebral column to abdominal wall ---median sacral artery: on posterior, just superior to bifurcation, passes over lower lumbar, sacrum, and coccyx 3. terminal: ---common iliac arteries: split of the abdominal aorta produces them |
|
|
Identify the major branches of the inferior vena cava and describe its course through the abdomen.
|
It is formed from the joining of the common iliac veins at L5, to right of midline; ascends anterior to vertebral column to right of abdominal aorta; leaves abdomen through central tendon of diaphragm
Major tributaries: ---common iliac veins, lumbar veins, right testicular/ovarian veins, renal veins, right suprarenal vein, inferior phrenic veins, hepatic veins ***ascending lumbar veins provide anastomoses between common iliac, iliolumbar and lumbar veins to azygos system (in case IVC is blocked)*** |
|
|
Identify and describe the adult structures derived from the embryonic foregut.
|
It is from the oral cavity to the 2nd part of duodenum (pharyngeal: oral cavity to diaphragm/foregut proper: diaphragm to duodenum):
---Pharynx, lungs, esophagus, stomach, first part of duodenum, liver, gall bladder, bile duct system, pancreas |
|
|
Identify and describe the adult structures derived form the embryonic midgut.
|
It is from the end of foregut to distal portion of transverse colon
---Second portion of duodenum, jejunum, ileum, cecum, appendix, ascending colon, proximal 2/3 of transverse colon |
|
|
Identify and describe the adult structures derived form the embryonic hindgut.
|
It is from end of midgut to anus
---distal 1/3 of transverse colon, descending colon, sigmoid colon, rectum, superior part of anal canal, epithelium of urinary bladder/most of urethra |
|
|
What forms the primitive gut tube?
|
Endodermal germ layer: inner layer that forms the epithelium lining (mucosa) of the gut and epithelial components of its glandular derivatives (pancreas, gall bladder, liver (hepatocytes) and bile duct)
Mesodermal germ layer: ---splanchnic lateral plate forms visceral peritoneum, submucosa and muscularis externa, all other components of gut tube wall (except nerves/ganglia - ectoderm) ---somatic lateral plate forms parietal peritoneum ------together, both form dorsal/ventral mesentery |
|
|
How is the gut tube separated from the amniotic cavity?
|
Oral and cloacal membranes provide separation
---occur where ectoderm and endoderm are directly opposed Stomadeum (mouth) and proctodeum (anus) are ectodermal depressions at cranial/caudal ends |
|
|
When and how does the oral membrane rupture?
|
Occurs by apoptosis during the 4th week
|
|
|
What are the three arteries that divide the gut tube and where do they anastomose?
|
Unpaired ventral branches from abdominal aorta:
---celiac trunk (foregut), superior mesenteric artery (midgut), inferior mesenteric artery (hindgut) At foregut/midgut junction: ---celiac/superior mesenteric anastomose through superior pancreaticoduodenal artery (from gastroduodenal) and inferior pancreaticoduodenal artery At midgut-hindgut junction: ---superior mesenteric/inferior mesenteric anastomose through branches of middle colic artery and branches of the left colic artery (at splenic flexure) |
|
|
Describe the formation of the greater omentum.
|
Dorsal mesentery connects gut tube with posterior body wall: forms greater omentum
---composed of double layer of peritoneum, with vessels/nerves running through ---it is where somatic/splanchnic mesoderm are continuous Position: ---altered by growth/rotation of stomach: rotates 90* clockwise onto right side (faces posterior); original posterior side grows faster, creating greater/lesser curvatures (greater omentum originates from dorsal mesogastrium on greater curvature) ---grows over transverse colon, extending like an apron |
|
|
Describe the formation of the lesser omentum.
|
Most of ventral mesentery died off because it had no blood vessels
---however, liver develops into ventral mesentery, separating it into two parts: 1. falciform ligament: between ventral body wall and liver (free margin contains umbilical vein which becomes the ligamentum teres hepatis) 2. lesser omentum between liver and stomach/duodenum ---connections formed between the liver/duodenum (and pancreas/duodenum) are endodermal because they are duct systems ---lesser omentum attaches to lesser curvature of stomach, forming the lesser peritoneal sac/omental bursa (continuous with greater omentum in embryo, eventually space mostly fuses together |
|
|
Where do the fusions of the greater omentum occur and what to they result in?
|
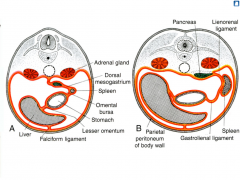
---transverse mesocolon fuses to the posterior surface of the greater omentum
---portions of dorsal mesogastrium fuse with posterior body wall, forming ligaments: ------splenorenal ligament: left kidney and spleen ------gastrosplenic ligament: spleen and stomach ------retroperitoneal pancreas (starts intraperitoneal, stomach rotation pushes it to posterior wall where omentum fuses) |
|
|
Where does the spleen develop?
|
It develops in the dorsal mesogastrium
|
|
|
What are the symptoms and clinical etiology of an abdominal aortic aneurysm?
|
It is a dilation of the aorta, tends to occur in the infrarenal region, retroperitoneally; usually occurs in atherosclerotic elderly males
---as aorta expands, risk of rupture increases Symptoms: sudden onset of severe, central abdominal pain, which may radiate to back and a pulsatile tender abdominal mass; if rupture occurs, hypotension and delirium may occur |
|
|
Describe the formation of the liver. Which germ layers form which parts?
|
It grows into the septum transversum (ventral mesentery); develops between heart and midgut
---septum transversum is splanchnic mesoderm (starts above the cardiogenic area before head folding) Develops where veins approach the heart; veins form the sinus venosus ---cardinal veins from embryo ---vitelline veins form yolk sac ---umbilical veins from placenta Liver cells surround the veins: ---vitelline veins become hepatic sinusoids, hepatic veins, ductus venosus (becomes ligamentum venosum between caudate and left lobes), hepatic part of IVC, portal vein and SMV ---left umbilical vein: carries blood from placenta to liver, hooks up to ductus venosus; becomes ligamentum teres hepatis Hepatocytes: formed from endoderm Sinusoids/blood vessels/etc: formed from mesoderm Bare area: forms as liver and central diaphragm develop from septum transversum ---mesoderm on surface of liver differentiates into visceral peritoneum except on cranial surface (in contact with developing central tendon of diaphragm, so no covering ***only the tendon is from septum transversum (splanchnic mesoderm), muscle portion is from somatic mesoderm*** |
|
|
Describe the development of the pancreas.
|
Dorsal and ventral buds unite to form pancreas
---grow out of foregut endoderm: forms acinar cells and ducts (exocrine) ---surrounding mesoderm: forms islet cells (endocrine) Clockwise rotation of foregut moves ventral bud (uncinate process/head) dorsally to fuse with dorsal bud ---gallbladder buds off above ventral pancreatic bud, from liver bud |
|
|
What happens with the two buds of the pancreas don't fuse normally?
|
Annular (ring) pancreas:
---ventral bud has two parts that normally fuse then rotate dorsally ---if they move in opposite directions, can surround the duodenum, causing constrictions and obstruction |
|
|
Describe the rotation of the midgut.
|
Midgut loop grows rapidly and extends into the umbilical cord (physiological herniation)
---forms a U-shaped primary loop at wk 6: cranial limb forms jejunum and upper ileum; caudal limb forms lower ileum to proximal 2/3 transverse colon Rotation: counterclockwise 270* ---allows midgut to fit in abdominal cavity; elongation continues during rotation ---SMA serves as axis of rotation: rotates 90* during herniation and 180* during return to abdominal cavity (during wk 10) ---proximal jejunum returns first to left, remaining loops return to right ---cecum returns last and moves from right upper quadrant to right iliac fossa; places ascending colon on right; appendix develops during descent so position varies Fixation of dorsal mesentery: ---rotation twists dorsal mesentery around origin of SMA ---mesentery of ascending and descending colon is pressed against/fuses with posterior abdominal wall (secondarily retroperitoneal) ---transverse mesocolon fuses with posterior wall of greater omentum ---mesentery of jejunoileal loops attach diagonally from ileocecal junction to duodenal-jejunal junction |
|
|
What are some problems that can occur during midgut rotation?
|
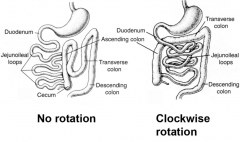
No rotation:
---midgut loop rotates 90*, positioning small intestine on right and large intestine on left, but no 180* rotation Clockwise rotation: ---large intestine enters cavity first so it is posterior to the duodenum and SMA ---this can lead to the small intestine constricting the large intestine |
|
|
What are some defects that occur during GI development?
|
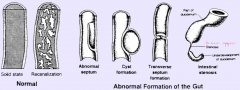
Incomplete recanalization:
---lumen of GI tract is occluded early in 2nd month due to epithelial proliferation/migration; recanalization occurs as vacuoles appear and coalesce due to apoptosis (mesodermal projections into epithelium: forms villi; endodermal invagination into mesoderm: forms crypts) ---stenosis/duplication can result (four main issues) |
|
What is this defect, what caused it and what are its problems?
|
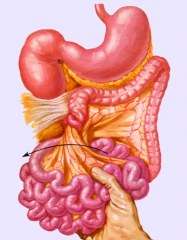
Volvulus:
---twisting of the small intestine around the axis of the mesentery is caused by malrotation ---can cut off blood supply and lead to blockages |
|

Describe this defect.
|
Intussusception:
---segment of intestine invaginates or telescopes into adjacent segment. |
|
Describe this defect in GI development.
|
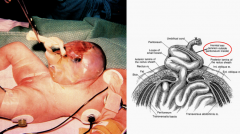
Omphalocele:
---herniation of the intestine or other viscera through umbilical ring; covered by thin peritoneal sac and amnion ---usually associated with other congenital anomalies (2.5/10000 births) |
|
Describe this defect in GI development.
|
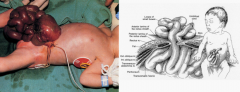
Gastroschisis:
---defect in anterior abdominal wall leading to herniation of intestine/other viscera; not covered by peritoneal sac (but visceral pleura is present) - leads to problems with infection ---not usually associated with other congenital anomalies (1/10000 births) |
|
Describe this defect in GI development.
|
Meckel's (ileal) diverticulum:
---persistant yolk stalk; present in 2% of population and twice as common in men; most have no symptoms but gastric mucosa may be present which leads to ulceration, perforation or GI bleeding ------connection between gut tube and yolk sac (yolk stalk) narrows to become vitelline duct; remains attached to midgut for some time |
|

Describe the defect in GI development.
|
Aganglionic megacolon (Hirschsprung's disease):
---lack of parasympathetic ganglia in myenteric plexus distal to dilated portion of colon; 80% of cases involve rectum to mid-sigmoid colon; caused by defect in RET gene (receptor tyrosine kinase involved in neural crest cell migration - moves cranial to caudal during 5th to 7th wks) |
|
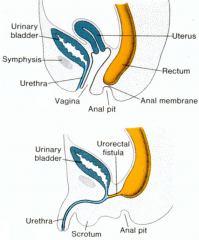
Describe this defect in GI development.
|
Imperforate anus:
---can result from abnormal development of urorectal septum (divides cloaca into bladder and anorectal canal) ---failure of cloacal membrane to perforate at 8 wks; lack of recanalization of distal hindgut |
|
|
Describe the overall organization of the GI tract and identify the different histological layers.
|
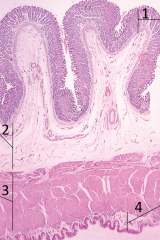
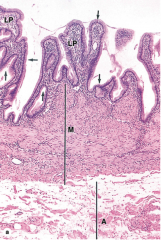
GI Tract Organs: esophagus, stomach, small intestine, large intestine
---functions: swallowing, digestion, absorption, waste removal, immune surveillance 1. Mucosa: inner lining ---epithelium: stratified squamous/columnar (depends on location) ---lamina propria: connective tissue with associated lymph/vascular structures ---muscularis mucosa: smooth muscle cells 2. Submucosa: middle layer ---fibroelastic loose connective tissue; associated vascular, lymph, autonomic nerve plexus (submucosal plexus) and fat (glands) 3. Muscularis externa: muscular outer layer ---smooth muscle: inner circular, outer longitudinal layers; had autonomic nerve plexus (myenteric plexus) 4. Serosa/adventitia: outer lining ---loose connective tissue ------only connective: adventitia (retroperitoneal) ------connective and mesothelial covering (visceral peritoneum): serosa |
|
|
Describe the structures and cell types of the esophagus as well as its specializations.
|
---Non-keratinized stratified squamous epithelium
---muscularis externa: proximal third skeletal muscle, middle third combination of skeletal and smooth, distal third smooth muscle ---lubrication by mucous glands in submucosa ---covered by adventitia (serosa covers portion in abdominal cavity) |
|
|
Describe the structures and cell types of the stomach and its specializations.
|
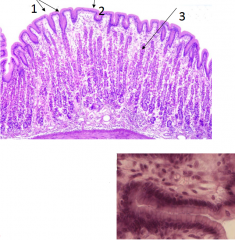
----surface eptithelium: simple columnar; forms mucus (cells stain light because don't do absorption, so don't need lots of stuff)
---gastric pits: invagination of surface epithelium into lamina propria ---gastric glands: epithelial-lined tubular glands empty into gastric pits ***contains enteric nerve plexus (submucosal and myenteric)*** |
|
|
Describe the gastric glands in the stomach.
|
Surface lining cells: produce mucus
Regenerative cells: replace all cell types Mucous neck cells: produce mucus Parietal cells: dark staining; intrinsic factor for uptake of Vit B12 in small intestine; produces HCl Chief cells: light staining; produce HCl, pepsinogen (which HCl actives to pepsin) and lipase/leptin Enteroendocrine cells: produce gastrin (stimulates parietal prod. of HCl), serotonin (gut motlility) and somatostatin (endocrine regulation) |
|
|
Describe the structure and cell types of the small intestine and its specializations.
|

Involved in terminal digestion, nutrient absorption* and endocrine secretion
---villi: simple columnar epithelium with microvilli; form cicular folds (circularis plicae) - increase surface area ---paneth cells: within crypts and provide innate immunity; produce lysozyme, phospholipase and defensins |
|
|
What are the specializations within the duodenum?
|
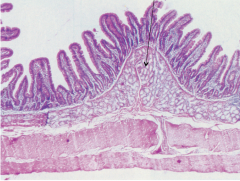
Brunner's glands: found in submucosa, secrete alkaline product to neutralize chyme
|
|
|
What are the specializations within the ileum?
|
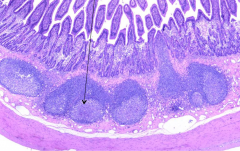
Peyer's patches: accumulation of lymphoid nodules in submucosa
|
|
|
Describe the absorption of different molecules in the small intestine.
|

Carbohydrates and proteins:
---broken down into monosaccharides and amino acids ---actively transported through intestine to blood stream Lipids: ---bile acids and lipase break down lipids into glycerol, fatty acids and monoglyercides ---absorbed through villi, then resynthesized into triglycerides in SER; synthesis of protein in RER and synthesis of glyco- and lipoproteins in golgi ---triglyceride and (lipo)protein cover creates chylomicron which exits small intestine to blood stream |
|
|
Describe the hormones produced by the enteroendocrine cells.
|
Secretin: affects pancreas and gall bladder - bicarbonate and water secretion
Gastric inhibitory peptide (GIP): affects stomach - inhibition of acid secretion Glucagon-like peptide (GLP-1): affects CNS - decrease sense of hunger Cholecystokinin (CCK): affects pancreas - enzyme secretion; affects gall bladder - contraction Motilin: affects GI tract - increased motility Vasoactive intestinal peptide (VIP): affects GI tract - increased motility |
|
|
Describe the structure and cell type of the large intestine and its specializations.
|
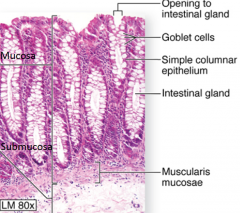
Function: absorption of water*; formation of fecal mass from undigested material; production of mucus for lubrication of intestinal surface
---simple columnar epithelium with no villi and many crypts/goblet cells; epithelium has quick turn over, so large number of stem cells in mucosa) Four major cell types: ---enterocytes ---goblet cells ---stem cells ---enteroendocrine cells |
|
|
Describe the structure and function of the salivary glands.
|

Secrete in response to parasympathetic stimuli
---produce hypotonic solution containing variable amounts of mucus, enzymes, antibodies and ions Two types of cells: ---serous: darker staining with rounded nuclei; secrete protein and digestive enzymes ---mucus: lighter staining with flattened nuclei; produce mucus for lubrication Intralobular ducts: ---secretory endpieces empty into intercalcated discs (cuboidal epithelium), which join to form striated ducts (columnar epithelium) Interlobular ducts: ---located in connective tissue separating each lobule; initially lined with pseudostratified/stratified cuboidal epithelium leading to only stratified cuboidal with few mucous cells |
|
|
Describe the structure and function of the pancreas. How does secretion/flow of enzymes work?
|

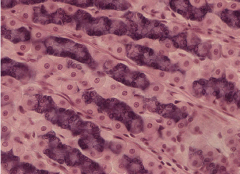
Mixed exocrine and endocrine gland producing digestive enzymes and hormones
1. Endocrine: islet of Langerhans (different types) produce insulin, glucagon and somatostatin ---lighter staining, clump of cells ---secreted through blood stream to reach targets |
|
|
Describe the structure and function of the liver.
|
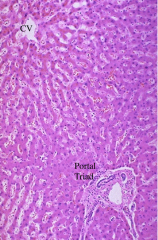
Function: synthesis of cholesterol and plasma proteins; glucose and lipid metabolism; inactivation/detoxification of various substances (alcohol, hormones, drugs); production of bile (exocrine: ~1 L/day)
---hepatocytes are organized into structures surrounding the central vein, with sinusoids (fenestrated endothelial/Kupffer cells) between them; space between two is perisinusoidal (space of Disse) which has lymph and hormones Portal triad: portal vein, portal artery, bile duct ---all GI tract blood passes through liver to vena cava |
|
|
Describe the functional organization of liver lobules.
|

Three related ways to view the liver's organization, each emphasizing different aspects of hepatocyte activity.
|
|
|
Describe the structure and function of the gall bladder.
|
Function: store, concentrate and release bile
---concentration is an osmotic event driven by flow of sodium ions ---release is driven by CCK released from enteroendocrine cells of small intestine in response to presence of dietary fats (muscularis contracts) |
|
|
Describe the problems gall stones can cause.
|
Cholelithiasis: presence of stones in gall bladder
Choledocholithiasis: presence of stones in common bile duct ---develop as a result of changes in solubility that lead to precipitation of cholesterol and calcium salts ---predisposing factors: Age >40, female, estrogen therapy, obesity, rapid weight loss, pregnancy, diabetes, total parenteral nutrition and octreotide use, living in dry climate |
|
|
Describe the structure and function of a nephron.
|
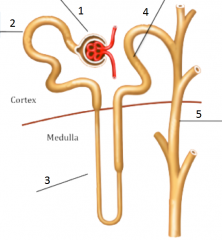
Basic functional unit of the kidney: together with the collecting duct (which is shared with other nephrons) is uriniferous tubule
Composed of: 1. Renal corpuscle: glomerulus and glomerular (Bowman's) capsule ---filtration from blood into nephron; high capillary pressure (55 mmHg) 2. Proximal convoluted tubule (PCT): ---reabsorption of water, amino acids, glucose, urea, HCO3- and electrolytes from fluid to blood 3. Loop of Henle: --- (ascending loop) secretion of K+ and NaCl in creation of hypertonic gradient in interstitium; (descending loop) reabsorption of water from fluid to blood 4. Distal collecting tubule (DCT): ---reabsorption of water, Na+, HCO3-; excretion of NH4+ and H+ 5. Collecting duct ---controlled reabsorption of water under influence of ADH (concentration of urine) |
|
|
Describe the function of the urinary system.
|
Important in maintaining composition of various fluid compartments of body for optimal function; acts only on blood plasma
---excretion of metabolic waste, toxins, foreign substances and other substances such as hormones ---regulation of blood osmolarity ---regulation of blood pressure/volume ---regulation of blood pH ---manufacture of substances involved with: RBC production (erythropoetin), bone/calcium maintenance (calcitriol) and blood pressure (renin, medullipin I) Processes: filtration, reabsorption, secretion, elimination and manufacture ---only 1% of filtrate is eliminated |
|
|
Describe the arteriole portal system found around uriniferous tubules.
|
afferent arteriole > glomerulus > efferent arteriole > capillaries
---peritubular capillaries surround PCT/DCT and in cortical nephrons (found mostly in cortex), also surround loop of Henle ---vasa recta: surround loop of Henle in juxtamedullary nephrons (with loop of Henle mostly with in medulla); |
|
|
What are podocytes?
|
They are a visceral layer of cells that line Bowman's capsule around glomerulus
|
|
|
How is filtration regulated in the Bowman's capsule?
|
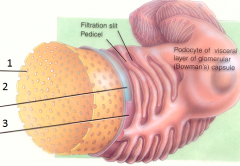
Three layers:
1. endothelial fenestrations of glomerulus (pores relatively small): prevents filtration of blood cells but allows all other components of plasma to pass 2. basement membrane: prevents filtration of larger proteins 3. slit membrane between pedicels: prevents filtration of medium-sized proteins ---all under high pressure; once filtrate passes through, enters Bowman's space and moves into PCT |
|
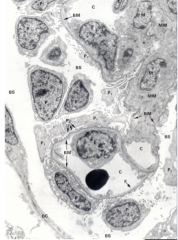
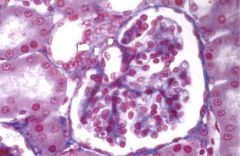
Identify the cells in the renal corpuscle.
|
BC: parietal layer (simple squamous epithelium) of Bowman's capsule
E: endothelium (nucleus) of capillaries C: lumen of capillaries P: podocytes (visceral layer) MM: mesangium (intraglomerular); modified smooth muscle cells, provide physical support for capillaries, maintain filtration slits by phagocytic activity, contractile properties regulate blood flow (capillary blood pressure), and secretion (in response to injury) BS: Bowman's space |
|
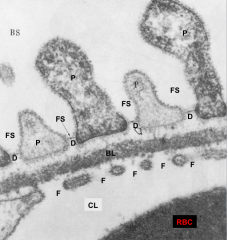
Identify the filtration barrier components.
|
CL: capillary lumen
F: fenestrations of endothelium BL: basal lamina (type IV collagen, fibronectin, lamimin, heparan sulfate, negatively charged to prevent movement of proteins/AA) P: podocyte foot process FS: filtration slit D: diaphragm of slit BS: Bowman's space |
|
|
What are the different cell types for each portion of a nephron?
|
Glomerular capsule: parietal layer - simple squamous epithelium
PCT: simple cuboidal with microvilli (brush border); needs increased SA for resorption/secretion Loop of Henle: ---thin descending limb: simple squamous ---thick ascending limb: simple cuboidal with sparse microvilli DCT: simple cuboidal with sparse microvilli Collecting duct: fat cuboidal/columnar |
|
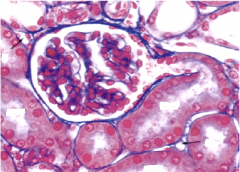
Identify renal corpuscle, PCT, DCT and capillaries.
|
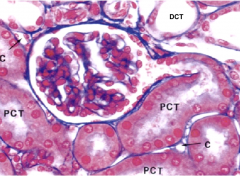
|
|
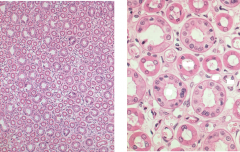
Identify the loops of Henle, collecting ducts and vasa recta.
|
All found in medulla
|
|
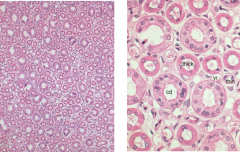
Identify and explain the components of the juxtaglomerular apparatus.
|
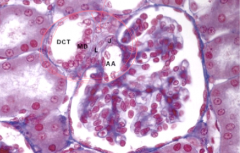
Found between the DCT and glomerular capsule; important for blood pressure regulation
DCT: distal convoluted tubule MD: macula densa - contains osmoreceptor which samples Na+ in DCT AA: afferent arteriole - contains baroreceptor for measuring blood pressure J: juxtaglomerular cells - modified smooth muscle cells of tunica media of AA; manufacture and secrete renin (stimulate increase in blood pressure) L: lacis cells (extraglomerular mesangium - communicate with J via gap junctions; connection mechanism to MD speculative |
|
|
Describe the affect of renin on blood pressure.
|
Renin cleaves angiotensinogen (produced by liver, circulating) to form angiotensin I
ACE (angiotensin converting enzyme; produced by endothelial cells of lungs/kidneys) converts angiotensin I into angiotensin II Angiotensin II: ---stimulates aldosterone release from adrenal glands which stimulates reabsorption of NaCl by DCT and collecting duct ---stimulates ADH (vasopressin) release from posterior pituitary which increase water reabsorption by increasing permeability of collecting duct ---increases thirst ---constricts arterioles ---increases blood pressure |
|
|
Trace the flow of filtrate from Bowman's space to urethra.
|
PCT > Loop of Henle (descending/ascending) > DCT > Collecting Duct > Ducts of Bellini (merged collecting ducts) > exit pyramids through papilla (now urine) > minor calyces > major calyces > renal pelvis > urethra
|
|
|
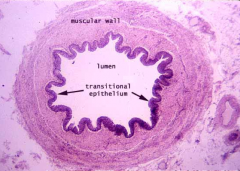
Describe the structure of a ureter.
|

Continuous with renal pelvis (formed from minor/major calyces which are lined with transitional epithelium)
---Mucosa: lined with transitional epithelium, has lamina propria and mucous glands ---Muscular layers: longitudinal (inner), circular (outer) and distal 1/3 has extra longitudinal layer ---Adventitia: has vaso vasorum |
|
|
Describe the structure of the urinary bladder.
|
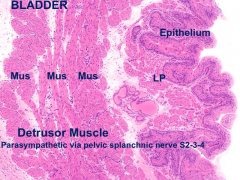
Lined with transitional epithelium; three layers of muscle
Detrusor muscle: outer muscle surrounding bladder; controlled by parasympathetic pelvic splanchnic nerves Internal urethral sphincter: not strong in females, can be absent; controlled by sympathetic hypogastric nerves External urethral sphincter: part of UG diaphragm; controlled by somatic pudendal nerves Urogenital (UG) diaphragm: muscular wall fused to pelvis |
|
|
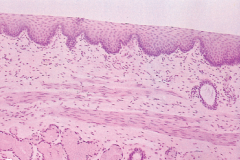
Describe the structure of the urethra.
|
Initially transitional epithelium, changes to stratified/pseudostratified columnar and becomes simple squamous epithelium at termination to blend with stratified squamous of outer eptithelium
|

