![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
191 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Skeletal Muscles |
Muscles attached to our bones and allow us to move those bones These mucsles are striated |
|
|
|
Cardiac Muscle |
it is specailized and only found in the heart. This muscle is striated. |
|
|
|
Smooth Muscles |
These line the tubes of our body. They work involuntaryly. Not straited. ex: digestive tract and blood vessels |
|
|
|
Straiated vs Unstraiated |
Straiated: muscles that have repeating layers of thicker and thinner cell density. This makes the muscle look like it has stripes. Ubstriated: the cell density is the same throught the cell |
|
|
|
Motor Unit |
one motor neuron and all of the muscle cells it intervates |
|
|
|
Muscle Cell =Muscle Fiber |
Made up of repeating units of sacromeres |
|
|
|
Sacromere |
Made up of actin and myosin. They have z-lines and a m-line |
|
|
|
Actin |
Also called the 'thin filament' because it has a smaller diamter than myosin |
|
|
|
Myosin |
Also called thick filament because it has a bigger diamter than actin. It is also considered the powerhouse of the muscle cell. They have heart shaped projections called myosin heads or myosin cross-bridges. The heads protrude everywhere on the filament |
|
|
|
How Sacromere contracts (see pg 42) PART 1 |
-AZ-line runs across the sacromere to B Z-line -M-line just runs down the mid of Sacromere -Actin is attchd. to the z-lines/z-discs but don't touch each other in the middle -Myosin is centered in the mid of the sacromere but does not run across the sacromere and touch the z-lines/discs. -Myosin and Actin don't quite overlap but they connect to each other by myosin heads and actin fillaments. They create a cross bridge fromation which allows myosin pull actin to the m-line. |
|
|
|
Tropomyosin |
Thing that encircles the actin filament |
|
|
|
How a f*cking muscle f*cking contracts part 2 |
-Tropomyosin covers up the myosin binding sites on the actin filament preventing cross-bridge formation which inhibits the sacromere from contracting. -Brain sends out a impulse via the motor neuron which innervates the muscle cell at the transverse tubules. -The transverse tubles then depolarize which cause the whole cell to depolarize. |
|
|
|
Troponin |
A thing that is bound to the tropomyosin and regulates the positioning of the tropomyosin and whether it blocks the myosin binding site or not. |
|
|
|
How a f*cking muscle f*cking contracts part 3 |
-Depolarization of the cell causes the sarcoplasmic recticulum to release its Ca2+ stores. - Ca2+ binds to troponin causing troponin Ca2+ complex to shift tropomyosin off the myosin cross-bridge binding site. -Myosin is now able to attach to the actin filaments forming cross-bridges and plls the actin filaments towards the m-line, shortening the sacromere and thus the muscle cell. |
|
|
|
What is a major source of energy for the muscle contraction? |
ATP |
|
|
|
ATP has three jobs: |
1)Helps myosin cross-bridge to pull actin toward the m-line. 2) Helps myosin head release the actin filament so it can reattach futher down the filament. 3) When the muscle is relaxing, ATP activates the Ca2+ ATPase pump to pump Ca2+ back into tje sacroplasmic reticulum for storage. |
|
|
|
neural control of a muscle involves |
1) # of motor units being stimulated (strength of stimulus) 2) the frequency of the stimulation (the speed of the stimulation) 3) The duration (length of time) of the stimulation |
|
|
|
amplitude |
strength of muscle twitch |
|
|
|
Tetanus |
the strongest contraction possible for a muscle |
|
|
|
inhibition |
a limp muscle effect no matter how hard you try to contract it |
|
|
|
Cardiovascular System |
Heart and Blood Vessels |
|
|
|
Heart |
Has: Two Atria Two Ventricles |
|
|
|
Atria |
smaller in size with thinner less muscular walls |
|
|
|
Ventricles |
Larger, thicker, and more muscular because they are pumping chambers of the heart. |
|
|
|
Vena Cavae |
Deoxygenate blood enters the heart *VIA THE VENA CAVAE* which is also the largest vein in the body. Blood here dumps into the Right atrium |
|
|
|
Pulmonary Valve |
This is the valve at which blood the right ventricle and closes so that the right ventricle can fill with blood. |
|
|
|
Pulmonary Arteries |
they take blood to the lungs, where CO2 will be exchanged for O2. *Oxygenated blood returns to the heart via the pulmonary veins. |
|
|
|
Pulmonary Vein |
Dumps the oxygenated (the only vein in adults to carry oxygenated blood) blood into the left atrium. |
|
|
|
What order does blood flow? |
1) Capillaries 2) Venules 3) Veins 4) Vena Cavae 5) Right Atrium 6) Trisupsid Valve 7) Right Ventricle 8) Pulmonary Semilunar Valve 9) Pulmonary Arteries 10) Lungs ~pulmonary capallaries 11) Pulmonary Veins |
13) Left AV Valve Bicuspid 14) 15) Aortic Semilunar Valve 16) Aorta/Aortic Arch 17) Arteries 18) Arterioles 19) Back to Cappillaries |
|
|
Systole |
describes when the cardiac muscle tissue when it is contracting. -When Atria go through the systole phase, they push blood into the ventricles -When the ventricles go through the systole phase, they eject bolld into the arteries -In the diastolic phases, atria and ventricles fill with blood passively. |
|
|
|
ECG |
Electro Cardio Gram measures the electrical current of the depolarized heart. |
|
|
|
Fun facts about arteries
|
-They go away from the heart -They're small to large -Thick -High Pressure |
|
|
|
Fun Facts about Vein |
- Goes to Heart - Small to large - Thin muscle lining -low pressure |
|
|
|
Heart Rate |
The number of heart beats per minute |
|
|
|
Calculation for Target Heart Rate |
% exercise intensity (220-Age-Resting heart rate)+ resting heart rate |
-THR=%exercise (220-21-70)+70 -THR=0.60 (129)+70 -THR=77.4+70 -THR= 147.4 B.P.M. Target Heart Rate in 10 seconds= 24.5 or 25 beats in 10 seconds |
|
|
"LUB" |
-sound occurs during the systole phase and is produced when the AV valves slam closed to prevent the blood from flowing back up into the atria |
|
|
|
"Dub" |
happens when sound occurs during the diastole phase and is produced when the pilmonary and aortic valves slam closed to prevent blood from flowing back into the ventricles from the pulmonary and aortic arteries. |
|
|
|
How do you measure blood pressure? |
Blood Pressure: Systolic Number ----------------------------- Diastolic Number |
B.P.= 120 ------- 70 |
|
|
How do you measure Pulse Pressure? |
Pulse pressure is the difference between the systolic and diastolic pressures |
|
|
|
What is MAP? How do you measure Mean Arterial Pressure (MAP)? |
MAP is the average of arterial pressure during a cardia cycle.* The period of diastole is about twice as long as systole. MAP= Diastolic pressure+1/3 pulse pressure. mmhg |
|
|
|
How to measure Cardiac Output Measurement? |
Cardiac Output= the volume of blood in milliliters that is pumped by the heart per unit if time (per minute). It is calculated by multiplying heart rate by stroke volume. |
-150 lbs divided by 2.2 lbs =68 kg -68 kg x 0.92= 62.5 ml/min of stroke volume -heart rate x stroke volume = cardiac output |
|
|
How do you measure Total Peripheral Resistance Measurement? |
Total Peripheral Resistance is a determinate of mean arterial pressure. It represents the pressure that your heart must overcome during ventricular contraction
|
TPR=MAP/Cadiac Output TPR__mmHg/ml/min |
|
|
Alveoli
|
Small pouches of the lungs with capillaries; this is where the oxygen and carbon dioxide transfer occurs between the lungs and the blood. |
blood dumps off its carbon dioxide into the lungs and picks up oxygen. |
|
|
Dead Air Space 'air |
air that cannot be completely inhaled into the lungs and the air that cannot be fully exhaled from our body is approximately 0.15 liters for an adult human. |
|
|
|
Residual Volume |
This is the air that cannot leave the lungs, even when the lungs contract. The lungs do this so they don't stick together, when they stick together the lungs will collaspe. |
There are 1.2 liters of residual volume in an adult
|
|
|
DRAW OUT |
THE |
PULMONARY SYSTEM |
|
|
What is the lung capacity at maximum inflation? |
5700ML |
|
|
|
What is the average lung volume in normal quiet breathing? |
~normal breathing~ Inspiration: 2700ml Expiration: 2200ml *Diff btwn end expiratory and end-inspiratory volume equals tidal volume (ave. 500 ml) |
|
|
|
What is the minimal lung volume (residual volune) at maximal deflation? |
1200ml |
|
|
|
Graph of Normal healthy young male |
TV= Tidal Volume, 500 ml IRV= Inspiratory reserve volume, 3000ml IC= Inspiratory Capacity, 3500 ml ERV= Expiratory reserve volume, 1000ml FRC= Functional Residual Capacity, 2200ml VC= Vital Capacity, 4500ml TLC= Total Lung Capacity, 5700ml |
|
|
|
What does the exchange of 02 and C02 rely on? Where does it take place? |
A) Diffusion btwn air and blood B) Aveolar air and blood takes place at the pulmonary capillaries. |
|
|
|
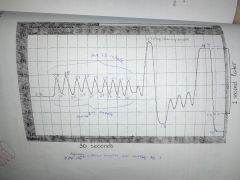
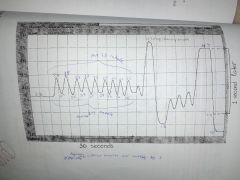
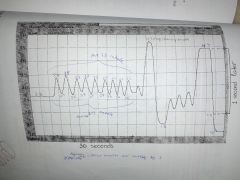
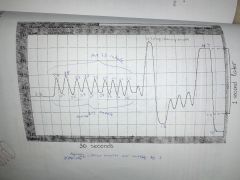
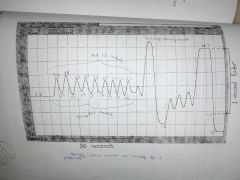
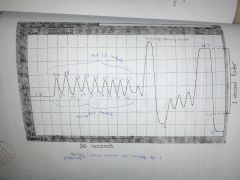
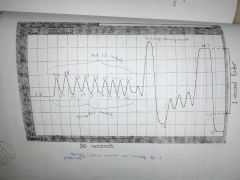
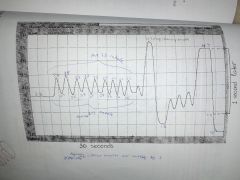
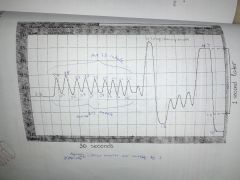
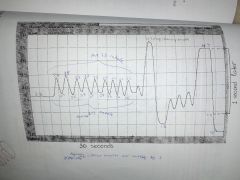
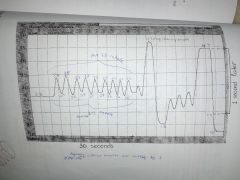
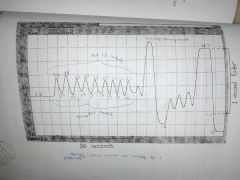
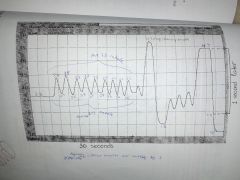
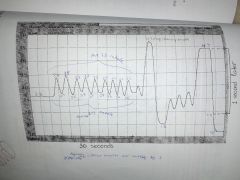
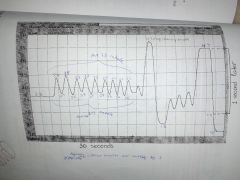
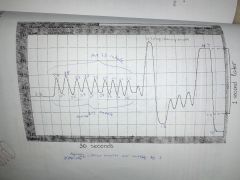
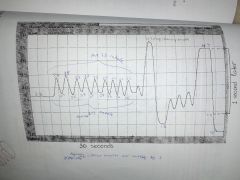
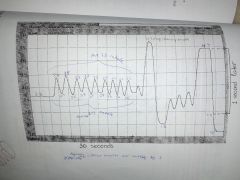
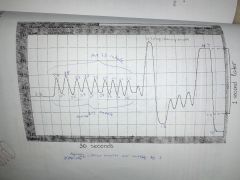
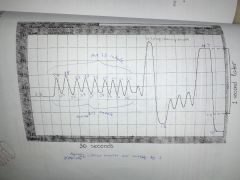
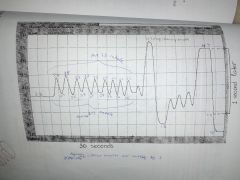
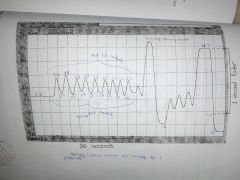
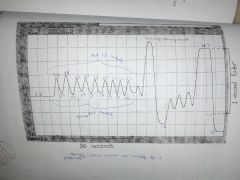
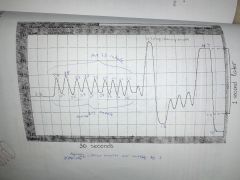
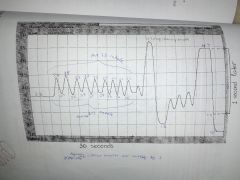
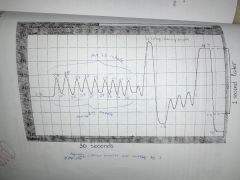
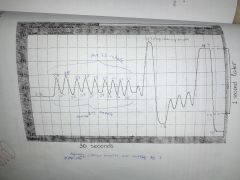
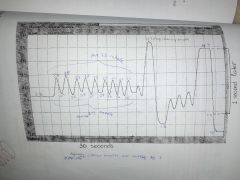
When reading a spirometer, what does inhalation look like? |
On a spirometer graph, inhalaltion is always displayed as an upward deflection. |
|
|
|
How do you calculate Respiration Rate while looking at a graph? |
Place a pencil at the peak of a breath cycle and second cursor on the peak of the adjacnt cycle. ex: T2-T1 Do this two more times to the other peaks and average them out. T2-T1=Ta, T3-T4=Tb, T5-T6=Tc Then average them out (Ta+Tb+Tc) / 3 = Respiration Rate THIS ISNT DONE YET! NOW DIVIDE BY 60 TO GET RESPIRATION RATE(Breaths/Minute): -T3/60 -RR= .x breaths/minute BPM |
|
|
|
How do you calculate Tidal Volume (TV) by looking at a graph? |
Tidal volume is the average amount of air you breathe in and out whe you breath normally. Calculate this by placing a pencil at the trough before the inhalation and the second point at the peak of the breath. Right down the values, V2-V1, do it two more times and then average the values. -V2-V1, V4-V3, V5-V6 -(Va+Vb+Vc)/3 -Tidal Volume=V3 liters |
|
|
|
How do you calculate Alveolar Tidal Volume (TVa) by looking at a graph? |
This is the average amount of air reaching your lungs when breathing normally. This is calculated by average tidal volume - dead air space. EX: ATV-DAS= TVa |
|
|
|
How do you calculate Minute Alveolar Ventilation Rate (MVa)? |
MVa is the amount of air reaching your lungs each minute when you breath normally? This is calculated by alveolar tidal volume x respiration rate: -ATV x RR -MVa= ATVxRR L/min |
|
|
|
How do you calaculate Vital Capcity (VC) by looking at a graph? |
This is the amount of air you can breathe in and out when taking a large breath. Place a pencil on the first peak of the forced breath and then a point on the flat line after air has been expelled from the patient's lungs. Write down the value: -V2-V1 -V |
|
|
|
How do you calculate Residual Volume by looking at a graph? |
Residual Volume is the volume of air remaining in the lungs after a maximal exhalation; this volume of air is always inside of your lungs beccause you cannot exhale all of the air from collasping. Use the average adult value of 1.2 L |
|
|
|
How do you calculate Total Lung Capacity (TLC)? |
This is the total amount of air your lungs can hold. This is calculated as Residual Volume +Vital Capcity EX: RV + VC = TLC xyz Liters |
|
|
|
How do you calculate Forced Vital Capacity (FVC)? |
The maximum amount of air you can forcefully breath in and out when taking a large breath. Place your pencil at the second peak of the forced breath cycle and the second point at the flat line after the patient has expelled the air from their lungs. Ex: V2-V1= xyz FVC |
|
|
|
How do you calculate Forced Expiratory Volume at 1 Second (FEV1)? |
FEV1 ia the Maximum amount of air you can forcefully exhale in one second. Place your pencil on the peak of the maximum breath cycle and the second point one second after the peak. Ex: V2-V1= xyz FEV1 |
|
|
|
How do you calculate Percent Expiratory FLow (% Exp. Flow)? |
This is the ratio of FEV1/FVC. Do this by Dividing the Forced Expiratory Volume at 1 Second by the Forced Vital Capacity and then multiplying by 100. Ex: -FEV1 / FVC = xyz -xyz x 100 -% Expiratory Flow xyz - |
|
|
|
When do you use the ratio of FEV1/ FVC? |
Doctors use them in Pulmonary Function Tests to determine whether people are healthy, have obstructive disease, or restrictive lung disease. |
|
|
|
Obstructive disease |
It is increased resistance in airways and thier FEV1/FVC is less than 80%. Some examples of Obstructive Disease are asthama, bronchitis and emphysema. |
|
|
|
Restrictive Lung Disease |
These people have normal resistance in thier airways but have impaired respiratory movement. So thier FEV1/FVC ratios are normal or higher than normal. This occurs in Fibrosis |
|
|
|
QUICK CALC: Respiation Rate (RR) |
RR=number of inhales in one minute RR= xyz breath/minute |
|
|
|
QUIK CALC: Tidal Volume |
TV= Average Normal Inhale - Average Normal Exhale TV = xyz liters |
|
|
|
QUICK CALC: Alveolar Tidal Volume (TVa) |
TVa= Tidal Volume-Dead Air Space TVa= xyz L |
|
|
|
QUICK CALC: Minute Alveolar Ventilation Rate (MVa) |
MVa= Alveolar Tidal Volume x Respiration rate MVa= xyz L/min |
|
|
|
QUICK CALC: Vital Capacity (VC) |
VC= maximum inhale - maximum exhale
VC= xyz |
|
|
|
QUICK CALC: Residual Volume (RV) |
RV= 1.2 L |
|
|
|
QUICK CALC: Total Lung Capacity (TLC) |
TLC = Residual Volume + Vital Capacity TLC= xyz L |
|
|
|
QUICK CALC: Forced Vital Capacity (FVC) |
FVC=Maximum held inhale-forced maximum exhale FVC= xyz |
|
|
|
QUICK CALC: Forced Expiratory Volume in One Second (FEV1) |
FEV1=Maximum held inhale - one second later FEV1= XYZ |
|
|
|
QUICK CALC: Percent Expiratory Flow (% Exp Flow) |
% Exp Flow= (Forced Expiratory volume in one second / forced Vital Capacity) x 100% % Exp Flow= xyz |
|
|
|
What is part of the Urinary Tract? |
Kidneys, bladder, Uretha and Ureters. |
|
|
|
How many kidneys do humans have? What do they do? |
A) Two B) filter and clean blood and help blood maintain homeostasis |
|
|
|
Label the urinary tract |
Pic |
Pic |
|
|
What do the kidneys do? (In depth)?? |
1) inorganic ion and water balance in blood 2) removal of nitrogenous waste from blood 3) removal of xenobiotics from blood 4) gluconeogenesis-make glucose 5) secretion of hormones |
|
|
|
What is a Nephron? |
It is the functional unit of the kidney, there are 1 millon nephrons in EACH kidney~two millon |
CHECK WITH INSTRUCTOR One million in a pair of kidneys or one million in one individaul kidney in one pair~ one million in each side = 2 mil |
|
|
What are Afferent Arterioles? |
Afferent Arterioles bring blood to the kidney but only some of the blood gets filtered into the kidney, the rest leave thru the efferent arteriole |
|
|
|
What does the efferent arteriole do? |
The blood that dosen't go through the Afferent Arterioles go thru the Efferent Arteriole without ever entering the kidney. |
|
|
|
What is the amount f blood filtered by the kidney called? |
Glomerular Filatration Rate (GFR) |
|
|
|
What is a glomerulus? |
A capillary bed in each of the kidney nephrons |
|
|
|
Side Facts about blood filtration (And in depth steps of 'flow') |
1) Only 20% of the blood from the afferent arteriole enters through the glomerulus into the nephron 2) 80% of the blood flow right pass the nephron dosen't get cleaned. 3) Some of the items in the blood are too large to fit through the glomerular filter and enter the nephron, these include blood cells and proteins. |
4) Water, inorganic ions (ex. K+, CL-, and Na+) and metabolic wastes are small enough to fit through the glomerular filter and enter the nephron. 5)The portion of the blood that does pass through the glomerulus into the kidneyenters Bowman's capsule of the nephron. 6) Then Filtrate will then pass through the proximal convoluted tubule to the desceding loop of Henle, then up the ascending loop of Henle, through the distal convoluted tubule into the collecting duct which dumps into the renal pelvis of the kidney. |
|
|
Nephron Filtrate Flow Condensed |
1)Bowman's Capsule 2)Proximal Tubule 3) Descending Loop of Henle 4) Ascendinf Loop of Henle 5) Hypoasmotic/ distal convoluted Tubule 6) Collecting Duct 7)Renal Pelvis of the Kidney |
Pic of flow |
|
|
What are the two hormones regulated by the kidney? |
1) Aldosterone 2)Vasopressin (aka ADH or Antidiuretic Hormone) |
|
|
|
Facts about Aldosterone |
-it is made by the kidneys -stimulates the collecting duct to reabsorb Na+ back into the bloodstream when Na+ levels are low in the blood. |
Due to our diets, most Americans use very little aldosterone. |
|
|
Facts about Vasopressin (ADH) |
-secreted by the pituitary gland -stimulates the collecting duct to reabsorb water when the water levels are low in the blood(the person is dehydrated) -Causes auaporins to be insterted back into collecting duct walls |
|
|
|
What are Aquaporins? |
Protein channels (tubes) through which water leaves the collecting duct in order to be reabsorbed back into the bloodstream. Vassopressin causes the sertion of aquaporins into the collecting duct walls. |
|
|
|
Bicarbonate Equation to regulate the pH of blood: |
H+ + HCO3- ↔H2CO3 ↔ CO2 +H2O
|
|
|
|
The kidney regulates blood pH by ___1___ and __2__ |
1) re-absorption of HCO3- 2) secrtion of HCO3- |
|
|
|
If blood pH is too basic (Higher than pH=7.45) then: |
Kidney will allow the HC03- in the nephron to be extreted. |
|
|
|
Reduction in buffer (bicarbonate) allows: |
[H+] to increase in the blood lowering pH making the blood more acidic. |
|
|
|
If blood is too acidic: |
the kidney will reabsorb more HCO3- which will bind [H+] and reduce acidity. |
|
|
|
TAKE PIC |
pH Spcfc Grvty Vlm Dcf Soda: ↓ ↔ ↔ Caf Sda: ↓ ↓ ↑ Hypo Sol: ↔ ↓ ↓ Iston Sol: ↔ ↔ ↔ Hypr Sol: ↔ ↑ ↓
|
|
|
|
How to create muscle recruitment? |
You adjust the stimulus. Bigger the stimulus, the bigger the contraction. When the stimulus is recruited there are more motor units. |
|
|
|
Summation |
Give less periods of break/relaxtion |
|
|
|
Teatnus |
No more calcium in sarcoplasmic reticulum which causes fatigue. |
|
|
|
Which reflexes are faster? Auditory or Visual? |
Auditory |
|
|
|
Monosynapse |
One Arch, Brain does not control reflex arch but LUMBAR VERTEBRAE AND SPINAL CORD DOES |
|
|
|
What are the 'mini brains' of the body? |
Interneurons |
|
|
|
What is Depolarization? |
Contraction |
|
|
|
What causes 'delays' in the heart?
|
AV Node |
|
|
|
How do we measure heart rate? |
We use beat periods, or Beats per minute, to determine heart rate. |
|
|
|
R Wave refers to: |
Arteriole relaxation and height of arteriole contraction |
|
|
|
Pulse Wave |
Amplitude refers to strength or weakness
|
|
|
|
Basal Dillation |
Heat on Skin sends blood cells there so heat can escape |
|
|
|
how many types of muscles are there?
|
Three
|
|
|
|
Another name for skeletal muscles, it’s due to repeating regions of thicker and thinner cell density
|
Striated Muscles
|
|
|
|
Sarcomere
|
are the repeating units of a muscle cell.
|
|
|
|
Myosin
|
is the thick filament in a muscle cell
|
|
|
|
Actin
|
is the thin filament in a muscle cell.
|
|
|
|
Tropomyosin
|
is wrapped around the actin filament
|
|
|
|
Troponin
|
is bound to the tropomyosin.
|
|
|
|
Motor Neuron
|
connects to the muscle cell at the transverse tubules.
|
|
|
|
Sarcoplasmic reticulum
|
is where Ca+2 is stored in the muscle cell.
|
|
|
|
Ca2+ ATPase Pump
|
pumps Ca+2 back into the sarcoplasmic reticulum.
|
|
|
|
Motor Unit
|
is one motor neuron and all of the muscles cells it innervates
|
|
|
|
Tetanus
|
The strongest contraction possible for a muscle, occurs when all of the troponin is bound with Ca2+ and there is none left in the sarcoplasmic reticulum.
|
|
|
|
Monosynaptic Reflex |
is produced by circuitry with only one synapse. |
|
|
|
cardiovascular
|
system includes the heart and blood vessels.
|
|
|
|
Atria
|
are the top two chambers of the heart.
|
|
|
|
Ventricles
|
are the bottom two chambers of the heart.
|
|
|
|
Vena Cavas
|
are the largest veins in the body and empty into the right atrium.
|
|
|
|
Right Atrium
|
pumps blood to the right ventricle.
|
|
|
|
Right Ventricle
|
pumps blood to the lungs
|
|
|
|
Left Atrium
|
pumps blood to the left ventricle
|
|
|
|
Left Ventricle
|
pumps blood to the majority of the body.
|
|
|
|
Right AV Valve
|
is the valve between the right atrium and right ventricle.
|
|
|
|
Left AV Valve
|
is the valve between the left atrium and left ventricle.
|
|
|
|
pulmonary valve
|
is the valve blood passes through to get to the lungs.
|
|
|
|
Pulmonary Veins
|
the only veins that carry oxygenated blood.
|
|
|
|
aortic valve
|
is the valve blood passes through to travel to the majority of the body.
|
|
|
|
Systolic and Diastolic
|
the two phases of the cardiac cycle.
|
|
|
|
P wave
|
is caused by the contracting atria.
|
|
|
|
QRS complex
|
is caused by the contracting ventricles.
|
|
|
|
Hidden Wave
|
is the wave caused by the filling/relaxing of the atria.
|
|
|
|
T-wave
|
is the wave caused by the filling/relaxing of the ventricles.
|
|
|
|
Myocardial cells
|
another name for heart muscle cells.
|
|
|
|
Sinoatrial Node (SA Node)
|
often referred to as the pacemaker of the heart.
|
|
|
|
Atrioventricular Node (AV Node)
|
transfers the electric signal to the Bundle of His and is responsible for the lag period
|
|
|
|
Bundle of His
|
transfers signal to Purkinje fibers.
|
|
|
|
Purkinje Fibers
|
transfers signal to ventricles which makes them contract.
|
|
|
|
Vasoconstriction
|
is when blood vessels shrink in diameter.
|
|
|
|
Vasodilation
|
is when blood vessels expand in diameter.
|
|
|
|
What are the two principles that regulate local blood flow?
|
Flow autoregulation and active hyperemia
|
|
|
|
What is the amount of oxygen carried by the red blood cells?
|
98%
|
|
|
|
Target Heart Rate =
|
% exercise intensity(220-age-resting heart rate) + resting heart rate
|
|
|
|
What is the sound caused by the AV valves closing during the systolic phase of the cardiac cycle?
|
Lub
|
|
|
|
What is the sound caused by the aortic and pulmonary valves closing during the diastolic phase of the cardiac cycle?
|
Dub
|
|
|
|
Mean Arterial Pressure=
|
Diastolic Pressure + ⅓ Pulse Pressure
|
|
|
|
Cardiac Output =
|
Heart Rate X Stroke Volume
|
|
|
|
where O2 and CO2 are exchanged?
|
Alveoli
|
|
|
|
air that isn’t fully inhaled into the lungs or exhaled from the body
|
Dead Air Space (0.15L)
|
|
|
|
amount of air that is always inside your lungs.
|
residual volume
|
|
|
|
the number of breaths each minute when breathing normally
|
respiration rate
|
|
|
|
the average amount of air you breath in and out when breathing normally.
|
Tidal Volume
|
|
|
|
the average amount of air reaching your lungs when breathing normally
|
Alveolar tidal volume
|
|
|
|
amount of air reaching your lungs each minute when breathing normally.
|
Minute alveolar ventilation rate
|
|
|
|
the max amount of air you can breath in and out when taking a large breath.
|
Vital capacity
|
|
|
|
the total amount of air your lungs can hold
|
Total lung capacity
|
|
|
|
the max amount of air you can forcefully exhale.
|
Forced Vital Capacity
|
|
|
|
the max amount of air you can forcefully exhale in one second.
|
Forced expiratory volume in one second
|
|
|
|
the % of air you can forcefully exhale in one second.
|
Percent expiratory flow
|
|
|
|
Glomerular Filtration Rate
|
is the % of blood your kidney filters normally. Also called the GFR.
|
|
|
|
the capillary bed in each of the kidney nephrons.
|
Glomerulus
|
|
|
|
the functional unit of the kidney.
|
Nephron
|
|
|
|
is a hormone made by the kidney that regulates Na+ reabsorption
|
Aldosterone
|
|
|
|
is a hormone made by the pituitary gland that regulates the reabsorption of water.
|
Vasopressin or ADH
|
|
|
|
are protein channels that facilitate the reabsorption of water from the collecting ducts.
|
Aquaporins
|
|
|
|
(H+ follows) the kidney maintains pH balance by regulating the reabsorption of this molecule.
|
HCO3
|
|
|
|
examples of diuretics
|
Alcohol and Caffeine
|
|
|
|
In the recruitment experiment what was happening as we increased the intensity and the muscle contractions became stronger?
|
Muscles twitch as the amount of motor neurons increased
|
|
|
|
Why are the ventricles so much thicker than the atria?
|
Ventricles have thicker muscular walls and blood is pumped out of the heart at greater pressure. Atria have less resistance to blood flow, so they have less muscle and thin walls. More blood flow through them during filling, the left side has to pump the blood to the entire body.
|
|
|
|
What are the changes in renal output you would expect to see if you drank a hypotonic (pure water) solution?
|
Urine volume-increase
Specific gravity-decrease Urine pH-no change |
|
|
|
What are the changes in renal output you would expect to see if you drank a hypertonic (salt water) solution?
|
Urine volume-decreas
Specific gravity-increase Urine pH-no change |
|
|
|
What are the changes in renal output you would expect to see if you drank an isotonic solution? (answer choices are: increase, decrease, no change)
|
Urine volume-no change
Specific gravity-no change Urine pH-no change |
|
|
|
What are the changes in renal output you would expect to see if you drank a caffeinated soda?
|
Urine volume-increase
Specific gravity-decrease Urine pH-decrease |
|
|
|
What are the changes in renal output you would expect to see if you drank a decaffeinated soda?
|
Urine volume-no changes Specific gravity- no change
Urine pH- decrease |
|
|
|
Where blood is oxygenated and deoxygenated?
|
Pulmonary artery: carries deoxygenated blood- referred to as artery because it goes away from the heart-Pulmonary vein (vein: towards the heart) carries oxygenated into the heart.
Red = oxygenated Blue= deoxygenated |
|
|
|
Respiration Rate:
|
Number of inhales in one minute
Count the number of inhales in the 30 second window and multiply by 2 9 x 2 = 18 |
|
|
|
Tidal Volume:
|
Average top and bottom, then subtract average inhale-average exhale
3.3 - 2.7 = .6 |
|
|
|
Alveolar Tidal Volume:
|
Tidal volume - dead air space (always .15) .6 - .15 = .45
|
|
|
|
Minute Alveolar Ventilation Rate:
|
Alveolar tidal volume x respiration rate
.45 x 18 = 8.1 |
|
|
|
Vital Capacity:
|
Max inhale - Max exhale
4.7 - 1.6 = 3.1 |
|
|
|
Residual volume:
|
1.2L
|
|
|
|
Total lung capacity:
|
vital capacity + residual volume
3.1 + 1.2 = 4.3 |
|
|
|
Forced Vital Capacity:
|
max held inhale - forced max exhale
4.4 - 1.3 = 3.1 |
|
|
|
Forced Expiratory Volume in one second:
|
Max held inhale - one second later
4.4 - 1.9 = 2.5 |
|
|
|
Percent Expiratory Flow:
|
(Forced expiratory volume in one second / forced vital capacity) x 100:
(2.5 / 3.1) x 100 = .806 x 100 (100 so it can turn into a percent) = 80.6% |
|

