![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
198 Cards in this Set
- Front
- Back
|
What are sites and types of rheumatic disease?
|
Muscle inflammation - myositis
Bursa - bursitis Bony end plate - osteonecrosis synovial membrane - rheumatoid arthritis enthesis - ankylosing spondylitis cartilage - osteonecrosis |
|
|
What are causes of monarticular joint pain?
|
osteoarthritis
septic arthritis gout pseudogout trauma hemarthrosis Charcot's joint/foot |
|
|
What are causes of polyarticular joint pain?
|
rheumatoid arthritis
SLE viral arthritis rheumatic fever reiter's syndrome lyme disease serum sickness drug-induced |
|
|
What are causes of periarticular pain?
|
bursitis
tendinitis cellulitis enthesitis |
|
|
What joints in the hand are commonly affected by RA?
|
MCP and PIP joints
|
|
|
What is the differential of symmetric polyarticular arthritis in the ED?
|
Gonococcal arthritis
Viral arthritis Lyme disease Drug-induced arthritis Reiter's syndrome Rheumatic fever Seronegative spondyloarthropaties |
|
|
What is the differential of asymmetric polyarticular arthritis in the ED?
|
Gonococcal
Acute rheumatic fever Lyme SLE Immune complex disease (viral) Reiter's syndrome Reactive arthritis |
|
|
What is a common radiologic finding in acute arthritis?
|
Soft tissue swelling
|
|
|
What are indications for ED arthrocentesis?
|
Obtaining joint fluid for analysis
Draining tense hemarthrosis Instilling local anesthetic/steroid for pain control |
|
|
What are characteristics of septic synovial fluid?
|
Translucent/opaque
Low viscosity >100,000 wbc >95% PMNs Positive culture |
|
|
What characterizes the crystals in gout?
|
Needle-like crystals
Negatively birefringent (yellow when parallel and blue when perpendicular) |
|
|
What characterizes pseudogout crystals?
|
rhomboid crystals
positively birefringent (yellow when perpendicular and blue when parallel) |
|
|
What are characteristics of inflammatory pain?
|
Morning stiffness for >1hour
Exercise makes things better Rest makes things worse Responds to NSAIDs Often accompanying systemic symptoms |
|
|
What are characteristics of non-inflammatory pain?
|
No morning stiffness
Exercise makes things worse Rest makes things better Poor response to NSAIDs No systemic symptoms |
|
|
What arthritides may involve the back?
|
Psoriatic
Reiter's Ankylosing spondylitis IBD |
|
|
What joints are typically involved in OA?
|
Hands
Hip Knee 1st MTP L-spine C-spine |
|
|
What joints are typically involved in RA?
|
PIP
MCP Wrist Elbow Shoulder Knee Ankle MTP |
|
|
What pathogens typically cause septic arthritis in infants and neonates?
|
Staph aureus
GBS Gram negative rods |
|
|
What pathogens typically cause septic arthritis in children?
|
haemophilus influenza
staph aureus |
|
|
What pathogens typically cause septic arthritis in adolescents?
|
gonorrhea
chlamydia |
|
|
What pathogens typically cause septic arthritis in older adults?
|
staph aureus
streptococcus gram negative rods |
|
|
What pathogens typically cause septic arthritis in sickle cell anemia?
|
Salmonella
|
|
|
What pathogens typically cause septic arthritis in IVDU?
|
pseudomonas
s aureus gram negative rods |
|
|
What is the treatment for septic arthritis?
|
Gram postitive -> cefazolin +/- vanco
Gram negative ->third generation cephalosporin |
|
|
What are the etiologies of gout?
|
Overproduction (inborn errors of metabolism, myeloproliferative disease)
Underexcretion by the kidney |
|
|
What joints are typically affected by gout?
|
First MTP
Knee Ankle Tarsals |
|
|
What are RF for gout?
|
Obseity
Weight gain HTN DM EtOH Proximal loop diuretics |
|
|
What is the treatment for gout?
|
NSAIDs - none shown to be superior, 5days then RA
Colchicine Corticosteroids ACTH Avoid allopurinol in acute phase (can worsen acute attack) Avoid ASA in the acute phase |
|
|
What causes pseudo gout?
|
Calcium pyrophosphate crystals
|
|
|
What are xray findings in late pseudo gout?
|
Linear calcification in cartilage
asymmetric joint space narrowing MP hook spurs osteophyte formation subchondral cyst formation lack of osteoporosis |
|
|
What are xray findings of late septic arthritis?
|
subchondral bone destruction
periosteal new bone loss of joint space osteoporosis late joint space narrowing |
|
|
What are xray findings in OA?
|
Joint space narrowing
osteophytes subchondral bone formation and cysts |
|
|
What are typical wbc counts in gonococcal arthritis?
|
wbc 40000-60000
|
|
|
What is the treatment of gonococcal arthritis?
|
Ceftriaxone IV x 48hours then cefixime 400mg BID 7 days
|
|
|
When does Lyme arthritis occur?
|
Usually asymmetric in the knees within 6 months of the bite
|
|
|
What is the pathophysiology of rheumatoid arthritis?
|
Immune complexes stimulate PMNs to release enzymes that destroy joint
|
|
|
What joints/areas are not involved in RA?
|
DIP joints
Back |
|
|
What is scleroderma?
|
A multisystem disease of unknown cause that is characterized by fibrosis of skin, blood vessels and visceral organs
|
|
|
What is CREST syndrome?
|
Calcinosis
Raynaud's Esophageal dysmotility Sclerodactyly Telangiectasias |
|
|
What is the number 1 killer in scleroderma?
|
pulmonary hypertension
|
|
|
What is polymyalgia rheumatica (PMR)?
|
An inflammatory syndrome of older individuals which presents with shoulder and/or pelvic pain
|
|
|
What are criteria for the diagnosis of PMR?
|
Age>50
Bilateral pain in shoulders, hips and neck for at least 1 month ESR >40mm/hr |
|
|
What is the mnemonic for PMR?
|
SECRET
Stiffness and pain without weakness Elderly Constitutional symptoms Rheumatism (polyarthritis) ESR elevated Temporal arteritis |
|
|
Which polyarthritides have back involvement?
|
Ankylosing spondylitis
Reiter's syndrome psoriatic arthritis Arthritis of IBD |
|
|
What is ankylosing spondylitis?
|
Systemic inflammation of the axial skeleton involving the SI joints and the spine
|
|
|
What is reiter's syndrome?
|
A reactive arthritis in genetically susceptible hosts after GI or GU infection
|
|
|
What organisms are associated with reiter's syndrome?
|
Chlamydia
Salmonella Shigella Yersinia Campylobacter |
|
|
What is the classic triad of reiter's syndrome?
|
arthritis
uveitis urethritis |
|
|
What is the treatment for Reiter's syndrome?
|
NSAIDs (the infection is gone by the time of arthritis onset)
Avoid steroids Treat STD |
|
|
What are the toxicities of methotrexate?
|
Hepatic
Bone marrow Lung |
|
|
What is the toxicity of hydroxychloroquine (plaquenil)?
|
Retinal
|
|
|
What are the major Jones criteria?
|
Polyarthritis
Carditis chorea Erythema marginatum Subcutaneous nodules |
|
|
What are the minor Jones criteria
|
Arthralgia
Fever Elevated acute phase reactants elevated ESR elevated CRP Prolonged PR interval on ECG |
|
|
What are criteria to diagnose acute rheumatic fever?
|
2 major Jones criteria
OR 1 major and 2 minor Jones criteria AND presence of laboratory evidence of prior GAS infection |
|
|
What is a bursa?
|
Flat round sac lined by synovium which may not connect with the joint cavity
|
|
|
What are causes of bursitis?
|
repetitive trauma
crystal deposition infection systemic disease (RA, SLE, psoriasis, gout, ankylosing spondylitis) |
|
|
What is the preferred term for tendinitis?
|
tendinosis (pathophys is less consistent with inflammation)
|
|
|
What is a tenosynovitis?
|
Inflammation of the tendon and its sheath
|
|
|
Why does impingement occur?
|
Compression of the tendons of the rotator cuff (usually supraspinatus) against the undersurface of the acromion
|
|
|
What is a positive Jobe's test?
|
pain or weakness when you resist the empty can test
|
|
|
What is a positive Neer's test?
|
Pain at the end of the 180 degree arc on forward flexion of the arm
|
|
|
What is the drop arm test and what does it indicate?
|
Abduct the arm to 90 degrees and ask the patient to maintain the abduction - if the arm drops to the side, a large rotator cuff tear must be considered
|
|
|
What is the pathophysiology of lateral epicondylitis?
|
inflammation at the insertion of the extensor carpi radialis brevis
|
|
|
What is the physical exam feature of lateral epicondylitis?
|
pain with resisted dorsiflexion of the wrist
|
|
|
What is the pathophysiology of medial epicondylitis?
|
pain at the insertion of flexor carpi radialis
|
|
|
What fluid analysis suggests infected olecranon bursitis?
|
Aspiration >5000 wbc/mm3
|
|
|
What is Finkelstein's test and what does it indicate?
|
hold thumb in the palm by the fingers and ulnar deviate. Pain with this maneuver is considered a positive finding
|
|
|
What are the criteria for the diagnosis of SLE?
|
SOAP BRAIN MD
Serositis (pleuritis or pericarditis) Oral ulcers Arthritis Photosensitivity Blood disorder (hemolytic anemia, leukopenia, lymphopenia, thrombocytopenia in the absence of offending drub) Renal disorder (>0.5g loss per day) Antinuclear antibody + Immune disorder (raised anti DS DNA, anti SM antibody) Neurologic disorder - seizure, psychosis Malar rash Discoid rash require 4 or more criteria serially or simultaneously |
|
|
What drugs are commonly implicated in lupus-like syndrome?
|
CV: procainamide, amiodarone, quinidine, hydralazine
Antimicrobial: isoniazid, penicillin, sulfonamides, tetracycline, nitrofurantoin anticonvulsant: phenytoin |
|
|
What is antiphospholipid antibody syndrome?
|
Requires a clinical event (thrombosis or pregnancy loss) and an antiphospholipid antibody (lupus anticoagulant or anticardiolipin) documented.
The antiphospholipid antibodies bind to the prothrombin activator complex resulting in prolonged PTT but clinically associated with clotting |
|
|
What are clinical manifestations of antiphospholipid antibody syndrome?
|
Arterial occlusion (myocardial infarction, extremity gangrene)
Venous occlusion (peripheral venous occlusion, budd-chiari, portal vein occlusion) Valvular heart disease Coomb's positive hemolytic anemia Recurrent fetal loss Thrombocytopenia |
|
|
What are large vessel vasculitides?
|
Temporal
Takayasu |
|
|
What are medium vessel vasculitides
|
Polyarteritis nodosa
Buerger's disease Kawasaki Primary angiitis of the CNS |
|
|
What are small vessel vasculitides?
|
Behcets
|
|
|
What is the triad for SLE?
|
Fever
Joint pain Rash in women of childbearing age |
|
|
What are treatments for SLE?
|
NSAIDs
Steroids Chloroquine/hydroxychloroquine immunosuppressants |
|
|
What are hypersensitivity vasculitides?
|
HSP
Mixed cryoglobulinemia Serum sickness |
|
|
What are criteria for the classification of temporal arteritis?
|
Need 3 out of 5
Onset of disease at the age of 50 or older New headache Temporal artery abnormalities (tenderness on palpation or decrease in pulsation) ESR >50mm/hr abnormal findings on temporal artery biopsy |
|
|
What is a general guide for estimating normal ESR?
|
Male: 0.5x age
Female: (0.5 x age) + 5 |
|
|
What symptoms suggest temporal arteritis?
|
Headache
Temporal artery tenderness Jaw claudication Unilateral visual loss/amaurosis fugax or diplopia Severe myalgia, morning stiffness of shoulder or pelvis |
|
|
What are the manifestations of serum sickness?
|
Fever
Arthralgia Skin finding (erythema on the sides of the fingers, toes and hands before and more widespread eruption that is morbilliform) Onset 12-36 hours after exposure Withdrawing the drug leads to rapid resolution |
|
|
What diseases can be associated with erythema nodosum?
|
idiopathic
drug induced : phenythoin, penicillin, sulfa, aspartame viral URI, strep, sarcoid, TB IBD, SLE, histoplamosis, yersinia |
|
|
What is anaphylaxis?
|
acute systemic reaction of multiple organ systems to an IgE mediated immunologic mediator release in previously sensitized individuals
|
|
|
What are the clinical criteria for diagnosing anaphylaxis?
|
Any of the following:
1) acute onset illness with involvement of the skin, mucosal tissue or both AND one of the following -respiratory compromise -reduced BP or associated symptoms of end-organ dysfunction OR 2) Two or more of the following occurring rapidly after exposure to a likely allergen a) involvement of skin-mucosal tissue b) respiratory compromise c) reduced BP or associated symptoms d) persistent gastrointestinal symptoms OR 3) Reduced BP after exposure to known allergen for that patients 1)infants and children: low SBP or greater than 30% decrease b) adults SBP of less than 90mmHg or 30% decrease from baseline |
|
|
What is a localized allergic reaction?
|
non systemic reaction from immune over-reactivity
|
|
|
What is an anaphylactoid reaction?
|
immune reaction similar to anaphylaxis but is independent of IgE antibodies
they occur with no previous sensitization |
|
|
What are common precipitants of anaphylactoid reactions?
|
Radiocontrast
ASA NSAID opioids |
|
|
What are the 4 types of immunologic reactions?
|
Type I - immediate hypersensitivity reactions; IgE causing mast cell degranulation, accounts for most of anaphylaxis
Type II - cytotoxic reaction; complement fixing IgG binds cell bound antigens activating complement pathway. C3a and C5a cause mast cell degranulation like Type I Type III Immune complex (IgG or IgM): immune complexes (Ag and Ab) migrate to the interstitial space and activate the complement system (serum sickness). Complement mediated anaphylaxis Type IV - delayed hypersensitivity reaction (T cells): only one that does not cause anaphylaxis |
|
|
What is the effect of beta blockers on anaphylaxis?
|
They may increase the risk of anaphylaxis and decrease the effectiveness of epinephrine
glucagon can be used in these situations |
|
|
What are typical agents that cause IgE mediated anaphylaxis?
|
Antibiotics (eg. penicillin)
Insect stings Therapeutic agnes (lidocaine, horse serum for anti venom, egg based vaccines) Foods Latex (remember to avoid nasal trumpets) |
|
|
What are immune complex mediated causes of anaphylaxis?
|
Blood products
Immunoglobulin administration |
|
|
What is the standard treatment protocol for patients with a history of radiocontrast induced anaphylaxis?
|
Prednisone 13, 7 and 1 hour before procedure
Diphenhydramine 50mg IM 1 hour before procedure Consider ephedrine 25mg PO 1 hour before procedure Consider H2 antagonist such as ranitidine 300mg PO 3 hours before procedure |
|
|
What is the differential diagnosis for anaphylaxis?
|
Upper airway obstruction
Bronchospasm Syncope Seizure MI Urticaria Scromboid poisoning (muscle of fish undergoes decomposition and histidine is converted to histamine) Angioedema (clue: angioedema is not itchy) Acquired angioedema |
|
|
What is the airway management in anaphylaxis?
|
Early intubation is important
Nebulized epinephrine 5cc (1:1000) may buy you some time IV epinephrine may reverse airway compromise (1-4mcg/min)(peds 1mcg/kg/min) Oral intubation is preferred but be ready for a surgical airway Heliox may improve oxygen delivery |
|
|
What are the mechanisms of action of epinephrine?
|
Alpha agonism - peripheral vasoconstriction
Beta agonist - bronchodilation, +ve ionotropy, +ve chronotropy |
|
|
What is the mechanism and dose of glucagon in anaphylaxis?
|
enhances cAMP synthesis
1-5mgmg SC/IM/IV and then infusion 1-5mg/hr |
|
|
What is biphasic anaphylaxis?
|
Recurrence of anaphylactic symptoms caused by a late-phase reaction which peaks 4-12 hours after the initial reaction and lasts up to 48 hours
|
|
|
What is the differential for flushing?
|
Carcinoid syndrome
Anaphylaxis Alcohol-induced flushing Emotions/exercise Mastocytosis Scromboidosis |
|
|
What is the treatment for refractory bronchospasm in anaphylaxis?
|
Aminophylline
|
|
|
What are the 2 types of angioedema?
|
Angioedema with urticaria and pruritus
-hypersensitivity IgE mediated reaction with a mast cell component Angioedema without urticaria and pruritus -usually kinin related -management with racemic epinephrine, FFP or C1 inhibitor replacement protein -epi/steroids/antihistamines do not usually work |
|
|
What is hereditary angioedema?
|
autosomal dominant condition
positive family history caused by c1-esterase deficiency confirmed by low levels of C4 and C1 esterase inhibitor activity |
|
|
What is acquired C1 inhibitor deficiency?
|
less common than hereditary
clinically indistinguishable from hereditary angioedema absence of family history involves older patients associated with underlying lymphoproliferative disease |
|
|
What is mastocytosis?
|
Disorders caused by too many mast cells in the body
|
|
|
How do you treat hypertensive crisis with due to unopposed alpha blokade in anaphylaxis?
|
nitroprusside 0.3-10ug/kg/min
phentolamine 5-20mg IV |
|
|
What is a macule?
|
Flat skin lesion where the color differs from the surrounding skin
|
|
|
What is a patch?
|
A macule with surface change (scale or wrinkling)
|
|
|
What is a papule?
|
Elevated skin lesion <0.5cm in diameter
|
|
|
What is a plaque?
|
Elevated skin lesion >0.5cm in diameter without substantial depth
|
|
|
What is a nodule?
|
Elevated skin lesion >0.5cm in diameter and depth
|
|
|
What is a cyst?
|
a nodule filled with expressible material
|
|
|
What is a vesicle?
|
Blisters<0.5cm in diameter filled with clear fluid
|
|
|
What is a bullae?
|
Blisters >0/5cm in diameter filled with clear fluid
|
|
|
What is a pustule?
|
vesicle filled with cloudy or purulent fluid
|
|
|
What is a crust?
|
liquid debris that has dried on the skin
|
|
|
What is a scale?
|
visible thickened stratum corneum
|
|
|
What is lichenification?
|
epidermal thickening characterized by visible palpable skin thickening and accentuated skin markings
|
|
|
What is induration?
|
dermal thickening that feels thick and firm
|
|
|
What is purpura?
|
red appearance of skin caused by blood extravasated from disrupted dermal blood vessels -> non blanch able
|
|
|
What is tinea capitis?
|
fungal infection of the scalp
|
|
|
What is the treatment for tinea capitis?
|
systemic antifungal for 6 weeks
Selenium sulfide shampoo derm f/u |
|
|
What is a kerion?
|
Fungal infection of the scalp that appears indurated, boggy, studded with pustules
|
|
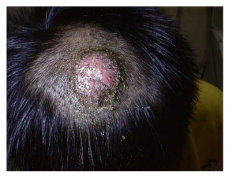
What is this lesion
|
kerion
|
|

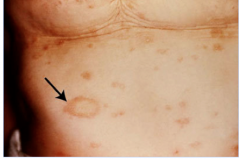
What is this lesion
|
tinea capitis
|
|

What is this lesion
|
tinea corporis
|
|

What is this lesion
|
tinea pedis
|
|

What is this lesion
|
tinea versicolor
|
|

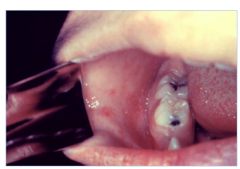
What is this lesion
|
tinea unguium
|
|

What is this lesion
|
oral thrush
|
|

What is this lesion
|
diaper dermatitis
|
|
What is this lesion
|
pityriasis rosacea
|
|

What is this lesion
|
atopic dermatitis
|
|

What is this lesion
|
impetigo
|
|

What is this lesion
|
folliculitis
|
|

What is this lesion
|
carbuncle
|
|

What is this lesion
|
gonococcal dermatitis
|
|

What is this lesion
|
morbilliform drug eruption
|
|

What is this lesion
|
tens
|
|

What is this lesion
|
staph scalded skin syndrome
|
|
What is this lesion
|
koplik spots
|
|
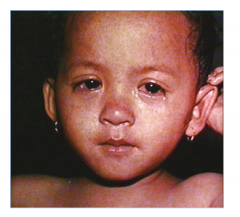
What is this lesion
|
measles
|
|

What is this lesion
|
erythema multiforme
|
|

What is this lesion
|
steven johnson syndrome
|
|

What is this lesion
|
erythema marginatum
|
|

What is this lesion
|
pediculosis
|
|

What is this lesion
|
scabies
|
|

What is this lesion
|
secondary syphilis
|
|

What is this lesion
|
herpetic whitlow
|
|

What is this lesion
|
cutaneous anthrax
|
|
What is this lesion
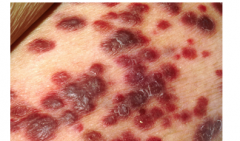
|
Kaposi sarcoma
|
|
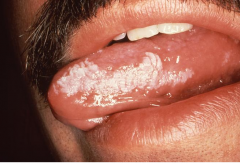
What is this lesion
|
oral hairy leukoplakia
|
|

What is this lesion
|
discoid rash of SLE
|
|
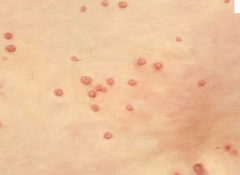
What is this lesion
|
molluscul contagiosum
|
|
|
What is the treatment for a kerion
|
Same treatment as tinea capitis (systemic anti-fungal, selenium shampoo and derm f/u) but add 1-2 weeks of prednixone 1mg/kg/day +/- 1 week of keflex or diclox if bacterial superinfection
|
|
|
What are the characteristics of tinea corporis?
|
sharply marginated annular lesions with raised or vesicular margins and central clearing
|
|
|
What is the treatment of tinea corporis?
|
topical antifungal for 1-3 weeks
|
|
|
What is the treatment of tinea pedis
|
same as the treatment for tinea corporis
|
|
|
What is the treatment for versicolor?
|
selenium sulfide shampoo
single oral dose of ketoconazole |
|
|
What is the treatment for tinea unguium?
|
long course of oral antifungal (ex fluconazole)
|
|
|
What is the treatment for oral thrush?
|
nystatin suspension swish and swallow QID until 5-7 days after the lesion disappear
|
|
|
What is the treatment for diaper dermatitis?
|
alter physical environment (frequent change, remove diaper when possible, avoid plastic or rubber diapers)
zinc oxide cream if severe -> 1% hydrocortisone topical cream |
|
|
What is pityriasis rosea?
|
xmas tree pattern with herald patch
|
|
|
What are diagnostic criteria for atopic dermatitis?
|
itchy skin
>/=3 of the following: dry skin, flexural dermatitis, history of flexural involvement, history of asthma or hay fever, onset of rash before 2 years of age |
|
|
What is the treatment of atopic dermatitis?
|
-avoid irritant materials
-wear cotton -daily warm baths to hydrate skin followed by pat drying and application of moisturizer -medium potency topical steroid -antihistamine for pruritus |
|
|
What is the treatment for impetigo?
|
topical muciprocin (if small)
cephalexine PO (if many lesions) |
|
|
What is the management of bullous impetigo?
|
same as impetigo
|
|
|
What causes folliculitis?
|
Staph aureus
but can be pseudomonas in infected swimming pools and hot tubs |
|
|
What is the treatment for folliculitis?
|
chlorhexidine skin cleaning daily for a few weeks. If extensive then oral erythromycin or cloxacillin
|
|
|
What is hidradenitis suppurativa?
|
Recurrent abscess formation in the axilla or groin
|
|
|
What is the treatment for hidradenitis suppurativa?
|
long course of cloxacillin or erythromycin
possible drainage of abscess may eventually require excision and skin grafting |
|
|
What is a carbuncle?
|
Large abscess that develops in the thick skin of the neck, back or thighs
associated with severe pain and fever |
|
|
What is the treatment of a morbilliform drug eruption?
|
D/c offending agent
calamine lotion cool compresses benadryl |
|
|
How do you differentiate TEN from SJS?
|
skin biopsy
|
|
|
What is the mortality of TEN
|
15-20%
|
|
|
What are the causes of TEN?
|
-Drugs: sulfa, penicillin, ASA, barbiturate, phenytoin, carbamazepine, NSAIDs
-post vaccination agains measles, small pox, polio -associated with lymphoma |
|
|
What are physical exam findings of TEN?
|
Nikolsky sign
skin is tender + mucous membrane involvement |
|
|
What is the management of TEN?
|
DC offending agent
fluid replacement aggressive infection control systemic corticosteroids are controversial |
|
|
What are the causes of urticaria?
|
food
plants textile cosmetics animal dander topical medications chemicals hereditary infections cholinergic urticaria |
|
|
What are koplik spots?
|
irregular bright red spots with bluish-white centres on the buccal mucosa
|
|
|
What are the complications of rubella?
|
encephalitis
arthritis thrombocytopenia fetal damage |
|
|
What is the complication of erythema infectious?
|
aplastic anemia
fetal hydrops |
|
|
What are precipitating factors for erythema multiform?
|
Drugs and HSV
Fungal infection Collagen vascular disease pregnancy malignancy |
|
|
What is associated with erythema marginatum?
|
Rheumatic fever
|
|
|
How is pediculosis diagnosed?
|
by seeing nits (white dots at the base of the hair or adult lice)
|
|
|
What is the treatment of pediculosis?
|
Permethrin applied to hair after shampooing
|
|
|
What is erythema nodosum associated with?
|
Drug induced
URI Streptococcal infection IBD SLE histoplamosis Yersinia |
|
|
What is pemphigus vulgaris?
|
A bullous disease.
Any area of the body affected cause unknown common in Jewish, Mediterranea, or south Asian descent |
|
|
What is the treatment for herpetic whitlow?
|
Acyclovir
Analgesics Cover lesion to prevent transmission |
|
|
What is the differential for purpura?
|
Thrombocytopenic:
-idiopathic/ITP -TTP -drug induced -splenomegaly -aplastic anemia -malignancy -TB -Sarcoidosis -SLE Non thrombocytopenic -drugs -qualitative platelet deffect -infection (meningococcemia, RMSF) -Vasculitis |
|
|
What are commonly used drugs that may be associated with purpura?
|
Amitriptyline
ASA Chloramphenicol Chlorpromazine Furosemide HCTZ Isoniazid Sulfonamides Penicillin |
|
|
What is bullous pemphigoid
|
A chronic autoimmune subepidermal blistering skin disease that rarely involves mucous membranes.
May be precipitated by UV radiation, xray therapy and exposure to drugs such as furosemide, ibuprofen, other anti-inflammatory agents, captopril, penicillamine -predilection for flexural areas |
|
|
What is the differential of a bullous rash?
|
Bullous impetigo
Bullous pemphigoid Pemphigus vulgaris Stevens Johnson syndrome Toxic epidermal necrolysis Epidermolysis bullosa acquisita Bullous lupus Bullous scabies |
|
|
What is the differential for life-threatening maculopapular rash in kids?
|
Staphylococcal scalded skin syndrome
SJS TEN TSS RMSF Rash associated with early meningococcemia Secondary syphilis |
|
|
Compare chicken pox and smallpox with respect to prodromal signs
|
Chickenpox - mild or absent prodrome
smallpox 1-4 ays of systemic signs |
|
|
Compare chicken pox and smallpox with respect to illness severity
|
Chikenpox - illness usually not severe
small pox - very ill from onset, may be toxic |
|
|
Compare chicken pox and smallpox with respect to lesion development
|
chickenpox - superficial vesibles developing rapidly in multiple stages
small pox - hard circumscribed pustules developing slowly, lesions in same stage in every affected area |
|
|
Compare chicken pox and smallpox with respect to lesion location
|
chickenpox - commonly on face and trunk
small pox - commonly on face and extremities, including palms and soles |
|
|
Compare chicken pox and smallpox with respect to contagiousness
|
chickenpox contagious until all lesions crusted over
smallpox contagious until all scabs have fallen off |
|
|
What rashes involve the palms and soles?
|
Dissminated gonorrhea
Syphilis Erythema multiform RMSF Hand foot and mouth disease Small pox |

