![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
74 Cards in this Set
- Front
- Back
|
What are the symptoms of a mass effect?
|
changes in vision, HA, seizures
|
|
|
What causes prolactinoma? What is the presentation?
|
tumor secretes excess prolactin which inhibits GnRH therefore decrease LH and FSH --> amenorrhea, galactorrhea, hirsutism, impotence, hypogonadism
|
|
|
What is used to diagnose prolactinoma? What is the treatment?
|
1. prolactin levels > 200ng/mL (seen in macroadenoma, >1cm); normal prolactin levels < 20ng/mL
2. bromocriptine or carbegoline; transphenoid surgery if fails |
|
|
How does hypothyroidism cause hyperprolactinemia?
|
hypothyroidism causes elevation of TRH which inhibits dopamine --> increase prolactin levels
|
|
|
What is the cause of acromegaly? How does it present?
|
tumor in the anterior pituitary producing excess GH which stimulates the liver to produce IGF (insulin like growth factor) leading to gluconeogensis and inhibition of peripheral action of insulin (causing hyperglycemia) --> large hands & feet, frontal bossing, deep voice, carpal tunnel, skin tags, colonic polyp, HTN
|
|
|
What can you use to help make the diagnosis of acromegaly, what is the confirmation test? What is the treatment?
|
1. initially with serum IGF-1 (should be elevated) --> confirm with GH levels using oral glucose tolerance test (normally GH is decreased with glucose but remains elevated in GH in acromegaly); CT/MRI for tumor size
2. transphenoid resection is initial treatment --> octreotide & lantreotide if GH levels remain; last resort is pegvisomant (GH receptor blocker) bromocriptine and carbegoline no longer recommended for acromegaly |
|
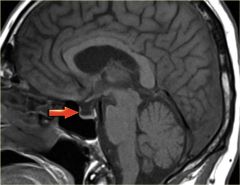
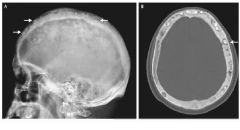
What is empty sella syndrome? How does it present?
arrow shows an empty sella |
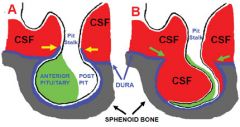
pituitary tissues normally sits at the sella but is pushed to the side or becomes flattened by invaginating diaphragm of the subarachnoid space --> OVERWEIGHT female with CONTINUOUS HEADACHE with confirmation of CT/MRI showing empty sella
no treatment is needed |
|
|
What causes Sheehan syndrome? How does it present?
|
due to infarction of the pituitary after pregnancy because of severe postpartum hemorrhage --> FATIQUE, WEIGHT LOSS, INABILITY TO LACTATE; can be panhypopituitarism or deficient in one hormone
|
|
|
What causes pituitary apoplexy? How does it present? What is used to help make the diagnosis? What is the treatment?
|
1. from bleeding into the pituitary or sudden pituitary infarction (lack of blood supply to the pituitary) from DM, warfarin, or recent radiation --> HA, N/V, DIPLOPIA, vertigo, altered mental consciousness, meningismus
2. CT/MRI shows bleed in the pituitary 3. steroids if mild; surgery if severe |
|
|
What is the most common cause of GH deficiency? How does it present?
|
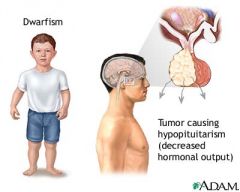
most common from a pituitary adenoma --> central obesity, hyperlipidemia, increase waist-hip ratio, decrease lean body mass; in children it causes dwarfism
|
|
|
What is used to diagnose GH deficiency, what is the confirmation test? How is it treated?
|
1. initialy test should reveal low IGF-1 levels; confirm test --> low GH levels even with induced hypoglycemia
2. human recombinant GH |
|
|
What is the cause of neurogenic (central) DI? How does it present?
|
lack of ADH production leading to polyuria, polydipsia, nocturia etc
|
|
|
What is used to help make the diagnosis of central DI? What is the treatment?
|
1. patient will have elevated sodium >142, urine is extremely dilute; in water deprivation test (restrict fluid) --> patient has low vasopressin (ADH) levels, next give SQ vasopressin or intranasal desmopression will increase urine osmolality by more than 50%
2. desmopressin (DDAVP) & fluids |
|
|
What is the cause of nephrogenic DI? How does it present?
|
kidneys are not able to respond to ADH due to damage from hypercalcemia, lithium induced DI, etc --> polyuria, polydipsia, nocturia, etc
|
|
|
What is used to help make the diagnosis of nephrogenic DI? What is the treatment?
|
1. plasma vasopression is NORMAL/elevated & administration of SQ vasopressin (ADH) or intranasal desmopression there will be no change in urine osmolality
2. thiazide diuretics (hydrochlorothiazide, amiloride, chlorthalidone)-works by decreasing urine flow to the distal tubule so more water can be reabsorbed by the distal collecting duct |
|
|
Differentiate between primary thyroidism vs secondary thyroidism
|
primary thyroidism affects the thyroid gland itself; secondary thyroidism affects the pituitary
|
|
|
Describe Hashimoto thyroiditis. How does it present?
|
autoimmune disease in which there is antibodies to the thyroid gland [ANTITHYROPEROXIDASE antibodies & ANTITHYROGLOBULIN antibodies] against TSH receptor --> painless goiter (enlarged thyroid) & hypothyroidism (fatique, amenorrhea, galactorrhea, constipation, depression, hair loss, dry skin, cold intolerance)
|
|
|
What lab findings would you see in hypothyroidism? What is the treatment?
|
1. low free T4 and elevated TSH levels
2. oral levothyroxine (start low dose in heart disease pts; celiac disease can cause decrease absorption) |
|
|
Define myxedema. What is the treatment?
|
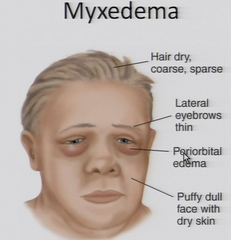
1. severe form of hypothyroidism with CHANGE IN MENTAL STATUS, HYPOTHERMIA, hyponatremia, hypoventilation
2. IV T4 or T3 with corticosteroids (until adrenal insufficiency is ruled out) |
|
|
Describe Graves disease. How does it present?
|
autoimmune disease in which the body produces thyroid stimulating antibodies that act on the RECEPTOR of thyroid gland (+ANTIMICROSOMAL & ANTITHYROGLOBULIN) --> exopthalmos, diffuse goiter, dermopathy and other autoimmune disease; sxs of hyperthyroidism (anxiety, panic attacks, hair loss, weight loss, polyphagia, diarrhea, irregular menses, osteopenia)
antithyroglobulin is also seen in hashimoto thyroiditis(antithyroperoxidase antibody) |
|
|
What lab findings would help you make the diagnosis of Graves disease? How is it treated?
|
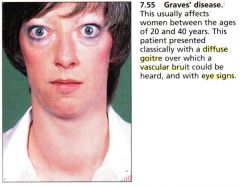
1. +antimicrosomal antibodies, +antithyroglobulin antibodes; decrease TSH, increase T4, increase radioactive iodine uptake (RAIU)
2. BB then thionamide[PTU or methimazole); once stable consider radioactive iodine ablation; PTU is safe during pregnancy; subthyroidectomy > total ablation during pregnancy @ 2nd trimester |
|
|
Describe toxic multinodular goiter (Plummer disease).
|
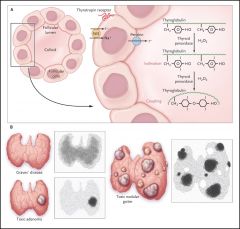
hyperfunctioning of thyroid nodules --> enlarged thyroid nodular gland and sxs of hyperthyroidism ( anxiety, panic attacks, weight loss, polyphagia, diarrhea, weakness, irregular menses, osteopenia, etc);
tx --> BB then thionamide (PTU or methimazole) |
|
|
In subclinical hyperthyroidism, patients present with low TSH but normal free T4 levels. There are no symptoms except an increase risk of osteoporosis and A-fib. What is the management of this disease?
|
consider methimazole if TSH < 0.1
|
|
|
Describe subacute thyroiditis. How does it present? What labaratory would help make the diagnosis? What is the treatment?
|
1. inflammation of the thyroid after a viral infection --> fever, neck pain, hyperthyroidism then hypothyroidism
2. decrease RAIU (radioactive iodine uptake) 3. NSAIDs and steroids |
|
|
Define thyroid storm. What is the treatment?
|
1. complication of hyperthryoidism --> delirum, fever, psychosis, A-fib or CHF
2. BB, PTU, iodine, steroids |
|
|
Define sick euthyroid syndrome. What lab findings will help you make the diagnosis?
|
1. dysfunction of the thyroid from a medical illness; often confused with hypothyroidism
2. low TSH, LOW T3, INCREASE REVERSE T3 [rT3], VARIABLE T4; increase rT3 because there is a change in metabolism from T4 -->rT3 |
|
|
You discover a nodule in the thyroid of your patient. You then order a serum thyroid function test and discover these results, what is your diagnosis?
1. low TSH and then get thyroid scintigraphy, if positive 2. high TSH, then get antithyroperoxidase antibody 3. normal TSH get FNA biopsy 4. if nondiagnostic get an US guided FNA or repeat FNA |
1. toxic multinodular goiter
2. Hashimoto thyroiditis 3. -85% are adenoma, cystic cells -if malignant do surgery -if indeterminant get thyroid scintigraphy *cold nodule [nonfunctioning] do surgery *warm nodule[functioning] observe -papillary carcinoma cannot be diagnosed with FNA but follicular carcinoma can be diagnosed with FNA |
|
|
Describe these thyroid cancers.
1. papillary carcinoma. How is it spread? 2. follicular carcinoma. How is it spread? 3. anaplastic carcinoma. |
1. most common type of thyroid cancer, spread via the LYMPHATICS; increase risk with RADIATION EXPOSURE
2. spread via HEMATOGENOUS (blood) 3. worst prognosis, seen in elderly, invades HEAD AND NECK DIRECTLY |
|
|
What hormones are produced by the adrenal cortex and medulla?
|
![1. cortex --> "GFR" [glomerulosa, fasiculata, reticularis] salt, sugar, and sex (androgens/estrogens)
2. medulla --> secretes epinephrine (under sympathetic nervous system control)](https://images.cram.com/images/upload-flashcards/30/21/86/5302186_m.jpg)
1. cortex --> "GFR" [glomerulosa, fasiculata, reticularis] salt, sugar, and sex (androgens/estrogens)
2. medulla --> secretes epinephrine (under sympathetic nervous system control) |
|
|
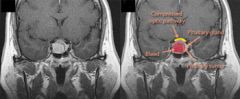
Differentiate Cushing syndrome from Cushing disease.
other causes of Cushing syndomes: ectopic ACTH production (bronchial carcinoid, small cell lung cancer, medullary thryoid cancer), cortisol secreting tumor, adrenal adenoma --> sxs depression, osteopenia, proximal muscle loss, moon facies, buffalo hump, central obesity, facial plethora, abdominal striae, peripheral insulin resistance (hyperglycemia), increase ACTH (causing hyperpigmentation |
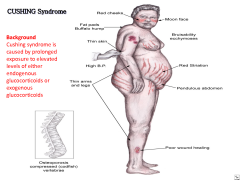
cushing syndrome is excess cortisol production from the adrenal cortex or excess intake of glucocorticoids; cushing disease is due to pituitary adenoma that secrets ACTH
|
|
|
What tests should you order to help make the diagnosis of Cushing syndrome? What is the treatment?
|
1. initially with a 24 hour urine cortisol level or 1mg overnight dexamethasone suppression test
2. then 8mg dexamethasone suppression test -if ACTH is suppressed = pituitary adenoma -if ACTH is not suppressed = ectopic ACTH producing tumor or adrenal tumor *if ACTH levels are high get CT (r/o lung cancer) or MRI (r/o adenoma) *if ACTH levels are low get CT abdomen 3. treatment is resection; if can't give KETOCONAZOLE, ETOMIDATE, MITODRINE |
|
|
Define adrenal insufficiency. What is the most common cause? How does it present?
|
low cortisol levels; most common cause is from sudden steroid removal after using steroids > 2 weeks; low mineralcorticoid levels--> hypotension, hypoglycemia, hyperkalemia, hyponatremia, sparse body hair, orthostatic hypotension, weakness/fatique, abdominal pain, hyperpigmentation (only seen with primary adrenal insufficiency because increase ACTH and POMC-proopiomelanocortin)
|
|
|
Differentiate between primary adrenal insufficiency vs secondary adrenal insufficiency.
|
1. primary adrenal insufficiency is from the adrenal gland itself) --> addison disease (MCC), bilateral adrenal hemorrhage, TB, Waterhouse-Friederichsen syndrome, surgical removal
; will have HYPERPIGMENTATION due to elevated ATCH and POMC 2. secondary adrenal insufficiency is from the pituitary therefore insufficient ACTH |
|
|
What is used to diagnose adrenal insufficiency? What lab findings suggest primary vs secondary/tertiary cause of adrenal insufficiency? How do you treat acute adrenal crisis? How do you treat it chronically?
|
1. initially get morning serum cortisol and ACTH levels
-normal response=cortisol levels > 18ug/dL -low cortisol & high ACTH =primary adrenal insufficiency (next get CT scan) -low cortisol & low ACTH = secondary or tertiary (hypothalamus) insufficiency; next step is to get an MRI of the brain 3. high dose of dexamethasone & fluids (get blood levels of cortisol, ACTH, and renin before giving dexamethasone) 4. in chronic disease --> give stress dose during stress/infection/surgery; oral glucocorticoid (hydrocortisone, dexamethasone, prednisone) for both primary and secondary adrenal insufficiency; PLUS MINERALCORTICOID replacement (FLUDROCORTISONES) for PRIMARY DISEASES ONLY |
|
|
What is the treatment of Schmidth syndrome (patient with adrenal and thyroid insufficiency)?
|
give glucocorticoid 1st before giving levothyroxine to prevent precipitation of adrenal crisis
|
|
|
What are the causes of primary vs secondary hypoaldosteronism? How does it present? What is the treatment?
|
1. primary hypoaldosteronism is due to the dysfunction of the adrenal gland caused by Addison disease, infection, trauma, ACEi (inhibits aldosterone release from decreasing angiotensin II), surgical resection, hemorrhage
2. secondary hypoaldosteronism is due to decreased decreased renin (from RTA type 4, loss of kidneys, NSAIDs, and BBs etc) 3. patient presents with symptoms of hyponatremia, hyperkalemia, metabolic acidosis 4. oral fludrocortisone (a mineralcorticoid) |
|
|
Differentiate the cause between primary hyperaldosteronism vs secondary hyperaldosteronism. How does it present?
|
primary hyperaldosteornism is due to CONN SYNDROME (most common), adrenocortical carcinoma, or bilateral hyperplasia; secondary hyperaldosteronism is due to excess RENIN (from hypoperfusion) --> patient presents with HTN, hypokalemia, and metabolic alkalosis
|
|
|
What labs would you get to help make the diagnosis of hyperaldosteronism (primary vs secondary)? What is the treatment?
|
1. initially get renin levels
-in primary aldosteronism, LOW RENIN levels that does not increase even after volume depletion and high aldosterone -in secondary aldosteronism, aldosterone levels is still high even AFTER SUPPRESSION WITH HIGH SALINE LOAD AND HIGH RENIN 2. next best step is to get plasma aldosterone:renin ratio -if plasma ratio > 30 --> primary disorder -if plasma ratio < 10 --> secondary disorder 3. in primary disease --> surgery if aldosteronoma; oral spironolactone or eplerenone for bilateral hyperplasia or nonresectable adenomas in secondary disease --> angioplasty/stent for renal artery stenosis; surgery for adrenal carcinoma or mitotane if nonresectable |
|
|
In apparent mineralocorticoid excess, it is described as a disease that is similar to primary hyperaldosteronism but with LOW SERUM ALDOSTERONE, sxs present as HTN, hypokalemia, metabolic alkalosis, and LOW RENIN. What do you find in lab workup to help make the diagnosis?
|
high deoxycorticosterone from deficient 11-B-hydroxysteroid dehydrogenase
|
|
|
Define pheochromocytoma. What is the rule of 10s? How does the disease present?
a/w MEN type 2, von Hippel-Lindau disease, neurofibromatosis type 2, familial carotid body tumors |
1. a tumor in the adrenal that produces excess catecholamines --> palpitations, pallor, perspiration, panic, pounding headache, increase BP
2. 10% bilateral, 10% extraadrenal, 10% malignant |
|
|
What lab findings or labs can you order to help make the diagnosis of pheochromocytoma? What is the treatment?
|
1. elevated METANEPHRINES AND; if test is equivocal can order clonidine suppression test (should decrease epinephrine); best next step is to get a CT or MRI to localize the tumor or metaiodobenzylguanidine (MIGB) or I-MIGB or I-scan if CT or MRI scan is negative
2. alpha blockage (phenoxybenzamine or phenotolamine) then BB for 10-14 DAYS then surgery |
|
|
Describe the 3 MEN. All are AD diseases.
|
1. MEN type 1: 3Ps --> pituitary, parathyroid, pancreatic (VIPoma, insulinoma, gastrinoma, serotonin, glucagonoma)
2. MEN type 2: parathyroid, pheochromocytoma, medullary thyroid carcinoma (increase calcitonin) - always check for RET - oncogene 3. MEN type 3: pheochromocytoma, medullary thyroid carcinoma, marfanoid body habitus, mucosal and digestive neurofibromatosis; always check for RET - oncogene |
|
|
Lab findings of primary male hypogonadism vs secondary male hypogonadism.
sxs of decrease libido, gynecomastia, fatique, hot flushes, erectile dysfunction |
1. primary hypogonadism --> low testosterone, high LH/FSH
2. secondary hypogonadism --> low testosterone, low/normal LH/FSH (secondary hypogonadism can be treated with testosterone replacement if patient is < 60 years of age seen in prostate cancer & erythrocytosis) |
|
|
Define metabolic syndrome. What criterias are needed to diagnose the disease? What is the treatment?
|

1. resistance to insulin (acanthosis nigrans is a sign of insulin resistance) therefore increase risk of becoming a diabetic.
2. 3/5 criteria --> male w/ waist > 40, female w/ waist > 35, blood glucose btw 100-125 (intermediate DM), BP >135 systolic or > 85 diastolic, triglyceride > 150, HDL < 40 male or < 50 female 3. diet, exercise, add statin if LDL remains high |
|
|
What are the 4 ways to diagnose DM?
|
HgA1c > 6.5%, fasting blood glucose > 126mg/dL (on 2 separate occasions), 2hr 75g oral glucose tolerance test > 200mg/dL, random glucose > 200mg/dL
|
|
|
Define honeymoon effect, dawn phenomenon, somogyi effect.
|
1. initial glucotoxicity of beta cells can inhibit insulin secretion but cells can be restored with tight glucose control and insulin (watch for hypoglycemia)
2. hyperglycemia in the morning but high glucose at 3AM from excess GH 3. hyperglycemia in the morning but low glucose at 3AM from excess NPH |
|
|
In monitoring DM, what is the function of glycosylated hemoglobin (HbA1c) and fructosamine (glycosylated albumin)?
|
1. HbA1c shows glucose control within the past 3-4 months
2. fructosamine shows glucose control within the past 3 weeks |
|
|
What is the criteria for DKA type 1? What is the treatment?
|
1. complication of type 1 DM with hyperglycemia > 250 mg/dL, INCREASED ANION GAP METABOLIC ACIDOSIS, (pH < 7.3; serum bicarbonate < 18), INCREASED SERUM BETA-HYDROXYBUTYRATE, ACETOACETATE, & ACETONE
2. IV fluids, 0.1 units/kg regular insulin IV then insulin drip at rate of 0.1 units/kg/hour; finger stick every hour *once blood glucose < 250 mg/dL change IV to D5-containing (D5W or D5 1/2 normal saline) solution *continue insulin drip until anion gap closed (ketoacids can only be converted to bicarbonate with presence of insulin) |
|
|
What is the criteria for hyperosmolar nonketotic coma (HONC - complication of type 2 DM)? What is the treatment?
|
1. HYPERGLYCEMIA 600-1000 mg/dL, neurological symptoms (possible coma), pH < 7.3, little to no keoacidosis, plasma osmolality > 330 mOsmol/kg
2. treatment is like DKA type 1 IV fluids, 0.1 units/kg regular insulin IV then insulin drip at rate of 0.1 units/kg/hour; finger stick every hour *once blood glucose < 250 mg/dL change IV to D5-containing (D5W or D5 1/2 normal saline) solution *continue insulin drip until anion gap closed (ketoacids can only be converted to bicarbonate with presence of insulin) |
|
|
In treating complications of DM, you might end up having hypokalemia. What is the treatment of hypokalemia, when should you stop giving insulin?
|
stop insulin if K <3.3; give KCl with 1/2 NORMAL SALINE at a rate of 20-30 mEq of KCl/hr if serum K < 5.3 meq/dL
|
|
|
In treating acidosis from DM, when can you use bicarbonate (what type of DM complication)?
|
add IV bicarbonate only if pH < 7.10 (applies only to DKA)
|
|
|
What is the treatment for DM type 1?
|
insulin
-rapid acting: lispro, aspart, glulisine -short acting insulin: regular -intermediate acting: NPH -basal insulin: glargine, detemir |
|
|
What is the treatment of DM type 2?
|
lifestyle modification --> metformin --> 2nd oral agent such as GLP-1 (incretins-exanatide) or DPP-4 inhibitors (sitagliptin) or insulin therapy alone (choose long acting agent)
*insulin therapy alone is preferred in ESRD patient *if dual oral therapy fails to control HgA1c give TZDs "glitazones" [rosiglitazone, pioglitazone] or sulfonylurea [glipizide, glyburide, glimepride] as 3rd oral agent |
|
|
What is the mechanism of biguanides (metformin) in treating DM? What is the AE?
|
1. decrease glucose production in the liver and decrease glucose absorption in the intestines
2. AE --> LACTIC ACIDOSIS (esp with serum creatinine > 1.4 in females, > 1.5 males); avoid in chronic renal patients, hepatic disease, CHF, COPD, and alcohol abuse |
|
|
What is the mechanism of GLP-1 (glucagon like peptide) such as incretins [exenatide] in treating DM type 2?
|
inhibits glucagon secretion; reduce gastric emptying and stimulate insulin release; NAUSEA in 30% of patients
|
|
|
What is the mechanism of dipeptidyl peptidase-4 inhibitors (sitagliptin) [DDP-4 inhibitors] in treating DM type 2?
|
inhibits enzyme that metabolizes GLP-1 (glucagon like peptide 1)
|
|
|
What is the mechanism of sulfonylureas (glipizide, glyburide, glimepiride) in treating DM type 2?
|
increase insulin release from beta cells; most commonly a/w with HYPOGLYCEMIA
|
|
|
What is the mechanism of thiazolidinediones "-glitazones" [rosiglitazone, pioglitazone] in treating DM type 2? What is the AE?
|
1. decrease insulin resistance & increase pancreatic B cell function
2. AE --> acute CHF exacerbation & bone loss |
|
|
What is the mechanism of alpha-glucosidase inhibitors (acarbose, miglitol) in treating DM type 2?
|
inhibits enzyme that digests complex carbohydrates; AE --> abdominal cramping
|
|
|
In what type of state is calcium found in the body?
|
mostly bound to albumin and free fractions
|
|
|
A patient presents with low calcium, you then check the albumin level. It is < 4g. How would you determine the "real" calcium level?
|
add 0.8 mg to serum calcium for every 1 g of albumin < 4g
|
|
|
What is a precise way to measure urinary excretion of calcium?
|
measuring urine calcium:creatine ratio
|
|
|
What is the treatment of serum calcium 12-14 (excess calcium) without symptoms? What is the treatment of calcium 12-14 with symptoms or calcium > 14?
|
1. oral bisphophonates
2. normal saline & subcutaneous calcitonin --> then start IV bisphosphonates --> oral bisphosphonates |
|
|
What causes primary hyperparathyroidism? How does it present?
|
single adenoma (most common cause), multiple adenomas, MEN syndrome, rarely parathyroid cancer --> kidney stones, osteopenia, bone cysts, resorption of distal phalanges
|
|
|
What lab findings would you find in primary hyperparathyroidism? What is the treatment?
|
1. elevated PTH (only in primary parathyroidism & FHH - all other diseases are low), elevated Ca, low phosphate
2. surgery if : serum > 12mg/dL, low bone density (T scores less than -2), osteitis fibrous cystica, kidney stones (nephrolithiasis), urine calcium < 400mg/day start BISPHOSPHONATES if serum <12 mg/dL, CI to surgery; add phosphate replacement and recommend low calcium diet < 400mg/day, increase water intake |
|
|
Define familial benign hypocalciuric hypercalcemia (FHH). How can you differentiate it from primary hyperparathyroidism? Do you need to treat it?
|
1. AD genetic disease in which calcium sensing receptors are partially inactivated --> increase PTH when calcium levels are normal
2. presents with symptoms that is similar to primary hyperparathyroidism except urinary EXCRETION OF CALCIUM < 200mg/day; family history with "failed" thyroid surgery or asymptomatic 3. no treatment is necessary but recognize to avoid unnecessary surgery |
|
|
How is calcium elevated in hypercalcemia of malignancy (ex: squamous cell carcinoma of the lungs)? What is the treatment?
|
elevated calcium levels due to increase PTH-related peptide (PTH-rP) from malignancy; treatment is with bisphosphonates
|
|
|
Why is calcium elevated (hypercalcemia) in granulomatous disease (TB, sarcoidosis, histoplasmosis, berylliosis, silicone breast implants)?
|
due to macrophages containing 1-alpha-hydroxylase
|
|
|
Describe milk alkali syndrome?
|
damage of the kidneys due to increase calcium; most common cause is from ingestion of calcium carbonate with decreases excretion of calcium and bicarbonate due to kidney failure (mech: decrease PTH --> decrease pohsphate clearance causing hyperphosphatemia which then causes excess calcium to deposit in the kidneys causing kidney stones which then damages the kidneys)
|
|
|
What are the sxs of hypocalcemia? What is the EKG findings?
from surgical removal of all parathyroid glands, primary hypoparathyroidism, magnesium deficiency, vitamin D deficiency, hungry bone syndrome, etc |
1. NUMBNESS, depression, cramps, fatique, anxiety, neuromuscular irritability
2. PROLONG QT INTERVAL |
|
|
Describe pseudohypoparathyroidism. What are the lab findings?
|
defective PTH receptor therefore increase PTH, increase phosphate, decrease calcium
|
|
|
Define pseudohypocalcemia. What is the cause?
|
normal ionized calcium but low calcium from low albumin (once corrected for low albumin; add 0.8 mg of serum calcium to each 1g of albumin below 4g, calcium levels are normal)
|
|

Describe paget disease of the bone. How does it present?
|
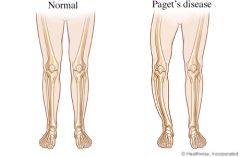
due to abnormal destruction and reformation of bones leading to bowing of the leg, abnormal growth of bones that can cause deafness (compressing on CN VIII)
|
|
|
What labs and diagnostic test can help confirm the diagnosis of paget disease of the bone? What is the treatment?
|
1. labs will reveal only ELEVATED ALKALINE PHOSPHATASE (normal calcium levels, etc; no history of liver disease); xray of the skull will show "hair on end" or "cotton wool" appearance
2. bisphosphonates is first line --> calcitonin |

