![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
110 Cards in this Set
- Front
- Back
|
When are ungated potassium channels open?
|
They are always open, unless the membrane potential has reached the potassium equilibrium potential.
|
|
|
Voltage-gated sodium channels are ________ (open/closed) under resting conditions.
|
closed
|
|
|
Voltage-gated sodium channels open and close ________ (quickly/slowly).
|
quickly
|
|
|
Voltage-gated calcium channels are ______ (open/closed) under resting conditions.
|
closed
|
|
|
Compare opening of sodium-channels and calcium-channels.
|
Voltage-gated calcium channels open more slowly than sodium channels upon depolarization of the cell membrane.
|
|
|
Voltage-gated calcium channels are sometimes called what?
|
(1) Slow channels
(2) L-type (long-acting) |
|
|
What is the role of calcium that enters the cardiomyocyte via voltage-gated calcium channels?
|
(1) Contraction (minor role)
(2) Calcium-induced release of calcium from SERCA |
|
|
What are the two most important voltage-gated potassium channels called?
|
(1) Inward rectifying channels (iK1)
(2) Delayed rectifying channels (iK) |
|
|
What type of voltage-gated potassium channels are only present in ventricular cells?
|
Inward rectifying channels (iK1)
|
|
|
Describe the inward rectifying potassium channels (iK1).
|
Open under resting conditions (at negative membrane potentials). Depolarization closes them. Closes during depolarization and main part of plateau phase.
|
|
|
Rectifying means?
|
Repolarization
|
|
|
Why is low potassium conductance during the plateau phase so important?
|
Depolarization would cause excessive loss of potassium from the cell during the plateau if there wasn't inward rectifying channels (iK1).
|
|
|
Describe delayed rectifying potassium channels (iK).
|
These potassium channels work just like in nerves. They open with depolarization and closes when the cell is repolarized.
|
|
|
Why are delayed rectifying potassium channels (iK) called delayed?
|
They are very slow to open. They typically open late in the plateau phase of the action potential to speed repolarization.
|
|
|
Fast fibers include?
|
(1) Ventricular fibers
(2) Atrial fibers (3) Purkinje fibers |
|
|
Slow fibers include?
|
(1) SA nodal fibers
(2) AV nodal fibers |
|
|
Fast fibers can be converted into _________.
|
slow fibers
|
|
|
What is the significance of phase 2 of the ventricular action potential?
|
It is long and allows time for contraction.
|
|
|
When is potassium conductance during the ventricular action potential the lowest?
|
Phase 2. Inward rectifying potassium channels (iK1) are closed.
|
|
|
What is meant by excitation-contraction coupling in the heart?
|
As ventricle is conducting, it also contracts.
|
|
|
Describe phase 0 of the ventricular action potential.
|
Fast channels open quickly (voltage-gated sodium channels) and there is an increase in conductance to sodium. Na-influx then causes depolarization. Then they close quickly
|
|
|
Describe phase 1 of the ventricular action potential.
|
There is a slight repolarization due to a transient potassium current (Ungated-potassium channels) and the closing of sodium channels.
|
|
|
What ventricular fibers lack a phase 1 in their action potential?
|
Subendocardial fibers.
|
|
|
Describe phase 2 of the ventricular action potential.
|
L-type calcium channels are now open and there is an increased conductance to calcium permitting a calcium influx. iK1 are closed.
|
|
|
What would happen if voltage-gated potassium channels (iK1) didn't close upon depolarization of the cell?
|
Excessive loss of potassium causing an early repolarization and then preventing the full development of the plateau phase.
|
|
|
Development of the plateau phase is dependent on what?
|
It is dependent on closing of voltage-gated potassium channels.
|
|
|
Describe phase 3 of the ventricular action potential?
|
L-type calcium channels close, decreasing conductance to calcium. Delayed rectifier iK channels are opening.
|
|
|
What would happen if the voltage-gated potassium channels did not open during phase 3?
|
The cell would still repolarize but more slowly, because of closure of calcium channels and potassium efflux through the ungated potassium channels.
|
|
|
Describe phase 4 of the ventricular action potential.
|
Conductance to potassium is high. Delayed rectifiers (iK) gradually close.
|
|
|
The specialized cells of the heart consist of?
|
Cells of the SA node, AV node and Purkinje fibers.
|
|
|
What is special about SA, AV and purkinje cells?
|
Unstable phase 4 (unstable resting membrane potential).
|
|
|
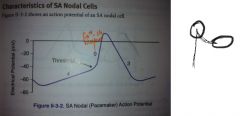
What does the action potential of an SA nodal cells lack that a ventricular action potential?
|
|
|
|
How is the initial resting membrane potential for SA nodal cells versus regular contracting fibers?
|
The initial RMP of SA nodal cells are not as negative.
|
|
|
What factors produce the pacemaker property?
|
(1) i_f (funny channel)
(2) iK channels close (3) Near the end of the pacemaker potential there is an increase in calcium conductance (calcium-T channel). |
|
|
When does the funny channel in SA nodal cells open?
|
When the cell repolarizes.
|
|
|
Describe phase 0, 3 and 4 of the SA nodal action potential.
|
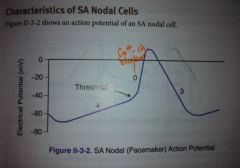
Phase 4: funny channel
Phase 0: slow calcium channel opens Phase 3: rapid potassium efflux |
|
|
Describe the molecular changes in SA nodal cells after sympathetic stimulation.
|
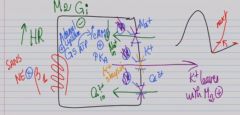
|
|
|
Draw the SA nodal action potential before and after NE stimulation.
|
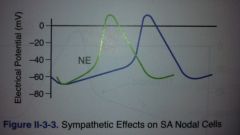
|
|
|
Draw the SA nodal action potential before and after acetylcholine stimulation.
|
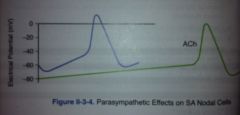
|
|
|
How does the AV nodal action potential compare to the SA nodal action potential?
|
AV node has slower rate of phase 4 depolarization.
|
|
|
Increased conduction velocity in the AV node means what on an ECG?
|

Decreased PR interval.
|
|
|
What is the effect of sympathetics and parasympathetics on the AV nodal cells?
|
Sympathetics increase conductance to Ca2+ (increase in rate of rise and height of phase 0). This increases conduction velocity.
Parasympathetics increase K+ conductance. This counteracts inward Ca2+ and decreases the rate of rise and the height of phase 0. |
|
|
Describe the conduction pathway in the heart.
|
SA node --> Atrial mm. --> AV node (delay) --> Purkinje fibers --> Ventricular mm.
|
|
|
The fastest conducting fiber in the heart is?
|
Purkinje cells
|
|
|
The slowest conducting fiber in the heart is?
|
AV nodal cells
|
|
|
What is the intrinsic rate of SA nodal cells?
|
100-120/min
|
|
|
What is the intrinsic rate of AV nodal cells?
|
40-60/min
|
|
|
What is the intrinsic rate of purkinje cells?
|
30-40/min
|
|
|
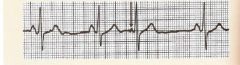
Draw a normal pattern of an ECG. Describe it.
|

P wave: Atrial depolarization
QRS complex: Ventricular depolarization R wave: First upward deflection. S wave: First downward deflection after an R wave T wave: Ventricular repolarization |
|
|
What is the R wave on an ECG?
|

The first upward deflection of ventricular depolarization is the R wave.
|
|
|
What wave/segment/interval roughly corresponds to the plateau phase of the action potential?
|
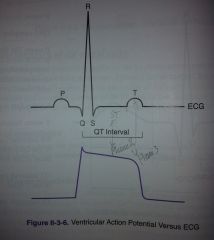
ST-segment
|
|
|
What is the standard chart speed of an ECG machine?
|
25 mm/sec
|
|
|
What is the size of a small box on an ECG chart paper?
|
1 mm
|
|
|
Each small division (1 mm) represents how much time on an ECG paper?
|
0.04 seconds
|
|
|
What does the PR interval include? Describe it.
|

PR interval includes conduction delay through atrial muscle and the AV node. Most of this interval is the result of slow conduction through the AV node.
|
|
|
Increased sympathetic activity decreases the PR interval. What is another cause of decreased PR interval?
|
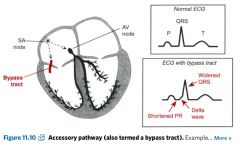
Accessory pathways which bypass the AV node (WPW syndrome).
|
|
|
What can lead to an increased PR interval?
|
(1) PANS
(2) Beta-blockers (3) Ca2+-channel blockers (4) Adenosine |
|
|
QRS duration should be less than _____ seconds.
|
0.12
|
|
|
What does prolonged QRS interval indicate?
|
Abnormal conduction through the ventricles.
|
|
|
What are some pathologies associated with shorter than typical QRS duration?
|
No pathologies are associated with this.
|
|
|
What is the QT interval?
|
It's a measure of the duration of a ventricular action potential which includes both ventricular depolarization and repolarization.
|
|
|
What can decrease the QT interval?
|
Anything that decreases the duration of the action potential: Ca2+ channel blockers, hyperkalemia,
|
|
|
A prolonged QT is often associated with what?
|
A prolonged QT interval is often associated with a conduction problem in the ventricular myocardium. It may lead to a potentially fatal arrhythmia (torsades).
|
|
|
The ST segment deviates from the isoelectric line on an ECG paper. What may this indicate?
|

Ischemic damage to the myocardium.
|
|
|
A QRS greater than ____ small boxes means prolonged QRS.
|
3
|
|
|
A PR-interval greater than ____ big box(es) means prolonged P-interval.
|
1
|
|
|
A wide QRS means what type of tachycardia?
|
Ventricular tachycardia
|
|
|
What makes the pen writing on an ECG paper deflect upward?
|
A wave of depolarization approaching a positive electrode.
|
|
|
How can you estimate the HR with ECG paper?
|
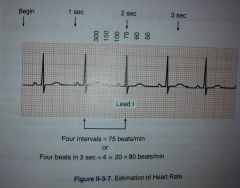
(1) Count the number of major divisions (stor boks, 5 mm) between R wave peaks. 300-150-100-75-60-50
(2) Interval method |
|
|
How does ventricular depolarization and repolarization proceed throughout the heart? Why?
|
Depolarization: Proceeds from endocardium to epicardium.
Repolarization: Proceeds from epicardium to endocardium. Epicardial cells have a shorter plateau (phase 2) and therefore repolarize sooner than endocardial cells. |
|
|
You want to estimate the heart rate by looking at an ECG, but it is irregular. How can you approximate it?
|
Count the number of complexes during 6 sec of the recording and multiplying that number by 10.
|
|
|
What can increase the QT interval?
|
(1) Hypocalcemia
(2) Hypokalemia (3) Hypomagnesemia (4) Long QT syndrome (5) Drugs |
|
|
What happens in a partial (First-Degree) block?
|
Slowed conduction through the AV node. The PR interval i increased (> 200 msec).
|
|
|
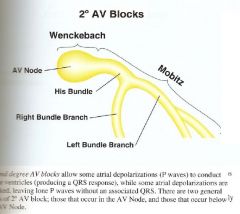
Describe second-degree heart block.
|
Every QRS is preceded by a P wave, though not every P wave leads to a QRS complex; some impulse are not transmitted through the AV node.
Mobitz I (Wenchebach): PR interval progressively lengthens Mobitz II: No measurable lengthening of the PR interval |
|
|
How would an ECG look in Wolff-Parkinson White syndrome?
|
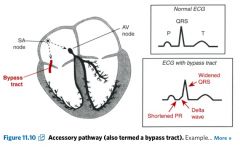
Shortened PR interval, widened QRS, slurred upstroke of the R wave
|
|
|
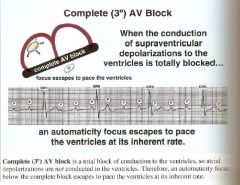
What happen with conduction in complete (Third-Degree) heart block?
|
No impulses are conducted from the atria to ventricles. Atria and ventricles beat independently.
|
|
|
Give examples of causes leading to third-degree heart block.
|
(1) Caused by IgG anti-SS-A (Ro) antibodies crossing the placenta (SLE).
(2) Lyme disease (3) Heart block occurs in 5% of those with inferior AMI and 3% of those with anterior AMIs. |
|
|
What is the consequence(s) of third-degree block?
|
The low HR is associated with a lower than normal CO and syncope.
|
|
|
Tx of third-degree block?
|
Implantation of pacemaker can alleviate the problem.
|
|
|
What is WPW syndrome?
|
Syndrome where there is an accessory pathway present between the atria and ventricles.
|
|
|
What may happen in WPW syndrome?
|
The cardiac impulse can travel in retrograde fashion to the atria over the accessory pathway and initiate a reentrant tachycardia.
|
|
|
How do you read an ECG in an appropriate and systematic way?
|
Rate --> Rhythm --> Intervals
|
|
|
Compare normal and pathological Q waves in an ECG.
|
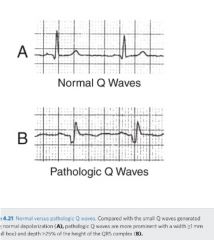
|
|
|
What should you routinely do when assessing an ECG?
|
Look for long QT syndrome.
|
|
|
What is the role of phospholamban?
|
To regulate the return of Ca++ from the cytosol to the SR.
|
|
|
What is used to record a lead?
|
A pair of electrodes (+ & -)
|
|
|
How do we attach limb electrodes?
|
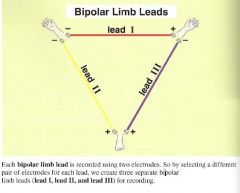
|
|
|
Why are limb leads called bipolar?
|
Each limb lead consists of a pair of electrodes, one is positive and one is negative, so these leads are caled "bipolar" limb leads.
|
|
|
Lead I is horizontal, and its left arm electrode is _________ (positive/negative) while its right arm electrode is negative.
|
positive
|
|
|
What is "Einthoven's triangle"?
|
The bipolar limb lead configuration.
|
|
|
The AVF lead uses the left foot electrode as ___________ (positive/negative) and both arm electrodes as _________.
|
positive; common ground (negative)
|
|
|
To obtain the AVR, AVL and AVF leads, these limbs are made positive. What are they?
|
AVR - Right arm positive
AVL - Left arm positive AVF - Foot (left foot) positive |
|
|
Limb leads are composed of what?
|
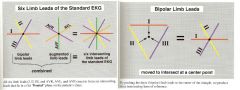
|
|
|
Why do we have so many limb leads?
|
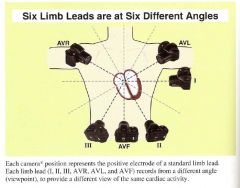
|
|
|
Explain that a wave of depolarization causes an upward deflection on the EKG.
|
A wave of depolarization is a progressive wave of positive charges passing through the myocardial cells. So, when a depolarization wave moves toward a positive electrode, a positive (upward) deflection is produced on the EKG for that particular lead.
|
|
|
Leads I and AVL are called what? And why?
|
Lateral leads (left lateral understood) because each has a positive electrode positioned laterally on the left arm.
|
|
|
Leads II, III and AVF are called what? Why?
|
Inferior leads, because each of these leads has a positive electrode positioned inferiorly on the left foot.
|
|
|
If leads V1 through V6 are imaged to be the spokes of a wheel, the center of the wheel is the ________.
|
AV Node
|
|
|
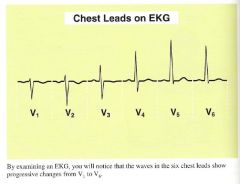
What changes from lead V1 through V6?
|
|
|
|
These chest leads are oriented over the right heart and left heart, respectively.
|
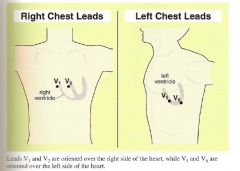
|
|
|
These leads are oriented over the interventricular septum.
|
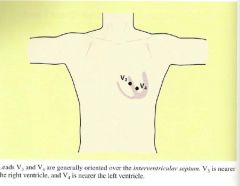
|
|
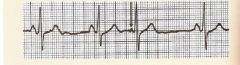
What do you see?
|
Premature beat - an irritable focus spontaneously fires a single stimulus earlier than expected in the rhythm. Atrial and junctional foci become irritable because of increase sympathetic activity, epinephrine, caffeine and stimulants.
|
|
|
Where do we see mobitz and wenchebach blocks in the conduction system in the heart?
|
|
|
|
Draw an example of second degree heart block (both types).
|
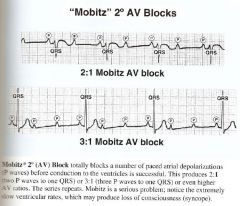
|
|
|
What is a third degree heart block? Draw an EKG example.
|
|
|
|
Draw an example of a wenchebach EKG.
|
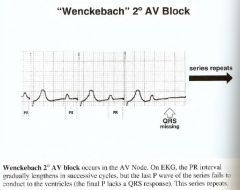
|
|
|
What is normal variation in the mean electrical axis of the haert?
|
It may be within -30 to +110 degrees.
|
|
|
Left axis deviations are caused by?
|
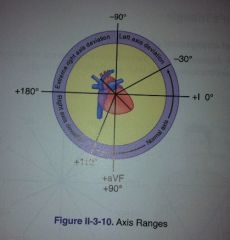
(1) Left heart enlargement, either LV hypertrophy or dilation
(2) Conduction defects of LV (3) Acute MI on right side |
|
|
Right axis deviations are caused by?
|
(1) Right heart enlargement, hypertrophy, or dilation
(2) Conduction defects of RV (3) Acute MI on left side tends to shift axis right unless LV dilates |
|
|
The mean electrical axis of the heart tend to move toward ________ tissue and away from _________ tissue.
|
hypertrophied; infarcted
|

