![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
7 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
How is cirrhosis defined histologically |
Cirrhosis is defined histologically as a diffuse hepatic process characterized by fibrosis and the conversion of normal liver architecture into structurally abnormal nodules. The progression of liver injury to cirrhosis may occur over weeks to years. Indeed, patients with hepatitis C may have chronic hepatitis for as long as 40 years before progressing to cirrhosis. |
|
|
|
What is the liver fibrosis? |
Many forms of liver injury are marked by fibrosis, which is defined as an excess deposition of the components of the extracellular matrix (ie, collagens, glycoproteins, proteoglycans) in the liver. This response to liver injury potentially is reversible. By contrast, in most patients, cirrhosis is not a reversible proces |
|
|
|
What is the pathogenesis of liver fibrosis |
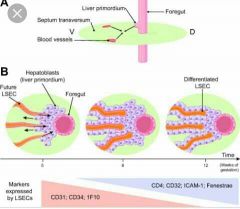
The development of hepatic fibrosis reflects an alteration in the normally balanced processes of extracellular matrix production and degradation. [6]The extracellular matrix, the normal scaffolding for hepatocytes, is composed of collagens (especially types I, III, and V), glycoproteins, and proteoglycans. |
|
|
|
What is the role of stellate cells in the pathogenesis of cirrhosis? |
Stellate cells, located in the perisinusoidal space, are essential for the production of extracellular matrix. Stellate cells, which were once known as Ito cells, lipocytes, or perisinusoidal cells, may become activated into collagen-forming cells by a variety of paracrine factors. Such factors may be released by hepatocytes, Kupffer cells, and sinusoidal endothelium following liver injury. |

|
|
|
What is the role of serum cytokines in the pathogenesis of cirrhosis? |
presence of distinct cytokine phenotypes was associated with cirrhosis severity. [7] Relative to the healthy patients, those with cirrhosis had elevated levels of proinflammatory cytokines (interleukin [IL]-6, -7, -8, -10, and -12, and tumor necrosis factor-alpha [TNF-α]) and chemoattractant elements. Leukocyte count was positively correlated with disease severity across the scoring systems used, levels of IL-6 and IL-8 had positive correlation with Model for End-Stage Liver Disease (MELD) score, and IL-6 alone had a positive correlation with chronic liver failure-sequential organ failure assessment (Clif-SOFA) score at day 7 (but a negative correlation with IL-2 at admission). [7] |
|
|
|
What is the role of collagen in the pathogenesis of cirrhosis? |
Increased collagen deposition in the space of Disse (the space between hepatocytes and sinusoids) and the diminution of the size of endothelial fenestrae lead to the capillarization of sinusoids. Activated stellate cells also have contractile properties. Capillarization and constriction of sinusoids by stellate cells contribute to the development of portal hypertension. |
|
|
|
What are the complications of cirrhosis? |
In addition to fibrosis, the complications of cirrhosis include, but are not limited to, portal hypertension, ascites, hepatorenal syndrome, and hepatic encephalopathy |
|

