![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
1760 Cards in this Set
- Front
- Back
|
What are the symptoms of influenza "the flu"? |
main symptoms |
|
|
What is Tamiflu? When can it be given? Write a prescription for a patient who is eligible for tamiflu?
|
An anti-viral that has very little evidence of benefit in treating influenza A + B. |
|
|
What is mononucleosis?
|
Mononucleosis (also called "kissing disease"), is a disease most commonly caused by the Epstein-Barr virus (EBV). EBV affects the lymphocytes which are white blood cells involved in the adaptive immune system. Mononucleosis can also be caused by cytomegalovirus (HCMV), a herpes virus most commonly found in body fluids. While CMV can cause mononucleosis, 85% of the cases are associated with EBV. The disease can be found in anyone but is most commonly contracted by adolescents and young adults ages 15–35. |
|
|
What are the symptoms/signs of infectious mononucleosis?
|
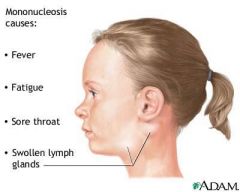
symptoms:
- fever - fatigue (extended periods of time) - pharyngitis signs: - LAD (tender especially posterior cervical LNs) - splenomegaly - palatal petechiae __________________________________________________ Rare complications include splenic rupture and airway obstruction. A generalized maculopapular, urticarial, or petechial rash is occasionally seen. Rash is more common following the administration of ampicillin or amoxicillin. NOTE: it may take 6 wks to 3 months to recover from mononucleosis |
|
|
For a patient with confirmed mononucleosis based on clinical impression and bw, what is the most important thing to warn patients?
|
Avoid all contact sports (possibility of spleen rupture if enlarged); however, even if not palpable on exam, recommend avoiding all contact sports.
In the f/u visit, if the patient says that they feel all better, it is important to recheck the spleen at this point to clear them. |
|
|
For suspected mononucleosis, what test would you order?
|
1. monospot (70-92% sensitive and 96-100% specific)
2. CBC (to look for atypical lymphocytes, inc. lymphocytes and leukocytes) 3. EBV titres (not needed, monospot is a relatively good test) Note: for monospot tests, a positive test is very likely to rule mononucleosis to be the case; whereas, a negative test cannot rule it out |
|
|
Image of palatal petechiae in mononucleosis
|

|
|
|
When prescribing antifungals, it is important to check what in B/W?
|
LFTs
|
|
|
laryngitis (hoarseness) + sore throat is almost always what? (bacterial or viral) ?
|
Viral
|
|
|
What is Hydrasense (saline mist) and what is it used for?
|
Used to relieve nasal congestion in babies and children, also adults. Different products available:
Easydose Vials: newborns and infants Ultra-Gentle mist: babies (<2 yrs) Gentle mist: adults and children 2 yrs and older Medium stream: adults and children 2 yrs and older Full stream: adults and children 12 yrs and older Congestion relief: adults and children 12 yrs and older note: it is advisable to use a nasal applicator Website: www.hydrasense.ca/en |
|
|
T/F. Decongestants are contraindicated in pregnancies?
|
True
In pregnancy, pseudoephedrine may cause vasoconstriction of the uterine arteries, which reduces fetal blood supply. This may cause the link between pseudoephedrine use in the first trimester and the development of gastroschisis. In this anomaly, a fissure develops in the fetus' abdomen, perhaps allowing protrusion of the intestines. Using decongestants while breast-feeding may cause irritability, insomnia, and tachycardia in the baby. Further, pseudoephedrine has been shown to reduce mean milk volume by 24%. |
|
|
When prescribing high dose steroids (eg. dexamethasone 12mg or prednisone 50mg), one must always caution patients about a rare but potentially dangerous S/E. What is this S/E?
|
Avascular necrosis (especially in younger patients); however, patients of any age should be warned of this possibility even though rare.
|
|
|
A patient comes in with stress incontinence. What are some management options for this patient?
|
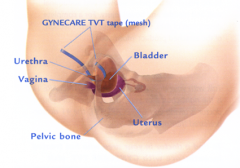
1. Physiotherapy (Kegel exercises - can refer to physiotherapist Carolyn)
2. Pessaries (not very effective) 3. Tension-free vaginal tape surgery (band placed around urethra) Carolyn Vandyken Physiotherapy Associates of Cambridge 163 Hespeler Road, Cambridge, ON N1R 3H7 phone no. 519-624-8798 |
|
|
You see a patient with stress incontinence. You've discussed treatment options: Kegels vs pessary vs TVT. The patient is interested in Kegel exercises. Who do you refer the patient to?
|
Write a script saying:
Physiotherapy at therapist's discretion Dx: stress incontinence And tell the patient to book at appointment with Carolyn Vandyken for Kegel training. 1. Physiotherapy Associates of Cambridge 163 Hespeler Road, Cambridge, ON N1R 3H7 phone no. 519-624-8798 |
|
|
What are Kegel Exercises?
|

A pelvic floor exercise, more commonly called a Kegel exercise, consists of repeatedly contracting and relaxing the muscles that form part of the pelvic floor (aka Kegel muscles). Exercises are usually done to reduce urinary incontinence after childbirth, and reduce premature ejaculatory occurrences in men, as well as to increase the size and intensity of erections.
The many actions performed by Kegel muscles include holding in urine and avoiding defecation. HOW TO FOR KEGEL EXERCISES: - When you've found the right way to contract the pelvic muscles, squeeze for 3 seconds and then relax for 3 seconds. - Repeat this exercise 10 to 15 times per session. Try to do this at least 3 times a day. Do this for 6 weeks. Kegel exercises are only effective when done regularly. The more you exercise, the more likely it is that the exercises will help. |
|
|
What is TVT surgery?
|
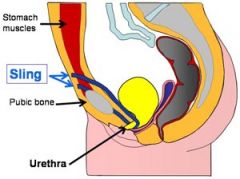
Tension-free trans vaginal tape
Stress urinary incontinence (SUI), also known as effort incontinence, is due essentially to insufficient strength of the pelvic floor muscles. Apart from Kegel exercises, TVT is a good option. The TVT sling procedure treats urinary stress incontinence by positioning a polypropylene mesh tape underneath the urethra. The 20-minute outpatient procedure involves two miniature incisions and has an 86-95% cure rate. Complications, such as bladder perforation, can occur in the retropubic space if the procedure is not done correctly. This minimally invasive procedure is a common treatment for stress urinary incontinence. |
|
|
For patients with PCOS, if they want to get pregnant, what medication would you prescribe them?
|
Metformin
NOT clomiphene citrate (as its benefit is very modest and risk of harmful s/e is much greater). NOTE: patients with PCOS continue to ovulate; however, rate of ovulation is less than patients w/o PCOS. |
|
|
What is the management of BPPV? (including prescription for medication)?
|
1. Epley maneuver (performed by M.D.)
2. Brandt-Daroff exercises (performed by patient 3. anti-emetics for N/V 4. SERC 24mg (have with meal as it may cause GI upset) Take 1 tablet po BID M: 7d |
|
|
What is onychomycosis? How do you make the diagnosis. What are some non-pharmacological options? What medication would you prescribe?
|

Fungal infection of the nail. It is the most common disease of the nails and constitutes about a half of all nail abnormalities. This condition may affect toenails or fingernails, but toenail infections are particularly common. The prevalence of onychomycosis is about 6-8% in the adult population.
The most common symptom of a fungal nail infection is the nail becoming thickened and discoloured: white, black, yellow or green. As the infection progresses the nail can become brittle, with pieces breaking off or coming away from the toe or finger completely. If left untreated, the skin can become inflamed and painful underneath and around the nail. To avoid misdiagnosis as nail psoriasis, lichen planus, contact dermatitis, trauma, nail bed tumor or yellow nail syndrome, laboratory confirmation may be necessary. The three main approaches are: potassium hydroxide smear, culture, and histology. This involves microscopic examination and culture of nail scrapings or clippings. Non-pharmacological options: keep feet dry, good hygiene, socks, avoid trauma, well-fitting footware Prescription Lamisil (terbinafine) 250mg po od x 6 weeks for fingernails (check LFTs at baseline) Lamisil (terbinafine) 250mg po od x 3 months for toenails (check LFTs at baseline and 6 wks) NOTE: important to do LFTs as terbinafine can be hard on the liver. NOTE: for using lamisil cream, no need to check LFTs b/c this medication is acting on a focal location and hardly any of it will make it to the blood. NOTE: the appearance may not have improved much but that does not mean that the treatment was ineffective. The nails will grow out and then look normal. |
|
|
A patient comes in and your diagnosis is bacterial vaginosis? Write prescription for medication. What precaution would you advise them?
|
Metronidazole (flagyl) 500mg BID x 7d
Avoid alcohol until 3d after Rx; metronidazole blocks the breakdown of alcohol leading to the accumulation of acetaldehyde --> facial flushing, headaches, palpitations and nausea |
|
|
What is post-infectious / post-viral cough?
|
A post-viral cough is a lingering cough that follows a viral respiratory tract infection, such as a common cold or flu, and lasting up to eight weeks.
One possible cause for post-viral cough is that the receptors that are responsible for stimulating the cough during the respiratory tract infection are up-regulated by respiratory tract infection and continue to stimulate after the virus has disappeared. |
|
|
A patient comes in to the office for a 2nd visit re: his insomnia. He has tried sleep hygiene techniques but these have not been effective. What would you do now?
|
Prescribe Trazodone 50mg
Take 1 tablet po qhs M: 30d (f/u in 1 months time; if stable prescribe 3 months + 1 repeat) or Melatonin (3mg, 6mg, 9mg, 12mg) Now after a few followups the patient continues to complain of insomnia + depression; can consider adding any of the following: - doxepin (10-50mg) qhs - seroquel 25mg qhs - amitriptyline (10-50mg) qhs - remeron (15-->30mg-->45mg) qhs (major s/e is wt gain) - zopiclone 5mg qhs prn M:14d (avoid more than this; if needed longer term, then avg. 3 tabs per week prn) |
|
|
Discuss the management to insomnia (non-pharmacological and pharmacological)
|

|
|
|
What 2 functions does Remeron (mirtazapine) treat? Write a prescription for remeron for the 2 functions remeron serves.
|
depression + insomnia
remeron 15mg qhs (note: can go up to 30mg qhs, then 45mg qhs (max dose)) (dose must be tapered gradually when discontinuing) note: however, a major S/E of Remeron is weight gain. Weight gain may be a desired effect if the pt has anorexia or weight loss |
|
|
A diabetic patient visits you in the clinic for his diabetic f/u. How often would you f/u with this patient after this visit?
|
3 months if uncontrolled diabetes ('diabetes long' requisition should be given and done 1-2 wks before next visit)
4 month if almost stable but not quite ('diabetes long' requisition should be given and done 1-2 wks before next visit) 6 months if controlled diabetes ('diabetes long' requisition should be given and done 1-2 wks before next visit) NOTE: Diabetes long requisition includes FBS, HbA1C, urine, AC ratio |
|
|
A diabetic patient who checks his glucose at home uses a glucometer. He loses it and wants a new one? He also requests for test strips. What would you write?
|
Just write " glucometer x 1" on the prescription (handwritten) or put in PSS system (however, it will crowd the medication history)
TEST STRIPS: Ascensia contour strips 100 strips + 10 repeats |
|
|
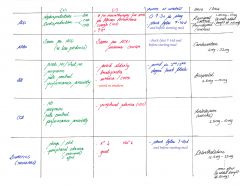
Describe 4 effective hypoglycemic medications (for diabetes mellitus)?
|

|
|
|
Discuss the mechanism of actions of the following oral hypoglycemic agents used for diabetes:
- metformin - diamicron - januvia - victoza |

|
|
|
A 67F pt comes to your office. You called her in b/c her HbA1C came back 9.1. You discuss with her lifestyle changes, but then also decide to put her on a oral hypoglycemic agent. Write the plan (incl. prescription)
|
PLAN
1. Metformin 500mg tablet Take 1 tablet po od x 1wk, then take 1 tablet BID M: 3 months 2. BW_diabetes (long) in ~ 3 months 3. f/u in 3 months time after bw NOTE: this is diabetes_inadequately controlled and therefore, a 3 mo f/u is arranged. |
|
|
A diabetic patient comes in for a diabetes f/u at 6 months. His diabetes is under control; however, his LDL is 3.0, and it is trending upwards despite adequate lifestyle management. What would you do?
|
Calculate his Framingham risk score for CAD.
If severe risk, prescribe: Crestor Take 10mg po od M: 6 wks (initially) F/U in 6 wks with repeat LFTs, then if things are stable, prescribe: Crestor Take 10 mg po od M: 3 months f/u in 3 months with LFTs, then if things stable prescribe q6 months (3 months + 1 repeat) to q12 months (depending on patient) (NOTE: if moderate risk (10-19% 10 yr risk), then you want LDL <3.5 |
|
|
A 85F pt comes in with polydipsia. What is your ddx?
|
- diabetes mellitus
- psychogenic polydipsia - diabetes insipidus (central vs. peripheral) |
|
|
What is diabetes insipidus?
|

|
|
|
What is the dosage given for Actonel (risedronate)?
|
1. osteoporosis, postmenopausal: 35mg po qwk or 150mg po qmo
2. osteoporosis, steroid-induced: 5mg po od for tx and prevention in pts on >7.5mg/d prednisone or equiv 3. osteoporosis, male: 35mg po qwk (take with water >30mins before first meal, remain upright x 30 mins; Ca and Vit D supplementation recommended if inadequate intake |
|
|
A 55 male on prednisone treatment complains of not tolerating Actonel well and refuses to take it. What is the next medication you would prescribe this patient?
|
Fosamax 70mg: Take 1 tablet po qweekly M: 3 mo + 1 repeat
Same prescription for postmenopausal women if they're not tolerating Actonel well. |
|
|
What are the different drug options for management of erectile dysfunction?
|
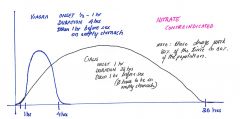
1. Cialis 5-20mg/dose
2. Viagra 25-100mg/dose Must warn patients of 4 S/Es: - flushing - H/As - nasal congestion / rhinitis - dyspepsia CONTRAINDICATION: Nitro eg. nitroglycerin NOTE: When counseling patients, it is important to mention that these drugs work in 80% of the population 80% of the time. |
|
|
Why would you choose to prescribe Viagra over Cialis in a patient with erectile dysfunction?
|
Rare circumstance:
A patient who has a hx of using 'nitro' meds should not be taking PDE5-inhibitors such as cialis, viagra, or levitra. B/c the effects of cialis last much longer than viagra, it is risky in a patient who may end up taking nitro. This may cause severe hypotension. Viagra would be a better choice in this circumstance. |
|
|
Write a prescription for cialis, viagra?
|
Cialis 10mg: Take 1 tablet po prior to sexual activity prn M: 10 or 15 tablets + 1 repeat
Viagra 50mg: Take 1 tablet po 1 hr prior to sexual actvity prn M: 10 or 15 tablets + 1 repeat (if pt >65 start at 25mg tablet od) note: Viagra should be taken on an empty stomach; this does not apply to cialis. |
|
|
A patient comes in with a sore throat. You calculate the GAS score. Explain what you would do for the various GAS scores:
0-1: 2-3: 4+: |
0-1: Do not culture; do not treat
2-3: culture: Rx only if positive culture 4+: Rx, don't bother doing culture For scores < or = to 3, recommend gargling with lukewarm salt water, tylenol/advil, and/or offer tantum tantum 0.15% liquid gargle and spit 15mL q2h prn M: 250mL |
|
|
A asymptomatic patient comes in requesting STI testing? What would your discussion be re: this and what would you do for this patient.
|

- GC + NG are ~ 70% of all STIs
- counsel patient that HIV test must be repeated after 3 months (if there is suspicion of recent exposure) |
|
|
A 52M patient comes in with an anal fissure. He also complains of scant bleeding on toilet paper and pain with BM. Also complains of constipation x 1 month.
What would be your management? |
1. check FOBT vs colonscopy dates
2. increase fibre intake; benefibre (otc) vs. metamucil (otc); consider stool softener 3. tylenol prn 4. sitz baths 5. Nitroglycerin Prescription (in pss): Medication: nitroglycerin Instructions: 0.2% ointment; apply perianally BID M: 15g repeat: 1 |
|
|
Explain the link between prednisone use and BMD?
|
BMD testing should be done for any patient who has been on prednisone 7.5mg x 3 mo or equivalent.
Treatment with Actonel (bisphosphonate) should be strongly considered in a patients taking prednisone 7.5mg x 2 years. |
|
|
What is actinic keratosis? What are some treatment options?
|
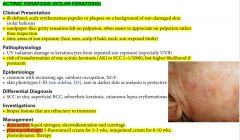
|
|
|
What is seborrheic keratosis? What are some treatment options?
|

|
|
|
A patient comes in for bloodwork f/u. His cholesterol is 6.54. What would you do?
|
Counsel: diet, exercise, weight loss (if obese)
(note: you can expect conservative management to reduce cholesterol / LDL by about 20%, consideration for a statin (crestor) should be taken into account. So if this patients cholesterol is reduction from his prev. cholesterol level, then you can wait and see what his next cholesterol level is. If its the same or higher, consider crestor; otherwise, conservative management. Now if this patient had other RFs such as heart disease, HTN, diabetes, smoking, it is best to be more aggressive in bringing his cholesterol levels lower. NOTE: use the framingham cardiovascular risk calculator to calculate is 10yr risk of CAD. If high risk, err towards treating with statin. Moderate risk ... can be watched. |
|
|
Which foods should you counsel a patient to avoid/reduce in order to prevent/decrease GERD?
|
alcohol
tobacco caffeine fatty foods spicy foods citrus fruits peppermint chocolate |
|
|
Which PPIs are covered only by ODB? Write prescriptions for 2 of the PPIs that I'll use in practice most commonly. Write a prescription for an h2-antagonist used to treat gerd. What are some non-medical management strategies for gerd?
[gerd, reflux] |
i. pariet ec
ii. nexium (esomeprazole) backup option is: tecta 40mg od Prescriptions: ------------------------------------------------------------ PPIs: 1. pariet ec 20mg tablet 1 tablet daily M: 30 days (for hypersecretory conditions max of 120mg od) 2. nexium 20mg tablet 1 tablet daily M: 30 days (for hypersecretory conditions, max of 120mg bid) ------------------------------------------------------------- h2 antagonist: 1. ranitidine 150mg 1 tablet bid ------------------------------------------------------------- non-medical strategies for gerd: - weight loss - elevating head of bed - avoid trigger foods: alc, tabacco, caffeine, chocolate, peppermint, spicy foods, fatty foods, citrus fruits |
|
|
A patient comes in with first time GERD with no red flags. Write a prescription for this patient.
|
Avoid all triggering foods
Prescription: 1. pariet ec take 20mg tablet po od M: 30 days |
|
|
If a patient is having GERD like symtpoms, would you ever prescribe a PPI for 2 weeks?
|
No, it should be prescribed for 1 month with instructions to the patient to f/u if symptoms recur. If they recur, she may need to be started on a PPI for a longer duration, eg. 3 months + 1 repeat.
F/U prescription durations: 1 month --> 3 months --> 6 months (lifelong 3mo + 1 rpt) Advise the patient on diet management (avoidance of caffiene, spicy foods, fatty foods, citrus juices etc) May want to consider sending the patient for an endoscopy if any red flags are present; if symptoms controlled on medication, don't bother scoping them |
|
|
What are the red flags for dyspepsia / GERD (reflux)?
|

|
|
|
Patient comes in to your office with 2 months of hoarseness. What is your approach to this complaint?
|
1. GERD
2. Refer for laryngoscopy to r/o - malignancy - polyps - papules on vocal cords NOTE: this patient should be scoped by default; unless, you are certain he has GERD On history, ask about 1. RFs: alcohol, smoking, radiation 2. constitutional symptoms 3. reflux symptoms (heart burn, dyspepsia, cough, sob) 4. ROS: dysphagia, odynophagia 5. excess voice use |
|
|
A pregnant woman comes in for a prenatal checkup. Everything is fine; however, her urine comes back with 2+ leukocytes and 1+ protein (she does not have symptoms of a urinary tract infection). What would you do?
|
Check her bp and make sure its not elevated (protein was 1+ although this is quite common)
The 2+ leuks indicate a potential UTI. UTI in asymptomatic pregnant patients must be treated. Therefore, do a urine culture and send it to the lab. If positive treat for UTI. A f/u culture in 3-4 wks is recommended after treatment initiation. NOTE: nitrofurantoin / macrobid is CONTRAINDICATED between 36-42 wks GA, and during labour due to the possibility of hemolytic anemia. NOTE: septra is contraindicated in the 1st trimester b/c it may limit availability of folic acid to the fetus as well as the last 6 wks of pregnancy as it may cause kernicterus For the contraindications, consider amoxicillin 500mg tid x 7d or keflex 500mg qid x 7d |
|
|
Roughly how much weight gain is expected during pregnancy?
|
~20-30 lbs close to delivery
mothers often gain ~ 1 lbs every month in the 1st and 2nd trimester and ~ 1 lbs qweekly from week 30-40 (approximately) |
|
|
note
|
Bacterial conjunctivitis is more common in children (~50-75% than viral)
Viral conjunctivitis is more common in adults |
|
|
A 34 yr old female comes in with bacterial conjunctivitis. What would be your treatment options?
|
1. erythromycin ointment 0.5% opthalmic
2. fucithalmic 1% drops (note this is actually a viscous paste; not drops) 3. garamycin 0.3% drops 4. moxifloxacin 0.5% drops 1. erythromycin oph ointment 0.5%: Apply to affected eyes QID (duration 5-7d) M: 1 bottle 2. fucithalmic 1% drops: apply 1 drop BID to affected eye(s) (duration 5-7d) M: 1 bottle 3. garamycin 0.3% drops: apply 2 drops TID in affected eyes(s) (duration 5-7d) M: 1 bottle 4. [for contact lens wearers, corneal involvment, Rx failure] moxifloxacin 0.5% drops: apply 1 drop TID in affected eye(s) (duration 5-7d) M: 1 bottle NOTE: also use warm compresses to clean the affected eye(s) and maintain good hand hygiene NOTE: if you're on the edge between viral and bacterial conjunctivitis, then you can opt for polysporin drops (OTC). NOTE: difference btwn fucithalmic vs garamysin eyedrops is that garamysin covers pseudomonas (contact lens wearers); in addition moxifloxacin drops have pseudomonas coverage. |
|
|
A 1 month old baby comes in to your office with yellowish crusts on the eyelashes. Mother complains that his eye are very sticky in the morning. There is no conjunctivitis. What is your likely diagnosis? What would be the management.
|
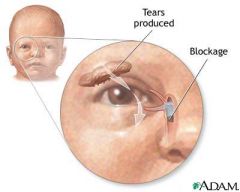
Blocked nasolacrimal (tear) duct (self-limiting condition); 90% resolve within first 6 months
Management: - reassurance (this is quite common) - clean with wet warm clean cloth - massage tear duct area 8 - if no improvement by the time the child is 1 yr, can refer the patient to a pediatrician for probing |
|
|
A patient comes in with bacterial conjunctivitis. What are the main pertinent negatives to r/o?
|
- vision changes / acuity / fields
- eye pain - photophobia - eye trauma - contact lens |
|
|
What are drugs that can help with premature ejaculation?
|
1. SSRIs (1st line)
more specifically Zoloft (sertraline) Prescription: Zoloft 50mg tablet Take 1 tablet po od (regularly) x 3 weeks; then 3-4 hrs prn prior to sexual activity M: 30 tablets 2. Clomipramine (2nd line) |
|
|
What is the management of urge incontinence?
|
1. behaviour modification
2. Kegel exercises 3. Vesicare Prescription (vesicare) Vesicare Take 5mg po od NOTE: starting dose is 5mg od; max dose is 10mg od Note: oxybutynin was used for urge incontinence; however, vesicare has fewer S/Es and is much less likely to cause "dizziness" / falls. Both oxybutynin and vesicare are anti-cholinergic agents. |
|
|
What are the 2 most common causes of throat irritation or "globulus sensation" at the back of the throat?
|
1. postnasal drip
2. reflux |
|
|
Write a prescription for a medication for postnasal drip.
|
Nasonex 50mcg nasal spray
Take 2 sprays in each nostril od M: 1 device Note: for nasal sinus congestion, the prescription for nasonex would be Take 2 sprays in each nostril bid (never prn, because steroids take a while to start working) |
|
|
A patient comes in with an infected and erythematous looking toe. What would you prescribe this patient?
What would you prescribe is this patient had a suspected anaphylactic reaction to penicillins? |
Keflex 500mg
Take 1 tablet po qid M: 7d NOTE: Keflex has a <5% chance of cross-reactivity with penicillin. Given that the patient has a questionable anaphylactic reaction to penicillin, it would be appropriate to prescribe: Biaxin 500 mg tablet Take 1 tablet po bid M: 7d If this patient just had a mild allergic reaction to penicillin, then keflex would be a reasonable choice. |
|
|
How do you know that a patient is undergoing an anaphylactic reaction? What is the emergent management in this patient?
[anaphylaxis] |

|
|
|
A patient has an anaphylactic reaction. You secure the airway if required and establish an IV line. What 3 drugs are important to administer in this situation?
|
1. epinephrine
2. benedryl (anti-histamine) 50mg IM/IV q4-6h 3. methylprednisone 50-100mg IV 4. (ventolin - nebulized if bronchospasm) 5. (glucagon (for those on β-blockers w/ resistant hypotension and/or cardiac disease) |
|
|
After a patient is discharged from the ER post-anaphylactic reaction, which 3 drugs should he/she be on?
|
1. cetirizine 10mg po OD x 3d (H1 antagonist)
2. ranitidine 150mg po OD x 3d (H2 antagonist) 3. prednisone 50mg po OD x 3d (corticosteroid) |
|
|
What is a good tool to monitor a patient's level of pain? (note: file should be in JP Pain folder)
|

A measure of the patient's pain. This is good to see trends in pain management. Just add up the total for #9 and write as, eg: function BPI or fBPI: 49
|
|
|
How soon should you f/u with a patient after a hormonal contraceptive is prescribed?
|
6 weeks
|
|
|
note
|
For the periodic_bw avoid checking ck and lfts, unless there are indications for checking these.
Baseline ck and lfts can be done prior to starting a pt on a statin; however, followup ck and lfts are no longer required. |
|
|
List some atypical antipsychotics.
|
MOST COMMON (ROCS and in order of most potent to less potent)
- Risperidone - Olanzapine (zyprexa, zydis) - Clozapine (Clozaril) - Quetiapine (seroquel) LESS COMMON - Ziprasidone (Zeldox) - Aripiprazole (Abilify) NOTE: ALL OTHERS ARE TYPICALS including Haloperidol (Haldol), Pimozide (Orap), Chlorpromazine |
|
|
note
|
When starting someone on a new medication such as Lithium, Epival, BP meds, it is important to do bloodwork (generally AHE_BW) to see if the levels (including electrolytes) are okay.
|
|
|
A 22M patient comes to your office with manic symptoms typical for a manic episode. What do you do at this point?
|
? prescribe mood stabilizers
? refer to psychiatrist |
|
|
T/F. Screening for family hx of bipolar disorder in a patient with bipolar disorder is extremely important.
|
True.
Screening for a family history of bipolar disorder is critical. A positive family history among first degree relatives increases the likelihood of bipolar II disorder by 8–18 times compared to those with no family history. |
|
|
T/F. Benzodiazepines or SSRIs alone should not be used in Bipolar patients.
|
True
|
|
|
Discuss the medical management options for Bipolar Disorder.
|
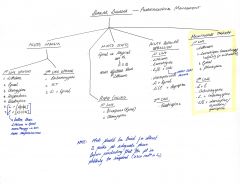
|
|
|
T/F. Lithium and lamotrigine have established antidepressant efficiency.
|
True
|
|
|
T/F. Lithium is teratogenic.
|
True
Therefore must rule out pregnancy before initiating lithium therapy |
|
|
What is lithium toxicity?
|
NOTE: lithium toxicity can present even at therapeutic levels. Common causes include:
- overdose - Na or fluid loss - concurrent medical conditions CLINICAL PRESENTATION: - GI: severe N/V + diarrhea - Cerebellar: ataxia, incoodination, slurred speech - Cerebral: drowsiness, myoclonus, seizures, delirium, coma, parkinsonian movements MANAGEMENT: - discontinue Li for several doses, begin again at a lower dose - serum Li, Cr, BUN, lytes - saline infusion - hemodialysis if Li > 2mmol/L, coma, shock, severe dehydration, failure to respond to treatment after 24 hrs, or deterioration |
|
|
What are the S/Es of Lithium treatment. What are 2 conditions Lithium can cause in the long term?
|
SIDE EFFECTS of LITHIUM:
GI: N/V, diarrhea, stomach pain, weight gain GU: polyuria, polydipsia, GN, renal failure, nephrogenic DI CNS: fine tremor, lethargy, fatigue, H/A HEMATOLOGICAL: reversible leukocytosis OTHER: teratogenic (Ebstein's anomaly), edema, psoriasis, hypothyroidism, hair thinning, acne, muscle weakness, ECG changes LONG TERM may cause: - nephropathy - diabetes insipidus |
|
|
What investigations must one do before initiating lithium therapy?
|
INVESTIGATIONS:
- ahe_periodic, lytes, tsh, β-hcg - urinalysis - ECG (if patient >45 yrs old or CV risk) Before initiating Lithium therapy: must screen for: 1. pregnancy 2. thyroid disease 3. seizure disorder 4. neurological, renal, CV disease |
|
|
A patient comes in with leg pain bilaterally. His work involves standing for 7 hrs in a row. He is requesting orthotics, back support, and compression stockings. Write the prescriptions.
|
1. bilateral custom orthotics M: 1 pair; Dx: mechanical feet pain
2. custom back support x 1; Dx: back strain 3. graded compression stockings. Below knee. Pressure 20-30mmHg M: 1 pair NOTE: its best to write these prescriptions separately so that the patient can submit these for insurance purposes. |
|
|
A mother is requesting a device that would ease the use of the puffer (such as ventolin) for her 2 yr old daughter. Write a prescription for this.
|
pediatric aerochamber M: 1 unit
|
|
|
T/F. NSAIDs and COX-II inhibitors should be avoided in patient with heart failure as this can exacerbate the heart failure.
|
True
|
|
|
note
|
B-blockers, ACEi, ARBs, and aldosterone antagonists increase serum potassium levels
furosemide (lasix) and thiazides decrease serum potassium levels |
|
|
What are 3 places to recommend for counseling provided they have coverage?
|
1. Qualia Counseling Services
16 Andrew St Kitchener, ON N2H 5R2 (519) 742-0500 2. KW Counselling Services 480 Charles St. East, Kitchener, ON N2G 4K5 P: 519-884-0000 3. Mosaic Counselling and Family Services 400 Queen Street South Kitchener, ON N2G 1W7 519-743-6333 |
|
|
NOTE:
|
Nortriptyline is better tolerated than Amytriptyline
|
|
|
What is the long term management of CHF?
|

|
|
|
What are the five most common causes of CHF?
What are the most common precipitants of heart failure? |
causes:
1. cad (60-70%) 2. htn 3. idiopathic (often dilated cardiomyopathy) 4. valvular (eg. AS, AR, and MR) 5. alcohol (dilated cardiomyopathy) precipitants: 1. HTN 2. Arrhythmia 3. Infection/Ischemia/Infarction 4. Dietary indiscretions 5. Failure to take meds |
|
|
What is the most common cause of r. heart failure?
|
l. heart failure
|
|
|
A 78 year old female comes in feeling very short of breath, some ankle swelling, her JVP is elevated. You treat her symptomatically (LMNOP) and optimize her mortality beneficial drugs (ACEi, B-blocker) etc. What investigations would you do ?
|
i. bw_ahe, tsh, ferritin
ii. ecg iii. echo iv. cxr |
|
|
T/F. Weight gain is common in patients on insulin Rx.
What is one important thing for patients (who are on insulin) to keep in mind re: their diet |
True.
Do not skip meals. They should be regular. Otherwise, they can run into hypoglycemic spells |
|
|
What is Altace (ramipril). What are the indications and dosing for this medication?
|
An Ace-inhibitor
INDICATIONS: ------------------------- HTN 2.5-20mg/d po (divided od-bid) start at 2.5mg po od CHF, post-MI 5mg po bid Start at 2.5mg po bid Cardiovascular event protection 10mg po od start 2.5mg po x 1 wk, then 5.0mg po x 3 wk, then 10.0mg po od NOTE: Ace-i are renally excreted |
|
|
You diagnose a patient with hypertension in your office (this is the third visit, BP 160/105 today. Discuss your plan. (you've done the SOA of the SOAP note)
|
PLAN:
1. Ramipril 5mg po od x 2 wks; then 10mg po od x 3 months (if pt has diabetes, kidney disease); otherwise chlorthalidone 12.5mg po od x 3 mo 2. BW - Cr, lytes in 2 weeks time (imp. b/c you want to see if anything has changed after starting them on an ACEi 3. f/u in 1 months time for repeat BP |
|
|
A patient was diagnosed recently with HTN. What should the f/u schedule for HTN be ?
|
Initially, inc. freq of visits
f/u 2-3 wks; if this is stable, then f/u in 3 months, if this is stable f/u in 6 months (therefore when giving prescription, give 3 months + 1 repeat) Now for elderly frail patients, may need to f/u in 3 months (do take into consideration that it may be hard for them to get to your office in which case f/u in 6 months. For someone, who is young (42) reliable, checks BP at home, watches their diet, may even f/u in 1 year |
|
|
A patient comes in to your office with onychomycosis (confirmed by lab review of nail clippings), you prescribe lamisil (terbinafine). However, the BP check that the nurse takes shows that his BP is 160/105. What do you do about this?
keyword: hypertension (HTN) |

|
|
|
T/F. A patient of African descent who has HTN should not be treated with ACEi as monotherapy.
|
True
|
|
|
What are the 4 classes of anti-hypertensives. Discuss how they can be combined (NOTE: this is for solely HTN)
|
Ace-inhibitors
B-blockers CCBs Diuretics A with C / D B with C/ D C with A / B D with A / B Therefore, A is not combined with B, C is not combined with D. NOTE: however, in patients with CHF (with or without HTN), ACEi are combined with B-blockers (mortality benefit) |
|
|
Distinguish between the 4 different classes of anti-hypertensives?
[htn] |
|
|
|
With respect to HTN, when should one consider referring the patient to a specialist?
|
- refractory HTN
- suspected secondary cause - worsening renal failure NOTE: hospitalization is required for malignant HTN i.e. BP often >200/140, papilledema, retinal hemorrhages, bulging discs, mental status changes, inc. creatinine |
|
|
note:
|
For elderly patients (>60yrs) with isolated diastolic/systolic HTN, B-blocker monotherapy or combination of ACEi with an ARB are both not recommended.
|
|
|
A mother comes in to your office with her 6 yr old girl. She wants her daughter to have a flu shot. What will you tell her?
|
If she has never had the flu shot before, then she needs to get a booster flu shot 1 month following the first flu shot. Subsequently after this, they do not require boosters.
note: boosters only apply for 1st time flu shot recipients ages 6 months to 9 years. |
|
|
What is the management of hyperlipidemia?
|
|
|
|
What is the Rx for otitis externa in adults and children?
|
Ciprodex
4 drops in affected ear BID x 7d M: 1 bottle Other option is: garasone otic solution 3 drops in affected ear TID x 7d M: 1 bottle NOTE: for a pt getting recurrent episodes of otitis externa may use diluted vinegar (1/2 vinegar) 1-2 drops in each ear (this is shown to prevent infections) if tm is intact and not perforated. |
|
|
A 38M patient comes to your office complaining of 2 weeks of severe neck pain. He says his neck went into a spasm when he rotated his head to the right. What would be your management?
|
1. Naproxen (if minimal relief with advil)
2. physiotherapy/massage therapy 3. icing/heat therapy 4. flexiril (cyclobenzapril) at qhs (sedating, can make pt drowsy) Prescription for flexiril: Flexiril 10mg tablet Take 1 tablet po qhs M: 14 tablets *note: max dose: flexiril 30mg / day Flexeril (cyclobenzaprine), is a muscle relaxant medication used to relieve skeletal muscle spasms and associated pain in acute musculoskeletal conditions. |
|
|
Write a pulmicort prescription for asthma control in a patient.
|
Pulmicort 200
Inhale 2 puffs BID M: 1 inhaler |
|
|
A patient is having occasional paresthesias in the arm noted for 6 months. As part of your workup you check B12 levels, which come back "low". Write a prescription for oral med B12.
|
oral B12
Prescription: none required - this is OTC Vitamin B12 1000mcg tablet (OTC) Take 1 tablet po od NOTE: you need a prescription for vitamin b12 injections Prescription: Vitamin B12 1000 mcg/mL Amp Administer 1cc IM qmonthly M: 1 + 1 repeat NOTE: foods rich in b12 include meats, eggs, dairy products |
|
|
What is considered to be b12 deficiency? What are the symptoms of b12 deficiency?
|
b12 levels <300 (as per bloodwork in pss)
Symptoms: - weakness - numbness - paresthesias - lack of dexterity - impaired memory - irritability |
|
|
Patient complains of dysuria x2d and says that this is very similar to her previous urinary tract infections. History points towards a urinary tract infection; however, urine dip comes back negative. What do you do?
|
This may be interstitial cystitis; but we can't make this diagnosis yet..
Patients can get dysuria with irritation from caffeine. (NOTE this patient drinks ++ coffee) MANAGEMENT: - lots of fluids - cranberry juice - advil - send urine for cultures; will treat if positive - abstain from caffeine x 1 mo to see if there is resolution of Sx - if recurrent dysuria; then need to completely abstain from coffee (not a drop of coffee) [note: other triggers may include alcohol, artificial sweeteners, and hot pepper] ** INTERSTITIAL CYSTITIS is a diagnosis that should be made by a urologist, so if abstinence from caffiene, or other triggers does not provide relief a referral should be sent. Rx for interstitial cystitis includes: elmiron (pentosan polysulfate), low dose amitriptyline (see TO notes for other management options) |
|
|
Patient is going to cuba for vacation. Asks you if he should get any immunizations?
|
Twinrix (hep A and B)
normal course: 0, 1, 6 months (3 shots) rapid course: 0, 7d, 21d, 12 months (in case patient is leaving in 2 weeks) Prescription: Twinrix: to be injected in office M: 1 vial + 2(3) repeats |
|
|
What is the management of chronic stable angina?
|

|
|
|
You diagnose a patient with stable angina. You put him on aspirin 81mg od and a B-blocker (bisoprolol 5mg od). The patient tells you that their angina comes about when they're mowing the lawn. You decide provide them with symptomatic control, ie. nitrates. What are the main S/Es of nitrates to warn the patient?
|
- hypotension (lightheadedness)
- H/A - facial flushing |
|
|
A patient with newly diagnosed atrial fibrillation is put on bisoprolol 2.5mg for rate control. She comes back 2 weeks later c/o feeling unwell on bisoprolol. O/E her pulse is 49. What would you do?
|
Discontinue bisoprolol, and start the patient on Cardiazem cd (diltiazem) 120mg po od as directed
|
|
|
Discuss the investigations and management for atrial fibrillation?
|

|
|
|
What investigations would you do in a patient complaining of angina?
|
Note if unstable angina, send them to the ER.
For stable angina: 1. bw: Hb, fasting glucose and lipids, tsh (in practice: ahe + tsh + ferritin) 2. ekg + 48hr holter, cxr, echo 3. stress test (if really old and you think they can't run on the treadmill, opt for nuclear stress test) 4. +/- angiography |
|
|
Discuss the CCS Functional Classification of Angina?
|
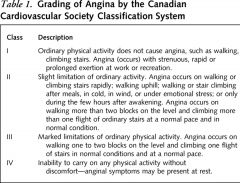
|
|
|
What is the acute vs chronic management of unstable angina/NSTEMI ?
|
acute management:
(BEMOAN) B-blocker Enoxaparin Morphine Oxygen ASA Nitrates ------------------------------------------------ chronic management: i. asa 81mg od ii. ace-i iii. statin iv. β-blocker NOTE: - for ace-i: coversyl (start 4mg od, double in 2wks to 8mg od (target dose), if able to tolerate; w/ elderly pts start at 2mg od x 1wk, then 4mg od x 1wk, then target dose of 8mg od) - for statin: crestor 10mg od; may go upto 40mg od if lipids not at target - for β-blocker: bisoprolol 5mg od (starting and target dose) |
|
|
What is the long-term management of acute coronary syndrome?
|

|
|
|
What is dyshidrotic eczema?
What is the management? |

Dyshidrotic eczema is characterized by:
- tense, deep seated vesicles or bullae localized on the palms and soles and often on the lateral aspect of fingers - acute onset w/ hx of recurrence and remissions (freq episodes for months/yrs) MANAGEMENT: i. moisturizer i i. steroid cream (high potency such as topicort 0.25% cream bid) |
|
|
A 14F comes in to your office complaining of sob after intense running at the gym; her friends seem to be okay, but she has difficulty catching her breath. She has noticed these symptoms for the past 3 wks. Prior to this she was mainly active 6 months ago playing baseball. Last week after a run in the gym, she started coughing ++, while catching her breath. What are the most probable causes of her symptoms? How would you manage this patient?
|
MOST LIKELY
1. deconditioning 2. exercise induced asthma LESS LIKELY 3. anemia (inquired with the patient, periods normal, no blood in stool) 4. CVS problem (no chest pain, no palpitations, color normal) 5. Respiratory problem (not smoking, no drugs, no blood with cough, no fever) MANAGEMENT (provided physical exam unremarkable) - reassurance: gradual inc. in intensity to build stamina - trial of ventolin: 2 puffs before exercise - if improvement with ventolin, (dx: exercise induced asthma, otherwise deconditioning is the likely dx and it is then important r/o anemia, CVS problem vs resp problem - rtc for further investigations) - B/W: cbc, ferritin (to do if no improvement with puffer) - rtc if symptoms ongoing or worsen |
|
|
Should nsaids be avoided in pregnancy? Why?
|
They should avoid nsaids (especially in the 3rd trimester); advise patient to avoid it all together to avoid confusion.
Can cause premature closure of the ductus arteriosus in the fetus note: the ductus arteriosis should close shortly after birth. In the fetal stages it allows oxygenated blood to bipass the lungs as blood moves from the r. ventricle straight to the aorta. If the ductus arteriosis closes prematurely, blood cannot go from the pulmonary artery to the aorta and instead forces its way into the lungs and puts reverse pressure on the r. side of the heart. This leads to: - r. heart hypertrophy and subsequently failure - lung damage |
|
|
A 88M patient comes in to your office complaining of R. aural fullness. On further inquiry, he mentions that he has noticed about a 90% reduction in sound from baseline from his R. ear. What is the management?
|
Call ENT on call
DDx: - viral neuritis - CVA (affecting nerve) NOTE: This patient will probably get a steroid injection in the middle ear. An audiogram must be done before the patient is sent in to the ENT specialists office. |
|
|
A 33F comes in to your office to confirm her pregnancy (home preg test positive). The urine in the office comes back positive for bHCG. What are the main things to talk to the patient about during this visit?
|

|
|
|
What are the features of allergic conjunctivitis?
What is the management for allergic conjunctivitis? |
Allergic conjunctivitis features:
* eyelid + conjunctival: erythema + swelling * almost always bilaterally * pruritis * tearing / watery discharge * burning * photophobia * other allergic sx NOTE: - allergic conditions are often accompanied by significant itch, whereas this is not very common in infection MANAGEMENT: General: - do not rub eyes - avoid contact with known allergen - Refresh eye drops for concomitant dry eyes Prescription (for patients with frequent episodes) Pataday 0.2% Apply 1 gtt in affected eye od M: 1 bottle OTC option if infrequent episodes: Visine-A |
|
|
A patient comes in with [bilateral eye irritation (R>L) with intermittent, red eye, tearing, itching] x 3 months. Eye drops have not made a difference to him. What is your DDx ? and what is the most likely cause?
|
Most likely allergic conjunctivitis,
- could also be dry eyes (unlikely b/c patient had been using eyedrops). Treatment: - Pataday eye drops (for allergic conjunctivitis) - Refresh tear drops for dry eyes If it is an allergic conjunctivitis, patients symptoms are likely to resolve within 2-3 days. Otherwise, regular use of Refresh tear drops will resolve his dry eyes within a month note: it is unlikely that this patient has a corneal abrasion, because both eyes are affected, he would be in ++ pain, symptoms would likely not last 3 months Other DDx: - viral/bacterial conjunctivities: unlikely b/c symptoms don't last 3 months |
|
|
Write a contingency prescription for a patient going to Latin America who is concerned about traveller's diarrhea.
|
Prescription:
Ciprofloxacin 500mg tablet Take 1 tablet po BID x 3 days. To take only with development of diarrhea (4 or more unformed stools/d, fever, blood/pus in stool M: 6 tablets For any patient travelling to Asia, latin america, Africa (except S. Africa) you should recommend the following: - safety precautions and medical insurance - travel's diarrhea - prevention: dukoral - Rx: ciprofloxacin - typhoid - hep A/B (twinrix) |
|
|
Explain how Dukoral is to be taken.
|
Dukoral (non-prescription) is available at most pharmacies; used for prevention of Traveller's diarrhea
A full immunization requires 2 doses taken 1 week apart, with the last dose taken at least 1 week before travel. Effective once taken last dose for 3 months |
|
|
Explain how typhoid vaccine is given.
|
Dosing: Adult Immunization:
Oral: (Vivotik) Primary immunization: One capsule on alternate days (day 1, 3, 5, and 7) for a total of 4 doses; all doses should be complete at least 1 week prior to potential exposure Booster immunization (with repeated or continued exposure to typhoid fever): Repeat full course of primary immunization every 7 years -------------------------------------------------------- I.M. (Typherix) Initial: 0.5 mL given at least 2 weeks prior to expected exposure Reimmunization: Typherix® 0.5 mL every 3 years |
|
|
What is the criteria for a migraine?
|
≥ 5 attacks meeting each of the following criteria
* 4-72h duration * 2 of the following: unilateral, pulsating, moderate-severe, aggravated by routine physical activity * 1 of the following: N/V, photophobia/phonophobia/osmophobia NOTE: important to ask about aura with migraines |
|
|
What are the treatment options for migraines?
|
1st Line: Tylenol
2nd Line: Advil 3rd Line: Axert (almotriptan) Prophylaxis: 1st Line: B-blockers (propanolol) 2nd Line: TCA (amitriptyline, nortriptyline) |
|
|
A patient comes in with migraines. She has tried tylenol and advil with no relief of Sx. What would you do now (write a prescription)
|
Axert (almotriptan) 12.5mg tablet
Take 1 tablet po od prn, may repeat x 1 after 2 hrs prn (max: 2 tabs in 24hr) M: 20 tablets |
|
|
What is the medication 'Axert' used for ? Write a typical prescription for its most common use.
|
Axert (almotriptan) is a 'triptan' used for migraines
Prescription: Axert 12.5mg tablet Take 1 tablet po od w/ H/A prn, may repeat x 1 after 2 hrs prn M: 10 tablets |
|
|
Why should one use Axert (almotriptan) instead of other triptans for migraines?
|
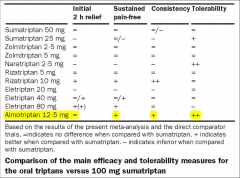
B/c it has the highest efficacy:tolerability ratio. However, this does not mean it'll be the most effective for certain pts; you may have to switch to a different triptan from which they may benefit.
|
|
|
What are options for migraine prophylaxis is someone who has frequent migraines?
|
1. B-blocker (propanolol)
2. TCA (amitriptyline / nortriptyline) 3. CCB (verapamil) 4. anticonvulsants (divalproex, gabepentin) ----------------------------------------- 1. B-blocker: propanolol Prescription: Propanolol Take 40mg po BID M: 90 tablets (45 days / 6 wks) rtc if no improvement or minimal improvement; can increase by 40mg / dose qmonthly upto a max of 160-240mg / d NOTE: B-blockers should not be used in patients >60yrs or smokers. If they're 60 or more and have an indication to use B-blockers such as a recent MI, then sure. 2. TCA: amitriptyline Prescription: Take 10mg po qhs M: 45 tablets (usual dose 150mg; can increase by 10-25mg qwkly) Note: if migraines recur after the 45 tablets, long term prophylaxis of 3 months + 1 repeat is acceptable Others: CCB: verapamil 80mg po TID NOTE: for a patient with chronic migraines, at some point it is worthwhile to consider a head CT/MRI (avoid CT if pt young due to radiation harm) NOTE: For TCA prophylaxis, you can choose between amitriptyline vs nortriptyline. The main difference is that amitriptyline is much more sedating. So if a patient says that they're having difficulty sleeping, then amitriptyline is a better choice. Both TCAs should be prescribed at night time. NOTE: Nortriptyline is better tolerated than amitriptyline. |
|
|
What are two COX-2 selective inhibitors that are used for treating pain from osteoarthritis?
|
Celebrex (celecoxib)
Prescription: Take 200mg po od M: 90 tablets + 1 repeat Mobicox (meloxicam) Prescription Initial: take 7.5mg po od (may increase upto 15mg/d) M: 90 tablets + 1 repeat NOTE: these two medications are NSAIDs and patient should be counseled about nsaid use (eg. take not on an empty stomach, renal impairment?, prev GI bleeds? NOTE: celebrex and mobicox are long acting anti-inflammatories so there isn't much sense in prescribing them prn |
|
|
Explain the PERC criteria?
|
Use of the PERC (Pulmonary Embolism Rule-out Criteria) rule can significantly decrease work-up for pulmonary embolism.
To apply this rule, the clinician must first use clinical gestalt to classify the patient as low risk. The PERC rule, which consists of eight clinical criteria including history, physical and vital signs, can then be used. If both of these criteria are met, then there is less than a 2 percent risk that this patient has a PE and no further work-up is needed. PERC Rule Age > 50 years Pulse > 100 bpm SaO2 < 94% (r. air) unilateral leg swelling hemoptysis recent trauma or surgery prior PE or DVT hormone use *score 1 for each question; a score 0/8 means pt has <1.6% chance of having a pe and avoids further investigation; if any one of these is pos. require further investigations for pe. |
|
|
What two criteria can be used to estimate the possibility of a PE?
|
1. Well's criteria
2. PERC ------------------------------------ Well's criteria: i. 3.0 clinical sx of dvt (leg swelling, pain w/ palpation) ii. 3.0 other diagnosis less likely than PE iii. 1.5 hr > 100 iv. 1.5 immobilization (≥3d) or surg. in prev 4 wks v. 1.5 previous dvt/pe vi. 1.0 hemoptysis vii. 1.0 malignancy score ≥5; pe likely score ≤4; pe unlikely ------------------------------------- PERC Rule Age > 50 years Pulse > 100 bpm SaO2 < 94% (r. air) unilateral leg swelling hemoptysis recent trauma or surgery prior PE or DVT hormone use *score 1 for each question; a score 0/8 means pt has <1.6% chance of having a pe and avoids further investigation; if any one of these is pos. require further investigations for pe. perc rule: - high NPV (when test is negative, that is likely true) - poor PPV (when test is pos, we're not sure its true) |
|
|
How does the an enlarged prostate (suspicious of BPH) present on physical exam?
|
On DRE:
- smooth - rubbery - symmetrically enlarged |
|
|
What are the symptoms of bph?
What are the complications of bph? |

- retention
- overflow incontinence - hydronephrosis and renal compromise - infection - gross hematuria - bladder stones |
|
|
What are the treatment options for bph?
For medical management, write prescription. |
MEDICAL MANAGEMENT:
Prescription Flomax 0.4mg tablet 1 tablet od (30 mins after same meal) M: 90d +/- 1 repeat If this fails, try substituting or adding Proscar 5mg tablet 1 tablet od M: 90 tablet + 1 repeat If both these fail, patient should see a urologist. Note: prior to sending the patient to a urologist a urinalysis, Cr, BUN, PSA, and renal U/S should be done note: combination of a α-adrenergic antagonist (Flomax aka tamsulosin) and a 5-α reductase inhibitor (Proscar aka finasteride) is shown to be synergistic note: onset of action for proscar is about 6 months for bph. Proscar is mainly effective when the prostate is large, otherwise it's not very useful note: 5-α reductase inhibitors stop the conversion of testosterone to the more potent dihydrotestosterone. |
|
|
What are the 2 main S/Es to warn patients about re: flomax?
|
1. orthostatic hypotension (pts need to get up slowly or else they may feel lightheaded)
2. H/As |
|
|
What are possible side effects of Proscar?
|
Sexual dysfunction (not common)
- dec. libido - erectile dysfunction |
|
|
T/F. Prednisone is contraindicated in pregnancy.
|
True
|
|
|
A patient is taking Atacand 16mg po od for her HTN. Her last visit BP was elevated at 150/98. Today it was 162/100. What dose adjustment would you make?
|
Inc. dose to 32 mg po od.
NOTE: dose effect. It needs to be doubled for it to benefit. Increasing the dose to 20mg won't do much for her HTN |
|
|
T/F. Prostatitis may present with pain at the glans penis.
|
True
|
|
|
Mum comes in with 2 month old. She is breast feeding but supplementing with formula feeds, also giving Vit D drops. She is wondering when she can stop giving the drops.
|
Breast milk has very little Vit D in it. Formula includes Vitamin D drops. So if they're getting formula, then they don't need the Vit D drops; however, best to recommend that they can stop taking Vit D drops between 6 months to 1 year; as they'll be getting more solid foods around 6 months and if they're formula feeding.
|
|
|
How do you make the diagnosis of acute bacterial sinusitis?
|
2 or more Major symptoms are present:
1. nasal congestion / purulent discharge / postnasal drainage 2. facial pressure / pain 3. hyposmia / anosmia Additionally, the symptoms have become worse after 5d of Sx onset or remained the same after 7d of Sx onset ---------------------------------------------------------- MANAGEMENT - fluids - NS rinse (Netipot) - decongestants (not more than 2d; long acting) - nasonex - amoxicillin Prescription: 1. Nasonex 50mcg Inhale 2 puffs each nostril BID M: 1 device/inhaler 2. Amoxicillin 500mg tablet Take 1 tablet po TID M: 5-10d note: antihistamines are NOT recommended note: decongestants may raise bp |
|
|
What is the management for chronic sinusitis?
|
In chronic sinusitis, Abx do not usually play a major role, For recurrent (4 or more episodes per yr) or signs of chronic sinusitis (8 wks or more of eg: nasal d/c / facial pressure / dec. ability to smell), refer them to ENT to r/o possibility of anatomical abnormalities that may require surgery.
NOTE: you only send them to ENT if they've failed abx treatment. Once the diagnosis of chronic sinusitis is made they should be referred to ENT. Antibiotics such as clavulin (augmented penicillin) or biaxin may be tried for 3-6wks for chronic sinusitis. In summary, management: - trial of abx - clavulin (augmented penicillin) or biaxin - ns rinse - decongestants (2 or less days; not more) - intranasal steroid (nasonex) - referral to ent |
|
|
Discuss approach to injecting corticosteroid in the shoulder.
[shoulder injection] |

Use posterior approach, get landmarks
i. lateral pointy edge of the scapula, approach 1 cm below towards coracoid process ~10° incline upwards, inject 1.5 inch needle 25 gauge, insert needle all the way, and inject 5cc solution of (4:1 [lidocaine:depomedrol]). Always take 4cc first of lidocaine, then 1 cc of depomedrol to avoid contamination. Wait 15s, move patients shoulder in small circles, wait for a minute and see if pain has improved. --------------------------------------------------------------------- note: it is important to tell pts that the shoulder will get stiff for the next day or two and then feel better |
|
|
What is the main difference between the TCAs: amitriptyline and nortriptyline
|
Amitriptyline is much more sedating than nortriptyline. Also, nortriptyline is better tolerated than amitriptyline
|
|
|
What are the main s/e of TCAs (amitriptyline and nortriptyline)?
|
- sedating, confusion, dec. memory
- dizziness - h/a - dry mouth - inc. appetite - wt. gain note: nortriptyline is better tolerated than amitriptyline. amitriptyline is more sedating than nortriptyline |
|
|
Write a prescription for depo-medrol (patient needs a steroid injection in shoulder)?
|
Depomedrol 40mg/mL vial
To be injected in office M: 1 Days: 1 (this way it will autodiscontinue) |
|
|
It is always best to refrain from benzodiazepines but if you have to prescribe a short course for a patient (low addiction risk) with ++ anxiety, what would you write for a prescription
|
Ativan 0.5mg tablet
Take 0.5-1 tablet po BID prn M: 15 tablets |
|
|
Write a prescription for tylenol elixir with codeine.
|
tylenol elixir with codeine
Take 10mL PO q6h prn M: 4.5L pharmacy instructions: dispense 1.5L every month |
|
|
Name 1 otc stool softener
Name 2 otc fibre pills |
STOOL SOFTENER
PEG stool softener FIBRE PILLS: - bene-fibre - metamucil |
|
|
What is the difference between GFR and eGFR?
|
eGFR is 'estimated' GFR
NOTE: eGFR tends not to be very accurate at high numbers (eg. 75-90); however, at lower numbers (eg. 32-40) it is quite a reliable estimate. For clinical purposes, we consider an eGFR to mean adequate renal function. |
|
|
Write a prescription for colace (for constipation).
|
Colace 100mg
1 tablet od M: 3 months repeat: 1 |
|
|
Where is the location of a pes anserine bursitis?
|
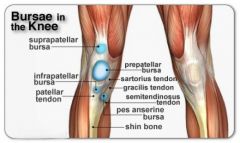
|
|
|
A 32F intending to become pregnant comes in to your office. She has HTN and is on 2 BP medications: Altace-Hctz and Norvasc. She is asking if there are any contraindications to HTN meds. What would you d/ with her.
|
d/ to discontinue Altace (ace-inhibitor)
- contraindicated in pregnancy usually pregnancy safe HTN meds include: - labetalol (most common) - α-methyldopa - (nifidipine) note: HCTz is considered safe; however, not as effective note: The following anti-hypertensives are not appropriate in pregnancy (teratogens) - ACEi - diuretics - propanolol |
|
|
At patient with 2 plantar warts comes in to your office. He has had 6 liquid nitrogen treatments 2 wks apart with modest improvement. Are there any other options for faster removal of warts?
|
PRESCRIBE:
Aldara (imiquimod) 5% cream packets Apply to affected area 3x / week at hs, then wash off in am M: 3 months Avoid aldara cream if you can and stick w/ liquid nitrogen or try other options for plantar warts including: - salicylic acid (compound W) - cantharidin |
|
|
What is a keloid?
|

A keloid is a type of scar which, depending on its maturity, is composed mainly of either type III (early) or type I (late) collagen. It is a result of an overgrowth of granulation tissue (collagen type 3) at the site of a healed skin injury which is then slowly replaced by collagen type 1. Keloids are firm, rubbery lesions or shiny, fibrous nodules, and can vary from pink to flesh-coloured or red to dark brown in colour. A keloid scar is benign and not contagious, but sometimes accompanied by severe itchiness, pain,[2] and changes in texture. In severe cases, it can affect movement of skin.
Keloids expand in claw-like growths over normal skin.[3] They have the capability to hurt with a needle-like pain or to itch without warning, although the degree of sensation varies from patient to patient. Keloids form within scar tissue. Collagen, used in wound repair, tends to overgrow in this area, sometimes producing a lump many times larger than that of the original scar. Although they usually occur at the site of an injury, keloids can also arise spontaneously. Keloids can develop in any place where an abrasion has occurred. They can be the result of pimples, insect bites, scratching, burns, or other skin trauma. Keloid scars can develop after surgery. They are more common in some sites such as the central chest, the back and shoulders and the ear lobes. The best treatment is prevention in patients with a known predisposition. This includes preventing unnecessary trauma or surgery (including ear piercing, elective mole removal), whenever possible. Any skin problems in predisposed individuals (e.g., acne, infections) should be treated as early as possible to minimize areas of inflammation. Intralesional corticosteroids are first-line therapy for most keloids. |
|
|
Which anxiolytic is indicated for generalized anxiety disorder? Write a prescription.
|
BuSpar (buspirone):
buspar take 7.5mg bid (can inc. by 5mg/d q3d; max of 60mg/d) |
|
|
A 19M comes to your office complaining of dandruff (mildest form of dermatitis) in the scalp. What is an easy otc treatment option? Note if this does not work, what is the next step in treatment (write the prescription)
|
Unfortunately dandruff cannot be entirely cured.
However, to get rid of it, Nizoral shampoo (OTC) Apply twice weekly x 8 wks prn; f/u prn Prescription: Valisone 0.1% scalp lotion Apply od prn x 1 bottle R: 1 |
|
|
A patient comes to your office with a cold sore on the lower lip. What do you do?
|
Cold sores are painful blisters that form on or near the lips and inside the mouth. They are caused by an infection with a virus called “herpes simplex virus.” There are two types of herpes virus. Type 1 causes most cases of cold sores. Type 2, also called genital herpes, usually affects the penis or vagina. Once you have the virus, you're stuck with it for the rest of your life.
MANAGEMENT: - usually required for 1st time episodes and when symptomatic Rx: Valtrex 2000mg po BID M: 2 tablets (1 day) Start with symptom onset (effectiveness dec. with delay) For suppression: Valtrex 500mg tablet Take 1 tablet po od (reassess treatment need in 4 months) |
|
|
What is gingivostamatitis?
|
Gingivostomatitis (also known as primary herpetic gingivostomatitis) is a combination of gingivitis and stomatitis, or an inflammation of the oral mucosa and gingiva. Herpetic gingivostomatitis is often the initial presentation during the first ("primary") herpes simplex infection. It is of greater severity than herpes labialis (cold sores) which is often the subsequent presentations. "Primary herpetic gingivostomatitis is the most common viral infection of the mouth"
The first time a person gets cold sores, the symptoms can include: Painful blisters on the lips, mouth, nose, or throat, which eventually pop and form scabs Mouth and throat pain Swelling in the neck Fever, body aches, and feeling ill After the first time, pain and blisters can come back, but the other symptoms do not usually happen again. Plus, the symptoms are usually milder and don’t last as long. |
|
|
A 31F pt comes in to your office requesting an OCP. She gave birth 7 wks ago
- not having any periods - difficulty lactating - taking domperidone (for breast milk secretion) What would you recommend? This woman was prescribed domperidone to aid in milk secretion. Write the prescription for domperidone. |
- estrogen in the combo ocps reduces breast milk secretion so that would not be beneficial in this case
- a progesterone only pill "Micronor" would be reasonable PRESCRIPTION: Micronor 0.35mg tablet Take as directed M: 6 months NOTE: prescription not given for 1 month with repeats b/c cost of dispensing fee each time. Better to give 6 months or 3 months + 1 repeat. The pharmacy will never dispense more than 1 month the first time for a new med. But thats their problem. Most likely, they'll give 1 month, and the 2 months worth, and then the 3 month refill. ------------------------------------------------------------- PRESCRIPTION (Domperidone) Domperidone 10mg tablet Take 3 tablets po TID x 3 wks; then dec. by 1 tablet/dose q4days until finished M: 270 tablets |
|
|
A patient comes in with menometrorrhagia for 6 months. What are some relevant investigations to do?
|
bw
- cbc, inr, ferritin - tsh, prl, lh, fsh, progesterone, NOT estrogen (no indication) - (β-hcg) pelvic u/s (r/o mass, fibroids, polyps) ----------------------------------------------------------------------- note: it is important to do a pelvic exam on this pt; before doing a pelvic exam you have to make sure the pt is NOT pregnant b/c if she is pregnant then placenta previa needs to be RULED OUT by u/s. note: pt should be treated / referred based on results. If no obv. cause a trial of OCPs is reasonable. |
|
|
What is the Shouldice Hospital?
|
Shouldice Hospital is the global leader in hernia repair. They have a 99.5% lifetime success rate for primary inguinal hernias.
It is a private institution; bed is ~$250 a day. Reasons for very high success rate are: - thats all they do (practice makes perfect) - they're selective about the pt population (generally healthy pts) |
|
|
A 45M comes in to your office. You are unsure if they're smoking. Why is it important to verify if they're smoking?
|
It is important because:
A patient who used to smoke and quit ≥10 years has the same risk of CAD as a patient who never smoked. However, once a patient has a 20 pack smoking hx, lungs are effected, and this is permanent. NOTE: in PSS (under risk), write smoking vs no smoking (enter quit date and smoking hx) |
|
|
A 4M comes in to your office with 4 day hx of fever. He also has a mild cough. How would you approach this situation?
|
- order CXR (if not already ordered) - do the Xray at GRH, so that incase you need to refer them to peds, they have the results on their system.
- even if the fever is improving, but is present on the 5th day, more investigations such as urine dip need to be done - refer them to pediatrics NOTE: fever is counted as number of days minus 1 (do not include the 1st day) NOTE: if on Day 4, the Xray results show pneumonia and pleural effusion, they need to be referred to pediatrics |
|
|
What is normal ACR for men vs women?
[as of 2014] |
Males: ≤2.0
Females: ≤2.0 |
|
|
What is a keratoacanthoma?
|

Keratoacanthoma (KA) is a common low-grade (unlikely to metastasize or invade) skin tumour that is believed to originate from the neck of the hair follicle. Many pathologists consider it to be a form of squamous cell carcinoma (SCC). The pathologist often labels KA as "well-differentiated squamous cell carcinoma, keratoacanthoma variant", because about 6% of KA manifest itself as squamous cell carcinoma when left untreated. KA is commonly found on sun-exposed skin, and often is seen on the face, forearms and hands.
TREATMENT: excision SOAP NOTE: O (observation description) 0.5cm nodular lesion w/ raised center keratinization |
|
|
Explain the approach to use when a patient c/o obstructive urinary symptoms?
|
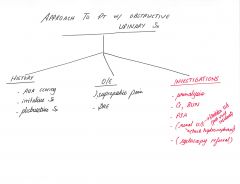
|
|
|
note
|
There is some evidence that cranberry juice can help prevent UTIs, but not treat the infection once you have it.
|
|
|
compare the S/E of PDE-5 inhibitors vs. nitro meds vs. flomax.
|
PDE-5 inhibitors: (think all in the head + dyspepsia)
- H/A - nasal congestion / rhinitis - facial flushing - dyspepsia Nitrates: - H/A - hypotension (orthostatic, advise to get up slowly) - facial flushing Flomax - H/A - hypotension (orthostatic, advise to get up slowly) |
|
|
A 72F heart failure patient comes to your office with peripheral edema and some shortness of breath. What would you do?
|
If severe shortness of breath, she needs to go to the ER; otherwise prescribe:
Lasix Take 40mg po bid M: 30d Have them f/u in 1 month, earlier prn; - at 1 month visit symptoms have improved. Do NOT discontinue lasix altogether; dec. dose PRESCRIPTION: Lasix Take 40mg po od, if wt inc. by 2-3 lbs, take 40mg po bid M: 100 tablets R: 1 - return to clinic prn, worsening shortness of breath |
|
|
How does the dosage of the beta-blocker bisoprolol differ for CHF management vs. chronic stable angina management?
|
CHF:
Bisoprolol Initially: take 1.25mg po od; double dose q2wks to target dose of 10mg Chronic stable angina: Take 5mg tablet po od (range: 5-20mg) |
|
|
What is compound W?
|

Compound W is an OTC remedy for wart removal.
It includes salicylic acid which aids in the breakdown of keratin There are 4 forms available for compound W: 1. wart remover pads 2. wart remover liquid 3. wart remover gel 4. freeze off wart remover system |
|
|
What is 'acne rosacea' ?
Write a prescription for a treatment cream |

Rosacea is a skin condition marked by redness with plaques or papules (pimples) hence the term acne rosacea. However, rosacea should not be confused with acne vulgaris that is commonly seen in teens as it is a different condition altogether. In fact, rosacea is more common in middle aged adults compared to acne vulgaris in the teenage years. Although rosacea may occur in episodes where it flares up and then resolve significantly for a period of time, the condition is progressive meaning that it will get worse over time if left untreated. The condition is more common in fair-skinned people and Caucasians but a variant of rosacea known as acne agnimata is more commonly seen in Asians and Africans.
TREATMENT: Prescription Metrogel 0.75% Gel Apply to affected areas BID M: 30g + 1 repeat |
|
|
What is the ddx for secondary dysmenorrhea?
note: primary dysmenorrhea is idiopathic (cause not known, if cause known then it is secondary dysmenorrhea) |
MORE COMMON
- endometriosis (most common) - adenomyosis - PID ------------------------------------------ LESS COMMON - polps (uterine) - fibroids (uterine) - anomalies (uterine) - intrauterine synechiae - ovarian cysts - cervical stenosis - imperforate hymen, transverse vaginal septum - IUD - copper - foreign body |
|
|
What is the indication for Ponstan? Write a prescription
|
Treatment of dysmenorrhea
Prescription: Ponstan 250mg capsule Take 2 capsules at onset of period; then 250mg QID prn M: 3 days (14 tablets) NOTE: (take with food) note: if ponstan does not do much, a trial of naproxen is reasonable. Prescription Naproxen Take 500mg tablet po BID prn M: 30 tablets |
|
|
Write a prescription for ventolin for a pt complaining of asthma symptoms.
|
Ventolin Hfa 100mcg inhaler
Take 1-2 puffs q4-6h prn M: 1 inhaler repeat: 2 |
|
|
A diabetic patient comes in with LDL levels of 4.2. What would you prescribe to lower his/her LDL levels?
|
A diabetic pt is automatically placed as high risk for cad (≥20%). Therefore, this pt would be on a statin to lower his/her ldl
PLAN: 1. Prescription Crestor 10mg od M: 3 months 2. bw_lipids, LFTs (ast, alt), ck in 6wks 3. f/u in 6-7 wks time after bw Based on the LDL levels, adjustments can be made on the crestor dosage. Max: crestor 40mg od |
|
|
Perioral dermatitis
Discuss abx management (including topical agent). |

prescription options include:
i. erythromycin base/ethyl alcohol 2 % gel (gram) topical apply to affected area bid M: 30 grams ii. tetracycline 500mg tablet bid M: 10 days Management: - d/c topical steroids - avoid all skin irritants (makeup) - erythromycin 2% gel bid vs tetracycline 500mg bid note: children <9 who have perioral dermatitis should not be treated w/ tetracycline due to potential adverse effects on teeth and bone development. Option for <9yrs would be topical or oral erythromycin. note: topical corticosteroids are not typically indicated for perioral dermatitis |
|
|
For any eye complaint, what are the main red flags to r/o?
|
- vision change / acuity / fields
- eye pain - photophobia - no trauma - ? contact lens note: important to do an eye exam for PERLA (pupils equal and reactive to light and accommodation) note: fucithalmic / erythromycin does not cover pseudomonas (contact lens wearers), whereas moxifloxacin drops does cover pseudomonas |
|
|
Define "recurrent" in the setting of urinary tract infection (uti). Write prescription for a 1st line treatment option for recurrent uti.
|
Recurrent UTI:
≥ 2 episodes in 6 months ≥ 3 episodes in 12 months PRESCRIPTION: Macrobid 100mg 1 tablet po qhs or post-coital M: 90 tablets + 1 repeat note: drug of choice should be based on urine cultures (therefore you may want to give prescription "90 + 1 repeat" after culture results come back) patients should be re-assessed following 6 months of therapy. About 50% of women may experience recurrence by 3 months after discontinuation of the prophylactic antimicrobial. If this occurs, prophylaxis may be reinstituted for as long as 1-2 years and remain effective. Women having frequent recurrences, despite prophylaxis, may require genitourinary investigation. |
|
|
Is liquid nitrogen a valid treatment for actinic keratosis?
|
yes
|
|
|
What does a myxoid cyst look like?
|

A myxoid cyst, also called a digital mucous cyst, is identified by the clear mucous that fills it. It’s a firm, smooth, rounded bump on the skin, often having a bluish tint. Inside, it is filled with clear, sticky, gelatinous fluid. The cysts appear most often on the fingers but can also show up on the toes. The myxoid cyst generally occurs in the proximal nail fold (the skin surrounding the cuticle. Cysts form from some sort of minor trauma to the site. The minor trauma can be caused by a repetitious act, including something as simple as typing or even repetitive rubbing of the area. A patient may not even be able to identify the cause.
Treatment: - liquid nitrogen - incision and compression to remove fluid |
|
|
A 4F comes in to your office w/ epistaxis x 2d (total blood loss 2 tablespoons).
Also has: - rhinorrhea, nasal congestion, sneezing What are the 2 most likely causes? |
1. viral urti (scuffing of nasal mucosa)
2. dry mucosa (winter time) Other common causes of epistaxis in kids include: - nose picking (very common) - foreign body - coagulopathies - trauma MANAGEMENT: - humidifier - nasonex (note this is a steroid, that can be used in kids >2yrs; however, like all steroids this one can make the mucosa dry, so its important to warn parent to use humidifier, and apply moisturizer/vaseline |
|
|
A patient comes in with a hx of CAD. You look at her chart and notice that she is not on a Beta blocker. She should be b/c bb are assoc. w/ a mortality benefit in pts with CAD. You put her on bisoprolol 2.5mg od. Apart from side effects what is one thing that you should warn her about that may take place in the 1st 1-2 wks?
|
dec. exercise tolerance initially (1-2 wks), then improvement
|
|
|
Discuss the preventative screening tests for men vs women.
|

|
|
|
A 24F does factory work. She wears gloves most of the time and washes her hands v. freq. at work. She comes in to your office complaining of redness, dryness, and pruritis on the dorsal surfaces of both hands. Whats your management plan?
|
MANAGEMENT
- avoid freq. hand washing unless required - use moisturizers - apply barrier cream (otc) at work Prescription: Elocom 0.1% Apply to affected areas OD M: 100g + 1 repeat |
|
|
List a few corticosteroid creams in order of potency.
|

|
|
|
When discussing Zostavax vaccine, what are some useful numbers to go over with a patient?
|
- the incidency of shingles is 1 in 3
- zostavax dec. the risk of developing shingles by 50% note: zostavax can be given in anyone ≥50 yrs; it is not covered by ohip and costs about $200-250 per vaccine |
|
|
For a pt w/ a h/a, what are some questions to ask the pt to determine if the h/a is a migraine?
|
- onset (4h-72h)
- unilateral vs. bilateral - moderate to severe intensity? - ? throbbing - ? photophobia / ? phonophobia - nausea / vomiting - does activity make h/a worse - does resting in a quiet dark room relieve the migraine ? |
|
|
A parent comes in with a child (18 months) c/o of child having only 6 words instead of 20 words. You are not concerned as you realize that kids can take longer sometimes to reach certain developmental milestones. Which is a place that you can recommend to the parent for further testing for this child?
|
Any Speech and Language Pathologist
Can easily look up a number of places in the KW region |
|
|
What is the definition of PERLA when doing an ocular exam?
|
Pupils Equal and Reactive to Light and Accommodation
|
|
|
Write a prescription of the transdermal contraceptive patch (birth control) prescribed in our office?
|
Evra 200 Mcg-35 Mcg/24Hr Patch
apply 1 patch qwk x 3wk, off x 1wk M: 3 months - Instructions to pt: start on day 1 of menstrual cycle or 1st sunday after onset of menses - restart >2wk after surgery w/ VTE risk - restart >3wk postpartum or >6wk postpartum if breastfeeding |
|
|
Before starting someone on a fentanyl patch, what must you check re: patient's current pain medications?
|
You start fentanyl at 25mcg/hr patch. For this they must be at an equivalent of at least 60mg of morphine daily.
That fentanyl patch in Canada is called "Duragesic". The patch is not for "acute" pain. It must be changed q3days |
|
|
note
|
For a patient with an MI (myocardial infarction), the guidelines recommend β-blockers; however, the benefit of β-blockers is only till the first 3 years post an MI.
|
|
|
note
|
For congestive heart failure (CHF), the guidelines recommend Ace-I and β-blockers for mortality benefit; however, evidence shows that these 2 drugs have mortality benefit only in systolic CHF with an ejection fraction of <40%.
There is no benefit in diastolic heart failure. |
|
|
What is the difference between spirometry vs. PFTs?
|
spirometry is part of PFTs (pulmonary function tests)
PFT equals: i. spirometry ii. lung volume assessment iii. diffusion capacity calculation PFTs are more useful when you're suspicious of a restrictive lung disease. If you're just concerned between distinguishing COPD from asthma, then spirometry is sufficient. |
|
|
What is the ddx for menorrhagia?
|
- hormonal imbalance
- fibroids - adenomyosis - uterine polyps - copper IUD |
|
|
For gynecological investigations - amenorrhea, menstrual irregularities, menopause, infertility, what are some bloodwork investigations to look for ?
|
- β-hcg
- cbc, lytes, inr, ferritin - lh, fsh, tsh, prl, (estrogen), progesterone, (dhea) |
|
|
What is the Rx for ptsd-related nightmares and sleep disruption?
|
Prazosin
Initial: 1mg po qhs Titrate: by 1mg po every 3 days upto a max dose of 15mg daily |
|
|
What is the management of PTSD?
|
i. cbt
ii. medications - SSRIs - benzos (avoid due to strong addictive potential) - atypical antipsychotics (quetipine, olanzapine, risperidone) iii. EMDR (eye movement desensitization and reprocessing) NOTE: for ptsd-related nightmares and sleep disruption, the following is used: Prazosin Initial: 1mg po qhs Titrate: by 1mg po every 3 days upto a max dose of 15mg daily |
|
|
For DM II, would you ever prescribe januvia and victoza together?
[diabetes] |
No
They both function to inc. the amount of incretins - januvia works by inhibiting dpp-4 (enzyme that eats away at the incretins released by the GI tract) and by delaying gastric emptying - victoza = injecting incretins SC - get absorbed into the blood Similarly insulin should not be used w/ diamicron. No point as diamicron is a secretagogue. |
|
|
What are some treatment options for superficial bacterial skin infections? Write the prescriptions.
|
note: for practical purposes advise/prescribe the following creams tid (3x/d)
i. polysporin (otc) apply to affected areas od-tid ii. fucidin 2% cream M: 30g repeat: 1 apply to affected areas bid-qid (duration usually 10d) iii. Fucidin H cream (fucidic acid 2% - hydrocortisone 1%) Apply to affected areas tid M: depends (duration usually 10d) iv. bactroban 2% cream Apply to affected areas tid M: 30g R:1 (NOTE: how much you give depends on the area) (duration usually 10d) note: fucidin H cream is 2% fucidin and 1% HC. This should be prescribed for treating an infection + inflammation. Fucidin H cream is prescribed TID |
|
|
What is the purpose of opioids such as morphine in shortness of breath (dyspnea) for CHF?
|
In a CHF exacerbation, patients may have severe sob. If the patient is palliative, then an opioid will reduce the respiratory drive (the need to breath) and provide some relief for their sob.
|
|
|
Whats the harm in stopping benzodiazepines abruptly?
|
inc. risk of seizure
|
|
|
Does wellbutrin increase or decrease your seizure threshold?
|
It decreases your seizure threshold. Hence, you are more likely (odds are still quite low) to get a seizure
|
|
|
Approach to fatigue?
|

|
|
|
What is one major s/e of beta blockers to look out for?
|
lightheadedness
|
|
|
note
|
People should not be put on januvia and victoza together. Both increase amount of incretin in blood stream. Victoza does this directly and Januvia inhibits the enzyme dpp-4 (enzyme that breaks down incretins secreted by the GI tract)
|
|
|
T/F leg swelling is a s/e of lyrica and gabapentin?
|
True
|
|
|
What is glucosamine used for ?
|
osteoarthritis (knee)
- minimal benefit for pain relief based on trials - dose studied was 500mg TID - should not be given to patients w/ shellfish allergy - also comes in a combination of glucosamine (500mg) + chondroitin (400mg) taken TID |
|
|
Explain the difference between the following nsaids?
- advil - naproxen - celebrex |
note: COX 1 and 2 are key enzymes in the inflammatory cascade of the body. When these two enzymes are inhibited, the production of arachidonic acid is blocked, thereby decreasing the amount of prostaglandin G2 (PGG2). As a result of decreased PGG2, there is a decrease in the production of prostaglandins, important factors in inflammation, pain and fever, as well as a decrease in the production of thromboxanes which normally activate platelets and cause constriction of blood vessels.
ADVIL is a non-selective nsaid that inhibits cox1 and cox2 enzymes. It is the shortest acting of the three drugs (can be taking q4h prn). NAPROXEN is v. similar to advil in that it inhibits both cox1 and cox2. Main difference is that naproxen is longer acting ie. an intermediate-acting nsaid (taken bid prn) CELEBREX (mobicox is similar) is a selective inhibitor of COX2. It does not inhibit COX1 and therefore is less likely than advil or naproxen to cause adverse gastric S/Es such as bleeding. It is a long acting nsaid (taken od prn) |
|
|
What is celebrex used for?
|
- osteoarthritis (200mg od)
- rheumatoid arthritis (100-200mg bid) - ankylosing spondylitis (200mg od) - dysmenorrhea (200mg bid) - acute pain (200mg bid) |
|
|
What are contraindications to nsaid use?
|
- impaired renal function
- gastric / peptic ulcers - cardiovascular disease inc. heart failure - nsaid allergy - ongoing treatment w/ anticoagulants / coagulopathy - pregnancy (may lead to premature closure of DA) - caution in pts > 80 yrs - caution in asthmatics --------------------------------------------------------------------------------- So if a patient needs NSAIDs and they have some inflammatory condition like a bursitis, you give them alternatives, like icing and tylenol (inflammation subsides on its own), or you give them NSAID + PPI or a combination pill (vimovo), or a topical anti-inflammatory such as Voltaren gel. |
|
|
Patient comes in to your office 2nd visit for acute gouty flare. On the first visit you prescribed colchicine. The patient is allergic to NSAIDs. What are your options for management?
|
Best option is corticosteroid injection (not typically done the GP office)
Other option is prednisone (eg. prednisone 50mg od po M: 5d (short duration; no tapering required) NOTE: make sure to mention rare possibility of avascular necrosis DO NOT prescribe allopurinol for an acute gouty flare as this can makes things worse. |
|
|
What are the signs / symptoms of acute gout?
|

- joint pain (++), erythema, swelling
- restricted joint mobility - tophi may be present (see picture) - kidneys: gouty nephropathy, uric acid calculi |
|
|
What does a gouty foot look like ?
|

NOTE: the 3 most common places for gout are:
i. 1st MTP (most common) ii. ankle iii. knee NOTE: gout is an asymmetrical arthritis |
|
|
How does gout differ from cellulitis?
|
An acute gouty attack may mimic cellulitis; however, joint mobility is preserved in cellulitis.
|
|
|
What investigations would you do for gout?
|
Gout is a clinical diagnosis
However, investigations include: i. serum uric acid levels ii. joint aspirate --> crystals of monosodium urate (negatively berefringent, needle shaped) iii. xray (may show punched out lesions) NOTE: serum uric acid is good for baseline; however, cannot diagnose or rule out gout as normal levels appear w/ acute flare ups |
|
|
What are the precipitants of gout?
|
DRUGS (pneumonic = fact)
furosemide asa / alcohol cytotoxic drugs thiazide diuretics FOODS (pneumonic = salt) shellfish anchovies liver / kidney turkey sardines (a type of fish) Gout is also associated in pts with - htn - dm - obesity - starvation - dehydration - trauma, illness, and surgery |
|
|
Discuss the medical vs. non-medical management of gout.
|

|
|
|
T/F. Tolerance is a major problem with the use of nitrates as chronic anti-anginal therapy.
|
True
To prevent tolerance, the main strategy would be to use it intermittently w/ adequate nitrate-free intervals. NOTE: tolerance would not be a problem for nitroglycerin spray or SL; however, the patch would cause tolerance |
|
|
For the various nitrate therapies used in acute on chronic stable angina...i.e. nitroglycerin SL (tablet), nitroglycerin spray, nitro-dur (patch), write a prescription.
note: there is a nitroglycerin ointment as well; however, the above 3 are more commonly prescribed |
nitroglycerin SL (tablet)
take 0.3mg tablet SL q5minutes prn; maximum 3 doses within 15 minutes M: 30 tablets nitroglycerin spray take 0.4mg/dose spray q5minutes prn; maximum of 3 sprays within 15 mintues M: 1 device + repeat: 1 nitro-dur (patch) apply 0.2(0.4)mg/hr patch for 12 hours on, then 12 hours off M: 90 patches (check what the Mitte should be ?????) note: max is 0.8mg/hr patch note: for acute stable angina, the tablet (SL) and spray would be more effective than the patch (nitro-dur); however, for angina prophylaxis the patch would be a better option OR the nitroglycerin SL tablet / nitroglycerin spray can be taken 5 minutes prior to strenuous activity. |
|
|
Discuss the target doses of the anti-hypertensives +/- ASA 81mg od used for the following cardiac conditions:
- HTN - CHF - chronic stable angina - CAD - atrial fibrillation |
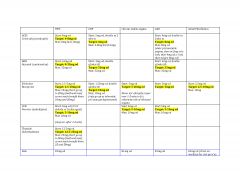
|
|
|
Discuss medication management for smoking cessation.
|
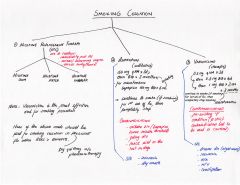
|
|
|
Discuss how the epley manuever is done in the office?
|

|
|
|
Discuss how the brandt-daroff exercise is done for bppv.
|
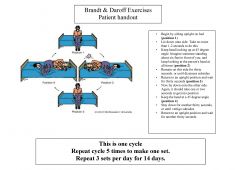
|
|
|
hepatitis c
- how is it transmitted? - what is the management? - discuss prognosis? |
transmission:
- parenteral (transfusion, iv drug use, sexual) management: - prevention: no vaccine - Rx: α-interferon SC injection wkly and ribavarin po bid (only 50-80% success rate, s/e common) prognosis: - chronicity 80%; 20% of these develop cirrhosis - hepatocellular carcinoma in 2-5% of cirrhosis / yr - may develop b-cell non-Hodgkin lymphoma |
|
|
hepatitis a
- how is it transmitted? - what is the management? - discuss prognosis? |
transmission:
- fecal-oral route management: - general hygiene - treat close contacts (w/ anti-HAV Ig) - prophylaxis for high risk grps unless immune prognosis: - no chronicity - virus clears up on its own |
|
|
hepatitis b
- how is it transmitted? - what is the management? - discuss prognosis? |
transmission:
- parenteral (transfusion, iv drug use, sexual) - vertical management: - prevention: HBV vaccine and / or hep b Ig (HBIG) for needlestick, sexual contact, infants of infected mothers unless already immune - for chronic hep b: minimize alcohol, and Rx w/ interferon, adefovir etc (see. toronto notes/uptodate) prognosis: - chronic in 20% of pts |
|
|
What are the 4 main anti-cholinergic side effects?
|
- blurry vision
- dry mouth - difficulty urinating - constipation |
|
|
Distinguish between 1°, 2°, and 3° syphilis.
|
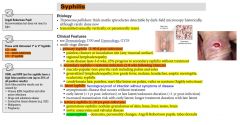
|
|
|
What is the treatment for syphilis?
|
for 1°, 2°, early latent:
- PenG 2.4M U IM x 1 for 3°, late latent: - benzathine PenG 2.4M U IM wkly x 3 if allergic to penicillin: doxycycline 100mg po bid x 14d note: neurosyphilis requires PenG 18-24M U/d IV x 10-14d |
|
|
Image of 1' syphilis chancre sore (ulceration)
|

|
|
|
Image of maculo-papular rash found in 2° syphilis
|

|
|
|
What is ODB?
Who is eligible for the ODB (ontario drugs benefit) program? |
ODB = Ontario Drug Benefit program that covers most of the cost of 3,800 prescription drug products, some nutrition products and some diabetic testing agents. The list of products covered by the ODB program is called the "Formulary". Some products listed on the Formulary will only be funded in limited circumstances and/or for a limited duration in time.
As well, under special circumstances the Exceptional Access Program may cover most of the cost of an additional 850 prescription drug products that are not on the Formulary for people in the ODB Program. Your doctor must apply on your behalf. Approval must be given by the ministry before a drug will be funded by the program if it is not on the Formulary. To qualify, an Ontario doctor or other authorized prescriber must prescribe the drugs and you must buy them from either: an accredited Ontario pharmacy OR an Ontario doctor who is licensed to sell prescription drug products and is linked to the ministry’s Health Network System. ----------------------------- You are eligible for ODB program benefits if you live in Ontario, you have a valid Ontario health card and at least one of these statements applies to you : - 65 years of age or older - live in a Long-Term Care Home or a Home for Special Care - enrolled in the Home Care program - have high drugs costs relative to my income and are registered in the Trillium Drug Program - receive social assistance through Ontario Works or the Ontario Disability Support Program. |
|
|
What are the contraindicative urinary tract infection (uti) drugs in pregnancy?
|
NOTE: nitrofurantoin / macrobid is CONTRAINDICATED between 36-42 wks GA, and during labour due to the possibility of hemolytic anemia.
NOTE: septra is contraindicated in the 1st trimester b/c it may limit availability of folic acid to the fetus as well as the last 6 wks of pregnancy as it may cause kernicterus For the contraindications, consider instead using amoxicillin 500mg tid x 7d or keflex 500mg qid x 7d |
|
|
Discuss the various stages of chronic kidney disease in terms of GFR.
|
stage I: GFR≥90 ml/min
stage II: GFR 60-89 ml/min stage III: GFR 30-59 ml/min stage IV: GFR 15-29 ml/min stage V: GFR <15 (or dialysis) |
|
|
What is the Rx for PID (pelvic inflammatory disease)?
|
prescription:
- cefixime 400mg tablet 2 tablets (800mg) x 1 M: 2 tablets AND - doxycycline 100mg bid M: 14 days Note: this is reportable and any partners must be treated |
|
|
What is the criteria for diagnosis of PID?
|
MUST HAVE:
- lower abdo pain - CMT - adnexal tenderness PLUS 1 or more of: - fever - mucopurulent cervical d/c - high risk partner - positive culture for N. gonorrhea or C. trochomatis, E. coli or vaginal flora - leukocytosis - cul-de-sac fluid, pelvic abscess or inflammatory mass on u/s or bimanual - elevated crp or esr |
|
|
Write a prescription for the Rx of urethritis - gonococcal.
|
cefixime 800mg x 1
PLUS azithromycin 1g x 1 Note: this is reportable and any partners must be treated |
|
|
Write a prescription for the Rx of urethritis - nongonococcal (chlymydia)
|
azithromycin 1g x 1
Note: this is reportable and any partners must be treated |
|
|
Write a prescription for cervicitis. NOTE: the causative agent are n. gonorrhea and c. trochomatis.
|
cefixime 400mg x 1
PLUS azithromycin 1g x 1 Note: this is reportable and any partners must be treated |
|
|
What are the common s/e of the atypical antipsychotics. What are the distinguishing s/e of each of the atypicals.
These atypicals are: - risperidone - olanzapine - clozapine - quetiapine (seroquel) |
- anticholinergic s/e: blurry vision, dry mouth, constipation, urinary retention
- antihistaminic s/e: sedation, drowsiness - antiadrenergic s/e: postural hypotension, impotence, failure to ejaculate - metabolic s/e - weight gain, hyperglycaemia, hyperlipidemia (NOTE these are not typically present in TYPICAL antipsychotics) --------------------------------------------------- Distinguishing s/e of ROCS (atypical antipsychotics) - Risperidone (Risperdal): EPS (more likely) - Olanzapine (Zyprexa, Zydis): ++ wt gain compared to the others (assoc with diabetes and hyperlipidemia) - Clozapine (Clozaril): 1% risk of agranulocytosis (required to do weekly blood counts for at least 1 month, then biweekly) - Quetipine (Seroquel): Most sedating |
|
|
Discuss the management of constipation.
|

|
|
|
What are sitz baths?
|

a bath in which a person sits in water up to the hips. It is used for conditions such as:
- hemorrhoids (piles), anal fissures, rectal surgery - episiotomy, uterine cramps - inflammatory bowel disease - infections of the bladder, prostate or vagina. It works by keeping the affected area clean and increasing the flow of blood to it. Warm baths are recommended for reducing the itching, pain and discomfort associated with conditions such as hemorrhoids and genital problems. An ordinary bathtub can be filled with 3 to 4 inches (7.6 to 10 cm) of hot water (about 110 °F (43 °C)), and sit in for 15–20 minutes or until the water cools down. Alternatively, a large basin can be used, and there are specially built devices that fit into toilet bowls. NOTE: you can use some salt in the water too. |
|
|
Discuss the management for hemorrhoids.
|
1. check FOBT vs colonscopy dates
2. increase fibre intake; benefibre (otc) vs. metamucil (otc); consider stool softener 3. tylenol prn (if pain) 4. sitz baths 5. anusol HC 1% NOTE: anusol hc comes in 0.5% (otc), 1%, and 2.5% (avoid the 2.5% cream because the rectal skin area is quite thin; the 1% cream is ideal. Prescription (in pss): Medication: Anusol HC 1% cream; apply to affected area tid and after bowel movement prn M: 15g repeat: 1 |
|
|
Patients with atrial fibrillation are at increased risk for stroke. The CHADS2 is a risk prediction tool used to estimate the odds of a stroke and therefore allow for managing the pt accordingly. What is the CHADS2 score?
|

|
|
|
A baby presents with oral thrush, what would you treat this baby with.
|
Nystatin
- topical antifungal - not absorbed systemically Prescription: Nystatin 100,000/mL suspension orally 1mL qid M: 7 days NOTE: it is best to treat the mum as well, because she may have thrush on the nipple(s) and can pass it on to the baby after it's treated. Prescription (mum): Nystatin 100,000 units/gram cream apply tid x 7 days M: 15 grams |
|
|
Give an example of PSS charting for 'PERS (personal)' section
[mammogram, pap, fobt, screening] |
daughters - Amy 1986, Lisa 1988, husband Spencer (job)
ahe bw **given** (or ahe 04/14) fobt **given** (or 'no fobt b/c age >75') pap 03/14 (or write 'no pap b/c hyst 1990' or 'no pap b/c age>70') bmd 04/14 mammo 08/14 (or 'no mammo given age>75') note: if the pt is >70 and has had 3 or more normal paps in the last 10 years, then paps can be stopped; however, they should be continued if they've had 1 or more abnormal paps |
|
|
List of important websites for calculating:
i. 10yr risk of having a heart attack ii. 10yr risk of developing general cardiovascular disease iii. cholesterol conversion |
i. framingham risk calculators
http://www.framinghamheartstudy.org/risk-functions/index.php ii. 10yr risk of having a heart attack http://cvdrisk.nhlbi.nih.gov/calculator.asp note: this risk assessment tool assumes the pt is free of coronary heart disease, intermittent claudication and diabetes, and is between ages 30-79 Variables include: age, gender, total cholesterol, hdl, smoking status, SBP, yes/no for htn Rx iii. 10yr risk of developing 'general' cardiovascular disease (coronary death, MI, coronary insufficiency, angina, ischemic stroke, hemorrhagic stroke, transient ischemic attack, peripheral artery disease, heart failure); this is for individuals aged 30-74 and w/o cardiovascular disease at baseline examination. http://www.framinghamheartstudy.org/risk-functions/cardiovascular-disease/10-year-risk.php# - once at this site scroll down and choose --> risk score calculator --> interactive --> using lipids Variables include: age, gender, sbp, yes/no for htn Rx, smoking status, diabetes status, hdl, total cholesterol iv. cholesterol conversion: http://www.onlineconversion.com/cholesterol.htm ------------------------------- NOTE: the 10 yr risk of developing 'general' cardiovascular disease should probably be used for determining management of pts' risk factors such as lipids, bp, smoking etc. as this tool is more inclusive; whereas, the 10yr risk of having a heart attack is very specific and underestimates the probability of general heart disease NOTE: in PSS, the calculator resembles the 10yr risk of developing 'general' cvd; therefore that is a good option as well. NOTE: the PSS calculator for predicting 10yr risk of cvd includes the following predictors: age, gender, hdl, total cholesterol, sbp, diabetes status, smoking status, established cvd (stroke, mi, angina, claudication), yes/no for htn Rx, 1° relative w/ CAD before 55 |
|
|
What is bronchitis (acute) ?
|
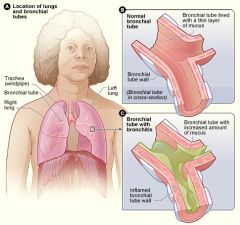
Acute inflammation of the tracheobronchial tree causing inflammation leading to bronchial edema and mucus formation. It is characterized by a cough (>5days), with or without sputum production. Other symptoms include sore throat, runny nose, nasal congestion (coryza), low-grade fever, pleurisy, malaise, and sputum production.
Chronic bronchitis on the other hand is a type of COPD characterized by the presense of a productive cough that lasts for 3 months or more per year for at least 2 years. |
|
|
What is the relative risk reduction of statins?
|
30%
Therefore, if a patient has a 10 yr risk of 6% you're reducing the risk by 1-2%. So even if the LDL is 5.05 which is >5, why put them on a statin unless they have familial hyperlipidemia. In someone with a 10 yr risk of 30% you would be reducing the risk by 9% by using statins; therefore much more useful in this group. Before deciding whether or not to put a pt on a statin (s/e of myalgias and liver toxicity) use the framingham 10yr general cvd risk assessment tool to see if the pt is a mild, mod, or high risk of developing cardiovascular disease. |
|
|
Which ocp should you prescribe for acne control and period regulation?
|
Diane-35 is indicated for acne control; however, other ocps like Alesse and Tri-cyclen Lo have some benefit for improving acne.
note: Diane is not typically marketed as an ocp, it is more for acne control; however, in theory it should be an effective ocp. |
|
|
Which STIs are reportable to public health Canada?
|
i. HIV
ii. Gonorrhea iii. Chlamydia iv. Syphilis v. Hep B,C,D |
|
|
T/F. Metformin is associated w/ weight gain.
Is insulin associated w/ weight gain ? |
False. Metformin is NOT associated w/ weight gain.
Insulin is associated with more rapid weight gain. Its a viscous cycle. The fatter you get the more insulin resistance you get and you require more insulin. The more insulin you take the fatter you get. |
|
|
T/F. Januvia is a weight neutral hypoglycemic agent.
|
True
|
|
|
What can precipitate irritable bowel syndrome?
|
stress
|
|
|
How long should one treat for depression with anti-depressants?
|
6-12 months: if 1st or 2nd episode
2 years: - if third episode - elderly - psychotic features - refractory depression - >2 episodes in 5 years |
|
|
According to the Women's Health Initiative (WHI), what are HRT benefits and HRT risks?
|
HRT Benefits:
- protect against colon cancer - protect against osteoporotic #s HRT Risks: - invasive breast cancer (no inc. risk w/ 1st 5 yrs of use) - coronary heart disease - stroke - DVTs or PEs - Dementia and mild cognitive impairment: women taking estrogen-alone before the age of 65 were less likely to develop dementia, however there was a 50% inc. risk of developing dementia when taken after 65 yrs of age (those taking combined HRT were at even greater risk) |
|
|
How can the estrogen component in HRT be given to patients in menopause?
|
- can be given orally or transdermally (eg. patch, gel)
- TRANSDERMAL is preferred in women with hypertriglyceridemia or impaired hepatic function - must be given in lose doses |
|
|
note
|
Osteoporosis is the single most important health hazard associated with menopause.
Cardiovascular disease is the leading cause of death post-menopause. |
|
|
What is the primary indication for using HRT?
|
vasomotor instability
- HRT should be prescribed at the lowest effective dose (0.3mg Premarin) and the duration of treatment should be short (<5 yrs) |
|
|
What are the absolute contraindications of HRT?
What are some relative contraindications of HRT? |
ABSOLUTE CONTRAINDICATIONS
ABCD - Acute liver disease - undiagnosed vaginal Bleeding - Cancer (breast/uterine) - DVT (thromboembolic disease) --------------------------------------------------- RELATIVE CONTRAINDICATIONS Relative contraindications include: - pre-existing uncontrolled HTN, familial hyperlipidemias, migraine H/As - DM (w vascular disease) - gallbladder disease, hypertriglyceridemia, impaired liver function (consider transdermal estrogen) - uterine fibroids and endometriosis - fibrocystic disease of breasts |
|
|
What are some of the S/E of HRT?
|
- abnormal uterine bleeding
- mastodynia (breast tenderness) - edema, bloating, heartburn, nausea - mood changes (progesterone) |
|
|
Why is progestin given as part of HRT?
|
It is given in combo with estrogen for women with intact uterus to prevent development of endometrial hyperplasia or cancer.
A women who has had a hysterectomy can be given unopposed estrogen. |
|
|
What is peri-menopause?
|
period of time surrounding menopause (2-8 yrs preceding + 1 yr after last menses) characterized by fluctuating hormone levels, irregular menstrual cycles, and symptom onset
|
|
|
For women in menopause getting treated with HRT, what is the risk of developing breast cancer?
|
relative risk is 1.3, therefore periodic surveillance and counselling is required. However, the absolute risk is very very low.
The 1.3 risk is associated with only the estrogen + progesterone HRT, but not with estrogen-only HRT note: there is no inc. risk at <5 years. The risk mentioned above applies to women taking HRT >5yrs |
|
|
What are the main clinical symptoms of menopause and how would you manage each of these?
|
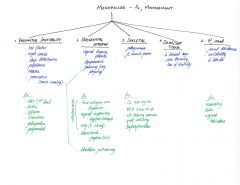
|
|
|
What are the types of menopause?
|
i. physiological (average age 51 - follicular atresia)
ii. premature ovarian failure, before age 40 (autoimmune disorder, turner's syndrome, infection) iii. iatrogenic - (surgical/radiation/chemo) note: menopause is defined as absense of menses for 1 yr |
|
|
What are the cardinal signs of infection?
|
- erythema
- pain - warmth - swelling - bleeding/pus/fever |
|
|
What is Raynaud's phenomenon?
|
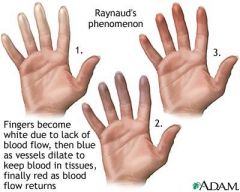
Vasospastic disorder characteristically causing discolouration of the fingers and toes (white --> blue --> red).
Classic triggers: cold and emotional stress |
|
|
note
|
Food triggers for IBS include:
- milk products - egg yolks - fatty foods - spicy foods - beans and lentils NOTE: it is often hard to pinpoint what the trigger food for one particular individual is; therefore, a food diary is very beneficial in isolating the cause. |
|
|
Which is a more valid measure of Diabetes? Fasting Blood glucose or HbA1C?
|
HbA1C
Therefore is a patient comes in and says that his/her BG levels have been ranging from 5-7; but his/her HbA1C comes out to 11, be very skeptical. This patient will likely have to go on insulin; b/c each of the antiglycemic agents reduce HbA1C from 1-2%. NOTE: All of the above being said, HbA1C can be misleading sometimes. An HbA1C can be 7 is a pt is having sugars that are lows half the time, and highs the other half to balance the HbA1C to a nice middle number such as 7. Therefore, be cautious of a good HbA1C reading if the pts blood sugars are in the extremes. It is beneficial to look at the pts sugar diary. |
|
|
When counselling a patient on acne it is very important to discuss what with the patient?
|
- Discuss not to pop or scratch lesions otherwise there is a risk of permanent scarring
|
|
|
If a patient comes in with mild localized acne, what are two most common prescription medications you could give them?
|
Must always wash, rinse, and dry area before applying cream/gels
1. Benzoyl peroxidase Gel 5-10% apply to affected areas bid M: 30g with 1 repeat (Must tell patient that this may cause bleaching of clothes sheets); if patient does not want to try this then try Stievamycin 2. Stievamycin mild gel apply to affected areas qhs M: 30g with 1 repeat |
|
|
If a patient has diarrhea, what RFs would increase the probability of them having C.difficile associated diarrhea?
|
- recent hospitalization
- recent antibiotic use - age > 65 - immunosuppression |
|
|
What are the problems with giving mixed insulin formulations?
|
Patients:
- must have regular activity levels - must have meals at consistent times (eating regularly); b/c if you miss a meal, you run the risk of hypoglycemia |
|
|
For a diabetic patient with HTN, what are the best anti-hypertensive drugs?
|
Ace-I and ARBs
- Ace-inhibitors is better for vascular and renal protection - ARBs work equally well but have been studied less than Ace-i |
|
|
When dealing with a clinical situation and coming up with a diagnosis, one must always ask 3 questions. What are they?
|
i. What is the most likely problem?
ii. What are the alternatives (DDx)? iii. What must I not miss? |
|
|
If someone is on an Ace-I, would it be appropriate to give ARBs with that medication?
|
No. studies show that there is no added benefit
The only case where ARBs are given with ACE-inhibitors is CHF (the benefit is not for mortality; only for hospitalization) |
|
|
Which thiazide diuretic is more potent? HCTz or chlorthalidone?
|
Chlorthalidone
|
|
|
What is the treatment for pharyngitis in children?
|
90% of pharyngitis is viral; if suspicious of bacterial pharyngitis, then:
amoxicillin 40 mg/kg/day divided BID / TID; note: (max 3g/day) M: 10d |
|
|
Which class of anti-hypertensives is not recommended for smokers and asthmatics?
|
β-blockers
|
|
|
Why is it important to check bloodwork before switching BP meds?
|
- to r/o electrolyte imbalances
|
|
|
What is the treatment for adult pharyngitis?
|
90% of pharyngitis is viral; if suspicious of bacterial pharyngitis, then:
penicillin V 600mg po BID M: 10d |
|
|
Which class of anti-hypertensives is not recommended as first line treatment for the elderly (>60)
|
b-blockers
|
|
|
T/F. For patients with bipolar depression, it is not a good idea to put them on monotherapy with antidepressants.
|
True
This is b/c a switch from depression to mania can occur. |
|
|
note
|
When prescribing anti-depressants, it is very important to be particularly vigilant over the first 2 weeks of therapy as neurovegetative Sx may start to resolve while emotional and cognitive Sx may not (patients may be particularly at risk for suicidal behaviour during this time)
|
|
|
What must you r/o when assessing for suspected urinary tract infection (uti)?
What should you do on physical exam? |
r/o pyelonephritis
Check for - suprapubic tenderness - check for CVA tenderness Must r/o fever |
|
|
What is the 1st line antibiotic for acute otitis media (aom) in children (with chronic TM perforation or ventilation tubes)?
|
ciprodex otic suspension 4 drops BID M: 7d
|
|
|
How soon to anti-depressants start working?
|
ONSET OF EFFECT:
- neurovegetative Sx: 1-3 wks - emotional/cognitive Sx: 2-6 wks |
|
|
What is the 1st line antibiotic for acute otitis media (aom) in children (without TM perforation)?
|
amoxicillin 80mg/kg/day divided BID / TID (max 3g/day)
M: 5d in children ≥ 2 yrs M: 10d in children < 2 yrs or recurrent otitis media |
|
|
T/F. Dry cough is a S/E of ACE-inhibitors but not of ARBs
|
True
|
|
|
What is the 1st line antibiotic for acute otitis media in adults (with chronic TM perforation or ventilation tubes)?
|
ciprodex otic solution 4 drops bid M: 7d
|
|
|
What is the 1st line antibiotic for acute otitis media in adults (without TM perforation)?
|
amoxicillin 500mg tid M: 5d
|
|
|
In younger people with HTN, what is the choice of anti-hypertensive?
|
- Diuretics eg. chlorthalidone
NOTE: both diuretics and Ace-inhibitors are equally effective; however, diuretics are cheaper, so we use these in younger patients. |
|
|
What is meant by complicated cellulitis?
|
cellulitis of the face or diabetic foot
|
|
|
What is the classification of migraines?
|
i. common migraine: no aura
ii. classic migraine: with aura iii. complicated migraine: with severe/persistent sensorimotor deficits |
|
|
How is a diagnosis of obstructive sleep apnea (OSA) made based on a nocturnal polysomnograph?
|
If it shows >15 apneic episodes / hr of sleep with arousal
NOTE: apneic episodes can last from 20 seconds to 3 minutes; can have 100-600 episodes/night |
|
|
What is the 1st line antibiotic for uncomplicated mild cellulitis?
|
MILD
Keflex 500mg po QID M: 7d with f/u prn MODERATE For moderate cellulitis M:10d with f/u prn --------------------------------------------- In children: Keflex 50-100mg/kg/day divided q6h (upto a max of 2000mg/day M:7 (mild) M: 10 (moderate) with f/u prn |
|
|
What are some treatment options for snoring?
|
- sleep on side (position therapy)
- weight loss - nasal dilators - tongue-retaining devices - mandibular advancement devices |
|
|
What are the RFs for osteoarthritis?
|
- genetic predisposition
- advanced age - obesity (for knee OA) - female - trauma |
|
|
What are some RFs for DM?
[diabetes] |
RFs for DM type I:
- personal or family hx of autoimmune disease DM type II: - first degree relative with DM - age >40 - obesity, HTN, hyperlipidemia, vascular disease - prior GDM, macrosomic baby - PCOS - hx of impaired glucose tolerance or impaired fasting glucose - presence of complications assoc. with diabetes - members of high risk populations (SE Asian, hispanic, Africans, Aboriginals) |
|
|
A patient comes in with a corneal abrasion and ++ conjunctivitis. What prescription would you write for eye drops (antibiotics)? What if this patient has ++ eye pain? What if this patient has photophobia? (CHECK THIS SLIDE WITH CHUBBS)
|
Antibiotics:
i. erythromycin ophthalmic 0.5% ointment Apply 1 cm ribbon tid to affected eye x 7 days M: 3.5g + 1 repeat ii. Fucithalmic 1% eye drops Apply bid x 7 days M: 1 bottle Analgesia: - Ketorolac ophthalmic 0.5% 1 gtt in eye qid x 7 days M: 1 bottle Photophobia: - homatropine 5% solution Apply 1-2 gtt q3-4 h x 4d M: 1 bottle |
|
|
What are the common joint sites of involvement in osteoarthritis?
|
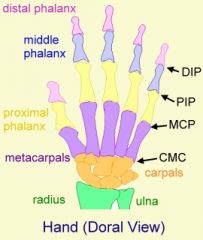
Hand (DIP, PIP, 1st MCP, 1st CMC)
Hip Knee 1st MTP (big toe) Spine (L4-L5, L5-S1) C-spine NOTE: - uncommon to have involvement in the shoulder, elbow, ankle, MCPs, rest of wrist |
|
|
hand anatomy
[joints, bones] |
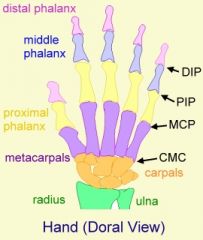
|
|
|
foot anatomy
[joints, bones] |
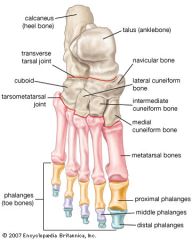
|
|
|
T/F. One should not delay antibiotics while waiting for a lumbar puncture if meningitis is suspected.
|
True
|
|
|
What are the radiological hallmarks of osteoarthritis (OA)?
|

i. joint space narrowing
ii. subchondral cysts iii. subchondral sclerosis iv. osteophytes |
|
|
What are the indications for a lumbar puncture? What are the contraindications?
|
INDICATIONS
Diagnostic: - CNS infection (meningitis, encephalitis) - Inflammatory disorder (MS, Guillain-Barre, vasculitis) - Subarachnoid hemorrhage (if CT negative) - CNS neoplasm (neoplastic meningitis) Therapeutic: - to administer anesthesia - chemotherapy - contrast media - to decrease ICP (pseudotumour cerebri, normal pressure hydrocephalus) _________________________________________________ CONTRAINDICATIONS - mass lesion causing increased ICP - could lead to cerebral herniation (requires CT first) - infection over lumbar puncture (LP) site - low platelets or treatment with anticoagulation (high INR or aPTT) - uncooperative patient |
|
|
What is Kussmaul breathing?
|
- Deep, labored breathing often associated with severe metabolic acidosis particularly diabetic ketoacidosis (DKA).
|
|
|
Is osteoarthritis a symmetrical or asymmetrical arthritis?
|
asymmetrical
|
|
|
How should you screen for DM?
[diabetes] |
Screen every 3 years starting at age 40; if one or more RF can screen earlier.
|
|
|
The most common cause of R. sided heart failure is __________?
|
L sided heart failure
|
|
|
What investigations would you do in a patient with suspected osteoarthritis?
|
- x ray* (most important and relevant)
other tests include: - CBCs and ESR (should be normal) - RF and ANA (should be negative) - synovial fluid analysis: should be non-inflammatory |
|
|
Discuss the main s/e of SSRIs?
|
i. sexual dysfunction (upto 90% incidence) - dec. libido, potency (males), ejaculation and orgasm
ii. GI s/e: n/v, diarrhea, bloating, cramps iii. h/a, tremor, insomnia, sedation iv. dry mouth, sweating |
|
|
Discuss the main s/e of typical antipsychotics?
|
Low potency:
- anticholinergic: dry mouth, blurred vision, constipation, urinary retention - antiadrenergic: orthostatic hypotension, impotence, failure to ejaculate - antihistaminic: sedation High potency: - EPS (dystonia, akathisia, pseudo-parkinsonism, dyskinesia) - neuroleptic malignant syndrome (allergic rxn) |
|
|
What should the BP and lipid levels be for a patient with DM?
[diabetes] |
BP <130/80
Lipids: - LDL <2.0 M - TC/HDL <4.0 M |
|
|
A patient comes in for a DM f/u after 3 - 6 months. What would you ask the patient. What would do for Physical Exam. What investigations would you do?
[diabetes] |
History:
- any urinary changes, blurry vision, energy levels, numbness or tingling sensation anywhere? - any hypoglycemic spells: confusion, sweating, tremors, chills, palpitations, seizures? - have you been monitoring your BG levels? how often? Taking meds regularly - currently smoking? If BP high ask: headaches, dizziness - diet, exercise - last time seen by ophthalmologist Physical exam: - Vitals: BP, weight, BMI, WC - CVS (N S1 and S2, any murmurs?) - Feet: sensation, pinprick, vibration sense, pulses, ulcers - Fundus (normal/abnormal) Investigations: - fasting blood sugars - fasting lipids: cholesterol, TG, LDL, HDL - microalbumin:creatinine ratio (yearly ECG if age>35, yearly urinalysis) - yearly eye exam (optometrist) |
|
|
What is the significance of albumin to creatinine ratio in diabetes?
|
- elevated levels indicated uncontrolled DM
- an indicator of subclinical CV disease - marker of vascular endothelial dysfunction - an important prognostic marker for kidney disease (in DM, HTN, post streptococcal glomerulonephritis) - a RF for venous thromboembolism |
|
|
What is a 'major' s/e of bisphosphonates?
|
severe esophagitis
|
|
|
What are the 2 most common causes of osteoporosis?
|
- post-menopausal decline in estrogen (worsens with age): most common cause
- corticosteroid therapy: second most common cause of osteoporosis. (note: individuals receiving ≥7.5 mg of prednisone daily for over 3 months should be assessed for bone-sparing therapy) |
|
|
Discuss the process of injecting a corticosteroid injection for a trochanteric bursitis?
|
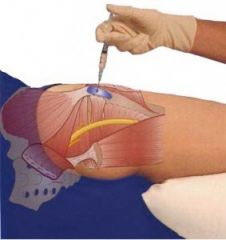
- draw up 3cc of lidocaine, then add 1cc of depomedrol into the same syringe
- clean area with chlorhexadine - insert 22 or 25G 1.5" needle perpendicular to pain of maximal pain all the way in and inject solution - if hit bone, then pull up slightly and then inject - if more disperse spread of pain, then pull needle up and go at an angle in a circular spread multiple times to cover a wider spread. |
|
|
Besides oral hypoglycemics and insulin, what are some other meds that are used in DM?
[diabetes] |
OTHER MEDS:
- ASA - for all diabetics unless contraindicated - Statins: as required to attain target lipid profile - ACEi: all HTsive patients with DM, elevated microalbuminuria (30-300mg albumin in 24h), overt nephropathy (>300mg albumin in urine in 24h). NOTE: ARBs are 2nd line for these conditions |
|
|
Is it right sided or left sided heart failure that is associated with hepatomegaly?
|
r sided heart failure
|
|
|
What is the definition of a recurrent urinary tract infection (uti)?
|
- 2 uncomplicated UTIs within 6 months OR
- ≥ 3 positive urine cultures in the prior 12 months |
|
|
Which disorders are strongly associated with osteoporosis?
|
|
|
|
note
|
In an elderly patient if there is no back pain midline, then the patient is unlikely to have a compression fracture. Must document specifics of back pain eg. lower right buttock.
NOTE: when doing a back exam on an elderly pt c/o of back pain, its important to check for midline back tenderness as they may have a compression fracture. |
|
|
What are the contraindications to metformin?
|
Contraindications (absolute):
- moderate to severe liver dysfunction - moderate renal dysfunction - cardiac dysfunction |
|
|
Triad of fatigue, SOB, and melena would make you suspicious of what?
|
Anemia (possible upper GI bleed)
|
|
|
A s/e of insulin is weight gain. T/F?
|
True
|
|
|
What are the pharmacological options for patients with osteoporosis?
|
otc
Ca 1200mg od Vit D 2000iu od ANTI-RESORPTIVE THERAPY - bisphosphonates (risedronate [actonel], alendronate [fosamax]) - monoclonal Ab (denosumab) - estrogen (1st line in women with menopausal Sx) - SERM (raloxifene) BONE FORMATION THERAPY - PTH (teriparatide) OTHER DRUGS - HRT - calcitonin NOTE: severe esophagitis is a major side effect of bisphosphonates |
|
|
What is a 1st line treatment for asymptomatic bacteriuria?
[urinary tract infection] |
EXCEPT during pregnancy and / or pre-op GU procedures, there are NO indications for screening or therapy for asymptomatic UTI (including the elderly)
------------------------------------------------------------------------- i. Macrobid 100 mg BID (contraindicated in pregnant patients at term (36-42 wks GA), during labour and in neonates due to the possibility of hemolytic anemia) ii. Amoxicillin 500mg TID - GU procedure: immediately before procedure and for its duration, unless there is an indwelling catheter present - Pregnancy: If positive, treat with 3-7d course therapy |
|
|
note
|
All men and women ≥ 65 should get bone mineral density testing.
|
|
|
What strengths does Anusol HC come in?
|
Its a combination steroid cream that is used for hemorrhoids.
0.5% - otc 1-2% - prescription (usually favor the 1% b/c area of thin skin) Prescription: anusol hc 1% cream apply to affected area tid and after bowel movement prn |
|
|
What are the clinical signs of fractures or osteoporosis?
|
1. height loss >3cm (Sn 92%)
2. weight <51 kg 3. kyphosis (Sp 92%) 4. tooth count <20 (Sp 92%) 5. grip strength 6. armspan-height difference > 5cm (Sp 76%) 7. wall-occiput distance >0cm 8. rib-pelvic distance ≤2 finger breaths (Sn 88%) |
|
|
What is a 1st line treatment for acute UTI in children?
[urinary tract infection] |
i. TMP/SMX 5-10mg/kg/day divided q12h x 7d
ii. Nitrofurantoin 5-7mg/kg/day divided q6h. Should not be used in infants <1mo of age; M: 7d NOTE: - in pss, when searching for septra, - type in "trimeth" and you'll see a suspension form --------------------------------------------------- |
|
|
A patient comes in w/ a urinary tract infection (uti) and she's allergic / does not tolerate macrobid. Write a prescription for a different antibiotic.
|
Septra (note in pss, you can't search for septra so you have to type it in manually as follows)
Prescription: Septra DS 1 tablet bid M: 5 days (even though guidelines say 3d) |
|
|
T/F. Nitrofurantoin is relatively contraindicated in renal impairment (CrCl < 60mL/min)
|
True
|
|
|
What is a Baker's cyst? How would you investigate it? What is the treatment for it?
|
A Baker's cyst, also known as a popliteal cyst, is a benign swelling of the semimembranous or more rarely some other synovial bursa found behind the knee joint. This is not a "true" cyst, as an open communication with the synovial sac is often maintained.
In adults, Baker's cysts usually arise from almost any form of knee arthritis (e.g. rheumatoid arthritis) or cartilage (particularly a meniscus) tear. They are posterior to the medial femoral condyle. A Baker's cyst can rupture and produce acute pain behind the knee and in the calf and swelling of the calf muscles. Diagnosis is by examination. A baker's cyst is easier to see from behind with the patient standing with knees fully extended. It is most easily palpated (felt) with the knee partially flexed. Diagnosis is confirmed by ultrasonography. A burst cyst can cause calf pain, swelling and redness that may mimic thrombophlebitis or a potentially life-threatening deep vein thrombosis (DVT) which may need to be excluded by urgent blood tests and ultrasonography. Baker's cysts usually require no treatment unless they are symptomatic. It is very rare that the symptoms are actually coming from the cyst. In most cases, there is another disorder in the knee (arthritis, meniscal tear, etc) that is causing the problem. Initial treatment should be directed at correcting the source of the increased fluid production. ----------------------------------------------------------------- Management (if symptomatic) i. rest ii. leg elevation iii. icing iv. nsaids (naproxen / vimovo) v. aspiration (if required) vi. corticosteroid injection vii. surgery (as a last resort) - orthopedic surgery |
|
|
For a pregnant patient that comes in with protein in urine, what is the most important thing to know?
|
What their BP is. Elevated BP could mean pre-eclampsia
Also would wanna know if: - any edema, h/a, blurry vision, n/v, lightheadedness |
|
|
T/F. LDL cannot be calculated reliably when TG>4.5
|
True
|
|
|
Which is a more common cause of sinusitis: viral or bacterial?
|
Viral
Viral: rhinovirus, influenza, parainfluenza Bacterial: s. pneumoniae, H. influenza, m. catarrhalis, anaerobes (dental) NOTE: - acute viral rhinosinusitis lasts <10d - if symptoms increase after 5d or persist >10d, then consider bacterial etiology |
|
|
When and how often should one screen for dyslipidemia?
|
Screening should be with full fasting lipid profile in males > age 40, females > 50 or who are menopausal, or any adults at any age with additional CAD RFs EVERY 1-3 years.
These RFs include: - diabetes - smoking - HTN - obesity - family hx of premature CAD - clinical signs of hyperlipidemia (xanthelasma, xanthoma, arcus cornealis) - evidence of atherosclerosis - rheumatoid arthritis, SLE, psoriasis - HIV infection on highly active antiretroviral therapy - chronic kidney disease (estimated GFR <60 ml/min - erectile dysfunction Screen children with a family hx of hypercholesterolemia or chylomicronemia note: other causes of dyslipidemia include: - hypothyroidism - alcohol abuse |
|
|
What is the most common organism involved in otitis externa?
|
Bacteria (~90% of otitis externa)
- most common organism is Pseudomonas, which is why otitis externa is treated w/ ciprodex. |
|
|
i. What is the 1st line antibiotic for mild/moderate acute prostatitis?
ii. What is the 1st line antibiotic for severe acute prostatitis? |
i. mild/moderate acute prostatitis
ciprofloxacin 500mg BID x 14d After 14d re-assess, once acute symptoms have resolved, an addition 2-4 wks of oral therapy (based on C+S) is indicated. If no / incomplete resolution of Sx after 6 wks of total treatment, a referral to urology is indicated. --------------------------------------------------------------------- ii. severe acute prostatitis These pts need to be admitted and treated with: - ampicillin IV 1-2g q4-6h PLUS gentamicin IV 6mg/kg q24h |
|
|
What is the 1st line antibiotic for epididymitis in someone who is > 35 years old? In someone who is ≤ 35 OR multiple sexual partners?
|
![>35 years old:
- ciprofloxacin 500mg BID x 14d
≤ 35 OR multiple sexual partners:
cefixime 800mg [single dose]
NOTE: May also give an anti-inflammatory for someone who comes in with epidydimitis (naproxen)
NOTE: epididymitis can be secon...](https://images.cram.com/images/upload-flashcards/67/11/98/2671198_m.jpg)
>35 years old:
- ciprofloxacin 500mg BID x 14d ≤ 35 OR multiple sexual partners: cefixime 800mg [single dose] NOTE: May also give an anti-inflammatory for someone who comes in with epidydimitis (naproxen) NOTE: epididymitis can be secondary to prostatitis and may require up to 6 wks of therapy. If after 6 wks Sx persist, a refer to urology is indicated. |
|
|
What is the 1st line antibiotic for trichomoniasis vaginitis?
|
metronidazole 2g [single dose]
NOTE: must treat partners as this is sexually transmitted NOTE: treatment is NOT recommended for asymptomatic pregnant women |
|
|
What is rhinitis medicamentosa?
|
- result of long term topical nasal decongestant abuse
- loss of vasomotor tone so nasal mucosa is swollen, with clear rhinorrhea - rebound swelling of mucosa when topical decongestant is stopped - if abuse continues, nasal mucosa becomes thin, irritated, red, and may bleed - Treatment: stop the abuse: sometimes saline/topical steroid helps the patient while they are trying to break this habit - if not successful and late stage disease occurs then nasal hydration with saline sprays and ointments is all we have to offer them |
|
|
T/F. Pulling on the pinna is extremely painful in otitis externa, but is usually well tolerated in otitis media.
|
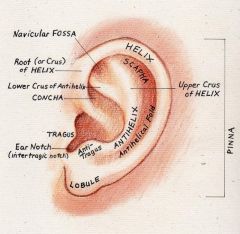
True
In otitis externa, pulling on the pinna and pushing on the tragus is painful. |
|
|
What is the 1st line antibiotic for bacterial vaginosis?
|
ASYMPTOMATIC PATIENTS:
- Treatment is unnecessary unless high risk pregnancy (eg. prior pre-term delivery), prior to IUD insertion, gynecological surgery, induced abortion, or upper tract instrumentation SYMPTOMATIC PATIENTS: - metronidazole 500mg BID x 7d NOTE: no treatment is needed for male sexual partner |
|
|
What is neurodermatitis / pathological skin picking (PSP)?
|
Pathologic skin picking (PSP) is the repetitive manipulation of the skin, with or without instrumentation, resulting in visible tissue damage and impairment in social functioning. Patients with PSP may present with features of impulse control disorder, obsessive compulsive disorder, or both. Multiple psychiatric comorbidities are associated with PSP, including depression, bipolar disorder, obsessive compulsive disorder, alcohol abuse or dependance, and trichotillomania.
PSP appears as excoriated, polymorphic lesions of variable size in all stages of evolution, localized most frequently on the face. PSP should be differentiated from the excoriations seen in subgroups of patients with primary pruritic skin conditions, chronic pruritus associated with systemic diseases, or other psychocutaneous diseases. Psychiatric referral is appropriate for patients with PSP, although many patients will not accept it. Patients with PSP should be either comanaged by a mental health specialist and dermatologist, or managed by a specialist who has experience in both psychiatric and dermatologic disorder. For patients with associated intense pruritus, we suggest POTENT topical corticosteroids or intralesional triamcinolone acetonide (Grade 2C). For patients with acne excoriée, aggressive treatment of the underlying acne should be initiated. Patients with skin infections should be treated with topical and/or systemic antibiotics. We suggest pharmacotherapy for patients with skin picking behavior whose severity interferes with daily functioning (Grade 2C). When pharmacotherapy is selected for the treatment of PSP, we suggest an SSRI antidepressant (Grade 2C). Evidence is limited, but we typically initiate treatment with fluoxetine 20 mg per day, titrating the dose up every two to four weeks as needed and tolerated. In patients presenting with features of delusional disorder, antipsychotic medications are indicated. Pimozide or olanzapine are options, but have only been reported in case studies. For patients accepting mental health professional referral, we suggest cognitive behavioral-therapy or habit reversal therapy (Grade 2C). In summary medical management includes: i. potent steroid (elocom 0.1% / topicort 0.25%) ii. ssri (fluoxetine 20mg, titrate q2wks as tolerated iii. cbt iv. specialist involvement: psychiatry / dermatology |
|
|
If you are prescribing someone with osteoporosis and bone pain Calcitonin, what dose and how often should be patient be taking it?
|
Prescription:
Calcitonin-salmon nasal spray - 200 units/spray 1 spray in one nostril od x 1 month (may switch to bisphosphonates such as actonel earlier if pain abates) -------------------------------------------------- NOTE: calcitonin is mainly used for acute bone pain in a pt w/ osteroporosis. It should not be used long term as it is: - expensive - ++ s/e including n/v, flushing - develop resistance - better alternatives for osteoporosis are present (actonel/fosamax) |
|
|
T/F. The oral contraceptive pill is contraindicated with complicated migraine due to risk of stroke
|
True
|
|
|
Write a steroid cream prescription for a patient who comes in with neurodermatitis on the arms?
|
Use moderate potency topical steroid
- Elocom 0.1% apply to affected areas od M: 60g - if this does not work, try - Topicort 0.25% cream: apply to affected areas bid M: 60g |
|
|
Discuss the role of calcitonin. What are its indications?
|
Calcitonin is a valid option for the therapy of established osteoporosis, since it increases spine bone density and may decrease vertebral fracture risk. It is especially attractive when back pain is a problem. It is not usually used as first-line therapy because of its expense, the relative inconvenience of nasal or parenteral administration, frequent side effects, and the possible development of resistance. In addition, more effective drugs are available for prevention of bone loss and reduction of fracture risk (bisphosphonates - actonel/fosamax)
We often administer calcitonin if pain from an acute osteoporotic fracture is a prominent problem, and then switch to other agents such as bisphosphonates once the pain has abated. -------------------------------------------------------------------------------------- Calcitonin binds to osteoclasts and inhibits bone resorption. Calcitonins from many species are effective in humans, but salmon calcitonin is the one most widely used. It has 40 times the affinity of human calcitonin and is much more potent. The administration of salmon calcitonin frequently is associated with side effects such as nausea, vomiting, and flushing; these side effects are much less common with the nasal route. Calcitonin has a beneficial short-term effect on acute pain relief in patients who have sustained a vertebral fracture, as illustrated by the findings of a meta-analysis of 10 trials comparing calcitonin (nasal or parenteral) with placebo in patients with acute (onset <10 days) or chronic (>3 months) pain due to an osteoporotic compression fracture. Calcitonin was not effective for patients with chronic pain. The main concern about treatment with calcitonin is that more effective drugs (eg, bisphosphonates) are available for the prevention of bone loss and reduction of fracture risk. |
|
|
Discuss the immunization schedule by age.
|
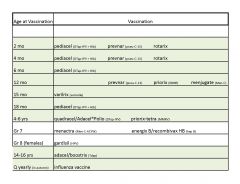
|
|
|
What is a 1st line treatment for Acute cystitis in Pregnant women?
|
i. Macrobid 100mg BID x 5d (contraindicated in pregnant patients at term (36-42 wks GA), during labour and in neonates due to the possibility of hemolytic anemia)
ii. Cephalexin 500mg QID x 7d |
|
|
What is encopresis ?
|
Encopresis (aka paradoxical diarrhea) is involuntary fecal soiling in adults and children who have usually already been toilet trained. Persons with encopresis often leak stool into their undergarments.
|
|
|
Treatment for urinary tract infection (uti) in Nursing Home / LTC patients?
|
macrobid 100mg BID x 7d (relatively contraindicated in patients with renal impairment, i.e. CrCl <60mL/min)
|
|
|
What investigations would you do for a patient with sinusitis?
|
- usually don't do any investigations as it is a clinical diagnosis
- x rays are warranted only when the diagnosis of sinusitis is in doubt - CT scans are not cost-effective and should not be used routinely to diagnosis sinusitis. |
|
|
note
|
B12 is as important as folate in preventing neural tube defects. Normal b12 as per CFFM's bw is considered levels >300.
|
|
|
What is characterized as a complicated urinary tract infection (uti)? Which antibiotic is appropriate for these patients?
|
Complicated UTI includes patients with:
structural abnormalities: - solitary kidney, polycystic kidney(s) - duplicated collecting system - vesicoureteral reflux - recent instrumentation, catheter use, ureteral stent - pyelonephritis obstruction - ureteral obstruction (tumor, fibrosis, stricture) - enlarged prostate - neurogenic bladder - calculi medical - immunocompromised (incl. dm, ckd) - recent hospitalization/nursing home male sex ------------------------------------------------------------ Mild to moderate lower tract (bladder) - ciprofloxacin 500mg bid M:7d (7-10) Upper tract (kidney) or systemic (high fever, sepsis, vomiting): - ciprofloxacin 500mg bid M:10d (10-14) ------------------------------------------------------------- Severe: - ampicillin IV 1g q6h plus gentamicin IV 6mg/kg q24h |
|
|
What is the 1st line treatment for uncomplicated, non-obstructed, mild pyelonephritis?
|
Ciprofloxacin 500mg BID x 7d (7-10)
|
|
|
What are some signs of hyperlipidemia?
|
i. atheromata: plaques in blood vessel walls
ii. xanthoma: yellow plaques or nodules in the skin especially eyelids iii. tendinous xanthoma: lipid deposit in tendon (esp. Achilles) iv. corneal arcus: lipid deposit in cornea |
|
|
Which class of antibiotics should not be used in otitis externa if there is a perforation of the TM?
|
Aminoglycosides such as gentamycin because of risk of ototoxicity.
|
|
|
What are the headache red flags?
|
- sudden onset of severe h/a
- worst h/a ever - new h/a after age 50 - h/a present on awakening - impaired mental status - fever - neck stiffness - seizures - focal neurological deficits - jaw claudication - scalp tenderness - worse with exercise, sexual activity or valsalva |
|
|
What is the 1st line antibiotic for vulvovaginitis candidiasis (VVC)?
|
ORAL
fluconazole 150mg capsule 1 tablet po M: 1 capsule CREAM clotrimazole (canestan) 10% cream one applicatorful intravaginally [single dose] |
|
|
What is intermittent claudication?
|
Patients with compromised blood flow to the extremities as a consequence of peripheral artery disease (PAD) may present with pain of one or more muscle groups, atypical pain or no symptoms. Intermittent claudication is defined as a reproducible discomfort of a defined group of muscles that is induced by exercise and relieved with rest. This disorder results from an imbalance between supply and demand of blood flow that fails to satisfy ongoing metabolic requirements.
---------------------------------------------------- DDx for Claudication: VASCULAR - artherosclerotic disease (most common) - vasculitis - diabetic neuropathy - venous disease (DVT, varicose veins) - popliteal entrapment NEUROLOGIC - neurospinal disease (eg. spinal stenosis) - reflex sympathetic dystrophy MSK - osteoarthritis - RA/connective tissue disease - remote trauma |
|
|
For a patient with Achilles tendonitis, which physical exam manoeuvres would reproduce pain?
|
- palpation of Achilles tendon
- resisted dorsiflexion |
|
|
What is de Quervain's tenosynovitis?
|
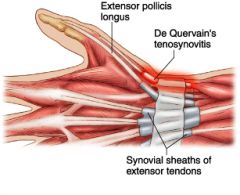
de Quervain’s tenosynovitis is a tendonitis of 2 thumb tendons that 1. help move the thumb sideways and 2. help move the thumb backwards.
|
|
|
What are some of the tests you can do for diagnosing de Quervain's tenosynovitis
|
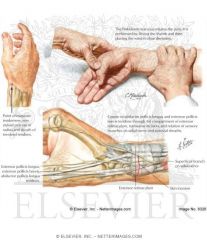
i. pain on palpation of tendon sheath
ii. finklestein's test |
|
|
If an 80 year old man comes in with midline lower back pain, what is the most important thing to rule out?
|
- r/o compression fracture
- must do an xray (ap and lateral in this case); also check to see if bmd is up to date note: lateral allows for better visualization of compression fractures |
|
|
How do you distinguish between mechanical back pain vs. sciatica?
|
Sciatic pain typically radiates with numbness and tingling all the way down to the foot. Pain that is localized above the knee may be either mechanical back pain or sciatic pain.
|
|
|
What is sciatica? What is the typical distribution of sciatic type pain (see picture).
|

Sciatica is a set of symptoms including pain caused by general compression or irritation of one of five spinal nerve roots of each sciatic nerve—or by compression or irritation of the left or right or both sciatic nerves. Symptoms include lower back pain, buttock pain, and pain, numbness or weakness in various parts of the leg and foot. Other symptoms include a "pins and needles" sensation, or tingling and difficulty moving or controlling the leg. Typically, symptoms only manifest on one side of the body. The pain may radiate below the knee, but does not always.
|
|
|
What are the 3 most common infections associated with vaginal discharge in adult women?
|
1. bacterial vaginosis (rx w/ flagyl 500mg bid x 7d)
2. vulvovaginal candidiasis (rx w/ fluconazole 150mg x 1; canestan cream; monistat cream) 3. trichomoniasis (sexually transmitted) (rx w/ flagyl 2g x 1) |
|
|
If a patient does have a compression fracture, what meds do they need to be on?
|
- bisphosphonates
- calcitonin (good for pain + osteoporosis) - pain meds as needed |
|
|
What are some predisposing factors for HTN?
|
- family history
- obesity (especially abdominal) - alcohol consumption - stress - sedentary lifestyle - smoking - male gender - age > 30 - excessive salt intake/fatty diet - African American ancestry - dyslipidemia |
|
|
If you're concerned about a patient blood pressure elevated and you would like to check it a month later, How should you measure it?
|
Consider getting a BP true (i.e. 5 readings, then avg is taken, considered very accurate)
|
|
|
A baby presents with diaper dermatitis (candida). What would you treat this baby with?
|
Topical nystatin cream
Prescription: Nystatin 100,000 units/g cream Apply to affected areas bid M:30g R:1 |
|
|
Which is the ideal drug to give for patients with acute symptomatic shingles?
|
valtrex (valacyclovir) 1000mg po tid x 7d
- works for severe pain and ophthalmic involvement Other drugs: [famcicyclovir and acyclovir] x 7d |
|
|
Explain what the following drugs do and how they work:
- salbutamol (ventolin) - flovent, pulmicort - salmeterol - advair - atrovent - spiriva |
Salbutamol (ventolin) or albuterol (ventolin) is a short-acting β2-adrenergic receptor agonist used for the relief of bronchospasm in conditions such as asthma and chronic obstructive pulmonary disease.
Fluticasone (Flovent), Budesonide (Pulmicort) are inhaled corticosteroids. The combination of fluticasone and salmeterol as Advair. Salmeterol is a long acting b-agonist used for maintenance treatment (prevention of bronchospasm in COPD, asthma) Advair - combination long acting b-agonist (salmeterol) and inhaled corticosteroid (flovent) Atrovent - aka ipratropium bromide: anticholinergic (short acting) that acts as a bronchodilator in COPD, bronchitis, and emphysema Spiriva aka tritropium bromide: anticholinergic (long acting) that acts as a bronchodilator in COPD, bronchitis and emphysema |
|
|
What are some triggers for migraines?
|
- food
- sleep disturbance - stress - weather - hormonal - alcohol - AGGRAVATED by physical activity |
|
|
What is the treatment for hand foot and mouth disease?
|

Conservative management and symptomatic control
- lots of fluids - tylenol for fever/sore throat - good hygiene - should recover in 3-7 days |
|
|
What is the emergency management of asthma?
|
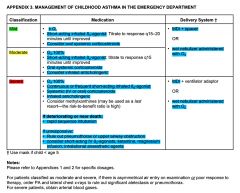
|
|
|
What is the criteria for determining if asthma is well controlled?
|
1. daytime symptoms <4x/wk
2. night time symptoms <1x / wk 3. normal physical activity 4. mild, infreq exacerbations 5. no asthma related absense from work/school 6. B2 agonist used <4x / wk |
|
|
What is hand foot and mouth disease?
|

Hand, foot and mouth disease (HFMD) is a human syndrome caused by intestinal viruses of the picornaviridae family (most common viruses to cause HFMD are the coxsackie A virus and enterovirus).
HFMD usually affects infants and children, and is quite common. It is moderately contagious and is spread through direct contact with the mucus, saliva, or feces of an infected person. It typically occurs in small epidemics in nursery schools or kindergartens, usually during the summer and autumn months. It is less common in adults, but those with immune deficiencies are very susceptible. The usual incubation period is 3–7 days. SYMPTOMS of HFMD include: - fever - h/a - sore throat - vomiting - referred ear pain - painful oral, nasal, or facial lesions, ulcers, or blisters - non pruritic rash with sores and blisters on the palms of hands, soles of feet, and sometimes on the lip; sometimes buttocks (but usually due to diarrhea) - irritability - loss of appetite - diarrhea Early symptoms include fever often followed by a sore throat |
|
|
What are some investigations that can be done in a patient with asthma?
|
- O2 sat
- CXR - ABGs - PFTs |
|
|
What are some of the triggers in asthma?
|
- stress
- heat/cold - allergies - URTI - allergens (pets, carpets) - irritants (cigarette smoke) - drugs (NSAIDs, B-blockers) |
|
|
What are some symptoms of anemia?
|
- fatigue, weakness, exercise intolerance
- syncope, palpitations, H/A, postural dizziness - dyspnea - irritability - feeling cold - confusion/loss of concentration - pallor - brittle hair, brittle nails (may have koilonychia (spoon-shaped) |
|
|
What is asthma?
|
- chronic inflammatory disorder of the airways resulting in reversible bronchospasm causing airflow obstruction
Characterized by: - dyspnea - wheezing - chest tightness - sputum production - cough (especially noturnal) May present with respiratory distress: nasal flaring, assessory muscle use |
|
|
What are the signs/symptoms of candida on the breast?
|
- very sore nipples, with burning, itching, or redness
- shooting pains in the breasts during feeding - shiny or flaky skin around the nipples |
|
|
A patient comes to the office c/o whitish coloration of the tongue. What is the most likely diagnosis? How would you treat it?
|

oral candidiasis
oropharyngeal candidiasis is a local infection of: - older adults who wear dentures - patients treated with antibiotics, steroids (puffers), chemotherapy, or radiation therapy to the head and neck, - pts w/ cellular immune deficiency states, such as AIDS. ------------------------------------------------- Rx 1. nystatin (oral); failure of this --> 2. fluconazole (systemic) Prescriptions: 1. nystatin 100,000u/ml 6mL qid x 10 days note: Nystatin should be swirled inside mouth for a little while before swallowing. 2. fluconazole 100mg 2 tablet on day 1; thereafter, 1 tablet od M: 14 days |
|
|
Describe the guidelines for asthma management?
|
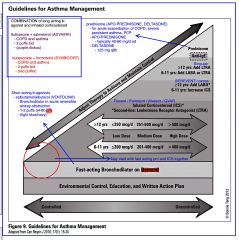
|
|
|
What is the DDx of asthma?
|
asthma
copd CHF bronchiectasis mechanical obstruction of airways |
|
|
Compare the inhaled corticosteroids divided in mild, moderate, and high doses.
|
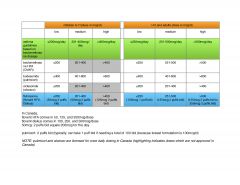
|
|
|
What is flovent and write a prescription for it.
|
Flovent is an inhaled corticosteroid
Prescription Flovent HFA 50mcg(or 125mcg depending)/spray 2 puffs bid M: 1 device |
|
|
What is the management for an ingrown toe nail?
|
- advise patient to allow toe nail to grow and cut more horizontally.
- pain meds as needed - if signs of infection (erythema, discharge, pus), then dip in warm water - if severe infection, patient can apply Polysporin bid x 7 days or come back for further assessment |
|
|
What is dyspepsia?
|
Dyspepsia, also known as upset stomach or indigestion, refers to a condition of impaired digestion. It is common and is often assoc. with GERD or gastritis. In a small minority it may be the first symptom of peptic ulcer disease (an ulcer of the stomach or duodenum) and occasionally cancer. Hence, unexplained newly onset dyspepsia in people over 55 or the presence of other alarming symptoms may require further investigations.
Defined as one or more the following symptoms: - postprandial fullness / bloating - early satiety - epigastric pain or burning - (some definitions include heart burn) - (can be accompanied by nausea) - Functional dyspepsia (previously called non-ulcer dyspepsia) is dyspepsia without evidence of an organic disease that is likely to explain the symptoms |
|
|
A pt comes in w/ Sx of dyspepsia....i.e. epigastric discomfort, burning, early satiety, postprandial bloating. What are the causes/ddx of dyspepsia?
|
Approximately 25 percent of patients with dyspepsia have an underlying organic cause. However, up to 75 percent of patients have functional (idiopathic or nonulcer) dyspepsia with no underlying cause on diagnostic evaluation.
Organic etiology (not limited to): - peptic ulcer disease (nsaid, h.pylori, stress induced) - gerd - gastroparesis (delayed stomach emptying) - biliary pain - pancreatitis - esophageal / stomach Ca - chr. abdo wall pain - stemi, other cardiac causes - meds including: oral abx, nsaids, narcotics, glucocorticoids NOTE: --> h. pylori tests include serology and urea breath test NOTE: better to check serology first b/c urea breath test can be more involving |
|
|
If a patient complains that they've gained +5 lbs in the past one week. Assuming this patient has a hx of CHF, what is one quick way to confirm that they're retaining fluids?
|
Weigh them and see if that has changed from the previous measure.
|
|
|
When a patient comes in with symptoms of CHF such as shortness of breath and swollen legs. What is a quick method of assessing how much fluid they may be retaining?
|
You can weigh them and check their previous weight
|
|
|
What are the contraindications of bupropion (zyban/wellbutrin)?
|
- seizure disorder (bupropion lowers seizure threshold; therefore good idea to ask about alcohol abuse --> more likely to get seizures with alcohol withdrawal)
- eating disorder (b/c of inc. risk of seizures due to electrolyte imbalances) - MAOI use in the past 14d note: bupropion is used for: i. smoking cessation ii. depression |
|
|
Which drug is more effect in terms of smoking cessation?
Bupropion or Varenicline (Champix)? |
Varenicline (Champix)
However in pregnancy only bupropion should be used between the 2. This is b/c the safety of varenicline has not been studied in pregnancy Also Varenicline should be used with caution in patients with pre-existing psychiatric condition. One major s/e of varenicline is night terrors. |
|
|
T/F. The most common cause of dyspepsia if 'functional' (idiopathic) dyspepsia
|
True
|
|
|
note
|
there is no need to do mammography in patients > 75
|
|
|
T/F. Any patient who gets has a negative xray of the wrist but has tenderness in the snuffbox, should be treated as if they have a scaphoid fracture.
|
True
|
|
|
T/F. If a patient is at high risk for developing ulcers, then prophylaxis with PPI is indicated
|
True
|
|
|
T/F. NSAIDs are more likely to cause gastric ulcers than duodenal ulcers
|
True
|
|
|
If a patient comes in with wrist injury, what is the one thing you have to r/o?
|

- must r/o tender snuff box b/c that could be a scaphoid fracture.
This is very bad, as the thumb can die (due to lack of blood supply) |
|
|
What are the guidelines for stable COPD management?
|
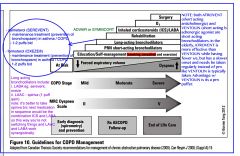
|
|
|
What are main risk factors in developing peripheral artery disease?
|
- cigarette smoking (most important RF)
- DM - HTN - hyperlipidemia |
|
|
What are some complications that can arise from GERD?
|
- esophageal strictures (scarring can lead to dysphagia (solids))
- ulcer - bleeding - Barrett's esophagus - esophageal carcinoma |
|
|
T/F. Gabapentin should be used with caution in patients who have poor renal function?
|
True
|
|
|
What are the pharmacological options for acne?
|

|
|
|
What is one OTC cream product for acne treatment?
|
Proactiv (has a component of benzoyl peroxidase)
|
|
|
What is the difference between nociceptive vs neuropathic pain?
|
1. NOCICEPTIVE PAIN - Examples include sprains, bone fractures, burns, bumps, bruises, inflammation (from an infection or arthritic disorder), obstructions, and myofascial pain (which may indicate abnormal muscle stresses).
Nociceptors are the nerves which sense and respond to parts of the body which suffer from damage. They signal tissue irritation, impending injury, or actual injury. When activated, they transmit pain signals (via the peripheral nerves as well as the spinal cord) to the brain. The pain is typically well localized, constant, and often with an aching or throbbing quality. Visceral pain is the subtype of nociceptive pain that involves the internal organs. It tends to be episodic and poorly localized. Nociceptive pain is usually time limited, meaning when the tissue damage heals, the pain typically resolves. (Arthritis is a notable exception in that it is not time limited.) Another characteristic of nociceptive pain is that it tends to respond well to treatment with opioids. 2. NEUROPATHIC PAIN - Examples include post herpetic (or post-shingles) neuralgia, reflex sympathetic dystrophy / causalgia (nerve trauma), components of cancer pain, phantom limb pain, entrapment neuropathy (e.g., carpal tunnel syndrome), and peripheral neuropathy (widespread nerve damage). Among the many causes of peripheral neuropathy, diabetes is the most common, but the condition can also be caused by chronic alcohol use, exposure to other toxins (including many chemotherapies), vitamin deficiencies, and a large variety of other medical conditions--it is not unusual for the cause of the condition to go undiagnosed. Neuropathic pain is the result of an injury or malfunction in the peripheral or central nervous system. The pain is often triggered by an injury, but this injury may or may not involve actual damage to the nervous system. Nerves can be infiltrated or compressed by tumors, strangulated by scar tissue, or inflamed by infection. The pain frequently has burning, lancinating, or electric shock qualities. Persistent allodynia, pain resulting from a nonpainful stimulus such as a light touch, is also a common characteristic of neuropathic pain. The pain may persist for months or years beyond the apparent healing of any damaged tissues. In this setting, pain signals no longer represent an alarm about ongoing or impending injury, instead the alarm system itself is malfunctioning. Neuropathic pain is frequently chronic, and tends to have a less robust response to treatment with opioids, but may respond well to other drugs such as anti-seizure and antidepressant medications. Usually, neuropathic problems are not fully reversible, but partial improvement is often possible with proper treatment. |
|
|
What is the biggest complication of a scaphoid fracture?
|
Avascular necrosis; patient may eventually suffer from arthritis.
|
|
|
When should one be cautious about using nicotine replacement therapy (NRT)?
|
- immediate post-MI
- serious/worsening angina - serious arrhythmia -------------------------------------------------------------------- note: nicotine: - It increases the heart rate - It causes the heart muscle cells to squeeze harder with each beat - It causes blood vessels in the heart to constrict to a smaller diameter All of these effects are temporary, however, because a person's body quickly becomes tolerant to the effects of nicotine; this is why nicotine is one of the most highly addictive substances known. Because of this tolerance to nicotine, for someone who chews tobacco regularly, the long-term heart effects are probably minimal. |
|
|
What are some withdrawal symptoms of cigarette smoking?
|
low mood
insomnia irritability anxiety difficulty concentrating restlessness decreased HR increased appetite |
|
|
Should pregnant women be smoking? If not what are some ways to help her quit?
|
NO
- advise to quit w/o pharmacotherapy (+/- counseling) - if that does not work, then nicotine replacement therapy (NRT) in the form of patches should be made available - Use bropropion (no evidence of fetal or reproductive harm) - Do not use varenicline (champix) as it has not been studied in pregnancy; therefore should not be used by pregnant women. |
|
|
What is the treatment for H. pylori eradication?
|
Prescription:
Hp-pac kit (includes lansoprazole 30mg, amoxicillin 500mg(x2), clarithromycin 500mg) M: 7 days -------------------------------------------------------------------------------- i. lansoprazole 30mg bid ii. amoxicillin 1g bid iii. clarithromycin 500mg bid *confirmation of eradication is required for complicated (bleeding, perforation, stricture) or refractory ulcers, but is controversial after the medical management of uncomplicated ulcers in pts who remain asymptomatic. |
|
|
What should you warn pts about who are being treated with metronidazole (flagyl)?
|
NOT to take alcoholic beverages during treatment w/ metronidazole and for 48h post-treatment to prevent disulfiram-like reaction.
A disulfiram like reaction means that the alc. dehydrogenase enzyme is inhibited thereby preventing the enzyme acetaldehyde dehydrogenase thereby leading to the accumulation of high levels of acetaldehyde. This makes the pt feel like they're having a hangover w/ symptoms of: flushing of the skin, accelerated heart rate, shortness of breath, nausea, vomiting, throbbing headache, visual disturbance, mental confusion, postural syncope, and circulatory collapse. |
|
|
What is an upper GI series (aka barium swallow)?
|

Upper GI series, also upper gastrointestinal (GI) tract radiography, is a radiologic examination of the upper gastrointestinal tract. It consists of a series of X-ray images of the esophagus, stomach and duodenum. The most common use for this medical testing is to look for signs of ulcers, acid reflux disease, uncontrollable vomiting, or unexplained blood in the stools (hematochezia or positive fecal occult blood).
This is a non-invasive test, consisting of an X-ray. In the X-ray room, the patient is given two medications to drink that help improve the quality of the resulting X-rays. The patient may also be administered glucagon, a pancreatic hormone that is injected intravenously. The first drink is very carbonated, made from baking-soda crystals which expands the stomach by causing gas to build in the stomach. The second drink is a contrast agent, typically a thick, chalky liquid containing a barium salt. (This test is sometimes called a barium swallow.) The barium outlines the stomach on the X-rays, helping the doctor find tumors or other abnormal areas. The patient then has X-rays taken. The doctors usually take a series of pictures with the patient in a number of different positions to capture different poses and views of the digestive system. Normally the patient needs to hold their breath to avoid the pictures from blurring and causing unneeded challenges in diagnosing the illness. |
|
|
What are the most common causes of chronic cough in healthy-appearing patients (cough > 3 months with normal CXR)?
|
The most common chronic causes are:
i. gerd ii. asthma iii. post-nasal drip iv. post-viral v. ACEi ------------------------------------------------------ Other causes of cough include: 1. A/W irritants: smoke, dust, fumes, allergens 2. A/W disease: COPD, neoplasm, bronchiectasis, acute/chronic bronchitis, URTI 3. Parenchymal disease: pneumonia, lung abscess cancer 4. Cardiac: CHF |
|
|
What is the management for epicondylitis (tennis and golf elbow)?
|
- activity modification (avoid aggravating activity)
- NSAIDs (regularly for first few days then prn) - Icing: 4 x 15 mins / day - physiotherapy |
|
|
A young 17 yr old patient comes in to your office complaining of anger (for no reason towards parents) and depression. Anger > depression. What would be your management approach?
|
1. lifestyle:
- sleep - exercise - diet (omega 3 fatty acids) 2. counselling (CBT) (ask if they have coverage, if not the CFFM can provide 8 free sessions) 3. Medications such as SSRIs. (This is the 3rd step b/c once a patient is put on SSRIs, they're committed to about 1 year, and SSRIs are not without S/Es) |
|
|
If a patient comes into the office complaining of "spacing out", losing focus, getting confused, after trauma to the head (and probable concussion), What advise would you give them beside pain management?
|
This pt probably has post-concussion syndrome.
ADVISE: - AVOID physical and mental stimulation. - they should not even read or watch TV till they get better. B/c any mental exertion can worsen their symptoms. *note: you can monitor sx of post-concussion syndrome using the SCAT2 tool |
|
|
Is there a vaccine for the prevention of shingles? If so what is it?
|
Zostavax [indicated for patients 50 and above]. Since most people >50 have had chicken pox, they are all at risk of developing shingles.
Zostavax is a live vaccine developed by Merck & Co. that has been shown to reduce the incidence of herpes zoster (known as shingles) by 51.3% in a study of 38,000 adults aged 60 and older who received the vaccine. The vaccine also reduced by 66.5% the number of cases of postherpetic neuralgia and reduced the severity and duration of pain and discomfort associated with shingles, by 61.1%. Local reactions at the injection site were generally mild. NOTE: tell pts that risk of getting shingles is 1 in 3 and zostavax cuts the risk in half. NOTE: Zostavax is not covered typically and costs about $200-250. Also it needs to be kept below a certain temperature to remain effective. |
|
|
What is the most common cause of hemoptysis (coughing blood)?
|
Bronchitis
|
|
|
What are some of the causes of pruritis (itch)?
|
Dermatological
- xerosis (dry skin) - atopic dermatitis - psoriasis - cutaneous infections - cutaneous T-cell lymphoma Systemic - chronic renal failure - liver disease - hematologic or proliferative disease - malignancy Neurologic - MS Psychogenic - depression - anxiety - psychogenic excoriation |
|
|
Describe the signs and symptoms of shingles?
|

The earliest symptoms of herpes zoster, which include headache, fever, and malaise, are nonspecific, and may result in an incorrect diagnosis. These symptoms are commonly followed by sensations of burning pain, itching, hyperesthesia (oversensitivity), or paresthesia ("pins and needles": tingling, pricking, or numbness). The rash and pain may be on separated areas of the body, innervated by the same nerve. The pain may be mild to extreme in the affected dermatome, with sensations that are often described as stinging, tingling, aching, numbing or throbbing, and can be interspersed with quick stabs of agonizing pain.
Herpes zoster in children is often painless, but older people are more likely to get zoster as they age, and the disease tends to be more severe. In most cases after 1–2 days, but sometimes as long as 3 weeks, the initial phase is followed by the appearance of the characteristic skin rash. The pain and rash most commonly occurs on the torso, but can appear on the face, eyes or other parts of the body. At first the rash appears similar to the first appearance of hives; however, unlike hives, herpes zoster causes skin changes limited to a dermatome, normally resulting in a stripe or belt-like pattern that is limited to one side of the body and does not cross the midline. Zoster sine herpete ("zoster without herpes") describes a patient who has all of the symptoms of herpes zoster except this characteristic rash. Later the rash becomes vesicular, forming small blisters filled with a serous exudate, as the fever and general malaise continue. The painful vesicles eventually become cloudy or darkened as they fill with blood, crust over within seven to ten days; usually the crusts fall off and the skin heals, but sometimes, after severe blistering, scarring and discolored skin remain. |
|
|
T/F. Pain from postherpetic neuralgia can be chronic.
|
True
Pain may persist or recur for months, years, or for life |
|
|
What are 2 good community resources that can help children with development disabilities (including speech) in the KW region?
|
1. Kidsability (about a 6 month wait)
2. BlueBalloon |
|
|
Distinguish between the symptoms of peripheral arterial/vascular disease (PAD) and peripheral venous disease/insufficiency?
|
In PAD, patients get intermittent claudication (pain) with exertion.
In vascular insufficiency, patients get edema of the extremities (usually legs). |
|
|
List 2 skeletal muscle relaxants?
|
Prescription meds:
- Flexiril (NOT covered by ODB) - Baclofen (covered by ODB) OTC meds: - Robaxacet --------------------------------------------- Prescription for Flexeril: Flexiril 10mg 1 tablet qhs prn M: 15 tablets Prescription for Baclofen: Baclofen 5mg 1 tablet tid prn M: 30 tablets [max per day 80mg] |
|
|
note: Contact dermatitis and herpes zoster can present very similarly. What is big difference between the 2 ?
|
The biggest difference is that you have ++ pain with herpes zoster, not so much with contact dermatitis.
|
|
|
T/F. Population based routine screening for PSA is not recommended; instead asymptomatic screening must be an informed decision.
|
True
One can offer baseline PSA screening to men at 40 with at least 10 yrs life expectancy, especially if at high risk (family hx, African descent) |
|
|
If someone is having unstable angina, where would you refer her for further testing?
|
These pts will need a stress test at either:
CardioPulmonary Services (KW) Cambridge cardiac care centre (Cambridge) - Dr. Pandey |
|
|
note
|
When a baby comes in with oral thrush, it is important to r/o if the mother has the infection on her breasts, i.e. cracked nipples. If the mother is feeding the baby, she may have the candida infection as well, so you have to make sure that both the baby and the mother have the medication (that is nystatin).
Nystatin - topical antifungal - not absorbed systemically Prescription: Nystatin 100,000/mL suspension orally 1mL qid M: 7 days note: it is best to treat the mum as well, because she may have thrush on the nipple(s) and can pass it on to the baby after it's treated. Prescription (mum): Nystatin 100,000 units/gram cream apply tid x 7 days M: 15 grams |
|
|
What is baclofen?
|
a skeletal muscle relaxant (prescription). It is covered by odb whereas flexiril is not
Prescription Baclofen 10mg 1 tablet tid prn M: 30 tablets |
|
|
What are the 2 most important blood tests to order for biliary colic?
|
i. bilirubin
ii. amylase |
|
|
What are 4 risk factors for gallbladder stones (cholelithiasis)?
|
4F's
fat female fertile forties |
|
|
Categorize the following: cholelithiasis, biliary colic, cholecystitis, choledocholithiasis, cholangitis with regards to being asymptomatic, pain only, or pain + infection?
|
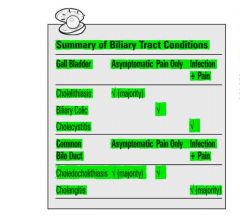
|
|
|
_________________ is the diagnostic procedure of choice for imaging the biliary tree.
|
abdominal ultrasound
|
|
|
What are the clinical features of gallstones (cholelithiasis) and what might they present as?
|

|
|
|
What is the common bile duct? What is it called when a gallstone is present in the common bile duct.
|
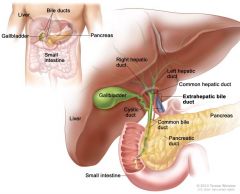
The common bile duct is where the cystic duct and common hepatic duct lead into.
A gallstone lodged in this duct is called choledocholithiasis. |
|
|
T/F. Biliary pain is a constant pain NOT colicky.
|
True. Colicky pain is severe, often fluctuating pain in the abdomen. Biliary colic is non-colicky pain. Biliary colic is constant pain.
|
|
|
What is cholelithiasis?
|
formation of gallstones
|
|
|
What investigations can be done for gallstones?
|
- bw_abdo set typically, more specifically, bilirubin, amylase, lipase, LFTs, cbc (possibly elevated wbc)
- U/S (diagnostic procedure of choice) - ERCP - endoscopic retrograde cholangiopancreatography (diagnostic and therapeutic) - MRCP - magnetic retrograde cholangiopancreatography (only diagnostic) |
|
|
What is biliary colic?
- Clinical features? - Investigations? - Management? |

|
|
|
What is acute cholecystitis?
- Clinical Features? - Investigations? - Complications? |

|
|
|
What is the management for acute cholecystitis?
|

|
|
|
In bilary colic there is no infection, only pain. T/F?
|
True
|
|
|
Treatment for acute cholecystitis vs biliary colic?
|
BILIARY COLIC
- rehydration - analgesia - elective cholecystectomy ACUTE CHOLECYSTITIS - antibiotics (ciprofloxacin 400mg IV q12h + metronidazole 500mg IV q8h) - early laparoscopic cholecystectomy |
|
|
What is choledocholithiasis?
- Clinical features? - Investigations? - Complications? - Management? |

|
|
|
What is Acute Cholangitis?
- Clinical features? - Investigations? - Treatment? |

|
|
|
What is gallstone ileus?
|

Gallstone ileus
- gallstone entering the intestine through a fistula (cholecystoenteric fistula) and getting lodged in the intestine creating an obstruction at the ileocecal valve |
|
|
Match the following to the list given in answers:
1. chronic pancreatitis 2. pancreatic cancer 3. biliary tract disease 4. chronic mesenteric angina |
A) Recurrent, intermittent epigastric abdo pain that occurs approximately 1 hr after meals
B) Daily postprandial abdo pain, assoc with 40 lb weight loss C) Chronic, persistent abdo pain and back pain of 1 month duration and a 10 lb weight loss D) diarrhea that occurs following fatty meals, steatorrhea, and chronic epigastric and back pain ANSWERS: 1D 2C 3A 4B |
|
|
What is Murphy's sign?
|
Test for cholecystitis
Classically Murphy's sign is tested for during an abdominal examination; it is performed by asking the patient to breathe out and then gently placing the hand below the costal margin on the right side at the mid-clavicular line (the approximate location of the gallbladder). The patient is then instructed to inspire (breathe in). Normally, during inspiration, the abdominal contents are pushed downward as the diaphragm moves down (and lungs expand). If the patient stops breathing in (as the gallbladder is tender and, in moving downward, comes in contact with the examiner's fingers) and winces with a 'catch' in breath, the test is considered positive. |
|
|
What is a acalculous cholecystitis?
|
- acute or chronic cholecystitis in the absence of stones
- typically due to gallbladder stasis --> sludge forms in gallbladder |
|
|
What is Boas's sign?
|
right subscapular pain that can be present in cholecystitis
|
|
|
T/F. A patient with choledocholithiasis may present with acholic stool, dark urine, and fluctuating jaundice
|
True
|
|
|
T/F. Hiatus hernia worsens reflux, does not cause it
|
True
|
|
|
What is the difference in treatment for biliary colic vs. acute cholecystitis?
|
biliary colic:
- analgesia, hydration, and elective cholecystectomy acute cholecystitis - antibiotics and early cholecystectomy |
|
|
What does molluscum contagiosum look like? Which virus causes it? How do you manage it?
|

Molluscum contagiosum (MC) is a viral infection of the skin or occasionally of the mucous membranes, sometimes called water warts. It is caused by a DNA poxvirus called the molluscum contagiosum virus (MCV). The virus that causes molluscum is spread from person to person by touching the affected skin. The virus may also be spread by touching a surface with the virus on it, such as a towel, clothing, or toys. Once someone has the virus, the bumps can spread to other parts of their body by touching or scratching a bump and then touching another part of the body. Molluscum can be spread from one person to another by sexual contact. This common viral disease has a higher incidence in children, sexually active adults, and those who are immunodeficient. and the infection is most common in children aged 1 to 10 years old.
Treatment is not necessary for this condition as it resolves on it own. Treatment options do include cryotherapy or curettage if absolutely necessary but should be avoided. |
|
|
What is a tonsillolith? What is the management?
|

- presence of calcified material in the crevices of tonsils.
Treatment is not necessary if asymptomatic. If symptomatic, then options include: - oral irrigation (low speeds) - curettage (ent referral) - laser treatment (ent referral) - tonsillectomy (ent referral) |
|
|
Write a prescription for champix (varenicline) for smoking cessation.
|
Champix (Varenicline)
0.5mg qam x 3d; then 0.5mg bid x 4d; then 1mg bid x 3mo repeats: 1 Instructions: continue to smoke (if smoking) for 1st week of treatment, then completely stop. contraindications: - preexisting pysch condition (not strict contraindication but be cautious) - pregnancy S/E: - night terrors - insomnia - h/a - n/v - constipation |
|
|
Write a prescription for bupropion (welllbutrin) for smoking cessation.
|
Bupropion
150mg qAM x 3d; then BID x 3mo repeats: 1 Instructions: continue to smoke (if smoking) for 1st week of treatment, then completely stop. contraindications: - seizure disorder (bupropion lowers seizure threshold; therefore good idea to ask about alcohol abuse --> more likely to get seizures with alcohol withdrawal) - eating d/o (b/c of inc. risk of seizures due to electrolyte imbalances) - MAOI used in the last 14d side effects: - insomnia - dry mouth |
|
|
note
|
ciprofloxacin is NOT covered by ODB. You need an LU code for it to be covered.
|
|
|
A 78M pt comes in to your office c/o of sudden onset unilateral hearing loss of 100% x4d ago. What is your differential diagnosis?
|
i. labyrinthitis
ii. cva iii. otitis media w/ effusion (no treatment necessary) - get an urgent audiology assessment - consult ent - if this pt has labyrinthitis (more often pt will c/o of vertigo), then this pt will need steroid medications such as prednisone. After speaking to one ENT, he recommended the following: i. prednisone 50mg od x 10d ii. zinc elemental 20mg od x 14d iii. ppi (pariet ec 20mg od x 10d) NOTE: make sure they don't have any contraindications to taking oral steroids. In some cases ent specialists will inject a steroid into the middle ear. note: caution / contraindications to oral steroids include (but not limited to): - severe renal failure - severe liver disease - osteoporosis - elderly pts - HTN, CHF |
|
|
What is SSRI discontinuation syndrome?
|
Caused by rapid dose reduction or abrupt cessation of an ssri/snri antidepressants. Symptoms include:
- brain zaps, confusion - (think anxiety) sweating, nausea, tremor, chills, dizziness - insomnia, nightmares - vertigo note: symptoms may last 1-3wks but can be relieved in 24h by restarting antidepressant at the same dose that was being taken, and initiating a slow taper over several weeks. May consider a drug w/ a long half-life such as fluoxetine. |
|
|
How is tylenol dosed in different age groups?
|
children 0-12:
- 15mg/kg q4h prn; max 5 times a day; max daily dose 3750mg/d ages >12 (adolescents and adults) tylenol 500mg-1000mg q4h prn; max daily dose 4000g/d note: regular tylenol is 325mg / tablet; extra strength tylenol is 500mg / tablet |
|
|
How is advil dosed in different age groups?
|
infants and children (<12 yrs)
10mg/kg q6h prn; max daily dose 40mg/day >12yrs and adults: for pain, fever, dysmenorrhea 200-400mg q6h prn; max daily dose of 1.2mg/d |
|
|
What is clavulin?
|
clavulin is a combination antibiotics:
amoxicillin-clavulanic acid note: common doses are: i. 500/125 (amoxicillin/clavulanic acid) ii. 875/125 (amoxicillin/clavulanic acid) |
|
|
note
|
pregnancy in a woman who has an IUD in place is an ectopic pregnancy until proven otherwise
|
|
|
note
|
In a normal pregnancy, the quantitative bHCG doubles every 48-72hrs
|
|
|
A pt develops a bump on the achilles tendon. What might that be?
|

ddx:
- tendonitis +/- nodule - bony spur |
|
|
How do you differentiate clinically acute cholecystitis from cholangitis?
|
Note: these two are quite similar in that they both present is ruq pain and fever; however, jaundice typically occurs w/ cholangitis. In addition stools will be acholic and urine dark in cholangitis.
|
|
|
When is screening for gestational diabetes typically done?
|
between 24-28 wks
|
|
|
What screening test do you order for gestational diabetes? What result from this screening test would lead to diagnose gestational diabetes?
|
50g 1hr oral glucose challenge test (OGCT). 1hr sugar > 10.3mmol/L = diagnosis of diabetes
|
|
|
For gestational diabetes screening, what result from the 1 hr oral glucose challenge test would lead you to do further investigations? What investigation would you do?
|
1 hr sugar >7.8 and <10.3 mmol/L
Investigation: 75g 2 hour oral glucose tolerance test |
|
|
Gestational diabetes may be associated w/ delivery complications. What other risk does gestational diabetes carry for the newborn? List 4
|
i. hypoglycemia
ii. hyperbilirubinemia and jaundice iii. hypocalcemia iv. polycythemia |
|
|
List the most common causes of hemoptysis (coughing up blood)?
|
- bronchitis (most common cause)
- bronchiectasis - pneumonia - fungal infection - TB - lung Ca |
|
|
What is the definition of massive hemoptysis?
|
- total blood volume >200ml /24hr
- blood loss of >100ml/d for 3 or more days |
|
|
A 23 female pt comes in to your office c/o of red eye and irritation of the r. eye. If this pt's condition was caused by certain broad group of pathogens, corticosteroid drops could worsen the condition. List 2 broad group of pathogens that could lead to worsening of the pts symptoms if she take corticosteroid drops.
|
i. viral pathogens
ii. fungal pathogens |
|
|
What are 2 potentially serious S/Es of prolonged use of topical corticosteroid drops in the eye?
|
i. cataracts
ii. increased intraocular pressure iii. optic nerve damage |
|
|
What is acute angle closure glaucoma?
|
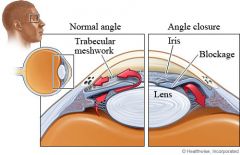
acute angle closure crises characterized by
- sudden ocular pain - seeing halos around lights - red eye - nausea and vomiting - suddenly decreased vision - very high intraocular pressure (>30 mmHg) - fixed, mid-dilated pupil. It is also associated with an oval pupil in some cases. Acute angle closure is an emergency. It is diagnosed by measuring intraocular pressure. |
|
|
What is glaucoma?
|
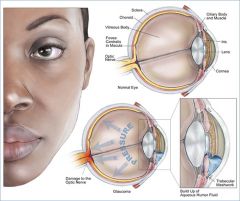
Glaucoma is a term describing a group of ocular disorders with multi-factorial etiology united by a clinically characteristic intraocular pressure-associated optic neuropathy. This can permanently damage vision in the affected eye(s) and lead to blindness if left untreated. It is normally associated with increased fluid pressure in the eye (aqueous humour), but not required for diagnosis.
Glaucoma can be classified as: i. primary open angle glaucoma ii. secondary open angle glaucoma (steroid induced, traumatic) iii. normal tension glaucoma iv. primary angle-closure glaucoma v. secondary angle-closure glaucoma (uveitis) |
|
|
What is the definitive treatment for acute angle closure glaucoma?
|
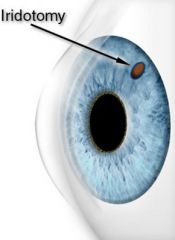
laser iridectomy which involves the removal of part of the iris.
|
|
|
Overuse of which class of constipation medications can cause resistance?
|
Stimulant laxatives such as senokot and bisacodyl. These drugs work by increasing the intestinal motor activity and the body may get used to this, and overtime these drugs may start losing their effect.
|
|
|
What is the treatment for tinea cruris?
|

lamisil 1% cream
apply to affected area od x 10d M: 30g note: should advise the pt that after completing treatment for 10d, it may take another 2 wks for the fungal infection to resolve. |
|
|
A 47F pt presents w/ what looks like a fungal infection around the anal region. How would you treat this condition?
|
canestan (clotrimazole) 1% cream w/ 1%HC powder
apply bid until resolution and then 2 more days |
|
|
What is the Kiesselbach's plexus and what is the significance of this area?
|

Kiesselbach's plexus, which lies in Kiesselbach's area, Kiesselbach's triangle, or Little's area, is a region in the anteroinferior part of the nasal septum where four arteries anastomose to form a vascular plexus of that name.
90% of nose bleeds (epistaxis) occur in Little's area, as it is exposed to the drying effect of inspiratory current. Alternatively, it can be argued, since most nosebleeds are provoked by nose-picking, that this very vascular area of nasal mucosa is within reach of the probing finger. |
|
|
What are the common causes of epistaxis in a child?
|
- dry mucosa
- foreign body - viral urti - inhaled corticosteroids - trauma - nose picking - blood dyscrasias |
|
|
A 4F child has had 2 uncomplicated urinary tract infection (uti). Her mother brings her to the office w/ Sx of urinary frequency, urgency, and dysuria for the past 12 hrs. What other Sx of Marianne's present illness would help you assess her problem? List 4
|
- chills (fever is not a Sx)
- nocturia - urinary incontinence (v. imp. in a child) - abdo pain |
|
|
What are 2 investigations you would do in a child w/ recurrent urinary tract infection (uti)?
|

- KUB ultrasound
- voiding cystourethrogram (vcug) note: VCUG is a technique for watching a person's urethra and urinary bladder while the person urinates (voids). The technique consists of catheterizing the person in order to fill the bladder with a radiocontrast agent. Under fluoroscopy (real time x-rays) the radiologist watches the contrast enter the bladder and looks at the anatomy of the patient. If the contrast moves into the ureters and back into the kidneys, the radiologist makes the diagnosis of vesicoureteral reflux. The exam ends when the person voids while the radiologist is watching under fluoroscopy. Consumption of fluid promotes excretion of contrast media after the procedure. It is important to watch the contrast during voiding, because this is when the bladder has the most pressure, and it is most likely this is when reflux will occur. Vesicoureteral reflux (kidney reflux) is diagnosed with an ultrasound and VCUG. Children who have recurrent urinary tract infections are given this test to determine the risk of subsequent infections causing potentially damaging kidney infections. |
|
|
What are absolute contraindications to using OCPs?
|
- acute liver disease
- abnormal vaginal bleeding - hx of breast/uterine Ca (estrogen dependent tumors) - prev DVT/PEs - migraine w/ aura - uncontrolled htn - smoking >35 - known suspected pregnancy |
|
|
What physical exam maneuvers would you do prior to prescribing OCPs?
|
i. BP check
ii. breast exam iii. cvs - s1, s2, murmurs iv. percussion + palpation of liver v. pelvic exam (+/- pap test; *note a physical exam but would do anyways if not done within 3 yrs) |
|
|
Should cervical swabs for gonorrhea and chlamydia be done prior to IUD insertion?
|
yes
|
|
|
Differentiate between the estrogen vs. progestin related side effects of OCPs.
|
Estrogen:
- nausea - breast tenderness, enlargement - fluid retention, bloating, edema - migraines Progestin: - depression - fatigue - dec. libido - increased appetite - acne/oily skin - hirsutism |
|
|
What is Androgenic alopecia?
|

Androgenic alopecia aka male-pattern baldness. Fronto-temporal areas progress to vertex, entire scalp may be bald
Androgenic alopecia is the most common cause of hair loss and thinning in humans. Variants appear in both men and women. In classic pattern baldness, hair is lost in a well-defined pattern, beginning above both temples. Hair also thins at the crown of the head. Often a rim of hair around the sides and rear of the head is left. This type of pattern is dubbed "Hippocratic balding" and may rarely progress to complete baldness. Women do not suffer classic male pattern baldness, instead the hair becomes thinner around the whole scalp, and the hairline does not recede. This is dubbed "female pattern baldness" and may occur in males. This variety of androgenic alopecia in women rarely leads to total baldness. Male pattern baldness is caused by a genetic sensitivity of hair follicles to DHT. This hormone causes follicles to shrink or "miniaturize". In turn, this shortens their lifespan and prevents them from producing hair normally. |
|
|
What is the management of androgenic alopecia?
|
- minoxidil (rogaine) lotion
- finasteride (propecia) (takes >3months to work) - spironolactone in women (anti-androgenic effects) - hair transplant |
|
|
What are some of the main causes of non-scarring (non-cicatricial) alopecia?
|
- Androgen alopecia (physiologic - most common in adult men and postmenopausal women)
- Telogen effluvium (loss of mature hair): uniform decrease in hair density secondary to an increased no. of hairs in the resting stage (telogen stage). Precipitated by: malnutrition, Fe deficiency, thyroid dysfunction, post-partum/miscarriage, scalp diseases (seborrheic dermatitis, allergic contact dermatitis), medications such as OCP, physical mental stress. Hair loss typically occurs 2-4 months after exposure to precipitant and regrowth occurs within a few months. Anagen effluvium (loss of growing hair): hair loss due to insult to hair follicle impairing its mitotic activity (growth stage). Most common cause is chemotherapy, other meds such as bismuth, levodopa, chochicine, cyclosporine), exposure to chemicals (thallium, boron, arsenic). Dose dependent effect. Hair loss 7-14 days after single pulse of chemo; most clinically apparent after 1-2 months. Hair loss is reversible and hair growth resumes after a few weeks post precipitating agent. Alopecia areata: autoimmune disorder characterized by patches of complete hair loss localized to scalp, eyebrows, beard, eyelashes Alopecia totalis - loss of all scalp hair and eyebrows Alopecia universalis: loss of all body hair Traumatic alopecia: eg. tight "corn-row" braiding of hair Trichotillomania: impulse-control disorder characterized by compulsive hair pulling with irregular patches of hair loss, and with remaining hairs broken at varying lengths Infections (e.g., tinea capitis) |
|
|
What is the main difference between non-scarring and scarring alopecia?
|
Non-scarring alopecia
- intact hair follicles on exam - biopsy not required Scarring alopecia - absent hair follicles on exam - biopsy required |
|
|
What is the management of alopecia areata?
|
- generally unsatisfactory
- corticosteroids (for isolated patches) - UV or PUVA therapy - immunomodulatory (diphencyprone) |
|
|
What are some of the main causes of scarring (cicatricial) alopecia?
What is the management of infectious causes and DLE? |
Irreversible loss of hair follicles with fibrosis
- radiation - burns - infections (bacterial, TB, fungal, herpes zoster, leprosy) - inflammatory (discoid lupus, lichen planus) - tumors - skin conditions (bullous diseases) - Androgenic alopecia (most common in 30 to 40% of adult men and postmenopausal women) MANAGEMENT: - Infections: treat underlying infection - DLE: treat with topical/intralesional steroid or antimalarial |
|
|
What is alopecia areata?
|

autoimmune mediated areas of hair loss breaking off and leaving exclamation point hairs.
may be due to: - pernicious anemia - vitiligo - thyroid disease - addison's - SLE |
|
|
What are the most common triggers for anaphylaxis?
|
i. food (nuts, shellfish etc)
ii. stings iii. drugs (penicillin, nsaids, ace-i) iv. blood products v. latex vi. radiographic contrast media |
|
|
Allergic / Anaphylactic reactions are typically Ig___ mediated.
[allergy, anaphylaxis] |
E
|
|
|
What is the management of an anaphylactic reaction?
|
i. ABCs (also establish IV lines and give fluids prn)
ii. monitoring iii. remove causative agent (if possible) iv. *epinephrine (most important drug for anaphylaxis) v. benedryl 50mg IM/IV q4-6h prn vi. prednisone 50-100mg IV vii. salbutamol (ventolin) via nebulizer if bronchospasm viii. glucagon (for those on b-blockers w/ resistant hypotension and / or cardiac disease *note: epinephrine dosing for IM vs. IV - moderate signs/sx: [adults] 0.3ml of 1:1000 solution IM; [child] 0.01ml/kg upto 0.4mL/dose 1:1000 solution IM - severe signs/sx: [adults] 1ml of 1:10,000 solution IV; [child] 0.01mL/kg of 1:10,000 solution IV |
|
|
What are some follow up instructions you would give to a parent of a child who has just been treated for an anaphylactic reaction in the ER?
|
- follow up w/ GP
- allergy testing - epi-pen x 2 to be carried |
|
|
Define sensitivity, specificity, PPV, NPV.
|
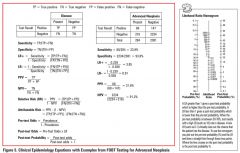
sensitivity: proportion of people with disease who are correctly identified by a positive test
specificity: proportion of people without disease who are correctly identified by having a negative test positive predictive value (ppv): proportion of people w/ a positive test who have the disease negative predictive value (npv): proportion of people w/ a negative test who are disease free |
|
|
Explain "SPIN" and "SNOUT" with respect to sensitivity and specificity.
|
SPIN: a test with a high SPecificity is likely to rule IN a hypothesis
SNOUT: a test with a high SeNsitivity is likely to rule OUT a hypothesis |
|
|
note
|
- sensitivity and specificity are characteristics of the test.
- ppv and npv are dependent on the prevalence of the disease in the population LR (likelihood ratio) depends on the test characteristics NOT the prevalence |
|
|
What are the components of a good randomized controlled trial.
|
- randomization
- blinding of both groups - similarity between treatment and placebo groups - both groups treated the same way - precise estimate of treatment effect - intention to treat analysis - reproducible design |
|
|
How do you confirm the diagnosis of onychomycosis?
|
Diagnosis (confirmation)
- KOH smear - culture - histology |
|
|
What is tinea pedis (athlete's foot). How is it treated?
|

fungal infection on the foot.
Rx Lamisil 1% cream Apply to affected areas bid M: 30g repeat:1 |
|
|
What are the non-pharmacological vs. pharmacological management options for onychomycosis?
|
Non-pharmacological options:
keep feet dry, good hygiene, socks, avoid trauma, well-fitting footware Prescription Lamisil (terbinafine) 250mg po od x 6 weeks for fingernails (check LFTs at baseline) Lamisil (terbinafine) 250mg po od x 3 months for toenails (check LFTs at baseline and 6 wks) note: Important to do LFTs as terbinafine can be hard on the liver. note: Important to warn pts that the nail may not change in appearance at the end of 6wk (or 3months) treatment. That does not mean treatment failure. The nail gets better over time. |
|
|
What is the criteria for metabolic syndrome?
|
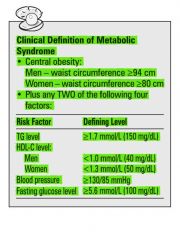
|
|
|
What are the risk factors for breast cancer?
|
- gender
- age - prev. breast cancer - 1st degree relative w/ breast cancer (greater if relative was premenopausal) - known brca 1 or 2 mutation - high breast density - nulliparity, first pregnancy >30 yrs old - menarche <12 - menopause >55 - radiation exposure - >5yrs of hrt NOTE: risk decreased with: - lactation - early menopause - early childbirth |
|
|
For the following 2 phases in the menstrual cycle, are they fixed or variable ?
1. Follicular phase/proliferative 2. Luteal phase/secretory |
1. Follicular phase / proliferative: variable duration (varies usually from 14-21 days)
2. Luteal phase / secretory: fixed duration (14 days) |
|
|
What are some risk factors for endometrial cancer?
|
COLD NUT
Cancer (ovarian, breast, colon) Obesity Late menopause DM Nulliparity Unopposed estrogen: PCOS, anovulation, HRT Tamoxifen: chronic use NOTE: Type I endometrial Ca is related to excess estrogen use Type II endometrial Ca is not related to estrogen; possibly due to tamoxifen |
|
|
Show graphically the results of the cipriani study in assessing efficacy vs. tolerance.
|
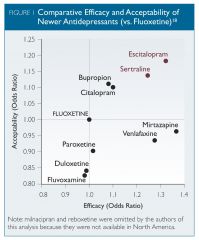
|
|
|
What are the 2 biggest RFs for breast cancer?
|
1. Gender (biggest RF)
2. Age (80% of breast cancers are in women > age 40 |
|
|
For women who have had breast cancer in the past, how often should mammograms be done?
|
annually
|
|
|
What are RFs for cervical cancer?
|

|
|
|
T/F. High serum urate is NOT diagnostic of gout.
|
True
- a high serum urate level does not rule in gout - a low serum urate level does not rule out gout However, a baseline serum uric acid level may be beneficial in case the patient will be put on allopurinol in the future in which case the target serum uric acid level should be <300umol/L. NOTE: when on allopurinol serum uric acid levels should be checked q2wks until levels are less than 300. |
|
|
What are some of the s/e of allopurinol?
|
- rash
- gout - GI: nausea, diarrhea |
|
|
T/F. A pregnant women with gestational diabetes mellitus (GDM) should be screened with a 2h 75g OGTT 6 weeks and 6 months postpartum.
|
True. There is about a 50% chance of these women developing DM II in the next 20 years.
note: It is important to fast for 10-12h for the 2h 75g OGTT |
|
|
Discuss the screening and diagnosis of gestational diabetes mellitus (GDM) in pregnancy. What are the tests available for this. What are the RFs for GDM.
|

|
|
|
What is the DDx for ruq pain?
|
- rll pneumonia
- acute hepatitis - biliary colic - cholecystitis - acute cholangitis - choledocholithiasis - pud - gastroenteritis - pyelonephritis |
|
|
What are some complications of acute cholecystitis?
|
- sepsis
- empyema - ascending cholangitis - pancreatitis - gallbladder perforation - duodenal perforation and gallstone ileus |
|
|
What is the DDx for constipation?
|
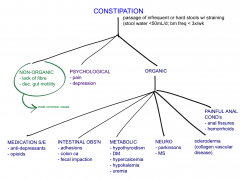
|
|
|
A 23F gets bitten by a dog. You are concerned about rabies. What questions would you ask on hx?
|
History:
i. wild or pet dog? ii. was the dog vaccinated? iii. any odd behavior by the dog? iv. provoked vs. unprovoked attack? v. attack site vi. attack depth vii. dog available for monitoring after attack? viii. prevalence of rabies in geographic location? |
|
|
Which animals are responsible for transmitting rabies to human?
|
- skunk (40%)
- bat (26%) - fox (11%) - racoon (8%) - dogs and monkeys |
|
|
What is rabies?
What are the symptoms? |
Rabies is a viral disease that causes acute encephalitis in warm-blooded animals. The disease is zoonotic, meaning it can be transmitted to humans from another species (such as dogs), commonly by a bite from an infected animal. For a human, rabies is almost invariably fatal if postexposure prophylaxis is not administered prior to the onset of severe symptoms. The rabies virus infects the central nervous system, ultimately causing disease in the brain and death.
The rabies virus travels to the brain by following the peripheral nerves. The incubation period of the disease is usually a few months in humans, depending on the distance the virus must travel to reach the central nervous system. Once the rabies virus reaches the central nervous system and symptoms begin to show, the infection is virtually untreatable and usually fatal within days. SYMPTOMS: Early-stage symptoms of rabies are malaise, headache and fever, progressing to acute pain, violent movements, uncontrolled excitement, depression, and hydrophobia. Finally, the patient may experience periods of mania and lethargy, eventually leading to coma. The primary cause of death is usually respiratory insufficiency. |
|
|
T/F. If suspicious of rabies, one should contact public health.
|
True. Rabies or suspicion of rabies is reportable to public health.
|
|
|
What is the prevention and treatment of rabies?
|
PREVENTION:
- vaccinate animals - pre-exposure prophylaxis vaccination for high risk individuals (eg. vets) TREATMENT: - passive immunization with HRIg (human rabies Ig) into wound site with any remaining volume into site distant from wound site. - active immunization with inactivated rabies virus series given at 0, 7, and 21 days |
|
|
What is developmental dysplasia of the hip? What investigations if any would you do? What is the treatment and complications of this condition.
|
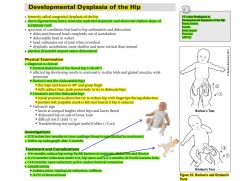
|
|
|
What are the 5Fs that predispose to developmental dysplasia of the hip?
|
Female
Family Hx Frank breech First born leFt hip |
|
|
What are the 2 physical exam manuevers you can do to confirm a dislocated hip?
|
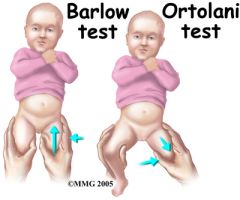
i. Barlow's test
ii. Ortolani's test |
|
|
What physical exam manuevers can you do for examining a patient with lateral epicondylitis (tennis elbow) vs. medial epicondylitis (golfers elbow)
|
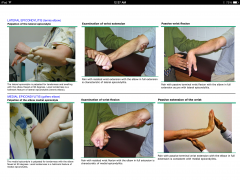
- in l. epicondylitis, you get pain w/ supination
- in m. epicondylitis, you get pain w/ pronation |
|
|
What are some management strategies for epicondylitis?
|
- rest, ice, elevation
- naproxen - brace - steroid injection |
|
|
What does the 'RICE' pneumonic for management of localized inflammatory conditions stand for?
|
Rest
Ice Compression Elevation |
|
|
What are some complications of H.pylori?
|
- pud
- gastric adenocarcinoma - gastric lymphoma - non-ulcer dyspepsia |
|
|
What are the ottawa ankle rules?
|
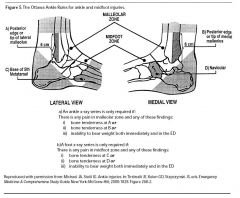
|
|
|
How does primary open angle glaucoma differ symptomatically from primary angle closure glaucoma?
|
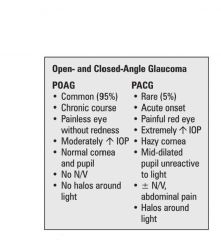
|
|
|
What are the RFs for primary open angle glaucoma?
|
A FIAT (age, fmhx, inc iop, african descent, thyroid)
MAIN RFs - age (10% in >80yr) - family hx - IOP - african descent MINOR RFs - htn - dm - hyperthyroidism (grave's disease) - thin cornea |
|
|
What are the RFs for primary angle-closure glaucoma?
|
- hyperopia (far-sightedness) [small eye big lens - large lens crowds the eye]
- age > 70 - female - family hx - asian and inuit ethnicity - mature cataracts - shallow anterior chamber - pupil dilation (stress, darkness, topical/systemic anticholinergics) |
|
|
note
|
primary open angle glaucoma makes up ~95% of glaucoma cases, whereas primary angle closure glaucoma makes up about ~5% of cases.
primary angle closure glaucoma is an EMERGENCY and the management includes: - laser iridoctomy (ophthalmology referal) - miotic drops (pilocarpine) to reverse pupillary block - dec. IOP by using topical b-blockers, adrenergics, cholinergics - systemic hyperosmotic agents - mannitol |
|
|
Diagram explaining difference between open vs. closed angle glaucoma.
|
(A) Normal outflow through trabecular meshwork (large arrow) and uveoscleral routes (small arrow) and related anatomy. Most aqueous flow is through the trabecular meshwork. Each pathway is drained by the eye's venous circulation. (B) In primary open-angle glaucoma, aqueous outflow by these pathways is diminished. (C) In angle-closure glaucoma, the iris is abnormally positioned so as to block aqueous outflow through the anterior chamber (iridocorneal) angle.
|
|
|
What is the management of primary open angle glaucoma?
|
Goal is to dec IOP by:
- increasing drainage and / or - dec. production of aqueous --------------------------------------------------------------------------- MEDICAL inc. aqueous outflow - topical α-adrenergics - topical cholinergics dec. aqueous production - topical β-blockers --------------------------------------------------------------------------- SURGICAL - laser trabeculoplasty - trabeculectomy |
|
|
You're working your shift in the local ER. What is some treatment optons for an allergic reaction such as a rash (maculopapulorash diffuse widespread)? NOTE: this is not an anaphylactic reaction.
|
i. benedryl (otc)
ii. benedryl spray - apply on rash iii. aveeno bath w/ lukewarm water (make sure water is not ++ hot as this can worsen Sx) iv. prednisone 50mg x 5d |
|
|
In a patient with sickle cell disease, what is the most common organism if the patient has:
a) sepsis b) osteomylitis |
a) sepsis: s. pneumoniae
b) osteomylitis: salmonella |
|
|
note
|
Women with Trichomoniasis vaginalis infection often present with pruritis and green, frothy, foul-smelling vaginal discharge. They may also have urinary symptoms or dysparunia.
|
|
|
note
|
Tamoxifen acts as an estrogen antagonist on breast tissue, and is used in the treatment and prevention of breast cancer.
However, It acts as an estrogen receptor agonist on the endometrium and increases the risk of endometrial carcinoma. Tamoxifen also decreases the risk of osteoporosis. |
|
|
The treatment for Candida vulvovaginitis typically involves oral flucanozole. What are 2 topical cream options?
|
i. clotrimazole (canestan)
ii. nystatin iii. monistat (otc) - for pregnancy this would be the best option note: nystatin is also given for oral thrush |
|
|
What is the treatment of atrophic vaginitis vs. lichen sclerosis?
|
![ATROPHIC VAGINITIS
- local estrogen cream (premarin)
LICHEN SCLEROSIS
- topical steroid
[picture of lichen sclerosis]](https://images.cram.com/images/upload-flashcards/74/81/75/2748175_m.jpeg)
ATROPHIC VAGINITIS
- local estrogen cream (premarin) LICHEN SCLEROSIS - superpotent topical steroid [picture of lichen sclerosis] |
|
|
What is lichen sclerosus?
What are the symptoms? What is the etiology? |
Lichen sclerosus (LS) refers to a benign, chronic, progressive dermatologic condition characterized by marked inflammation, epithelial thinning, and distinctive dermal changes accompanied by symptoms of:
- pruritus ++ - pain - dysparunia (late Sx) - dysuria - difficulty voiding (if fusion of labia minora over urethra occurs) LS usually occurs in the anogenital region (85 to 98 percent of cases), but can develop on any skin surface. Extragenital lesions are present in 15 to 20 percent of patients. Vulvar LS can occur at any age but tends to have two peaks of onset: prepubertal girls and perimenopausal or postmenopausal women. Etiology: Although it is not clear what causes LS, four theories have been postulated. i. autoimmune ii. infection iii. hormonal - low estrogen states iv. local skin changes |
|
|
T/F. lichen sclerosus is NOT contagious.
|
True
|
|
|
T/F. hyperprolactenemia can lead to ovulation suppression as it inhibits the release of GnRH from the hypothalamus resulting in amenorrhea
|
True
|
|
|
What is the difference between the ulcers in syphilis vs the ulcers in herpes and chancroid?
|
Syphilis ulcers are painless
Herpes and chanchroid ulcers are painful |
|
|
What is the treatment of postpartum endometritis?
|
IV clindamycin + gentamicin
|
|
|
Out of the 3 analgesics: Tylenol, NSAIDs, and Opioids; which of the following does/do not have a ceiling effect?
|
Opioids in general DO NOT have a ceiling effect except for codeine.
NOTE: Tylenol and NSAIDs do have a ceiling effect. |
|
|
Are there any other meds to consider giving when giving a patient strong opioids?
|
- anti-emetic (gravol) for N/V.
- laxative (colace aka. docusate sodium) for constipation. |
|
|
What is the maximum adult dose of tylenol per day?
|
4g/day (4000mg/day)
|
|
|
How does epinephrine (adrenaline) work?
|
As a hormone and neurotransmitter, epinephrine (adrenaline) acts on nearly all body tissues. Its actions vary by tissue type and tissue expression of adrenergic receptors. For example, high levels of adrenaline causes smooth muscle relaxation in the airways but causes contraction of the smooth muscle that lines most arterioles.
|
|
|
What is the management of intermittent claudication?
|
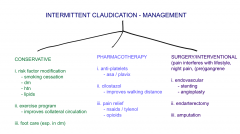
|
|
|
What are the key manifestations of child abuse?
|
- STIs
- developmental delay - emotional/behavioural problems Distinctive marks: - belt buckle - cigarette burns - hand prints Shaken baby syndrome: - retinal hemorrhages - intracranial hemorrhages - posterior rib #s |
|
|
T/F. With respect to elder abuse, physician reporting is mandatory only in Newfoundland, Nova Scotia and PEI; in Ontario, only abuse occurring in nursing homes is mandatory to report.
|
True
|
|
|
Discuss the Legal Duty to Report with re: child abuse.
|

|
|
|
What does lichen sclerosis look like?
|

|
|
|
What are the 3 main clinical features of intermittent claudication?
|
clinical features:
i. pain w/ exertion (usually in calves or any exercising muscle group) ii. relieved w/ short rest: 2-5 mins typically iii. reproducible: same distance to elicit pain, same location of pain, same amt of rest to relieve pain |
|
|
What are the investigation options for intermittent claudication? Discuss the degree of ischemia per ABI levels?
[ABI - ankle brachial index] [note: intermittent claudication also known as peripheral arterial disease, aka chronic arterial insufficiency] |

|
|
|
What are the RFs for intermittent claudication (peripheral arterial insufficiency)?
|
- smoking
- dm - htn - hypercholesterolemia - family hx - obesity - sedentary lifestyle - male |
|
|
T/F. For a patient with known intermittent claudication, rest pain occurs with an ABI of <0.3.
|
True
|
|
|
Discuss the classification of the ankle brachial index (ABI).
|

|
|
|
What is a peak flow meter?
|
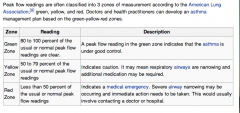
The peak expiratory flow (PEF), also called peak expiratory flow rate (PEFR) is a person's maximum speed of expiration, as measured with a peak flow meter, a small, hand-held device used to monitor a person's ability to breathe out air. It measures the airflow through the bronchi and thus the degree of obstruction in the airways.
|
|
|
What are possible GI complications of inflammatory bowel disease?
|
- intestinal malignancy
- strictures - abscess - fistulae - bowel obstuction - toxic megacolon - malabsorption |
|
|
What are the clinical differences between crohn's disease and ulcerative colitits?
|

|
|
|
What is the most common site of involvement for Crohn's disease?
|
ileum + ascending colon
often these pts will present w/ rlq pain |
|
|
What is the management of Crohn's disease?
|
- Nutrition (fluids only during acute exacerbations, those w extensive bowel inv or resection - req electrolyte, vitamin and mineral supplements
- Symtomatic relief (tylenol, loperimide) - ASA + corticosteroids (prednisone) - Immunosuppresents (methotrexate) - Immunomodulators (infliximab aka remicade) - Surgery (generally reserved for complications such as fistulae, obstruction, abscess, perforation, and bleeding) |
|
|
T/F. In ulcerative colitis, the rectum is always involved.
|
True
|
|
|
T/F. The risk of developing ulcerative colitis is less in smokers.
|
True
|
|
|
What is the management of ulcerative colitis?
|
- fluids and correct electrolyte disturbances (diet of little value in dec. inflammation but may alleviate symptoms)
- 5-ASA derivatives, corticosteroids - immunosuppressant (azathioprine - in steroid-dependent or resistant cases OR cyclosporine) - immunomodulators (infliximab) - surgery |
|
|
What are some extraintestinal manifestations of inflammatory bowel disease (IBD)?
[crohns, ulcerative colitis] |
i. oral ulcers
ii. uveitis iii. cholelithiasis iv. arthritis v. renal calculi |
|
|
What are the main causes of lower GI bleeds?
|
CHAND
Colitis (radiative, ischemic, IBD: UC>CD) Hemorrhoids/fissures Angiodysplasia Neoplastic - cancer/polps Diverticular disease |
|
|
What is the clinical presentation in a patient who has ulcerative colitis?
|
- In UC's initial presentation, non-bloody diarrhea is frequently seen; eventually progresses to bloody diarrhea
- abdo cramps, pain with defecation - tenesmus, urgency, incontinence - systemic symptoms: fever, anorexia, weight loss, fatigue in severe cases - extra-intestinal manifestations (oral ulcers, iritis, arthritis, cholelithiasis, renal calculi) |
|
|
What is the clinical presentation in a patient who has Crohn's disease?
|
- recurrent episodes of abdo cramps, diarrhea, weight loss
- most common location: ileum + ascending colon - ileitis may present with post-prandial pain, vomiting, RLQ mass; MIMICS ACUTE APPENDICITIS - fistulae, fissures, abscess are common - present with extra-intestinal features (arthritis, iritis, cholelithiasis, ulcers, renal calculi) - linear ulcers leading to mucosal islands and "cobblestone" appearance - present with granulomas |
|
|
When in the postpartum period should you test a patient with GDM for diabetes or glucose intolerance?
[diabetes] |
i. at 6 wks
ii. at 6 months |
|
|
What are the long term microscopic vs. macroscopic complications of diabetes?
|
Microscopic
i. retinopathy ii. nephropathy iii. neuropathy Macroscopic i. coronary artery disease ii. cerebrovascular disease iii. peripheral vascular disease |
|
|
When considering prescribing a morning-after pill, what is the most important question to ask the patient?
|
When did you have intercourse?
This is important, b/c the pill is to be taken within 72h and the efficacy does decrease with time. i.e. the pill taken at 24h is much more effective than taken at 72h. |
|
|
Write a prescription for an emergency postcoital contraceptive pill.
|
Plan B (levonorgestrel 750µg)
1 tablet q12h x 2 |
|
|
What is the main contraindication to the emergency postcoital contraceptive pill - eg. plan b
|
pre-existing pregnancy
|
|
|
What is social phobia (Social Anxiety Disorder)?
|
Marked or persistent fear of social or performance situations in which the person is exposed to unfamiliar people or to possible scrutiny by others; person fears he/she will act in a way that may be humiliating or embarrassing (eg. public speaking, initiating or maintaining conversation, dating, eating in public)
|
|
|
What is Generalized Anxiety Disorder ?
|
DIAGNOSTIC CRITERIA
A. Excessive anxiety and worry, occurring more days than not for at least 6 months, about a number of events and activities (such as work or school performance) B. The person finds it difficult to control the worry C. The anxiety and worry are associated ≥3 of the following 6 Sx (with at least some Sx present for more days than not for the past 6 months): [pneumonic BESKIM] - blank mind - easily fatigued - sleep disturbance - keyed up - irritable - muscle tension D. Significant occupational and social distress; not due to GMC or substance |
|
|
What is a Panic disorder? (without agoraphobia)
|
1. recurrent unexpected panic attacks: a discrete period of intense fear or discomfort, in which ≥4 of the following Sx develop abruptly and reach a peak within 10 minutes.
S T U D E N T S FEAR 3C's - sweating - trembling - unsteady (dizziness) - depersonalization / derealization - elevated hr - nausea - tingling - sob fear of losing control, going crazy, dying chest pain, chills, choking 2. At least 1 of the attacks has been followed by 1 month or more of 1 or more of the following: i. persistent concern about having more attacks ii. worry about the implications of the attacks and its consequences iii. a significant change in behaviour related to the attacks 3. Absence of agoraphobia 4. not due to GMC or substance |
|
|
What is panic disorder with agoraphobia?
|
- criteria for panic disorder + agoraphobia
Agoraphobia - anxiety about being in PLACES or SITUATIONS from which escape might be difficult (or embarrassing) or where help may not be available in the event of having an unexpected panic attack. - Fear commonly involves situations: being out alone, being in a crowd, standing in line, or travelling on a bus TREATMENT: Similar to Panic d/o w/o agoraphobia |
|
|
What is the management for panic disorder?
|
i. psychological
- relaxation techniques (box-breathing) - cbt - desensitization / exposure therapy ii. pharmacological - ssri: eg. cipralex - snri: eg. effexor - benzodiazepines: short term, low dose, regular schedule, no prn, long half-life |
|
|
What is bronchiolitis?
|
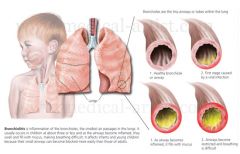
Bronchiolitis is defined as the FIRST episode of wheezing associated with urti and signs of respiratory distress. It is inflammation of the bronchioles, the smallest air passages of the lungs. It usually occurs in children less than two years of age with the majority being aged between 3-6 months.
Symptoms include: - prodrome of urti, with cough + fever - wheezing - sob, tachypnea - difficulty feeding - irritability - tachycardia This inflammation is usually caused by respiratory syncytial virus (70% of cases) and is much more common in the winter months. Treatment is typically supportive but may involve the use of nebulized epinephrine or hypertonic saline. Bronchiolitis is common with up to one third of children being affected in their first year of life. |
|
|
What are some modifiable RFs for acute otitis media (AOM)?
|
- exposure to 2nd hand smoke
- bottle vs. breast fed - crowded conditions - daycare - any type of feeding in supine position |
|
|
T/F. Egg allergy is NOT a contraindication to the influenza (flu) vaccine.
|
True
|
|
|
Explain the difference between heat exhaustion and heat stroke and their management.
|

|
|
|
What are some of possible complications of a heat stroke?
|
- encephalopathy
- seizure (if develop this then give benzos) - coma - respiratory failure - myocardial injury - pancreatic injury - hepatocellular injury - intestinal ischemia or infarction - acute renal failure - rhabomyolysis - DIC NOTE: heat stroke involves multi-organ failure |
|
|
What is rhabdomyolysis?
|
Rhabdomyolysis is a condition in which damaged skeletal muscle tissue breaks down rapidly. Breakdown products of damaged muscle cells are released into the bloodstream; some of these, such as the protein myoglobin, are harmful to the kidneys and may lead to kidney failure. The severity of the symptoms, which may include muscle pains, vomiting and confusion, depends on the extent of muscle damage and whether kidney failure develops. The muscle damage may be caused by physical factors (e.g., crush injury, strenuous exercise), medications, drug abuse, and infections. Some people have a hereditary muscle condition that increases the risk of rhabdomyolysis. The diagnosis is usually made with blood tests and urinalysis. The mainstay of treatment is generous quantities of intravenous fluids, but may include dialysis or hemofiltration in more severe cases.
|
|
|
What is ankylosing spondylitis (AS)?
(symptoms are discussed in another slide) |

AS is a form of spondyloarthritis, a chronic, inflammatory arthritis where immune mechanisms are thought to have a key role. It mainly affects joints in the spine and the sacroiliac joint in the pelvis, and can cause eventual fusion of the spine.
Complete fusion results in a complete rigidity of the spine, a condition known as "bamboo spine". There is no cure for AS, although treatments and medications can reduce symptoms and pain. It is HLA-B27 positive Symptoms appear gradually, usually around 23 years of age. Initial symptoms are typically chronic pain and stiffness in the middle part of the spine or the entire spine, often with pain referred to one or other buttock or the back of thigh from the sacroiliac joint. |
|
|
What investigations would you do in someone you suspect to have ankylosing spondylitis?
|
- bw_HLA B27
- xray: lumbar + sacroiliac joints |
|
|
What is the difference between cardiac arrest and a heart attack?
|
Cardiac arrest, also known as cardiopulmonary arrest or circulatory arrest, is the cessation of normal circulation of the blood due to failure of the heart to contract effectively.[1] Medical personnel may refer to an unexpected cardiac arrest as a sudden cardiac arrest (SCA).
A cardiac arrest is different from (but may be caused by) a heart attack, where blood flow to the muscle of the heart is impaired. |
|
|
note
|
The most common initial rhythms in witnessed sudden cardiac arrest are VF or rapid, pulseless VT (which will rapidly deteriorate into VF). VF deteriorates to asystole if not treated. The earlier defibrillation occurs the higher the survival rate.
|
|
|
Discuss the 'pulseless arrest' algorithm to treatment of VF and pulseless VT.
|
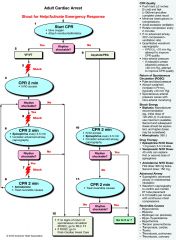
|
|
|
What should the defibrillator settings be in treating for VF/VT?
|
monophasic 360J
biphasic 200J |
|
|
T/F. Defibrillation is NOT appropriate in asystole and/or pulseless electrical activity (PEA).
|
True
|
|
|
What does ventricular fibrillation look like on ecg?
[ekg] |

|
|
|
What does monomorphic vs. polymorphic ventricular tachycardia look like on ecg?
[ekg] |
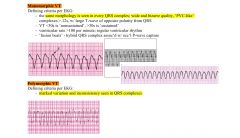
|
|
|
What does torsades de pointes look like on ecg?
[ekg] |

|
|
|
What does sinus tachycardia look like on ecg?
[ekg] |

|
|
|
What does atrial fibrillation vs. atrial flutter look like on ecg?
[ekg] |
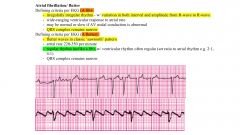
|
|
|
What does an SVT (supra-ventricular tachycardia) look like on ecg?
[ekg] |
|
|
|
What do the two types of 2° heart block look like on ecg?
[ekg] |
|
|
|
What do the two types of 3° heart block look like on ecg?
[ekg] |
|
|
|
What are the reversible causes of arrhythmias?
|
5H's and 5T's
- hypoxia - hypovolemia - hypothermia - acidosis (hydrogen ion) - hypo/hyperkalemia - tamonade (cardiac) - thrombosis (coronary) - tension pneumothorax - thrombus (pulmonary) - toxins |
|
|
What are some measures of knowing that endotracheal placement is appropriate?
|
i. chest expansion w/ ventilation
ii. breath sounds on ausculation iii. water vapour / misting within tube iv. end-tidal capnography v. cxr |
|
|
What are 2 indications for endotracheal intubation?
|
i. cardiac arrest when bag-mask ventilation is not possible or ineffective.
ii. patient is unable to protect airway (eg. coma, areflexia, or cardiac arrest) |
|
|
What are 2 methods that can be used to estimate weight in children/babies?
|
i. age based formulas
wt = 2 x (age in yrs + 4) ii. length measurements, such as Broselow tape NOTE: these methods often underestimate the child's actual weight. Nevertheless, they provide reasonable estimates when weights cannot be measured. |
|
|
Discuss the treatment for 'adult tachycardia (with pulse)' algorithm.
|
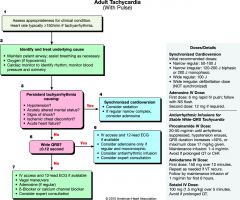
|
|
|
Discuss the treatment for 'adult bradycardia (with pulse)' algorithm.
|
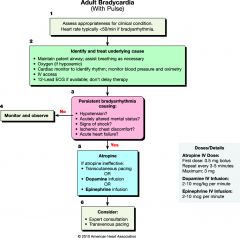
|
|
|
For drug reactions, what is the difference between type A and type B reactions?
|
TYPE A
- predictable - can occur in anyone given high dose (eg. diarrhea w/ abx, gastritis w/ nsaids) TYPE B - hypersensitivity reaction in susceptible individuals, may be exaggerated hypersensitivity, idiosyncratic, or immunologic (allergy) |
|
|
What is atopy?
|
Atopy (atopic syndrome) is a syndrome characterized by a tendency to be “hyperallergic”. A person with atopy typically presents with one or more of the following: eczema (atopic dermatitis), allergic rhinitis (hay fever), allergic conjunctivitis, or allergic asthma. Patients with atopy also have a tendency to have food allergies.
Patients with atopy usually develop what is referred to as the “allergic triad” of symptoms, i.e., eczema (atopic dermatitis), hay fever (allergic rhinitis), and allergy-induced asthma (allergic asthma). They also have a tendency to have food allergies, and other symptoms characterized by their hyperallergic state. |
|
|
note
|
For drug allergies, hypersensitivity type I and type IV are the most common.
|
|
|
Discuss the mechanism of type I hypersensitivity reactions.
|

|
|
|
Discuss the mechanism of type II hypersensitivity reactions. What are the most common conditions that cause this reaction?
|

|
|
|
Discuss the mechanism of type III hypersensitivity reactions. What are the most common conditions that cause this reaction?
|

|
|
|
Discuss the mechanism of type IV hypersensitivity reactions. What are the most common conditions that cause this reaction?
|

|
|
|
Discuss the mechanisms of the 4 hypersensitivity reactions.
|
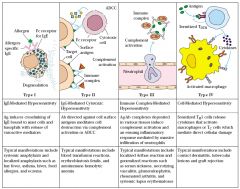
|
|
|
note
|
An epipen should be prescribed to every pt who has a history of or is at risk for anaphylaxis.
In adults: EpiPen - 0.3mg In children < 30kg EpiPen - 0.15mg NOTE: pts with any known drug allergy or previous major allergic reaction should get a MedicAlert bracelet. |
|
|
In the particular case of a child who recently developed an anaphylactic reaction (currently asymptomatic) to food, what would you do?
|
i. prescribe an epipen for the house, car, school, and daycare
ii. advise family to educate child, teachers, and caretakers about signs and Sx of anaphylaxis and about when and how to use the EpiPen. |
|
|
What are reticulocytes?
|
- reticulocytes are immature erythrocytes and are markers of erythrocyte production.
- should normally increase when there is a decrease in rbc. - with blood loss, reticulocytes should increase 2-3x initially and then 5-7x over the next week - a normal reticulocyte count in anemia should be interpreted as a sign of decreased production |
|
|
What is the definition of anemia?
|
a decrease in rbc mass that can be detected by hemoglobin (hb) concentration, hematocrit (hct), and rbc count
- adult males: Hb <135g/l or Hct <41% - adult females: Hb <120g/l or Hct <36% |
|
|
What is a blood film?
|

A blood film or peripheral blood smear is a thin layer of blood smeared on a microscope slide and then stained in such a way to allow the various blood cells to be examined microscopically. Blood films are usually examined to investigate hematological problems (disorders of the blood) and, occasionally, to look for parasites within the blood such as malaria and filaria.
|
|
|
Discuss an approach / classification of anemia.
|
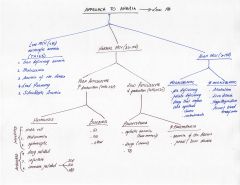
|
|
|
What are some key investigations for an anemia workup?
|
Initial tests:
- bw: cbc (hb, mcv, mch), reticulocyte count, ferritin On basis of initial testing, order 2° testing as needed: - bw_tsh, b12, ldh, unconjugated bilirubin, d-dimer, fibrinogen, pt, ptt - blood smear - fobt, colonoscopy other tests include: - (Cr, lfts) |
|
|
What are the main causes of microcytic anemia (mcv<80)?
|
pneumonic TAILS
i. thalessemia ii. anemia of chronic disease iii. iron deficiency anemia (most common) iv. lead poisoning v. sideroblastic anemia |
|
|
What are the causes of macrocytic anemia (mcv>100)?
|
megaloblastic
- b12 deficiency - folate deficiency - drugs that impair dna synthesis (methotrexate, chemo) non-megaloblastic - alcoholism - liver disease - hypothyroidism - recent blood transfusion ----------------------------------------------------- note: Especially common causes of macrocytic anemias are the so-called megaloblastic anemias, in which cells are larger because they cannot produce DNA quickly enough to divide at the right time as they grow, and thus grow too large before division. Causes of the DNA synthetic problem range from lack of certain vitamins needed to produce DNA (notably folate and B12), to poisons or inhibitors of DNA replication, such as some kinds of antiviral drugs and chemotherapeutic agents. Classically these megaloblastic types of anemias are associated also with more specific features, such as megaloblasts in the bone marrow, the presence of ovalocytes in the (peripheral) blood smear, and the pathognomonic presence of hypersegmented neutrophils. |
|
|
note
|
For iron deficiency anemia, treatment with iron supplements should continue for 3-6 months after lab values are normal to help replenish stores
|
|
|
What is thalessemia?
|
Thalassemia are forms of inherited autosomal recessive blood disorders that originated in the Mediterranean region. In thalassemia, the disease is caused by the weakening and destruction of red blood cells. Thalassemia is caused by variant or missing genes that affect how the body makes hemoglobin. Hemoglobin is the protein in red blood cells that carries oxygen. People with thalassemia make less hemoglobin and fewer circulating red blood cells than normal, which results in mild or severe anemia. Thalassemia will be present as microcytic anemia which may be differentiated from iron deficiency anemia using the mentzer index calculation.
Manifestations include: - growth stunted - bony deformities - hepatosplenomegaly - jaundice - cardiovascular illness |
|
|
How is the diagnosis of thalessemia made:
|
i. mentzer index (not the best test)
ii. hemoglobin electrophoresis (definitive diagnosis) __________________________________________________________ NOTE: The mentzer index is calculated from the results of a cbc. If the quotient of the mean corpuscular volume (MCV, in fL) divided by the red blood cell count (RBC, in Millions per microLiter) is less than 13, thalassemia is said to be more likely. If the result is greater than 13, then iron-deficiency anemia is said to be more likely. The principle involved is as follows: In iron deficiency, the marrow cannot produce as many RBCs and they are small (microcytic), so the RBC count and the MCV will both be low, and as a result, the index will be greater than 13. Conversely, in thalassemia, which is a disorder of globin synthesis, the number of RBC's produced is normal, but the cells are smaller and more fragile. Therefore, the RBC count is normal, but the MCV is low, so the index will be less than 13. (In practice, the MCV has to be extremely low and/or the RBC extremely high to produce an index of less than 13, something rarely encountered, further calling into question the usefulness of the index. |
|
|
define the various cbc parameters:
- hb - hct - mcv - mch - rbc count - rdw |
hb: amt of hemoglobin in the blood
hct: hematocrit of packed cell volume - fraction of whole blood volume that consists of rbcs mcv: mean corpuscular volume - the average volume of red cells mch: mean corpuscular hemoglobin - the average amount of hemoglobin per red blood cell rbc count: total number of rbcs in a volume unit rdw: red blood cell distribution width - the variation in cellular volume of the rbc population |
|
|
What is the management of thalessemia?
|
- allogenic bone marrow transplantation (treatment of choice)
- blood transfusions (for symptomatic control) - folate supplementation - deferoxamine (iron chelator) given to prevent 2° hemosiderosis is usually given concomitantly - prenatal diagnosis is available - genetic counseling should be offered to high risk families |
|
|
What is ferritin?
|
Ferritin is an intracellular protein that stores iron and releases it in a controlled fashion. The amount of ferritin stored reflects the amount of iron stored.
|
|
|
What is pernicious anemia?
|
Pernicious anemia is one of many types of the larger family of megaloblastic anemias. It is caused by loss of gastric parietal cells, which are responsible, in part, for the secretion of intrinsic factor, a protein essential for subsequent absorption of vitamin B12 in the ileum.
Usually seated in an atrophic gastritis, the autoimmune destruction of gastric parietal cells (and autoantibody inactivation of intrinsic factor) leads to a lack of intrinsic factor.[1] Since the absorption from the gut of normal dietary amounts of vitamin B12[2] is dependent on intrinsic factor, the loss of intrinsic factor leads to vitamin B12 deficiency. While the term 'pernicious anemia' is sometimes also incorrectly used to indicate megaloblastic anemia due to any cause of B12 deficiency, its proper usage refers to that caused by atrophic gastritis, parietal cell loss, and lack of intrinsic factor only. The loss of ability to absorb vitamin B12 (B12) is the most common cause of adult B12 deficiency.[3] Impaired absorption of vitamin B12 may be due to a loss of intrinsic factor or to a number of other conditions that decrease production of gastric acid, which also plays a part in the absorption of B12 from foods. |
|
|
What are the common causes of b12 deficiency anemia?
|
i. strict vegetarian diet
ii. pernicious anemia iii. gastrectomy iv. ileal dysfunction (crohn's disease, surgical resection) other causes include: alcohol abuse, liver disease, and hypothyroidism NOTE: pernicious anemia occurs when the gastric parietal cells (which make the intrinsic factor that help in b12 absorption) are destroyed. |
|
|
What is sickle cell anemia?
|
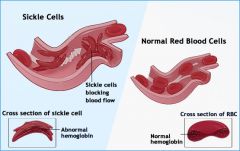
- autosomal recessive condition
- valine replaces glutamic acid at the sixth position in the globin chain - rbcs sickle under conditions of stress: dehydration, low pO2, fever, acidosis ----------------------------------------------------- This condition is predominantly seen among african-americans who have a strong family hx, symptoms include stigmata of hemolysis: - anemia - fever - jaundice - splenomegaly - dactylitis (often first presentation) - crisis: vaso-occlusive, aplastic, acute splenic sequestration ------------------------------------------------------ note: dactylitis or sausage digit is inflammation of an entire digit (a finger or toe), and can be painful. vaso-occlusive crisis (presents as fever and pain in any organ but most commonly in the long bones of arms and legs, chest, abdomen) aplastic crisis: depression of erythropoiesis generally assoc. w/ infection acute splenic sequestration: sudden, massive pooling of red cells in spleen, splenomegaly, tender spleen |
|
|
Explain how erythropoiesis works?
|
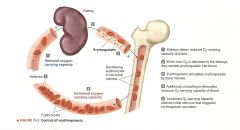
|
|
|
What is the diagnostic test for sickle cell anemia?
|
hemoglobin electrophoresis
|
|
|
What is the management of sickle cell anemia?
|
- vaccinations including: strep pneumoniae, influenza, h. influenzae type b, and hepatitis b
- educate pt to avoid dehydration, hypoxia, intense exercise, and high altitudes - transfusions for severe anemia, sickle cell crisis - antibiotic prophylaxis - folic acid supplementation In pts w/ frequent pain crisis consider: - hydroxyurea or bone marrow transplantation |
|
|
What are the signs/symptoms of anemia?
|
- fatigue
- malaise - dyspnea - palpitations - h/a - lightheadedness physical signs: - pallor - mucous membranes, skin, conjunctiva - tachycardia, orthostatic hypotension - jaundice (if due to hemolysis) |
|
|
What are the some conditions that atrial fibrillation is associated with?
|
cardiac conditions:
- htn - cad - chf - valvular heart disease - pericarditis/myocarditis non-cardiac causes - thyrotoxicosis - acute infections - PE - copd - dm - hypoxia - ingestions of caffeine, cocaine, alcohol |
|
|
What are some of the complications of atrial fibrillation?
|
- stroke
- chf - cardiomyopathy |
|
|
T/F. For atrial fibrillation, digoxin only provides rate control at rest.
|
True
|
|
|
note
|
For atrial fibrillation, there are NO differences between rate and rhythm control strategies in terms of cardiovascular events, strokes, or death.
In fact, rate control strategies lead to fewer s/e, and fewer hospital admissions. Therefore, rate control would be preferable to rhythm control in AF. However, rhythm control is recommended for patients with AF who remain symptomatic with rate control therapy or in whom rate control is unlikely to control symptoms. |
|
|
When is a β-blocker preferred over a CCB for rate control in atrial fibrillation? When is a CCB preferred over a β-blocker for rate control in atrial fibrillation?
|
β-blocker over CCB:
- angina - previous MI - left ventricular systolic dysfunction unless there are contraindications or the β-blocker cannot be tolerated in which case a CCB can be used ------------------------------------------------------------------------ CCB over β-blocker: - chronic pulmonary disease - those at risk of bronchospasm Avoid using for post MI pts and those w/ chf |
|
|
If medications fail to control the rate in atrial fibrillation or are not tolerated, what is another option for rate control?
|
PV ablation
|
|
|
What is the recommended goal of heart rate in patients who have atrial fibrillation?
|
<100
|
|
|
What is the difference between antiplatelet drugs and anticoagulants?
|
An antiplatelet drug is a member of a class of pharmaceuticals that decrease platelet aggregation and inhibit thrombus formation. They are effective in the arterial circulation, where anticoagulants have little effect. They are widely used in primary and secondary prevention of thrombotic cerebrovascular or cardiovascular disease. Common antiplatelet agents include:
- aspirin (asa) - clopidogrel (plavix) Anticoagulants reduce blood clotting. This prevents deep vein thrombosis, pulmonary embolism, myocardial infarction and stroke. Common anticoagulants include: - warfarin - heparin |
|
|
What is the average risk of stroke for patients with non-valvular atrial fibrillation.
|
4% per year.
Anticoagulation with warfarin or dabigatran (inr 2-3) reduces the risk of stroke by 50-68% compared w/ placebo. Aspirin reduces the risk of stroke by about 22-36%. |
|
|
What are the pros and cons of dabigatran compared to warfarin?
[atrial fibillation] |
dabigatran compared to warfarin
PROs - more efficacious - lower rates of intracranial bleeds - does not require frequent blood tests for INR monitoring, no freq. changes to dosing CONS - not reversible - given bid, so compliance may be poor - s/e - dyspepsia - long term safety and efficacy data unknown - 7x more expensive |
|
|
note
[atrial fibrillation] |
For older patients with atrial fibrillation, their risk of falling is NOT a significant factor when deciding on oral anticoagulation therapy. People taking warfarin must fall ~295x in 1 year for warfarin NOT to be the optimal therapy. A pt with a history of falls will have 1.8 falls/yr on average.
|
|
|
For a pt with atrial fibrillation requiring cardioversion, what are the requirements if any for anticoagulation?
|
- if AF <48h, can usually cardiovert w/o anticoagulation
- if AF >48h (or unknown duration), anticoagulate 3wks prior and 4wks after cardioversion - if pt unstable (hypotensive, shock, ischemic CP, acute heart failure), should cardiovert immediately; if time permits a transesophageal echo (TEE) and immediate anticoagulation w/ lmwh should be used |
|
|
Should an atrial fibrillation patient ever be on ASA and warfarin at the same time for MI and stroke prevention?
[atrial fibrillation] |
NO.
No benefit of asa+warfarin (antiplatelet and anticoagulant) over warfarin alone in MI or stroke prevention in pts w/ AF. But, bleeding risk is higher in asa+warfarin vs. warfarin alone. Therefore, asa should NOT be added to an oral anticoagulant for AF pts unless there is compelling indications for antiplatelet therapy (such as the presence of CAD). |
|
|
What are 2 strategies for lowering a pt's INR whose levels are above the therapeutic range of 2-3?
|
- withhold warfarin/reduce dose
- give Vit K (can be given oral or SC); although Vit K is typically given when the INR is much higher than 3.5 |
|
|
What is the dose of diltiazem for rate control in a patient w/ atrial fibrillation?
|
diltiazem 120mg - 480mg od
|
|
|
For a pt w/ atrial fibrillation who has a CHADS2 score ≥1, what should his INR be (therapeutic range)? Does his stroke risk go up if his INR is lower than the therapeutic range?
|
therapeutic range
INR 2-3 if INR <1.8, stroke risk doubles |
|
|
Discuss the classification of atrial fibrillation.
|
first-detected AF:
- symptomatic or asymptomatic - self-limited paroxysmal or persistent paroxysmal AF: - ≥2 episodes of AF lasting >30s - terminates spontaneously persistent AF: - sustained AF; may be recurrent paroxysmal AF - termination by electrical or pharmacological therapy does not change designation permanent AF: - long-standing AF (usually >1yr) - cardioversion has failed or not been indicated |
|
|
What are some physical signs to look for in atrial fibrillation?
|
- irregularly irregular pulse
- irregular jvp w/ absent a waves - variations in intensity of the 1st heart sound |
|
|
Name an anti-arrhythmic agent used for rhythm control in atrial fibrillation.
|
amiodarone
|
|
|
note
|
Propensity to fall is NOT a contraindication to anticoagulant treatment. People taking warfarin must fall ~295x to have a major bleed.
|
|
|
Discuss the 'SPIKES' protocol for breaking bad news.
|
|
|
|
What are some paediatric upper respiratory conditions and what is the DDx for stridor?
|
- croup
- bacterial tracheitis - epiglottitis - foreign body aspiration - subglottic stenosis: congenital or iatrogenic - laryngomalacia/tracheomalacia: collapse of epiglottis cartilage on inspiration - retropharyngeal abscess - peritonsillar abscess |
|
|
What are the causative agents in croup?
|
- parainfluenze (75%)
- influenza A and B - RSV - adenovirus |
|
|
What is the treatment for croup?
|
- Humidified O2
- Dexamethasone - racemic epinephrine: nebulized - intubation if not responsive to treatment note: dexamethasone dosing: same dose by oral, im, or iv 0.6mg/kg x 1 single dose [max: 10mg (16mg as per uptodate)] for epinephrine, they need to go to the ER and typically get epinephrine nebulized |
|
|
What is the clinical presentation in croup?
|
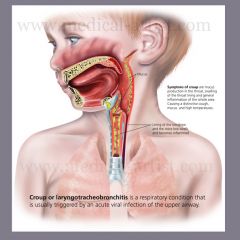
- stridor
- hoarseness - barky cough - worse at night note: the course of croup is fluctuating; it is a self-limited condition; it is contagious. * on CXR, one can see a 'steeple' sign (from subglottic narrowing) but this is NOT a reliable test as the steeple sign is often seen without croup. |
|
|
What is the DDx of wheezing in children?
|
COMMON
- asthma - bronchiolitis (first episode wheezing) - recurrent aspiration - pneumonia (fever, cough, malaise) UNCOMMON - cystic fibrosis - foreign body - bronchopulmonary dysplasia (often develops after prolonged ventilation in the newborn) |
|
|
Differentiate the following:
- croup (laryngotracheobronchitis) - bacterial tracheitis - epiglottitis |

|
|
|
T/F. Lower respiratory tract diseases produce more expiratory sounds such as wheezing, whereas upper respiratory tract diseases produce more inspiratory sounds such as stridor, hoarseness and suprasternal retractions
|
True
|
|
|
What would be the management for someone with bronchiolitis?
|
MILD DISTRESS:
- supportive: rehydration, antipyretics for fever - humidified O2 (maintain O2 sats > 92%) - inhaled bronchodilator by mask (ventolin) MODERATE to SEVERE DISEASE: - same as per mild distress plus: - ipratropium (Atrovent), note: steroids are not effective - nebulized epinephrine - antibiotics not necessary unless bacterial cause |
|
|
What is bronchiectasis?
|
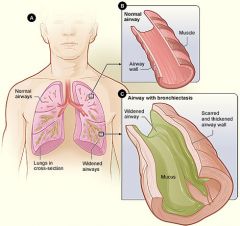
Bronchiectasis is a disease state defined by localized, irreversible dilation of part of the bronchial tree caused by destruction of the muscle and elastic tissue. It is classified as an obstructive lung disease, along with emphysema, bronchitis, asthma, and cystic fibrosis.
Involved bronchi are dilated, inflamed, and easily collapsible, resulting in airway obstruction and impaired clearance of secretions. Bronchiectasis may result from a variety of infective and acquired causes, including severe and recurrent pneumonia, tuberculosis, and cystic fibrosis. Some people with bronchiectasis may produce frequent green/yellow sputum (up to 240ml (8 oz) daily). Bronchiectasis may also present with hemoptysis in the absence of sputum, called "dry bronchiectasis". Sputum production may also occur without coloration. People with bronchiectasis may have bad breath indicative of active infection. Frequent bronchial infections and breathlessness are two possible indicators of bronchiectasis. |
|
|
What are the symptoms of a retropharyngeal infection / abscess?
|
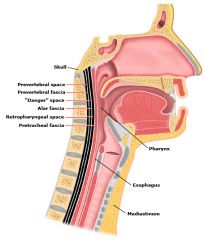
- dysphagia, odynophagia, and / or drooling
- unwillingness to move neck due to pain (torticollis) - “hot potato” voice, gurgling sounds - respiratory distress (stridor, tachypnea) - neck swelling, lymphadenopathy - trismus (spasm of the jaw muscles, causing the mouth to remain tightly closed, typically as a symptom of tetanus) - chest pain (if extension to mediastinum) investigations: - bw_cbc, blood cultures - xrays – lateral neck +/- CT w/ contrast management: - urgent referal to otolaryngologist - maintain airway - empiric abx treatment - surgical drainage if airway compromise |
|
|
What are some of the complications of acute sinusitis?
|
ORBITAL
- periorbital cellulitis - orbital cellulitis - subperiosteal abscess - orbital abscess INTRACRANIAL - meningitis - abscess BONY - osteomyelitis NEUROLOGIC - superior orbital fissure syndrome (CN III/IV/VI palsy, immobile globe, dilated pupils, ptosis) |
|
|
What is the 1st line treatment for mild to moderate pelvic imflammatory disease (PID)?
|
cefixime 800mg [single dose] + doxycycline 100mg BID x 14d
|
|
|
What are the causes of secondary headaches?
|
- 2° H/As are caused by underlying organic disease
- account for <10% of all headaches, may be life-threatening. They include: - space occupying lesion - giant cell arteritis - CNS infection (meningitis, encephalitis) - TMJ - traumatic head injury - stroke - aneurysm - SAH - systemic disorders (thyroid disease, HTN, pheochromocytoma) |
|
|
What are the symptoms of temporomandibular joint dysfunction (TMD)?
|
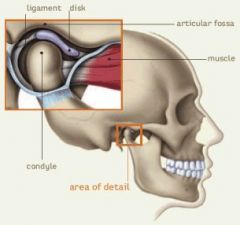
The most common presenting signs and symptoms of TMD are:
- acute or chronic facial pain triggered by jaw motion - dysfunction of the masticatory system - tmj tenderness - neck stiffness + pain - h/a - ear discomfort |
|
|
What is the management for individuals with anorexia nervosa?
|
i. admit to hospital if
- <65% of std body wt (<85% of std body wt for adolescents) - hypovolemia requiring IV fluids - heart rate < 40 - abnormal serum chemistry - actively suicidal ii. psychotherapy (individual psychotherapy, cbt, family therapy) iii. Monitor for refeeding syndrome REFEEDING SYNDROME: - potentially life-threatening metabolic response to re-feeding in severely malnourished patients resulting in severe fluid and electrolyte shifts - complications include hypophosphatemia, CHF, cardiac arrhythmias, delirium, and death - prevention: slow refeeding, gradual increase in nutrition, supplemental phosphorus, close monitoring of electrolytes and cardiac status NOTE: antidepressants for the treatment of anorexia nervosa have limited effectiveness and should NOT be used as the sole treatment modality. |
|
|
What is the management for bulimia nervosa?
|
Hospitalization: for significant electrolyte/fluid abnormalities.
BIOLOGICAL - SSRIs - treatment for starvation effects PSYCHOLOGICAL - psychotherapy: cbt, interpersonal therapy - group therapy note: cbt combined with antidepresants are more effective than cbt alone or antidepressants alone note: wellbutrin is contraindicated in these pts as it lowers the seizure threshold, and patients who purse are more likely to have electrolyte disturbances and hence seizures |
|
|
What is the diagnostic criteria for bulimia nervosa?
|
A. Recurrent episodes of binge eating. An episode of binge eating is characterized by both of the following:
i. eating in a discrete period of time, an amount that is definitely larger than most people would eat in a similar period under similar circumstances ii. a sense of lack of control over eating during the episode (eg. feeling that one cannot stop eating or control what or how much one is eating) B. recurrent inappropriate compensatory behaviour in order to prevent weight gain, such as self-induced vomiting, misuse of laxatives, diuretics, fasting, or excessive exercise C. the binge eating and inappropriate compensatory behaviour both occur on avg at least 2x a week for 3 months D. self-evaluation is unduly influenced by body shape and weight E. the disturbance does not occur exclusively during episodes of anorexia nervosa 2 types: purging and non-purging |
|
|
What are some compensatory mechanisms for preventing weight gain used by patients with bulemia nervosa?
|
- self-induced vomiting
- laxatives - diuretics - fasting - excessive exercising |
|
|
What is the diagnostic criteria for anorexia nervosa?
|
A. REFUSAL to maintain body weight at or above a minimally normal weight for age and height (e.g. weight loss leading to maintenance of body weight < 85% of that expected; or failure to make expected weight gain during period of growth, leading to body weight < 85% of that expected)
B. intense FEAR of gaining weight or becoming fat, even though underweight C. disturbance in the way in which one's body wt or shape is experienced, undue influence of body wt or shape on self-evaluation, or denial of the seriousness of the current low body weight D. In postmenarcheal females, amenorrhea, i.e. the absence of at least 3 consecutive menstrual cycles 2 types: Restricting and binge-eating/purging Anorexia Nervosa is also associated with: deteriorating mood, isolation, trouble concentrating, malnutrition, and poor sleep |
|
|
What is the Athletic Triad?
|
- disordered eating
- amenorrhea - osteoporosis |
|
|
Discuss the epidemiology of anorexia nervosa (AN) and bulimia nervosa (BN).
|
anorexia nervosa
- 1% of adolescent and young adult females; onset 13-20yrs bulemia nervosa - 2-4% of adolescent and young adult females; onset 16-18yrs F:M ratio is 10:1 |
|
|
Discuss some of the risk factors for anorexia nervosa and bulimia nervosa?
|
- obesity
- chronic medical illness (dm type I) - career choice with expectations of being thin (gymnast, dancer, models) - competitive athletes - family history of mood/eating disorders - sexual abuse - other psychiatric illness (depression, anxiety, ocd) - poor self-esteem - substance abuse (specifically for BN) |
|
|
What is a useful screening tool for eating disorders (anorexia nervosa, bulimia nervosa)?
|
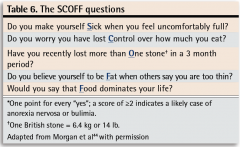
SCOFF
- 12.5% false positive rate - not diagnostic for eating disorders |
|
|
note
|
Amenorrhea is part of the criteria for anorexia nervosa in postmenarcheal females.
|
|
|
Discuss the physiological complications of eating disorders.
|

|
|
|
What are some co-existing psychiatric conditions associated with eating disorders?
|
- depression (lifetime prevalence in anorexia nervosa - 80%)
- anxiety disorders: especially panic disorder, agoraphobia - ocd - substance abuse - personality disorders |
|
|
Compare some of the features of anorexia nervosa and bulimia nervosa?
|

|
|
|
note
|
When assessing a patient presenting with a problem that has defied diagnosis. Eg:
- arrhythmias w/o cardiac disease - electrolyte imbalance w/o drug use or renal impairment - amenorrhea w/o pregnancy Think of 'eating disorder' in the DDx |
|
|
What would be the DDx for 'eating disorder'?
|
- anorexia nervosa
- bulimia nervosa - dm - hyperthyroidism - malnutrition - immunodeficiency - IBD |
|
|
Broadly list the main categories of an 'eating disorder' history.
|
i. weight history
ii. desired weight iii. perception of current shape and size iv. preoccupations v. dietary patterns vi. binge-pattern eating vii. inappropriate compensatory mechanisms |
|
|
What is Russell's sign?
|

Calluses on the knuckles or back of the hand due to repeated self-induced vomiting over long periods of time. The condition generally arises from the afflicted's knuckles making contact with the incisor teeth during the act of inducing the gag reflex at the back of the throat with their finger(s).
|
|
|
T/F. If a man has ≥3 urinary tract infection (uti) in 1 year, he should be referred to urology.
|
True
|
|
|
What are some characteristics that increase the risk of medication related problems in the elderly?
|
- age ≥85
- ≥4 meds - multiple doses per medication / day - >6 active chronic medical diagnoses - kidney disease - low bmi - previous failure to take medications appropriately - previous adverse drug reactions |
|
|
What is the formula for creatinine clearance?
|
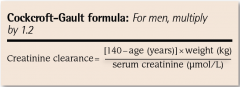
|
|
|
In the elderly, which drugs should be:
- avoided - caution advised |
drugs to avoid:
- anticholinergics (inc. risk of delirium, urinary retention, constipation, glaucoma) - antiarrhythmics - antiemetics - antihistamines - antiparkinson agents - antipsychotics - antispasmodics - skeletal muscle relaxants - TCAs benzodiazepines (inc. risk of falls, fractures, MVCs, and delirium) _______________________________________________________ drugs to be careful with: - antibiotics (esp. with impaired CrCl) - nsaids (may worsen chf and peptic ulcer disease) - antidepressants (esp. TCAs) - anticonvulsants (risk of thrombocytopenia, hepatotoxicity) _______________________________________________________ |
|
|
What are some strategies to enhance drug safety in the elderly?
|
- review meds regularly
- start low, go slow - try safer alternatives when possible - warn pts of side effects of drugs - adjust drugs based on CrCl - in liver failure, be careful with drugs that undergo hepatic metabolism |
|
|
note
|
In the elderly pt, it is important to inquire about non-prescription medication use (eg. herbal medicine, cough drops, over-the-counter drugs, vitamins)
- herbal meds are widely used by the elderly and 1/3 of users are at risk for a herb-drug interaction (most common interaction -> ginkgo with aspirin) |
|
|
List 3 common herbal medications taken by the elderly and discuss their interactions.
|
i. Ginkgo (interacts w/ asa, nsaids, warfarin)
ii. St. John's Wort (interacts w/ ssris, TCAs) iii. Ginseng (interacts w/ warfarin) |
|
|
note
|
In the elderly patient, screen for modifiable risk factors (e.g. visual disturbance, impaired hearing) to promote safety and prolong independence.
In the elderly patient, assess functional status to: - anticipate and discuss the eventual need for changes in the living environment - ensure that social support is adequate In older patients with diseases prone to atypical presentation, do not exclude these diseases without a thorough assessment (e.g. pneumonia, appendicitis, depression). |
|
|
Diagram of eustachian tube.
|
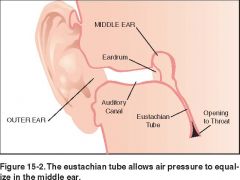
|
|
|
Diagram of normal appearing tympanic membrane. (r. tm)
|
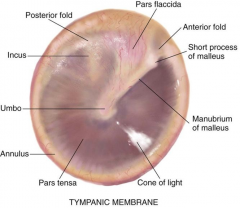
|
|
|
Diagram of otitis media with effusion.
|

|
|
|
What is otitis media with effusion? What are the clinical features of OME?
|

Presence of fluid in the middle ear without signs or symptoms of ear infection. Frequently follows acute otitis media in children.
clinical features: - hearing loss ± tinnitus - aural fullness - ±otalia, low gr. fever otoscopy: - amber or dull grey - meniscus fluid level behind tm - air bubbles - retraction pockets/tm atelectasis investigations: - audiometry - tympanogram treatment: - 90% resolve by 3 months - NO antibiotics (no benefit) - surgery: myringotomy ± ventilation tubes ± adenoidectomy (if enlarged) complications of ome: - hearing loss - speech delay - learning problems - ossicular erosion - cholesteatoma |
|
|
What is sialadenitis?
|
Inflammation of a salivary gland, typically caused by sialolithiasis (salivary gland stone)
Management: i. ++fluids, discontinue/reduce anticholinergics if appropriate ii. massage gland w/ moist cloth iii. nsaids (eg. naproxen 500mg bid x 5d; then prn M: 20 tablets) iv. keflex 500mg qid x 7d v. rtc if symptoms persisting, recurrent, develop fever; may need ent referral |
|
|
What are the 3 major salivary glands?
|
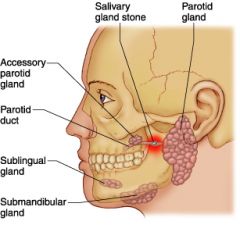
i. parotid
ii. submandibular iii. sublingual |
|
|
What is sialolithiasis? What are some RFs associated w/ sialolithisis? What investigations can one do for this condition?
|
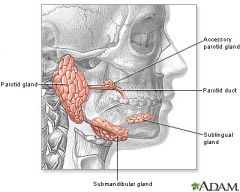
The presence of stones or calculi in the salivary glands or ducts.
- >80% of stones are from the submandibular glands - ~20% of stones are from the parotid glands - 1-2% of stones are from the sublingual and other minor glands The submandibular gland is more prone to stone formation b/c the duct is long and large (flow of saliva is slow and against gravity) ------------------------------------------------------------------ RFs associated with salivary gland stones: - dehydration - diuretics - anti-cholinergics - trauma - gout - smoking ------------------------------------------------------------------ Investigations: - u/s (better than xray) - xray - sialography (dye injected into duct and xray taken) - CT (modality of choice, but must weight in radiation risks) |
|
|
What is autonomic dysreflexia?
|
Autonomic dysreflexia (AD), also known as autonomic hyperreflexia, is a potentially life threatening condition which can be considered a medical emergency requiring immediate attention. AD occurs most often in spinal cord-injured individuals with spinal lesions above the T6 spinal cord level, although it has been known to occur in patients with a lesion as low as T10.
Acute AD is a reaction of the autonomic (involuntary) nervous system to overstimulation. It is characterized by: - paroxysmal hypertension (the sudden onset of severe high blood pressure) associated with throbbing headaches, profuse sweating, nasal stuffiness, flushing of the skin above the level of the lesion - slow heart rate - anxiety - cognitive impairment The sympathetic discharge that occurs is usually in association with spinal cord injury (SCI) or disease (e.g. multiple sclerosis). AD is believed to be triggered by afferent stimuli (nerve signals that send messages back to the spinal cord and brain) which originate below the level of the spinal cord lesion. It is believed that these afferent stimuli trigger and maintain an increase in blood pressure via a sympathetically mediated vasoconstriction in muscle, skin and splanchnic (gut) vascular beds. |
|
|
What is meant by diabetic autonomic neuropathy?
|
CVS: orthostatic hypotension (most common)
GI: gastroparesis (delayed gut motility), nausea, bloating, diarrhea GU: inc. urinary freq, urgency, incontinence |
|
|
T/F. Children with recurrent ear infections should be checked for hearing loss and/or speech delay.
|
True
|
|
|
What is the differential diagnosis of earaches?
|
- acute otitis media
- otitis media with effusion - otitis externa - tmj - tooth abscess - trigeminal neuralgia - pharyngitis - sinusitis - tumor * temporal arteritis * mastoiditis * malignant (necrotizing) otitis externa * serious causes |
|
|
What is the DDx for pruritis?
|

|
|
|
What investigations would you do for pruritis?
|
If no obvious source such as eczema and suspicious of a systemic cause, then:
bloodwork: - cbc, lytes - Cr, bun, alt, alp, ast, bilirubin - ferritin, b12 - tsh, glucose - esr, crp |
|
|
What are the clinical features of acute otitis media (aom)? What are the physical features of aom?
|

Triad of:
i. otalgia ii. fever iii. hearing loss (conductive) - otorrhea if tm perforated - rarely tinnitus, vertigo, and/or facial nerve paralysis infants and toddlers may present w/: - ear tugging - irritability, dec. sleep - vomiting, diarrhea, dec. appetite --------------------------------------------------------------------- o/e: i. hyperemia ii. bulging, pus may be seen behind tm iii. loss of landmarks (tm) iv. dec. mobility of tm |
|
|
What is mastoiditis?
What are the clinical features? What is the management? |

Mastoiditis requires IV Abx and urgent ent referral for surgical debridement.
|
|
|
What is malignant (necrotizing) otitis externa?
|
- osteomyelitis of the temporal bone
- occurs in elderly diabetics and immunocompromized pts - complication of otitis externa - Sx of otalgia and purulent otorrhea that is refractory to medical therapy; granulation tissue present on floor of auditory canal. - requires hospital admission, IV abx, and debridement |
|
|
What is the criteria for the diagnosis of giant cell arteritis (GCA)/temporal arteritis?
|

|
|
|
What are the signs / symptoms of giant cell arteritis? What is the treatment for this condition? What is a cardiac complication of this condition?
|

|
|
|
How do you determine who / who not to give antibiotics to for acute otitis media?
|

|
|
|
What is the single most effective modifiable risk factor in preventing otitis media with effusion in children?
|
avoiding exposure to passive smoking
|
|
|
For how long should children w/ acute otitis media be treated for?
|
5 days for children ≥ 2 yrs
10 days if child - <24mo - perforated ear drum - recurrent aom - failure of 1st line agents |
|
|
What are some indications for myringotomy and tympanostomy tubes in recurrent acute otitis media and otitis media with effusion (tubes commonly inserted for ome, rarely for aom)?
|
- persistent effusion >3 mo
- lack of response to >3 mo of abx - recurrent aom (>7x in 6 mo) - bilateral conductive hearing loss of >20dB - chronic retraction of tm - complications of aom (eg. mastoiditis, meningitis) |
|
|
List 5 complications of acute otitis media.
|
i. tm perforation
ii. ossicular necrosis iii. persistent effusion (leading to hearing loss) iv. mastoiditis v. meningitis |
|
|
Discuss the following gender-specific topics that may present differently in males vs. females
- CAD in females - depression in males - alcohol/street drugs - eating disorders |
cad in females
- leading cause of death in females in NA; ~2x all Ca related deaths in females - atypical cp presentation - exercise stress test is inferior to nuclear stress test depression in males - may not be as forthcoming as females - males more liekly to commit suicide than females (4:1) - 2nd most common cause of death for ages 15-24 alcohol/street drugs - more common in males than females eating disorders - should consider in males as well; f:m ratio 10:1 - especially if high intensity athlete |
|
|
Distinguish between substance abuse and dependance.
|

|
|
|
Discuss the CAGE questionnaire.
|
C ever feel the need to CUT DOWN on drinking?
A nnoyed at criticism of drinking? G ever feel GUILTY about drinking too much? E eye opener - ever need a drink 1st thing in the morning? For men ≥2 is a positive screen; for women ≥1 is a positive screen. If positive CAGE, then assess further to distinguish between problem drinking and alcohol dependance. |
|
|
Discuss how you would identify and manage domestic violence.
|
|
|
|
note
|
In a child presenting with croup, it is important to identify the need for respiratory assistance.
- assess ABCs - respiratory distress: paradoxical breathing, intercostal indrawing, grunting, nasal flaring - impending respiratory failure: fatigue, somnolence/change in loc, dec. breath sounds, dusky colour, decreased retractions Intubate as needed |
|
|
How do you differentiate between an upper respiratory tract infection vs. a lower respiratory tract infection?
|

|
|
|
note
|
Croup is a clinical diagnosis, and once the diagnosis is made, treatment should follow with avoidance of cxr unless other etiology is suspected (eg. pneumonia).
i.e. judicious use of xrays Do not obtain if pt is respiratory distress as airway obstruction can compromise airway rapidly. These pts need immediate attention (eg. epinephrine, intubation etc.) |
|
|
When should dexamethasone be used for croup?
|
When a diagnosis of croup is made (i.e. stridor, hoarseness, barky cough, worse at night)
Even with a mild case of croup, giving dexamethasone is warranted prescription: dexamethasone dosing: same dose by oral, im, or iv 0.6mg/kg x 1 single dose [max: 16mg] |
|
|
Arrangement the following in decreasing severity of GI bleed:
melena, hematochezia, occult blood, hematemesis |
hematochezia > hematemesis > melena > occult blood
|
|
|
What are the top 2 causes of UGI bleed in rank order?
|
1. peptic ulcer disease (PUD)
2. esophageal varices |
|
|
Esophageal varices are associated with massive upper GI bleeding. True or False
|
True
|
|
|
Discuss management for patient with UGI bleed (e.g. patient presents with melena/hematemesis)
[upper gastrointestinal bleed] |
- ABCs
- Stabilize patient (IV fluids, 2 large bore IVs, monitor) - CBCs, lytes, Plt, PT, PTT, RFT, LFTs - KEEP NPO - NG tube to determine upper vs lower GI bleeding - endoscopy - establish bleeding site and treat lesion: inject epinephrine, sclerosants (ethanol), thermal hemostasis, bipolar electrocoagulation, endoclips - if stable non-variceal bleed and endoscopy not available - then IV PPI or high oral dose PPI - for variceal bleeds - octreotide |
|
|
T/F. Diverticulitis DOES NOT bleed typically; however, diverticulosis CAN bleed
|
True
|
|
|
What is angiodysplasia?
|

In medicine (gastroenterology), angiodysplasia is a small vascular malformation of the gut. It is a common cause of otherwise unexplained gastrointestinal bleeding and anemia. Lesions are often multiple, and frequently involve the cecum or ascending colon, although they can occur at other places. Treatment may be with endoscopic interventions, medication, or occasionally surgery.
|
|
|
How do internal vs external hemorrhoids present symptomatically?
|
INTERNAL HEMORROIDS
- bleeding NO pain EXTERNAL HEMORRHOIDS - pain and bleeding |
|
|
Discuss the ddx for upper GI bleed (often present with melena or hematemesis).
|
Above GE junction:
- epistaxis - esophageal varices - esophagitis - esophageal Ca - Mallory-Weiss Tear Stomach - gastritis - ulcer - Ca Duodenum - Ca Coagulopathy - anticoagulants (warfarin) - blood clotting disorder |
|
|
What is Horner's syndrome?
|

Horner's syndrome is a sympathetic defect
- ptosis (droopy eyelid) - miosis (constricted pupil) - anhydrosis (lack of sweating) One can do a clinical confirmation with cocaine test: cocaine does not dilate a miotic Horner's pupil |
|
|
note
|
It is important to ask about nsaid/aspirin or anticoagulant therapy in GI bleed.
|
|
|
What are esophageal varices? What is the management of an esophageal variceal bleed?
|
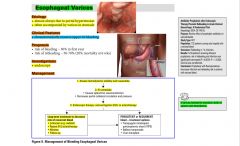
|
|
|
What is a mallory-weiss tear?
Etiology? Presentation? Management? |

|
|
|
note
|
When suspecting lower GI bleed, first and foremost exclude upper GI bleeding before localizing the site of the lower GI bleed.
|
|
|
What are the approach to hematochezia?
|
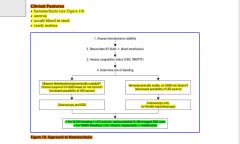
|
|
|
What is CEA?
|
CEA is not used to diagnose or screen for colorectal cancer, but it’s the preferred tumor marker to help predict outlook in patients with colorectal cancer.
The normal range of blood levels varies from lab to lab, and smokers often have higher levels. But even in smokers, levels higher than 5.5 ng/mL are not normal. The higher the CEA level at the time colorectal cancer is detected, the more likely it is that the cancer is advanced. CEA is the standard marker used to follow patients with colorectal cancer during and after treatment. In this way CEA levels are used to see if the cancer is responding to treatment or if it has come back (recurred) after treatment. |
|
|
note
|
melena is rarely present in lower GI bleeds
|
|
|
What are dietary causes of melena?
|
- black licorice
- blueberries - lead - peptobismol - Fe supplementation |
|
|
What is pepto-bismol?
|
Pepto-Bismol is an over-the-counter drug used to treat minor digestive system upset. Its active ingredient is bismuth subsalicylate. The primary symptoms aided by Pepto-Bismol are diarrhea, nausea, heartburn, indigestion, upset stomach, and other temporary discomforts of the stomach and GI tract.
Bismuth subsalicylate (the active ingredient in Pepto-Bismol) is used as an antidiarrheal and to treat some other gastro-intestinal diseases (oligodynamic effect, which relates to killing microbes with small doses of heavy metals). |
|
|
What are some RFs for upper GI bleeds?
|
- ++ alcohol
- chronic nsaid use - h. pylori infection - previous GI bleed |
|
|
note
|
With regards to screening for upper GI bleeds, all those pts with cirrhosis should have an endoscopy
- no varices: repeat q3 years - small varices: repeat q1-2yrs |
|
|
What are some options to reduce the risk (prophylaxis)of an UGI bleed from esophageal varices?
|
i. β-blocker (non-selective: eg. propanolol, nadolol)
ii. nitrates iii. endoscopic variceal ligation (EVL) or sclerotherapy |
|
|
What would you look for on physical exam if you were suspicious of esophageal varices based on history?
|
stigmata of liver disease
- jaundice - palmar erythema - ascites - caput medusa - splenomegaly |
|
|
How does the scheduling of the well baby visits work?
|
as per the rourke guide:
- within 1 wk - 2 wks (optional) - 1 mo - 2 mo - 4 mo - 6 mo - 9 mo - 12 mo - 15 mo - 18 mo - 2 yrs - 3 yrs - 4 yrs - 5 yrs |
|
|
The rourke baby record is divided into 5 guides. What are the areas that are addressed within each visit?
|
There are a total of 8 categories:
i. growth (wt, ht, hc) ii. parental concerns iii. nutrition iv. education and advice v. development vi. physical exam vii. problem and plan viii. immunization |
|
|
note
|
When measuring the growth of an infant, it is important to use corrected age for premature infants born < than 37 weeks gestation at least till 24-36 months.
|
|
|
At what age should a baby be 2x birth weight, 3x birth weight.
|
2x birth weight = 6 months
3x birth weight = 12 months |
|
|
Till what age are the following parameters checked?
- wt - ht - hc |
weight: 0-5 yrs
length/height: 0-5 yrs head circumference: from 0 - 2yrs |
|
|
Discuss normal physical growth with respect to bw, length/height, and hc.
|
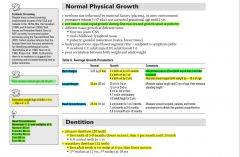
|
|
|
What is the criteria for failure to thrive?
|
i. wt <3rd percentile or
ii. falls across 2 major percentile curves iii. <80% of expected wt |
|
|
What are the energy requirements in an infant by weight?
|
0-10kg: 100 cal/kg/d
11-20kg: 1000 cal + 50 cal/kg/d for each kg>10 >21kg: 1500 cal + 20 cal/kg/d for each kg>20 |
|
|
Discuss failure to thrive. What questions would you ask on hx? What would you do on physical exam?
|
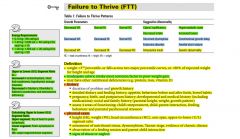
|
|
|
What investigations would you consider doing in a child who presents with failure to thrive?
|

|
|
|
What is considered obesity in children with regards to bmi?
|
bmi >95th percentile for age and height
|
|
|
Discuss necessary supplements for breast-fed babies.
|
i. vitamin K (given IM at birth)
ii. vitamin D (Ddrops) 400IU/d, 800IU/d in northern communities iii. fluoride: (after 6 months if not sufficient in water supply) iv. iron: from 4mo to 6mo (iron fortified cereals or ferrous sulphate solution) |
|
|
What causes breastfeeding jaundice?
|
Occurs in the first 1-2 weeks. Due to lack of milk production and subsequent dehydration.
|
|
|
T/F. Jaundice in the first 24 hrs and conjugated hyperbilirubinemia are always pathological?
|
True
|
|
|
What are the causes of neonatal jaundice in the first 24 hrs?
|
ALWAYS PATHOLOGICAL
HEMOLYTIC - Rh or ABO incompatibility SEPSIS - GBS - Congenital infection (TORCH) |
|
|
Differentiate breastfeeding jaundice from breast milk jaundice?
|
BREASTFEEDING JAUNDICE
- common - due to lack of milk production and subsequent dehydration, leading to exaggerated physiologic jaundice BREAST MILK JAUNDICE - rare - inhibitor of glucoronyl transferase found in breast milk - onset 7 days of life, peak at 2nd to 3rd week of life |
|
|
What is kernicterus?
|
- Neurological condition caused when unconjugated bilirubin concentrations exceed the albumin binding capacity, which causes bilirubin to enter and deposit in the brain resulting in permanent brain damage (often basal ganglia and brain stem).
- Increased incidence when bilirubin levels > 340 umol/L. Can also occur with lower levels in presence of sepsis, meningitis, hemolysis, hypoxia, hypothermia, hypoglycaemia, and prematurity - CLINICAL PRESENTATION: Acute form - lethargy, hypotonia, poor feeding, high-pitched crying, emesis, seizures. May then develop hypertonia, fever, opisthotonic posturing, bulging fontanelle, pulmonary hemorrhage. In its chronic form - hypotonia, delayed motor skills, extrapyramidal abnormalities, gaze palsy, MR, sensorineural hearing loss. This condition can be prevented by doing exchange transfusion. |
|
|
Explain breastfeeding with respect to a) signs of inadequate intake; b) feeding schedule; c) supplements that are required?
|

|
|
|
What are some contraindications to breastfeeding?
|
mother
- chemotherapy or radioactive compounds - HIV/AIDS, active TB, herpes in breast region - alcohol or illicit drugs - certain meds: bromocriptine, diazepam, metronidazole, tetracycline, lithium, antimetabolites NOTE: OCPs are not contraindicated to breastfeeding |
|
|
What are the advantages of breast feeding?
|
Current recommendation is exclusive breastfeeding for first 4 months of life
- easily digested - low renal solute load - immunologic - lower allergenicity - lower pH promotes growth of lactobacillus in the GI tract (protective against pathogenic intestinal bacteria) - cheap, readily available - parent child bonding |
|
|
What is mastitis, how does it occur, and what is the treatment for it ?
|

Mastitis (complication of breastfeeding) is the inflammation of breast tissue. S. aureus is the most common etiological organism responsible, but S. epidermidis and streptococci are occasionally isolated as well.
TREATMENT - cold compresses between feeds - cloxacillin for mother - continue nursing +/- I & D |
|
|
How would one treat unconjugated hyperbilirubinemia?
|
- this is done to prevent kernicterus
- treat the underlying cause (eg. sepsis) 1) PHOTOTHERAPY (insoluble unconjugated bilirubin is converted to excitable form via photoisomerization; need to monitor serum bilirubin during and immediately after therapy as there is a risk of rebound, b/c photoisomerization is reversible when phototherapy is discontinued). S/E include hypernatremic dehydration, skin rash, eye damage, diarrhea. CONTRAINDICATED in conjugated hyperbilirubinemia as it results in a 'bronzed' baby (due to production and accumulation of a toxic metabolite). 2) EXCHANGE TRANSFUSION - prevents toxic effects of bilirubin by removal from body. Indicated when there are high bilirubin levels as per published graphs based on age, weeks gestation. Most commonly performed for hemolytic disease and G6PD. |
|
|
What is the main cause of 'milk caries' in children?
|
often occurs in children put to bed with a bottle of milk or juice
|
|
|
T/F. ankyloglossa (aka tongue tie) is NOT a contraindication for breast feeding.
|
True
|
|
|
Discuss weaning with respect to breast feeding.
|
- allow slow progressive weaning whenever possible.
- introduce iron fortified infant cereals as first solid food at 6mo - soy based formulas not recommended for term infants and contraindicated for preterm infants - transition to low fat diets starts at 2yrs and canada's food guide is followed |
|
|
What is the difference between a mastitis and breast abscess?
|

|
|
|
For the 'education and advice' section on the rourke baby record, what are some things to discuss with the parent?
|
- car seat
- sleeping position - carbon monoxide/smoke detectors - hot water checks - childproofing electrical outlets - choking/safe toys - stair gates - poisons - soothability - parent child interaction - toilet training - sleep - familial stressors - second hand smoke - dental care - bike helmets |
|
|
T/F. As per the Canadian Pediatric Society recommendations, children <6 yrs should not be given cold and cough medications.
|
True
|
|
|
Discuss the pediatric developmental milestones. Note key milestones are at 12mo, 2yrs, 3yrs, 4 yrs.
|
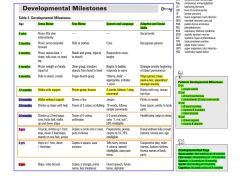
|
|
|
What are the developmental red flags with respect to:
- gross motor - fine motor - speech - social - cognitive |
gross motor: not walking at 18mo
fine motor: handedness at <10mo speech: <3 words at 18mo social: not smiling at 3mo cognitive: no peek-a-boo at 9mo |
|
|
All immunization vaccines are given IM, except for 2. What are these 2 and how are they given?
|
i. MMR
ii. Varicella Given SC |
|
|
What are contraindications to any vaccine?
When one might consider delaying giving the vaccine What are possible side effects/adverse reactions? |
contraindications:
i. hx of anaphylaxis to vaccine/vaccine component ii. significant immunocompromised pts (no live vaccines) iii. pregnant pts (no live vaccines) delay vaccinations if: i. moderate-severe illness ± fever (no need to delay vaccination for mild urti, rash, aches, pains, antibiotic use, or local reactions) ii. hx of being treated with blood products (delay live vaccines for 3+ months for optimal efficiency iii. if live vaccines are not given on the same day (mmr and varicella), then these vaccines should be given by a time interval of 28days or more ----------------------------------------------------------------- possible side effects/adverse reactions - local: induration or tenderness (mmr v. painful) - systemic: rash, fever - allergic: urticaria, rhinitis, anaphylaxis note: Tylenol can be used for pain / fever relief 1/2 hr prior to the injection of after injection. note: live vaccines are mmr and varicella |
|
|
T/F. Premature infants who are doing well clinically should be immunized with age appropriate doses of vaccines at the same chronological age and according to the same schedule as full term infants.
|
True.
This means that a baby born at 34 wks GA, will get the first set of immunizations at 2 months after birth and follow the same schedule as a term baby. |
|
|
What are the three main classes of chemical restraints?
|
i. benzodiazepines (eg. lorazepam)
ii. typical antipsychotics (haloperidol) iii. atypical antipsychotics (risperidone) |
|
|
i. For a pt w/ agitation due to drug intoxication or withdrawal, which chemical restraint should be used?
ii. For patient with agitation with a known psychiatric disorder, which chemical restraint should be used? |
i. benzodiazepine
ii. typical or atypical antipsychotic NOTE: For severely violent patients requiring immediate sedation, one can use an acting typical antipsychotic or benzodiazepine alone or in combination. |
|
|
What is normal (physiological) vaginal discharge?
|
- 1-4mL fluid / 24hrs
- white or transparent, thick, usually odourless - pH 4-4.5 - formed by mucoid endocervical secretions, sloughing epithelial cells, bacteria, vaginal transudate - increases with pregnancy, OCPs, mid-cycle, pcos (i.e. high estrogen states) NOTE In patients with no worrisome features on history or physical, and negative tests, make a positive diagnosis of physiological discharge and communicate it to the patient to avoid recurrent consultation, inappropriate treatment, and investigation in the future. |
|
|
Explain how the contraceptive ring (nuvaring) works?
|
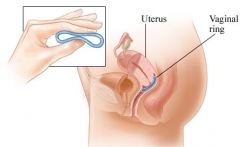
- thin flexible plastic ring
- works for 3 weeks then removed for 1 week to allow menstruation - Avoids first pass effect - S/E: vaginal infection/irritation, vaginal discharge - may have better cycle control, i.e. decreased breakthrough bleeding |
|
|
How would you treat endometriosis?
|
MEDICAL
- nsaids - anaprox/naproxen - ocp, depo-provera (medroxyprogesterone) - danazol - gnrh agonists (lupron) - suppress pituitary SURGICAL - conservative laparoscopy using laser ablation, electrocautery +/- laparotomy - definitive: bso + hysterectomy |
|
|
The transdermal (Ortho Evra) hormonal patch method should not be applied where?
|
breast
It is applied to the buttocks, back, upper arms, lower abdomen. Worn for 3 consecutive weeks (changed weekly), with 1 week off to allow menstruation. This method may be less effective in women > 90Kg |
|
|
What are complications of PID?
|
- Infertility
- Ectopic pregnancy - Abscesses - Chronic pelvic pain - Peritonitis - Intestinal obstruction - Disseminated disease (sepsis, arthritis, meningitis, endocarditis) - Fitz-Hugh-Curtis syndrome (involves liver capsule inflammation) NOTE: Fitz-Hugh-Curtis syndrome is a rare complication of PID. The symptoms are acute onset, RUQ abdo pain and tenderness aggravated by breathing, coughing or movement, and referred to the right shoulder following an episode of PID |
|
|
note
|
Menopause is a clinical diagnosis. BW is not necessary unless it is occurring quite early.
|
|
|
Define the following:
- menopause - postmenopause - premature menopause |
Menopause
- 12 months of amenorrhea after lmp Postmenopause - early: first 5 years after the final menstrual period. It is characterized by further and complete dampening of ovarian function and accelerated bone loss. Many women in this stage continue to have hot flashes. - late: period between 5 yrs after lmp and death Premature menopause: - menopause before 40 years of age |
|
|
Compare the 3 commonest causes of infectious vulvovaginitis?
|

|
|
|
What are the causes of vaginitis?
|
MOST COMMON
i. bacterial vaginosis (40-45%) ii. vulvovaginal candidiasis (20-25%) iii. trichomoniasis (15-20%) OTHERS - atrophic vaginitis (usually postmenopausal) - lichen sclerosis - vulvar cancer - cervicitis - foreign body (toilet paper - most common) - contact dermatitis - irritants, allergens - colovaginal fistula |
|
|
What are some symptoms of vaginitis?
|
- pruritis
- discharge - odour - vulval erythema - vaginal bleeding - post-coital spotting - dysparunia |
|
|
note
|
In patients with recurrent vaginal discharge, no worrisome features on history and physical examination, and negative tests, make a positive diagnoses of physiological discharge and communicate it to the patient to avoid recurrent consultation, inappropriate treatment, and investigation in the future.
|
|
|
What are some factors that may alter the vaginal environment, thereby allowing for vaginitis potentially?
|
- age
- antibiotics - immunocompromised states, diabetes - sexual activity - STDs - contraceptives - feminine hygiene products - vaginal medications - stress - pregnancy - foreign body |
|
|
Antibiotic use is most likely to cause which type of vaginitis among the following:
i. candidiasis ii. bacterial vaginosis iii. trichomoniasis |
candidiasis
|
|
|
note:
|
In a child with a vaginal d/c, r/o STI, foreign bodies, and trauma. Do not assume that the child has a yeast infection; although, if you think that the child does have a yeast infection, then one should look for underlying illness (e.g. immunocompromise, diabetes)
|
|
|
Which anti-hypertensives are recommended in patients with:
a) DM with nephropathy b) DM without nephropathy c) ichemic heart disease d) isolated diastolic HTN e) isolated systolic HTN f) Asthma g) Elderly (>60) |
a) DM with nephropathy: AceI or ARB
b) DM w/o nephropathy: AceI, or ARB, or CCB, or thiazide c) IHD: AceI d) isolated diastolic HTN: thiazide diuretic e) isolated systolic HTN: monotherapy with low dose diuretics f) Asthma: K-sparing + thiazide diuretics for patients on salbutamol (B blockers to be avoided unless specific indications like angina or post-MI g) Elderly (>60yrs) - Ace-I (B blockers not recommended as first line) |
|
|
Explain the classification of the different forms of hypertension (HTN)?
|

|
|
|
What are the causes of secondary HTN?
|

|
|
|
What are the investigations to do in a patient with HTN?
|
For all pts w/ htn:
- cbc, lytes, Cr - fasting glucose, fasting lipids - urinalysis, ekg For specific pt subgroups: i. dm or renal disease: urinary excretion (albumin) ii. increasing Cr/hx of renal disease/proteinuria/htn resistant to 3 meds/presence of abdo bruit: renal u/s, captopril renal scan, mra/cta iii. if suspected endocrine cause: plasma aldosterone, plasma renin iv. if suspected pheochromocytoma: 24h urine for metanephrines and catecholamines v. echocardiogram for left ventricular dysfunction if indicated |
|
|
What is the management approach to HTN?
|

|
|
|
note
|
In appropriate pts w/ htn (e.g. young pts requiring multiple meds, patients w/ an abdominal bruit, pts w/ hypokalemia in the absence of diuretics, one should suspect secondary htn and investigate appropriately.
|
|
|
What are some lifestyle modifications one should recommend for a pt that presents w/ htn?
|
- exercise (moderate intensity)
- diet (dash, low salt, low cholesterol) - wt loss - alcohol in moderation - smoking cessation - stress management |
|
|
What is the classic triad of Sx in pheochromocytoma?
|
PHE
palpitations h/a (pounding) episodic sweating (diaphoresis) |
|
|
Distinguish hypertensive urgency from hypertensive emergency?
|
hypertensive urgency:
- sBP >210 or dBP >120 w/ minimal or no target organ damage hypertensive emergency - high BP + acute target organ damage |
|
|
Patient is requesting Depo-provera injection as a form of contraception. Write a prescription.
|
Depo-provera 150mg/mL vial. For office use. M: 1
|
|
|
Most OCPs are made up of estrogen (ethinyl estradiol) and progestin (different types). Which of these varies?
[contraception] |
All OCPs have ethinyl estradiol; however, OCPs vary in the type of progestin they contain.
|
|
|
What are the 2 main disadvantages of using Depo-Provera?
[contraception] |
1. S/E of decreasing bone mineral density (BMD, which may be reversible in some cases)
2. restoration of fertility may take 1-2 years |
|
|
Patient comes in for repeat OCP refill. What are the main things you want to check?
|
1. bp
2. ? migraines w/ aura (note: migraine itself is not a contraindication) 3. smoking status 4. Pap (up to date) 5. Briefly sexual hx - same partner - prev STIs - dysparunia - other contraception |
|
|
Compare Mirena IUD vs Copper IUDs
[contraception] |

|
|
|
What are some emergency postcoital contraception (EPC) methods?
|
HORMONAL
- Yuzpe method - Plan B NON-HORMONAL - Postcoital IUD (copper) - upto 7 days post-coitally NOTE: emergency postcoital contraception does not include mirena |
|
|
What is the most common s/e of the oral post-coital contraception?
|
nausea
|
|
|
T/F. Mirena IUD cannot be used as an emergency postcoital contraception.
|
True
|
|
|
Compare the following hormonal methods of birth control: OCPs, Ortho Evra, Nuva Ring
[contraception] |
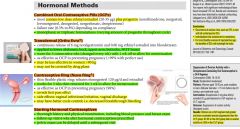
|
|
|
What are the various contraceptive options?
[contraception] |

|
|
|
For combined OCPs, what is the mechanism of action, advantages, S/Es, and contraindications?
[contraception] |
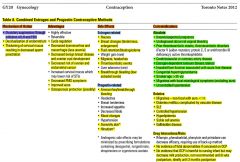
|
|
|
Compare the following OCPs?
[contraception] |
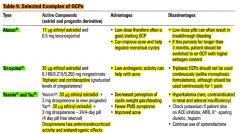
|
|
|
What should a patient do if she misses taking her
i. combined OCPs ii. progestin-only pills iii. depo-provera? |

|
|
|
note
|
Irregular breakthrough bleeding often occurs in the first few months after starting an ocp. Usually resolves after 3 cycles.
|
|
|
For progestin only contraceptive methods, what is the mechanism of action, advantages, S/Es, and contraindications?
|
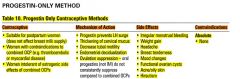
|
|
|
List and describe two examples of progestin-only methods?
[contraception] |

|
|
|
T/F. Cervical swabs for gonorrhea and chlamydia should be done prior to iud insertion.
|
True
|
|
|
Explain the different options of emergency postcoital contraception (EPC)?
[contraception] |
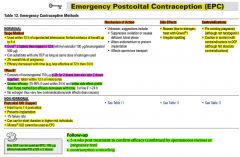
|
|
|
Discuss specific factors that may make the use of the following contraceptives less effective:
i. condoms ii. spermicide iii. ocps iv. transdermal patch |
- condoms may be less effective if there's a tear or delay in putting on
- spermicide may be less effective if lubricants are used - ocps may be less effective compliance poor (forgetting to take) - ocps may be less effective if pt os on certain meds: carbamazapine, phenytoin, St. John's Wart - transdermal patch (ortho evra) may be less effective in women > 90kg |
|
|
note
|
When parents are concerned about vaccination:
- take their concerns about vaccination seriously - discuss pt's sources of information - outline actual risks/benefits of being vaccinated - allow pt to make informed decision - religious/consciencious objections can be difficult |
|
|
What are the indications of the 23-valent pneumococcal vaccine (PPSV23) for adults?
|
Immunocompetent:
- age ≥65 - chronic heart disease (excl. htn) - chronic lung disease (eg. copd) - dm - cerebrospinal fluid leak - cochlear implant - alcoholism - chronic liver disease, cirrhosis - cigarette smoking Functional or anatomic asplenia Immunocompromised pts: - hiv - chr. renal failure - cancer - iatrogenic immunosuppression - solid organ transplant note: All adults aged ≥65 years should receive a dose of PPSV23 even if they were vaccinated when they were less than 65 years of age; however, a minimum interval of 5 years between PPSV23 doses should be maintained. Those who are receiving PPSV23 for the first time at or after age 65 should receive only a single dose (and do not require revaccination). |
|
|
note
|
The annual flu shot is not indicated for children <6 months; however, after 6 months they can get it. Children <8yrs getting the flu shot for the first time need to get 2 shots at least 28 days apart
It is indicated for any pt >6months The flu shot is encouraged in vulnerable pts including: i. children <5yrs ii. adults >65yrs iii. residents of ltc/nursing homes iv. pts w/ chronic illness (dm, Ca, lung/heart/kidney disease) v. pregnant pts vi. aboriginal people vii. obese viii. those at high risk of spreading virus to vulnerable patients (health care workers etc) |
|
|
Which population groups is the hep A vaccine indicated for?
|
Indicated for:
- travel to endemic countries - residents of communities w/ high endemic rates - iv drug use note: hep A is often given with hep B in the form of twinrix |
|
|
Differentiate between the causes of acute vs. chronic cough?
|
ACUTE COUGH
- infective (viral, pneumonia, tb) - irritant (GERD, environmental) - CHF CHRONIC - GERD - Asthma - postnasal drip - post viral - Ace-I |
|
|
Would you ever do spirometry in someone who comes in with a cough?
|
Yes. After appropriate imaging (Xrays) and given the history of asthma, or COPD (smoking), spirometry would be highly recommended
This tends to be the case for chronic cough |
|
|
Discuss the hx, physical exam, and relevant investigations for a pt with cough?
|
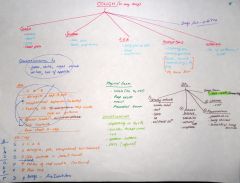
|
|
|
List and describe the common asthma/COPD meds
|
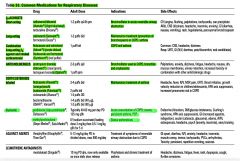
|
|
|
What are the pulmonary function criteria for diagnosis of asthma?
|
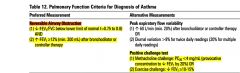
|
|
|
What is the ddx for airway obstruction (dec FEV1)?
|
- asthma
- COPD (chronic bronchitis, emphysema) - bronchiectasis - cystic fibrosis |
|
|
What is the DDx for acute bronchitis ?
|
URTI
Asthma Acute exacerbation of chronic bronchitis Sinusitis Pneumonia Pertusis Environmental/occupational exposures Post nasal drip |
|
|
What are some RFs for developing asthma?
|
- prenatal exposure to tobacco smoke
- low birth weight - hx of atopy (eczema, asthma, allergic rhinitis) - family hx of atopy, asthma - viral respiratory infections |
|
|
note
|
Asthma is typically diagnosed reliably by spirometry in individuals ≥6 yrs.
|
|
|
A pt comes in to the ER with an asthma exacerbation. Discuss criteria for home vs admission.
|
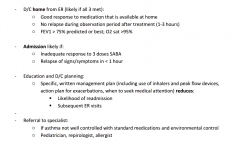
|
|
|
What is the management of acute copd exacerbation?
|

|
|
|
What are some long term complications of COPD?
|
- pulmonary HTN
- cor pulmonale from chronic pulmonary HTN - secondary polycythemia due to hypoxemia |
|
|
If someone comes in to your office with a ++ smoking hx and you suspect they have copd based on their symptoms and hx. How would you confirm this diagnosis?
|
spirometry
note: this is important b/c management of copd is different from management of asthma. Additionally, you should confirm if they have copd. note: spirometry can also be done periodically to document disease progression |
|
|
Which 2 vaccines would you recommend to a pt who has copd?
|
- annual influenza
- pneumococcal 23-valent |
|
|
Explain the clinical presentation and investigations for chronic bronchitis and emphysema
|
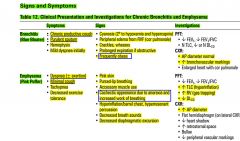
|
|
|
Discuss non-pharmacological management in copd.
|
- education of disease course
- smoking cessation - pulmonary rehabilitation - oxygen - vaccination: influenza annually and pneumococcal vaccine |
|
|
When should one consider referring a copd patient to a specialist?
|
- diagnostic uncertainty
- severe or recurrent copd exacerations - failure to respond to therapy - accelerated decline - symptoms disproportionate to level of airflow obstruction |
|
|
Distinguish between insomnias vs parasomnias vs excessive daytime sleepiness?
|

|
|
|
What is the difference between the etiologies of primary vs secondary sleep disorders?
|
PRIMARY SLEEP DISORDER:
- primary insomnia - OSA - narcolepsy - restless leg syndrome - periodic limb movements of sleep SECONDARY CAUSES: - Medical: COPD, asthma, CHF, hyperthyroidism, chronic pain, BPH - drugs: alcohol, caffeine, nicotine, B-agonist, antidepressants, steroids - psychiatric: mood and anxiety disorders - lifestyle factors: shift work |
|
|
What are some investigations one would consider in someone who presents with insomnia?
|
i. complete sleep diary (qam x 2wks: bedtime, sleep latency, total sleep time, # awakening, quality)
ii. rule out specific medical problems (cbc+diff, tsh) iii. sleep study referral - polysomnograph (if suspect sleep apnea or periodic leg movements) |
|
|
What are the 2 types of sleep apnea?
[insomnia] |
i. obstructive sleep apnea
ii. central sleep apnea |
|
|
note
[insomnia] |
When assessing pts w/ sleep complaints, obtain a collateral history from the bed partner, if possible
|
|
|
note
|
In appropriate patients with insomnia, use hypnotic medication judiciously (eg. prescribe it when there is a severe impact on function, but do not prescribe it without a clear indication).
|
|
|
What might you check on physical exam for a pt with insomnia?
|
- vitals
- h+n, cn exam, thryoid - cvs - chest - neuro |
|
|
What are some of the main side effects of benzodiazepines?
|
- drowsiness
- dizziness - memory impairment - tolerance/dependance - rebound insomnia |
|
|
What is obstructive sleep apnea?
[insomnia] |

|
|
|
What is the management of obstructive sleep apnea?
[insomnia] |

|
|
|
What is central sleep apnea?
What investigations would you do? What is the treatment for this condition? |

|
|
|
What are the RED FLAGs for back pain? What are the 3 categories of red flags?
|
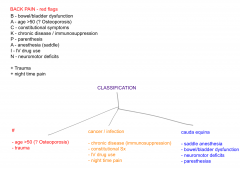
|
|
|
What are the most serious causes of lower back pain?
|
- cancer
- fracture (+/- compression) - pyelonephritis - ruptured abdominal aneurysm - cauda equina syndrome note: cauda equina and ruptured aaa are surgical emergencies |
|
|
Define the following terms with regards to back pain:
- spondylosis - spondylolisthesis - spondylolysis - ankylosing spondylitis - spinal stenosis - radiculopathy - sciatica - cauda equina syndrome |
spondylosis:
arthritis of the spine (imaging shows disc space narrowing and arthritic changes of facet joint) spondylolisthesis: anterior displacement of vertebrae on the one beneath it (imaging will show degree of slippage from gr I-IV) spondylolysis: # in the pars interarticularis where vertebral body and posterior elements, protecting the nerves are joined ankylosing spondylitis: - involve sacroiliac jts, lumbar spine - morning stiffness - decreased back motion, tenderness over sacroiliac jts spinal stenosis: local, segmental, or generalized narrowing of central spinal canal by bone or soft tissue (usually bony hypertrophic changes in facet joints and thickening of ligamentum flavum) radiculopathy: impairment of nerve root (pain, tingling, muscle weakness) sciatica: pain, numbness, tingling in distribution of sciatic nerve - down posterior or lateral aspect of leg to foot or ankle cauda equina syndrome: - bladder retention - bowel incontinence - saddle anesthesia - paresthesias/weakness in lower extremities - abnormal pressure on spinal canal - bony stenosis or herniated disc |
|
|
note:
|
90% of lower back pain resolved in 6wks, <5% become chronic
|
|
|
Discuss the different classifications of lower back pain.
|
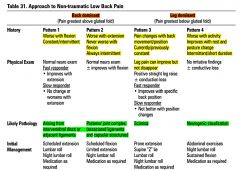
|
|
|
Discuss followup monitoring time intervals for pts who are started on statins.
|
After starting patient on statins monitor:
- ALT, AST, CK at baseline - Then 6 wks later - Then at 3 months check lipids and ALT, AST, and CK - If adequate response achieved, then check fasting lipids and LFTs q6-12 months |
|
|
Discuss the target lipid levels for primary prevention of cad.
note: risk of cad is classified as low (<10%), moderate (10-20%), and high (>20%) based on the framingham risk calculator. |
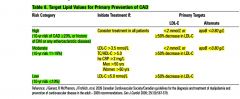
note: atherosclerotic disease includes
- previous mi, cabg, or pci - tia/cva - peripheral vascular disease - dm - eGFR <45ml/min - alb/Cr >30mg/mmol |
|
|
For pts w/ dyslipidemia, what are some modifiable RFs ?
|
- htn (optimize)
- dm (optimize) - hypothyroidism (optimize) - excessive alcohol - smoking |
|
|
What are some relevant investigations for hyperlipidemia prior to starting medication?
|
- fasting lipids
- fasting sugars - tsh - alt, ck - Cr |
|
|
note
|
In pts who are on statins for hyperlipidemia, it is important to check compliance b/c often pts will stop taking them due to myalgias (common s/e)
Other thing to watch out for with statins is liver dysfunction as these drugs can be hard on the alts are checked on bw |
|
|
T/F. hep d is only infectious in the presence of hbv (hBsAg is required for replication)
|
True
|
|
|
Which lfts are raised in hepatocellular causes of hepatitis? Which lfts are raised in obstructive causes of hepatitis?
|
hepatocellular (hepatitis)
- ast - alt obstructive (cholestasis) - alp - ggt note: - often ast/alt and alp/ggt are elevated. If both are elevated similarly --> suggests obstructive picture. If ast/alt elevations are twice that of alp elevation --> suggests hepatitis note: - in hepatitis, membranes of liver cells become permeable when damaged, allowing intracellular enzymes (ast and alt) into the bloodstream - obstructed or damaged intra or extrahepatic bile ducts lead to synthesis of alp and ggt - ggt is also raised in chronic alcoholism note: for cases of obstructive jaundice, liver/hepatobiliary u/s is important |
|
|
What are some RFs for liver disease in general? What are RFs for hepatitis b and hepatitis c?
|
General RFs for liver disease:
- alcohol (excessive) - dm, hyperlipidemia, obesity (non-alcoholic fatty liver disease) - FMHx (Wilson's, hemachromatosis, autoimmune) - medications (eg. acetaminophen, statins, isoniazid) RFs for hepatitis b and c: - injection drugs - blood transfusion prior to 1992 - tattooing, body piercing w/ shared materials - occupational exposure (needle stick injury) - infant born to mother with hbv and hcv infection - high risk sexual behaviour - born, traveled, or resided in region where hbv and hcv are common - incarceration |
|
|
Discuss the characteristics of the various viral hepatitides.
|
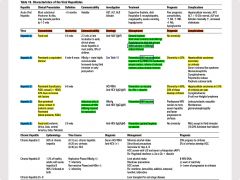
|
|
|
List some stigmata of liver disease.
|
- jaundice
- palmar erythema - spider nevi - asterixis - ascities - peripheral edema |
|
|
Patients who are chronically infected with hepatitis c are at greater risk of cirrhosis and hepatocellular cancer. What percentage of pts who are hepatitis c antibody positive are chronically infected with hepatitis c?
|
Chronicity is 80%; out of these 20% will develop cirrhosis
|
|
|
What is the most common route of transmission of hepatitis c?
|
injection drug use
|
|
|
A pt w/ hepatitis c is positive for anti-hcv antibodies (can be detected 8 wks after exposure). What test would you order to determine if this is an acute infection?
|
hcv rna; if this is negative, it should be tested again in 6 months. If the 2nd hcv rna test is also negative, this indicates the pt is immune to the virus (past hcv infection which has cleared; occurs in 20% of cases spontaneously) and does not require further management
|
|
|
What would be the management of a pt who presents with hepatitis c?
|
pegylated interferon (PEG-IFN) and ribavirin
|
|
|
A pt tests positive for hepatitis c. What bw would you make sure is recent before you sent the pt to see a specialist?
|
- lfts, albumin, inr
- Cr, lytes - liver u/s |
|
|
note
|
All pts w/ hepatitis c should be referred to a specialist to be assessed for antiviral therapy.
|
|
|
What investigations specifically would you order in someone with a hx of hepatitis b infection?
|
bw
- HBsAg - HBsAb - HCcAb - HBeAg - HBeAb - HBV dna - ast, alt, ggt, alp, albumin, inr - Cr, lytes ultrasound - liver u/s note: Cr checked due to hepato-renal syndrome |
|
|
Discuss the interpretation of the hepatitis b serology panel.
|
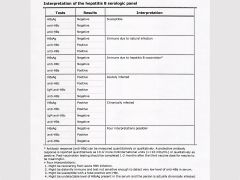
|
|
|
Diagrammatically show how the hepatitis b antigens and antibodies change over time.
|
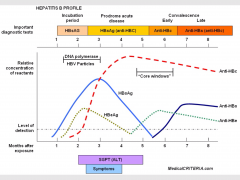
|
|
|
Discuss taking a hepatitis hx.
|

|
|
|
T/F. Post-exposure prophylaxis should be offered to pts who are exposed or possibly exposed to hepatitis a or b
|
True
For hep a, offer post-exposure prophylaxis to household/close contacts of proven or suspected cases of hep A; - give hep a vaccine preferably within 14 days - immunocompromised individuals: hep a vaccine and Ig For hep b, offer post-exposure prophylaxis to those exposed to infected blood or bodily fluids within 7-14d - HBIg |
|
|
note
|
For someone who has chronic viral hepatitis (especially hepatitis c), one should periodically look for serious complications such as cirrhosis and hepatocellular cancer.
|
|
|
note
|
For pts positive for hepatitis b/c, one should test them for hiv as well b/c they're more likely to get hiv as they have higher RFs (injection drug use, tattoos and piercings w/ shared needles, and high risk sexual activity)
|
|
|
A pt comes in with fatigue and you've done the appropriate fatigue hx and investigations (cbc, ferritin, b12, tsh, glucose). All tests come back normal and there is nothing significant on hx. What further investigations would you consider doing at this point?
|
bw
- lytes plus extended lytes (Ca, Mg, PO4) - Cr, lfts - esr, crp ekg |
|
|
What is the management of fatigue?
|

|
|
|
What is chronic fatigue syndrome?
|

|
|
|
What is the management of chronic fatigue syndrome?
|
- support and reassurance
- optimize diet, exercise - psychotherapy (cbt), family therapy, support groups - meds (to relieve Sx): antidepressants, anxiolytics, nsaids |
|
|
note
|
Patients with chronic fatigue syndrome may benefit from specialist referral.
|
|
|
Discuss the different types of altered level of consciousness (loc).
What are the causes of coma (gcs ≤8) |
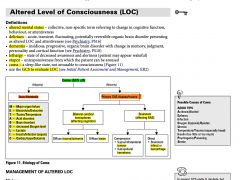
|
|
|
What is the difference between an essential tremor and a resting tremor?
|
Essential tremor (ET, also referred to as benign tremor or familiar tremor) is the most common movement disorder; its cause is unknown. It typically involves a tremor of the arms, hands or fingers but sometimes involving the head or other body parts during voluntary movements such as eating and writing. It should be distinguished from Parkinson's disease, although some individuals have both conditions. Essential tremor is commonly described as an action tremor (it intensifies when one tries to use the affected muscles) rather than a resting tremor; rigidity, such as is seen in Parkinson’s, is usually not included among its symptoms.
|
|
|
What are the causes of syncope?
|
cardiogenic
- arrhythmia - outflow obstruction (pe, tamponade, tension pneumothorax, pulmonary htn) - mi - valvular disease non-cardiogenic - peripheral vascular (hypovolemia) - vasovagal - cerebrovascular disorders - cns - metabolic disturbances (eg. etoh intoxication) |
|
|
What is syncope?
What are the causes? What would you assess in physical exam? |
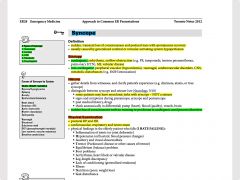
|
|
|
What investigations would you do in someone who comes in with a syncopal episode?
What would be your management? |

|
|
|
What is the ddx for loss of consciousness?
|
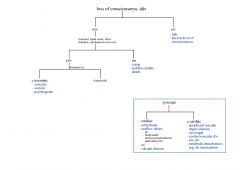
|
|
|
What is the management of a pt w/ loc or altered level of consciousness?
[loss of consciousness] |

|
|
|
note
|
In pts w/ loss of consciousness and a hx of head trauma, one must r/o intracranial bleeding according to the ct head rules
In pts w/ loss of consciousness who are anticoagulated, one must r/o intracranial bleeding |
|
|
Discuss the canadian CT head rules (CT for minor head injuries in pts >16).
|
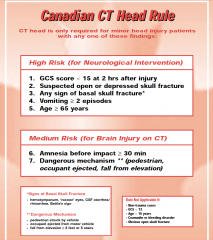
|
|
|
Discuss the CATCH rules (CT head for children with minor head injury).
[canadian] |
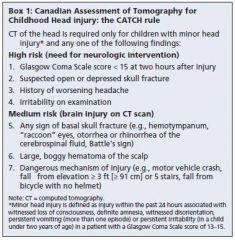
|
|
|
When someone has a concussion, what is a resource you can use to monitor their neurological/mental status?
|
SCAT2 (sports concussion assessment tool) and you can then do a f/u SCAT2 a week later to see if they've improved.
|
|
|
What would the f/u instructions be for a pt who has been assessed for a syncopal episode in the ER? Would their be any concerns re: driving?
|
followup instructions
- pts should f/u w/ a GP or cardiologist for reevaluation within 1 wk - f/u w/ specialist as appropriate - ekg if not already done driving: they should not drive when the have: - seizures - tia - presyncope or syncope - poorly controlled angina - hypoglycemic attacks - sleep attacks |
|
|
What are the driving rules for a pt who has a seizure?
|

|
|
|
What are some of the causes of weight loss?
|
Causes:
- endocrinopathies (incl. hyperthyroidism, dm type I, chr. primary adrenal insufficiency) - GI: ibd, gastric resections and bipass surgeries - malignancy (any) - hiv - advanced cardiac, pulmonary, and renal disease - neurological disease: stroke, dementia, parkinson's disease - psychaitric disorders - medications, drugs Investigations - cbc, lytes - glucose - tsh - fobt, urinalysis |
|
|
Define the following terms:
- seizure - epilepsy - ictal - post-ictal - inter-ictal - status epilepticus |

|
|
|
What is status epilepticus?
|
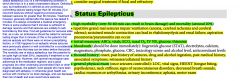
A seizure lasting >5min w/o spontaneous cessation, or recurrent seizures w/o full return to consciousness inter-ictally.
note: status epilepticus can cause irreversible brain damage without treatment |
|
|
note
|
Stroke is the most common cause of late-onset (>50 yrs of age) seizures, accounting for 50-80% of cases
|
|
|
Discuss the classification of seizures.
|

|
|
|
What are the signs and symptoms of the different types of seizures?
|

|
|
|
What is the ddx of convulsions?
|
- syncope
- pseudoseizure - hyperventilation - tia/stroke - panic disorder - hypoglycemia - movement d/o - alcoholic backouts - migraines - narcolepsy |
|
|
note
|
teratogenicity of anticonvulsants is due to increased risk of open neural tube defects. It is best to advise patient planning pregnancy to take 5mg/d of folic acid. Also, one should consider switching medications
|
|
|
Discuss the differences between seizure and syncope.
|
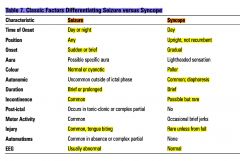
|
|
|
Discuss the differences between seizure and pseudoseizure (conversion disorder).
|

|
|
|
A pt has a seizure. List relevant investigations.
|
bloodwork
- cbc, lytes, Cr, bun - lfts - fasting blood glucose - Ca, Mg, PO4 - tsh - ck, prl, esr - eeg for unprovoked or recurrent seizures - ct/mri head +/- LP (if suspecting encephalitis/meningitis) |
|
|
When should seizures be treated?
|
seizures should be treated w/ anticonvulsants if:
- ≥2 unprovoked seizures in 6 months - known organic brain disease - eeg w/ epileptiform activity - 1st episode of status epilepticus |
|
|
List a few anticonvulsant medications.
|
broad spectrum (generalized-onset and partial-onset seizures)
- lamotrigine - epival (valproate) narrow spectrum (simple partial, complex partial and secondarily generalized seizures): - carbamazepine - gabapentin - phenytoin absence seizures: - ethosuximide |
|
|
Discuss the management of status epilepticus.
[seizures] |
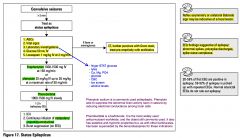
|
|
|
What is the etiology behind seizures?
|
Seizures are caused by several conditions.
Unprovoked seizures are typically idiopathic (called epileptic seizures) Provoked seizure have their own causes: STRUCTURAL - trauma/scar - congenital - neoplasm - vascular - infection (encephalitis) METABOLIC - hypoglycemia** - electrolyte abnormalitities - renal / liver failure OTHERS - toxicity - febrile seizures - withdrawal (eg. alcohol withdrawal) ------------------- note: metabolic abnormalities include: - hypoglycemia - hyponatremia - hypocalcemia - non-ketotic hyperglycemia - uremia - hyperthyroidism - hypoxia |
|
|
In general, list a few symptoms of seizures.
|
- tongue biting
- h/a - frothing - cyanosis - urinary incontinence - post-ictal confusion, somnolence - focal neurological signs |
|
|
A pt has a seizure. What are some things to look for on physical exam?
|
- assess loc
- vitals - heent - papilledema, tongue biting, neck stiffness - cn exam + neuro exam - cardiac murmurs - resp |
|
|
What is the most common s/e of most antiepilectic drugs?
|
fatigue
|
|
|
What is the definition of epilepsy?
|
Chronic condition characterized by ≥2 unprovoked seizures.
note: In a pt presenting with a seizure, one should take an appropriate hx to direct the investigation (e.g. do not overinvestigate; a stable known disorder may require only a drug-level measurement, while new or changing seizures may require an extensive work-up). |
|
|
Take a seizure hx.
|

|
|
|
What is Stevens-Johnson syndrome (sjs)?
|
Stevens–Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) are two forms of a life-threatening skin condition, in which cell death causes the epidermis to separate from the dermis. The syndrome is thought to be a hypersensitivity complex that affects the skin and the mucous membranes.
|
|
|
Discuss the use of anticonvulsants in pregnancy.
|
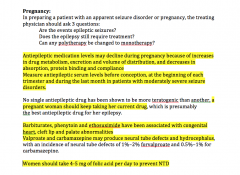
|
|
|
note
|
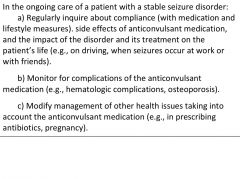
|
|
|
What is lyme disease?
What are the clinical features? What is the management? |
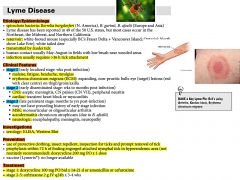
|
|
|
Compare the signs and symptoms of allergic vs. viral vs. bacterial conjunctivities?
|

|
|
|
What is the management of viral conjunctivitis?
|
- self limiting condition
- warm compresses - maintain good hygiene - avoid close contact (as highly contagious) |
|
|
T/F. Allergic conjunctivitis will almost always present bilaterally, whereas, bacterial and viral conjunctivitis will typically start in one eye and then move to the other eye.
|
True
|
|
|
What are the signs/symptoms of anterior blepharitis?
What is the management? |

|
|
|
What are the signs/symptoms of posterior blepharitis?
What is the management? |

|
|
|
What is the ddx for red eye?
|
lids/orbit/lacrimal system:
- hordeolum/chalazion - blepharitis - dacryocystitis - fb/laceration conjunctiva / sclera: - subconjunctival hemorrhage - conjunctivitis - dry eyes - episcleritis/scleritis - preseptal/orbital cellulitis cornea: - fb - keratitis (inflammation of the cornea) - abrasion/laceration - ulcer anterior chamber - iritis (anterior uveitis) - acute angle closure glaucoma - hyphema - hypopyon endophthalmitis (inflammation of the internal coats of the eye) |
|
|
What is the difference between a hordeolum (stye) and chalazion?
|

|
|
|
What is anterior uveitis (iritis)?
What are the causes What and the signs/symptoms? What is the management? |
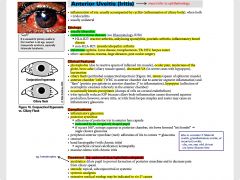
|
|
|
note
|
Acute angle closure glaucoma is an EMERGENCY and must be seen by an ophthalmologist asap
|
|
|
note
|
When addressing eye complains, it is important to assess visual acuity using hx, physical exam, and or the Snellen chart as appropriate.
One must also r/o the other red flags - ocular pain - photophobia - trauma - contact lens |
|
|
Distinguish between these causes of red eye?
- conjunctivitis - acute iritis - acute angle closure glaucoma - keratitis |

|
|
|
note
|
In pts presenting w/ a fb sensation in the eye, it is essential to clarify the mechanism of injury (high speed, metal on metal, not wearing eyewear)
Appropriate investigations to find an intraocular fb would include: - xray - ct Apart from the slit lamp examincation w/ fluorescene dye, it is important to flip the eye lids to check for any fb under the lid or on the conjunctiva |
|
|
You diagnose a pt to have highly purulent bacterial conjunctivitis suspicious of pseudomonas. The pt is also a contact lens wearer. What would you prescribe?
|
moxifloxacin 0.5% drops
1 drop in affected eye tid M: 7d note: moxifloxacin drops can be used for bacterial conjunctivitis in more severe cases, eg: - contact lenses - pseudomonas infection - corneal involvement - treatment failure |
|
|
What is bacterial keratitis?
|
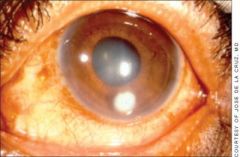
Bacterial keratitis — Bacterial infectious keratitis warrants evaluation by an ophthalmologist on the same day. The patient will complain of foreign body sensation and have trouble keeping the involved eye open, a sign of an active corneal process. Bacterial pathogens include Staphylococcus aureus, Pseudomonas aeruginosa, coagulase-negative Staphylococcus, diphtheroids, Streptococcus pneumoniae, and polymicrobial isolates [6].
Overnight wear of contact lenses is associated with a higher incidence of bacterial keratitis, but the entity can occur in patients who do not wear contact lenses or who wear them on a daytime only basis. Breakdown in local or systemic host defense mechanisms, including dry ocular surfaces, topical corticosteroid use, and immunosuppression, can predispose to bacterial keratitis. The diagnostic finding in bacterial keratitis is a corneal opacity or infiltrate (typically a round white spot) in association with red eye, photophobia, and foreign body sensation. This infiltrate or ulcer (>0.5 mm in size) can be seen with a penlight, and does not require a slit lamp for identification. It will stain with fluorescein. Mucopurulent discharge is typically present. Fulminant cases may present with an associated hypopyon (layer of white cells in the anterior chamber) Treatment requires urgent ophthalmological referral and prompt initiation of topical bactericidal antibiotics (ideally after obtaining cultures). These antibiotics are sometimes compounded in fortified concentrations, not commercially available. Topical glucocorticoids and topical drug combinations containing topical steroids should not be used in the initial treatment of suspected bacterial keratitis; their role is controversial and best left to the discretion of the consulting ophthalmologist. |
|
|
T/F. Steroid treatment should be avoided for keratitis and conjunctivitis.
|
True
Although steroid treatment is indicated for iritis |
|
|
List some conditions that may be associated w/ iritis (anterior uveitis).
|
- reactive arthritis
- ankylosing spondylitis - psoriatic arthritis - ibd - crohn's disease note: In pts with iritis, one should look at possible underlying systemic causes such as the ones listed above |
|
|
What is episcleritis?
What are the clinical features? What is the treatment? |

|
|
|
What is scleritis? What are the causes?
|

|
|
|
What are the clinical features of scleritis?
What is the treatment of scleritis? |

|
|
|
What is ophthalmia neonatorum?
What are the symptoms? What is the management? |
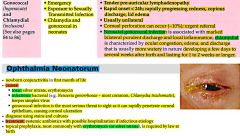
|
|
|
Discuss the different signs/symptoms of dehydration?
|

|
|
|
What are the 3 components of fluid resuscitation?
|
- maintenance (4:2:1)
- deficits - ongoing losses |
|
|
What is meant by 'maintenance' with respect to fluid resuscitation?
|

|
|
|
What is meant by 'deficits' with respect to fluid resuscitation?
|

|
|
|
What is meant by 'ongoing losses' with respect to fluid resuscitation?
|

|
|
|
When treating severe dehydration, one should use objective measures (eg. lab values) to direct ongoing management). What might these lab values be?
|
i. cbc (for hemoconcentration, infection, source of dehydration)
ii. lytes iii. bun, Cr (inc. in severe dehydration) iv. blood gas and HCO3 for metabolic acidosis |
|
|
Dehydration if often caused by GI losses; i.e. vomiting and diarrhea. What are some non-GI causes of dehydration?
|
- vascular: hemorrhage
- skin/resp: fever, sweating, burns - cardiac: chf - kidneys: diuretics, hypoaldosteronism, diabetes insipidus (central/nephrogenic) - 3rd spacing: hypoalbuminemia, pancreatitis, peritonitis, sepsis) |
|
|
note
|
1st line Rx for mild to moderate dehydration is with ORT.
|
|
|
note
|

It is important to treat the dehydrated pregnant patient aggressively with fluids, as there are additonal risk of dehydration in pregnancy.
|
|
|
Discuss your approach to H/As when dealing w/ a pt?
[headache] |

|
|
|
What is Medication Overuse H/A (MOA)?
What is the management for MOA? |
Definition:
Medication overuse headaches (MOH), also known as rebound headaches usually occur when analgesics are taken frequently to relieve headaches. Rebound headaches frequently occur daily and can be very painful and are a common cause of chronic daily headache. They typically occur in patients with an underlying headache disorder such as migraines or tension headaches that "transforms" over time from an episodic condition to chronic daily headache due to excessive intake of acute headache relief medications. MOH is a serious, disabling and well-characterized disorder, which represents a worldwide problem and is now considered the third-most prevalent type of headache. In the case of ergotamine, triptans, opioids and combination medications in particular, intake on > 10 days/month for > 3 months is required, whereas simple analgesics are considered overused when they are taken on > 15 days/month for >3 months. Management: i. patient education ii. withdrawal of overused medications iii. bridge therapy with Naproxen iv. f/u and relapse prevention (to prevent redevelopment of MOH, the freq of acute symptomatic medication usage should be limited, and the rational for restriction should be explained to the patient |
|
|
Classify and describe the primary H/As?
|
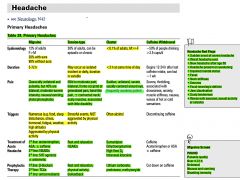
|
|
|
Likelihood of having a migraine can be diagnosed by the POUND pneumonic. What is this pneumonic?
|

|
|
|
T/F. Tension H/As are triggered by stressful events and NOT aggravated by physical activity.
|
True
|
|
|
A pt presents with a headache. What are some things to check for on:
- physical exam? - investigations? |
physical exam:
- vitals: esp. bp - head: scalp, jaw (temporal arteritis, tmj) - fundoscopy (papilledema, retinal hemorrhages) - neck stiffness, bruits - kernig's, brudzinski - cn exam - neuro exam - generalized (motor, sensation, reflexes) investigations (only in presence of red flags) - bw: cbc (infections), esr (temporal arteritis) - ct/mri: to r/o space occuplying lesion, aneurysm, sah, stroke - lp: clinical suspicion of infection, inflammatory etiology of h/a; or sah in the setting of normal/negative head ct |
|
|
What does cerebrovascular disease comprise of ?
|
- stroke (ischemic, hemorrhagic)
- sah - ich (intracerebral hemorrhage) - aneurysms (intracranial) - carotid stenosis |
|
|
Is a lumbar puncture ever done if you're suspecting subarachnoid hemorrhage?
|
A non-contrast ct is done first; if this is negative but there's a high suspicion of sah, then a lumbar puncture is indicated.
|
|
|
Discuss the approach to subarachnoid hemorrhages (sah).
|

|
|
|
What is a subarachnoid hemorrhage (sah)?
What are the causes? What are the RFs? What are the clinical features? |
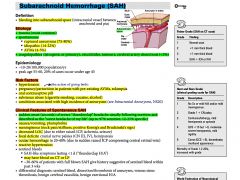
|
|
|
What are relevant investigations for a suspected subarachnoid hemorrhage?
|

|
|
|
T/F. If a diagnosis of giant cell arteritis/temporal arteritis is made clinically, one should start high dose corticosteroids (prednisone) immediately and perform a temporal artery biopsy to confirm diagnosis within 2 wks of initial presentation.
|
True
One should not wait to TREAT if diagnosis is suspecteded on clinical findings. |
|
|
What is a cardiac complications of giant cell arteritis/temporal arteritis?
|
i. thoracic aortic aneurysm (11%)
ii. aortic dissection (40%) |
|
|
note
|
If a diagnosis of meningitis is suspected clinically, one should start empiric IV antibiotic treatment before waiting for investigation results (eg. lp)
|
|
|
Explain the McIsaac Criteria for pharyngitis and how it applies to the diagnosis and management of GABHS?
[GAS score] |

|
|
|
Which SSRI has been most extensively been studied and which one would be the first one you would try?
|
Cipralex (do not give past 20 mg/day)
- may start with 5mg/d or 10mg/d Clinical trial data has shown that Cipralex can cause electrical changes in the heart known as QT interval prolongation. These electrical changes can lead to abnormal heart rhythms, which can be life threatening. The risk is dose-related, meaning that the risk increases as dosage increases. A warning on the dose-related risk of QT interval prolongation has been added to the drug label for Cipralex, as well as revised prescribing and dosing recommendations: Cipralex should not be used in patients with a heart condition known as congenital long QT syndrome, or in patients with QT interval prolongation. Use of Cipralex is discouraged in patients who are also taking drugs that prolong QT interval or that decrease electrolyte levels in the body. Examples of drugs that affect QT interval include: drugs used to treat heart rhythm problems, certain antipsychotics, certain antidepressants, opioid painkillers and certain drugs used to treat infections. Examples of drugs that may affect electrolyte levels include: diuretics (water pills) and laxatives (including enemas). 10 mg per day is the maximum recommended dose for patients who: - are 65 years of age or older, or - have liver problems, or - are taking the heartburn drugs omeprazole or cimetidine which can increase the blood level of Cipralex. 20 mg per day is still the maximum recommended dose for most other patients. |
|
|
What causes plantar warts?
What are the treatment options? |
human papilloma virus (hpv) is the cause of all warts
hpv 1 (most common for plantar warts) Most warts often regress on their own (2/3 of patients within 2 years) TREATMENT OPTIONS i. salicylic acid ii. liquid nitrogen - apply every 2 weeks (5-6 times) (often avoided in young children b/c it can cause pain) iii. cantharidin (canthacur) - multiple treatments iv. shave excision Flat warts are treated with liquid nitrogen or topical applications such as imiquimod |
|
|
note
|
In a male pt who is:
- unable to void - blood at the urethral meatus - scrotal hematoma there is urethral injury until proven otherwise, therefore Foley catheter insertion is generally CONTRAINDICATED unless performed gently by urology staff/resident |
|
|
note
|
A hordelum may progress to a chalazion, which is a chronic inflammatory lesion that develops with a meibomian tear gland of the eyelid becomes obstructed.
note: Antibiotics are NOT indicated as chalazion is a granulomatous condition. note: a hordeolum is acute; a chalazion is chronic |
|
|
What does a stye look like?
|

|
|
|
What does a chalazion look like?
|

|
|
|
For a patient who requires orthotics what do you type in after pressing ctrl B in PSS?
|
Custom bilateral orthotics
|
|
|
List two OTC treatments for tinea capitis (fungal infection on the head)
|
Apply these shampoos q weekly:
- Nizoral - Selsun gold |
|
|
note
|
Average age of onset of adhd is 3 yrs
Children w/ adhd are at risk of: - substance abuse - depression - anxiety - academic failure - poor social skills - cd/odd/aspd - adult adhd |
|
|
Discuss treatment strategies for refractory depression with respect to: optimization, augmentation, combination, and substitution?
|
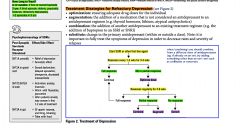
|
|
|
List some commonly used antidepressants?
|
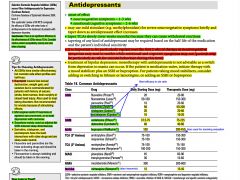
|
|
|
What is the onset of effect for antidepressants?
|
Well it depends
- For neurovegetative Sx (SIGECAPS, not mood): 1-3 wks - For emotional/cognitive Sx: 2-6 wks NOTE: for severe neurovegetative symptoms, may use a mild stimulant (eg. methylphenidate) briefly and taper down as antidepressant effect increases NOTE: when prescribing antidepressants, it is important to be particularly vigilant over the first 2 wks of therapy as neurovegetative Sx may start to resolve while emotional and cognitive Sx may not and patients are at higher risk of suicidal behaviour during this time |
|
|
How long should someone with depression be treated for?
|
6-12 months: if first or second episode
2 yrs: if third episode, elderly, psychotic features, refractory depression, >2 episodes in 5 yrs |
|
|
T/F. There is no significant difference in the effectiveness of SSRIs versus TCAs for depression
|
True
One should consider relative pt acceptibility, toxicity, and cost when choosing between SSRIs and TCAs. |
|
|
List one NDRI (norepinephrine and dopamine reuptake inhibitors) and 2 TCAs?
|
NDRI:
- Bupropion (wellbutrin) TCAs: - amitriptyline (Elavil) - nortriptyline (Aventyl) MAOI: - phenelzine (Nardil) |
|
|
What are the indications for SSRIs?
|
- depression
- Anxiety - OCD - eating disorders |
|
|
What are the side effects (s/e) of SNRIs?
|
S/E:
- Lower dose: insomnia - Higher dose S/E include: tremor, tachcardia, sweating, insomnia, dose dependent increase in BP |
|
|
What are some RFs for depression?
|
- sex: female > male
- age: onset 25--50 - family hx: depression, alcohol abuse - childhood experiences: abuse, loss of family member - personality: insecure, dependent, obsessional - recent stressors: illness, financial, legal - postpartum >6mo - lack of intimate, confiding relationships or social isolation - chronic pain - low ses - co-morbid psychiatric illnesses |
|
|
note
|
When assessing a pt w/ depression, one should also look for and diagnose other co-morbid psychiatric conditions such as: anxiety, bipolar disorder, psychosis, substance abuse, and personality disorder
|
|
|
note
|
In a pt that presents with depression, it is important to inquire about social hx:
- recent stressors - relationships - abuse: physical, mental, sexual - finances - substance abuse |
|
|
If a pt is treated with several different antidepressants for depression and there is no improvement, what are some other possible diagnoses?
|
- refractory depression
- bipolar disorder - schizoaffective disorder - organic disease (cardiac, endocrine, infectious, neoplastic) |
|
|
Discuss some of the organic causes of mood disorders.
|
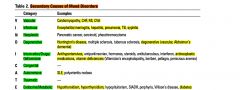
|
|
|
What are some investigations one may consider in someone who has depression?
|
bw
- cbc, lytes, Cr, bun - fasting glucose - tsh, b12, calcium mri brain |
|
|
What is an adjustment disorder?
What is the management? |
Adjustment disorder (AD) is a psychological response to an identifiable stressor or group of stressors that cause(s) significant emotional or behavioral symptoms that do not meet criteria for anxiety disorder, PTSD, or acute stress disorder. The condition is different from anxiety disorder, which lacks the presence of a stressor, or post-traumatic stress disorder and acute stress disorder, which usually are associated with a more intense stressor.
Management: * brief psychotherapy (individual, group), crisis intervention * biological - benzos may be used for anxiety Sx (short-term, low dose, regular schedule, long half-life, no prns) - SSRIs for both depressed and anxiety Sx |
|
|
What is dysthymic disorder?
|
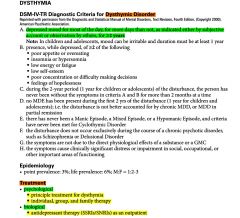
|
|
|
Distinguish between postpartum blues, postpartum depression, and postpartum psychosis.
|

|
|
|
note
|
In a pt presenting w/ multiple somatic complains for which no organic cause is found after appropriate investigations, one should consider the diagnosis of depression and explore this possibility with the pt.
|
|
|
What is grief?
|
Grief is a natural response to loss.
- The emotional suffering you feel when something or someone you love is taken away. - The more significant the loss, the more intense the grief will be. Though grief is most often associated with the death of a loved one—any loss can cause grief, including: - Divorce or relationship breakup - Loss of health - Losing a job - Loss of financial stability - A miscarriage - Retirement - Death of a pet - Loss of a cherished dream 1969 Psychiatrist Elisabeth Kübler-Ross’ five stages of grief: • Denial: “This can’t be happening to me.” • Anger: “Why is this happening? Who is to blame?” • Bargaining: “Make this not happen, and in return I will ____.” • Depression: “I’m too sad to do anything.” • Acceptance: “I’m at peace with what happened.” Common symptoms of Grief • Shock and disbelief • Sadness • Guilt • Anger • Fear • Physical symptoms fatigue, nausea, lowered immunity, weight loss or weight gain, aches and pains, and insomnia. |
|
|
What is complicated grief?
|
10-20% of bereaving (grieving) people develop complicated grief: an abnormal form of grief that continues for at least six months following the loss and involves a distinct cluster of symptoms including persistent yearning, disbelief the deceased is really gone and guilt about moving on with one’s life
The repercussions from the enduring distress and dysfunction of CG could include • increased risk of cancer, hypertension, cardiac events and suicidal ideation • social, occupational and family dysfunction • increased consumption of alcohol and cigarettes • increased rates of hospitalization • reduced quality of life. |
|
|
What are some RFs for complicated grief?
|
• A relationship with the deceased that was close, confiding and/or dependent
• Childhood abuse or serious neglect • Separation anxiety in childhood • Past history of psychiatric problems, particularly depression • Lifestyle rigidity (being averse to change) • Poor social support • Loss of a child or fetus • Death that is unexpected and/or traumatic (e.g., suicide, homicide, accident) • Deaths where the body could not be viewed, if this were important to the survivor |
|
|
What is the management of complicated grief?
|
post loss 6-18 months:
psychotherpay - cbt - group therpay - traumatic grief therpay (imaginal re-living of the death) Antidepressants |
|
|
note
|
In all pts who are grieving for example from the loss of a loved one, it is important to ask about depressive Sx and suicidal ideation.
|
|
|
note
|
In suicidal pts presenting at the ER w/ a suspected drug overdose, always screen for acetylsalicylic acid and acetaminophen overdoses, as these are common, dangerous, and frequently overlooked.
|
|
|
What are the RFs for atherosclerotic heart disease?
[acute coronary syndrome/ACS/ischemic heart disease] |
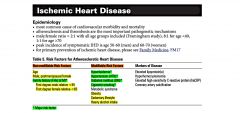
|
|
|
note
[acute coronary syndrome/ACS/ischemic heart disease] |
Chronic stable angina is most often due to a fixed stenosis caused by an atheroma; whereas acute coronary syndromes are the result of plaque rupture.
|
|
|
note
[acute coronary syndrome/ACS/ischemic heart disease] |
thrombolysis is NOT administered for unstable angina/NSTEMI; but it can be used for STEMI
|
|
|
List 2 cardiac serum biomarkers in a presentation of acute coronary syndrome (acs)?
[acute coronary syndrome/ACS/ischemic heart disease] |
i. cardiac troponins
ii. creatinine kinase - mb |
|
|
What is the definition of unstable angina?
[acute coronary syndrome/ACS/ischemic heart disease] |
UA is defined as any 1 of the following:
i. angina at rest ii. new onset angina (<2 months) iii. increasing angina (inc. in intensity, duration, and/or freq, occurs w/ dec. exertion, dec. response to Rx) |
|
|
How do unstable angina and nstemi differ?
[acute coronary syndrome/ACS/ischemic heart disease] |
UA and NSTEMI differ primarily in whether ischemia is severe enough to cause enough myocardial damage to release detectable amounts of marker (i.e. troponin).
Unstable Angina/NSTEMI involve acute plaque rupture and thrombosis with incomplete transient vessel occlusion. STEMI involves acute plaque rupture and thrombosis with total coronary artery occlusion resulting in necrosis. UA and NSTEMI are often grouped together as they present the same before we get cardiac markers back. |
|
|
What is a STEMI?
[acute coronary syndrome/ACS/ischemic heart disease] |
1. New ischemic changes on ECG: ST elevation in 2 contiguous leads (>1mm in limb leads or >2mm in precordial leads or new left or right BBB) AND 1 or more of:
2. Ischemic symptoms 3. Cardiac enzyme elevations |
|
|
What is the classification of acute coronary syndrome?
[acute coronary syndrome/ACS/ischemic heart disease] |
unstable angina --> nstemi --> stemi
|
|
|
Diagrammatically discuss the reperfusion management of a stemi.
What are the contraindications for thrombolysis in stemi? [acute coronary syndrome/ACS/ischemic heart disease/chest pain] |
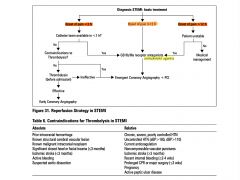
|
|
|
Discuss the treatment algorithm for chest pain (cardiac).
[acute coronary syndrome/ACS/ischemic heart disease] |
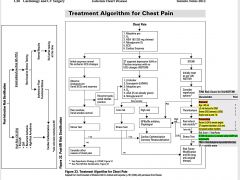
|
|
|
note
[acute coronary syndrome/ACS/ischemic heart disease] |
It is recommended that an ekg be obtained within 10 minutes of presentation for pts with ongoing chest discomfort (or anginal equivalent) or other Sx of acs.
|
|
|
Distinguish between the classic vs. atypical presentation of ischemic heart disease.
[acute coronary syndrome/ACS/ischemic heart disease] |
Classic Presentation
- substernal pressure/pain that increases with exertion, decreases with rest (unless unstable angina or MI) - +/- radiation to back, neck, jaw, arm or shoulder - unaffected by inspiration, not reproducible with palpation - diaphoresis, nausea, vomiting - Levine’s sign: patient describes pain by clenching fist over sternum ----------------------------------------- Atypical presentation - atypical presentations more common in women, elderly and those with DM, the young, and those w/ no risk factors - jaw and neck pain, dyspnea, fatigue, palpitations, indigestion, cough, nausea, emesis - dyspnea could be only sign in the elderly - epigastric pain/indigestion - anginal equivalents: dyspnea, acute left ventricular failure with flash pulmonary edema - (pts may have no pain at all!) |
|
|
note: atypical presentations of ischemic heart disease (ihd) are more common in women, elderly, pts w/ dm, the young, and those at no risk. What symptoms would be atypical for ishcemic heart disease?
[acute coronary syndrome/ACS/ischemic heart disease] |
- jaw and neck pain, dyspnea, fatigue, palpitations, indigestion, cough, nausea, emesis - dyspnea could be only sign in the elderly
- epigastric pain/indigestion - anginal equivalents: dyspnea, acute left ventricular failure with flash pulmonary edema - (pts may have no pain at all!) |
|
|
note
[acute coronary syndrome/ACS/ischemic heart disease] |

|
|
|
What are the indications for fibrinolysis in the acute management of STEMI?
[acute coronary syndrome/ACS/ischemic heart disease] |
- no contraindications
- pci unavailable in 90 minutes - contraindications to pci - symptoms <12 hours |
|
|
T/F. A normal ekg does not rule out ischemic heart disease.
[acute coronary syndrome/ACS/ischemic heart disease] |
True
|
|
|
What are some complications of an MI?
[acute coronary syndrome/ACS/ischemic heart disease] |
CRASHPAD
Cardiac Rupture Arrhythmia Shock Htn/heart failure Pericarditis/PE Aneurysm Dvt |
|
|
Should pts who have a stemi be given β-blockers?
[acute coronary syndrome/ACS/ischemic heart disease] |
IV β-blockers: promptly particularly if tachyarrhythmia or htn present as long as they do not have any contraindications
oral β-blockers: initiate within first 24 hrs to pts without contraindications contraindications: - severe heart failure - inc. risk of cardiogenic shock |
|
|
What is the role of antiplatelets and antithrombotics in the acute management of pts with stemi?
[acute coronary syndrome/ACS/ischemic heart disease] |
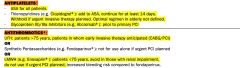
|
|
|
A pt presents with symptoms suggestive of ischemic heart disease but the diagnosis is not obvious. EKG, cardiac enzymes, and exercise testing comes back normal. What would you do in this situation.
[acute coronary syndrome/ACS/ischemic heart disease] |
Do further investigations:
- cxr (if not already done) - echo - angiography |
|
|
What is the TIMI score?
[acute coronary syndrome/ACS/ischemic heart disease] |

|
|
|
What is the classic quartet of cardiac tamponade?
What is Beck's traid? |
classic quartet of tamponade:
i. hypotension ii. jvp elevated iii. tachycardia iv. pulsus paradoxus (inspiratory fall in sBP>10mmHg) beck's triad i. hypotension ii. elevated jvp iii. muffled heart sounds |
|
|
What is the ddx for pulsus paradoxus (inspiratory fall in sBP>10mmHg)?
|
- constrictive pericarditis (rarely)
- cardiogenic shock - cardiac tamponade - severe obstructive pulmonary disease (eg. asthma) - tension pneumothorax - pe |
|
|
What is the etiology of cardiac tamponade?
|
Any cause of pericarditis but especially:
- trauma - malignancy - uremia - proximal aortic dissection w/ rupture |
|
|
For cardiac tamponade, what are
- relevant investigations? - management? |
investigations:
- ekg - echo - cardiac catheterization management: - pericardiocentesis (echo guided) - pericardiotomy - avoid diuretics and vasodilators (these decrease venous return to already under filled rv --> dec lv preload --> dec. CO) - fluids (may temporarily inc. CO) - treat underlying cause |
|
|
How might a dvt present?
How might a pe present? What are some relevant investigations for: - dvt - pe [dvt/pulmonary embolism] |

|
|
|
T/F. When investigating for dvt/pe, d-dimers are only useful if they are negative and the likelihood of dvt/pe is low.
[dvt/pulmonary embolism] |
True
If there is a moderate to high probability of having a pe, go straight to spiral ct |
|
|
Discuss the diagnostic approach to suspected pe?
[dvt/pulmonary embolism] |

|
|
|
D-dimer can be elevated in pts w/ a dvt/pe. What are some other causes of elevated d-dimers?
[dvt/pulmonary embolism] |
- recent surgery
- cancer - infection, inflammation - severe renal dysfunction |
|
|
What is the management of pulmonary embolism?
[dvt/pulmonary embolism] |

|
|
|
What are the clinical features of an aortic dissection?
What are some relevant investigations? |

|
|
|
What is the management of a pt who has an aortic dissection?
|
pharmacological (lower bp and dec. cardiac contractility)
- sodium nitroprusside - β-blocker surgical - resection of segment - replacement of affected aorta w/ prosthetic graft |
|
|
note
|
If a pt presents w/ a pneumothorax with:
- severe respiratory distress - tracheal deviation to contralateral side - distended neck veins (inc. jvp) - hypotension One DOES NOT need to perform a cxr. The pt needs treatment right away. |
|
|
What are the causes of pneumothorax?
What are the signs and Sx? |

|
|
|
For a pneumothorax, what investigation(s) would you do?
What would be the management? |

|
|
|
What is the ddx for chest pain?
|
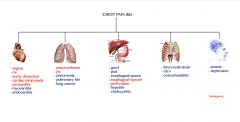
|
|
|
Discuss the approach to dysphagia?
|

|
|
|
List 3 investigations that may be useful in someone who has dysphagia?
|
1. Barium swallow
2. Endoscopy (refer to gastroenterologist) 3. esophageal manometry (esophageal motility study) NOTE: esophageal manometry would be useful in someone with esophageal motor disorders such as achalasia and scleroderma (dysphagia with solids + liquids) |
|
|
Discuss the differences between the following 3 esophageal motor disorders.
|
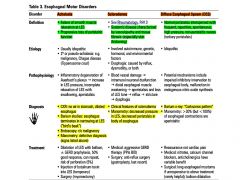
|
|
|
What is a hiatus hernia?
What are the RFs? What are the symptoms and complications? |

|
|
|
For a pt w/ suspected hiatus hernia discuss:
- investigations - management |
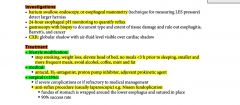
|
|
|
What is the ddx for cough ?
|
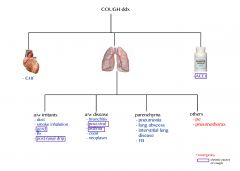
|
|
|
note
|
One should not ascribe a persistent cough to an adverse drug effect (eg. from ACEi) without first considering other cause.
|
|
|
A pt has been complaining of a persistent cough. You find from the hx that he is a chronic smoker for many years. Is it reasonable to do spirometry on this pt?
|
Yes, at some point preferably earlier, one should do spirometry to confirm copd and treat accordingly
|
|
|
A pt presents with ongoing hemoptysis for 3 months. Bw comes back normal; cxr and ct are suspicious of a mass. He was treated for a pneumonia, but the hemoptysis persists. What other investigations would you consider doing now?
|
- sputum c+s, cytology (tell pt to keep sample in fridge)
- bronchoscopy +/- biopsy (respirologist) |
|
|
Which are the most common sites affected in osteoarthritis?
|

|
|
|
What are the signs and symptoms of osteoarthritis?
|

|
|
|
What investigations would you consider doing in a pt that presents w/ symptoms suggestive of osteoarthritis?
What is the management of osteoarthritis? |

|
|
|
T/F. One of the symptoms of osteoarthritis is morning stiffness of <30 minutes.
|
True
|
|
|
What is the diagnostic criteria for diabetes mellitus?
|

|
|
|
What are some diabetes mellitus (dm) related Sx? What are some dm related long term complications?
|
dm related Sx:
i. hyperglycemia: polyuria, polydipsia, polyphagia, fatigue, weight change, blurry vision, yeast infections ii. hypoglycemia: chills, tremors, anxiety, palpitations, sweating, headaches, seizures, worst care scenario - coma iii. diabetic ketoacidosis (dka) - fruity breath - kussmaul breathing (deep, laboured breathing) - abdo pain, N/V, dehydration, anorexia - fatigue long term complications of dm: i. microvascular: nephropathy, neuropathy, retinopathy ii. macrovascular: cad, cvd, pvd |
|
|
note
|
Topical analgesics (eyes) should only be used to facilitate examination. They should NEVER be used as treatment for any ocular problem.
|
|
|
What are the causes of corneal abrasions?
What are the clinical features? complications? What is the management? |

|
|
|
T/F. One should NEVER patch a corneal abrasion if pt wears contact lenses as contact lens wearers are prone to pseudomonas infection.
|
True
|
|
|
What is congestive heart failure (CHF)?
What are the signs and symptoms of CHF? |
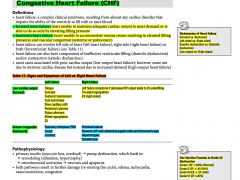
|
|
|
What are the most common precipitants of heart failure?
[chf] |
- htn
- arrhythmia - infection/ichemia/infarction - failure to take meds - dietary indiscretions |
|
|
List some of the precipitants of heart failure?
[chf] |
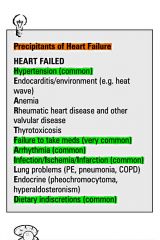
|
|
|
Discuss the NYHA functional classification of heart failure?
[chf] |
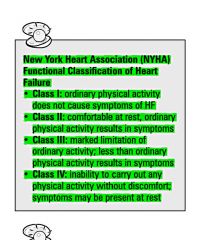
|
|
|
What investigations would you do for a patient with suspicious CHF?
|

|
|
|
What is the management for an acute case of pulmonary edema (CHF)?
|

|
|
|
A patient comes in with erectile dysfunction. What investigations would you do?
What is the management of ED |

|
|
|
What is the definition of acute pain?
What is organization of the WHO analgesia ladder? |

|
|
|
What are the common s/e of opioids?
|
i. sedation
ii. n/v, constipation, abdo pain, urinary retention iii. respiratory depression iv. pruritis |
|
|
Compare:
- tylenol - nsaids - opioids |
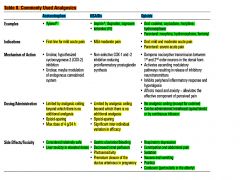
|
|
|
What are the signs and symptoms of neuropathic pain?
|

|
|
|
Define the following terminology involving 'pain':
- nociceptive pain and neuropathic pain - spontaneous pain - paresthesia - dysesthesia - allodynia - hyperalgesia |
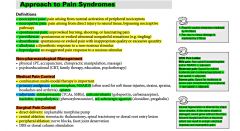
|
|
|
For 2,4,6 month olds, what do you check on physical exam?
|
- fontanelle, eyes, hearing
- cvs, chest, abdo - gu, hips, msk |
|
|
What is the management approach to neuropathic pain?
|
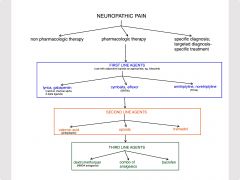
|
|
|
What physical exam maneuvers would be applicable for a patient who comes in with osteoporosis?
|
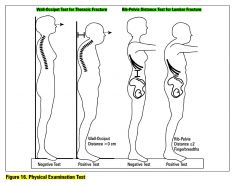
|
|
|
What is the treatment of pyelonephritis in a pregnant woman?
|
ceftriaxone 1-2g q24h
|
|
|
What is the management approach to nociceptive pain?
|

|
|
|
What are hemorrhoids?
- RFs? - clinical features? - management? |

|
|
|
What is patellofemoral syndrome?
What are the clinical features? What are relevant investigations? What are the treatment options? |
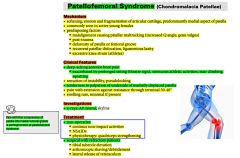
|
|
|
What are anal fissures? What is the cause? What are the treatment options?
|

|
|
|
What are 2 examples of intra-nasal corticosteroids (sometimes used in sinusitis)?
|
- nasonex
- rhinocort |
|
|
A patient comes in with a bee sting on her hand. Her hand has been swollen, red, warm. Its been 24 hrs and its getting worse. How do you distinguish between and inflammatory reaction vs. cellulitis?
|
Both present very similarly. One big difference, however, is that with cellulitis you get increased pain on palpation.
Inflammatory rxns secondary to bee stings present with symptoms (redness, swelling, warmth) relatively quickly (within 1 hour); cellulitis can take upto 24h. If symptoms are getting more progressive past 24 hrs, better to lean towards cellulitis. Treat this patient as a cellulitis + inflammatory rxn secondary to bee sting: - keflex 500mg po qid x 7d - advil - icing - elevate hand - rtc if develops fever or swelling, redness worsens |
|
|
What is the management for fibromyalgia?
|
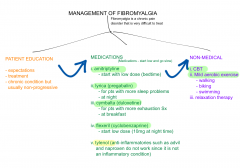
|
|
|
What are the manifestations of fibromyalgia?
|
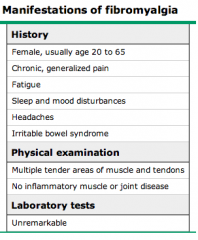
|
|
|
What is the clinical presentation of meningitis?
What are relevant investigations? |
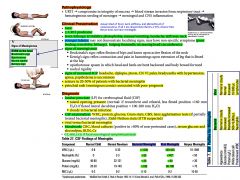
|
|
|
What are the 3 main symptoms of meningitis?
What are the main signs of meningitis? |
Symptoms:
i. fever ii. neck stiffness iii. altered LOC ~95% of the patients w/ meningitis have 2 of the 3 Sx ------------------------------------------------------------ Signs: BONK on the head Brudzinski's sign Opisthotonos Nuchal rigidity Kernig's sign |
|
|
Which tetanus shots are given after a pt gets a wound?
|
tetanus toxoid IM +/- tetanus Ig
|
|
|
note
|
For suspected bacterial meningitis it is essential to start empiric IV abx even before investigations are complete.
|
|
|
If someone is diagnosed w/ meningitis, is it important to contact public health?
|
Yes. Family and friends and other contacts of the patient should receive appropriate prophylaxis.
|
|
|
For meningitis, what is the management?
|

|
|
|
What are some complications of meningitis?
|
- h/a
- seizures - cerebral edema - hydrocephalus - SIADH - deafness - neurological deficits - death |
|
|
What are the most common organisms in meningitis?
What are the RFs of meningitis? |
|
|
|
Illustrate the kernig's sign and brudzinski tests.
|

|
|
|
note
|
Approximately 50-90% of pts w/ bacterial meningitis have positive blood cultures, therefore it is always important to order blood cultures for suspected bacterial meningitis.
|
|
|
What is carpal tunnel syndrome and how is it caused?
- What are the clinical features? - What tests / investigations would you do? - What would be your management? |
|
|
|
T/F. Degenerative joint disease and arterial insufficiency frequently co-exist
|
True
|
|
|
What is narcolepsy?
|
Symptoms of narcolepsy include: CHAP
- Cataplexy (Cataplexy is a sudden and transient episode of loss of muscle tone, often triggered by emotions) - Hallucinations - Attacks of sleep - Paralysis on waking - irresistible sleep attacks (up to 30 minutes) and persistent daytime drowsiness occurring daily for ≥ 3 months - cataplexy (sudden temporary episodes of paralysis with loss of muscle tone) - sleep paralysis TREATMENT: i. stimulants (methylphenidate, D-amphetamine) ii. TCAs iii. SSRIs |
|
|
What are some key HRT treatment regimens?
|
|
|
|
What are some investigations you would do for a woman in menopause?
|
- Inc. levels of fsh (>35iu/l) on day 3 of cycle (if still cycling) and lh (fsh>lh). But csh level not always predictive dur to monthly variation. Use absence of menses for 1 yr to diagnose.
- Dec. levels of estradiol (later) |
|
|
What do you want to ask the patient on subsequent antenatal visits?
What do you want to check for on physical exam? What investigations would you do ? |
HISTORY
- bleeding - vaginal d/c - abdominal cramping PHYSICAL EXAM - bp - symphysis fundal height (at 20wks fundus should be at umbilicus; at 12 - the symphysis pubis - fhr - fetal position INVESTIGATIONS - urinalysis |
|
|
note
|
When prescribing Gabapentin for pain (neuropathic) it is important to start at lower doses and then gradually increase
PRESCRIPTION (may look like) Gabapentin 100mg Take 1 capsule po bid x 1 week; then take 1 tablet po tid thereafter |
|
|
What is the difference between secretory and osmotic diarrhea?
|
SECRETORY DIARRHEA:
- diarrhea persists with fasting OSMOTIC DIARRHEA: - diarrhea stops with fasting |
|
|
note
|
In any woman with vaginal bleeding, it is important to rule out pregnancy.
|
|
|
T/F. AUB in women > 40 requires an endometrial biopsy to rule out cancer even if known to have fibroids.
|
True
|
|
|
What is 'abnormal uterine bleeding' and what is the classification (not causes)?
[aub] |
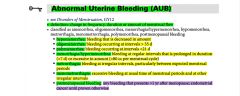
|
|
|
What are the causes of aub?
|
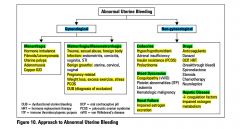
|
|
|
What is the management of abnormal uterine bleeding (aub)?
|

|
|
|
What are the 2 most common forms of diaper rash?
What is the management? |
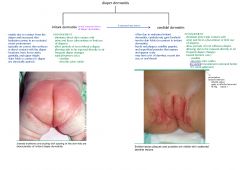
|
|
|
A patient comes in with aub. What are relevant investigations to consider in this patient?
|

|
|
|
Compare anovulatory vs. ovulatory AUB?
|
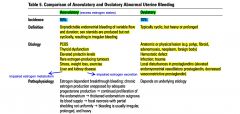
|
|
|
What is dysfunctional uterine bleeding (dub)?
|
- DUB is a form of AUB. It is a term used synonymously with AUB. In this case, estrogen is produced unopposed by inadequate progesterone production --> continuous proliferation of the endometrium --> thickened endometrium outgrows its blood supply --> focal necrosis with partial shredding --> bleeding is irregular, prolonged, and heavy.
NOTE: DUB is a diagnosis of exclusion. |
|
|
T/F. In pregnancy, expectant management of fibroids is normally optimal.
|
True
|
|
|
T/F. Even with known fibroids, abnormal uterine bleeding + age >40 always to endometrial biopsy to r/o cancer.
|
True
|
|
|
What is a leiomyomata (fibroids)?
|
Benign smooth muscle tumour of the uterus (most common gyne benign tumour)
NOTE: - diagnosed in 40-50% of pre-menopausal women >35yrs - more common, larger and occur at earlier age in black women - typically regress after menopause; enlarging fibroids in a postmenopausal woman should prompt consideration of malignancy (even though low malignancy potential) |
|
|
What are the different types of fibroids (based on anatomical location)?
|
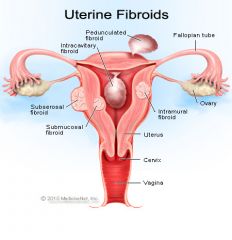
|
|
|
Which type of fibroids are most symptomatic?
|
submucosal fibroids
These are associated with increased bleeding and infertility. |
|
|
What are the clinical features of fibroids?
|

|
|
|
A woman comes to your office and based on the symptoms, you suspect fibroids.
What are some investigations to consider for fibroids? |

|
|
|
What are the treatment options for fibroids?
|

|
|
|
What is adenomyosis?
- clinical features? - investigations? - treatment options? |

|
|
|
Clinical features of adenomyosis?
|
- secondary dysmenorrhea
- dyspareunia - dyschezia (difficulty defecating) - pelvic discomfort/bloating - menorrhagia Halban sign: tender, softened uterus on premenstrual bimanual exam |
|
|
What is the treatment for adenomyosis?
|
- nsaids, analgesia
- ocp - depo-provera (medroxyprogesterone) - danazol - gnrh agonist (lupron) |
|
|
What is the ddx of bleeding in pregnancy?
What investigations would you do? |
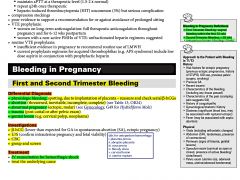
|
|
|
What is the classification of spontaneous abortions?
What is the management of the different types of spontaneous abortions? |

|
|
|
T/F. In abortions, it is important to rule out ectopic, check Rh (if neg, give Rhogam), and always ensure patient is hemodynamically stable.
|
True
|
|
|
Plasma b-hCG levels less than expected by dates suggests what?
|
- ectopic pregnancy
- abortion - inaccurate dates |
|
|
Plasma b-hCG levels more than expected by dates suggests what?
|
- multiple gestation
- molar pregnancy - trisomy 21 - inaccurate dates |
|
|
What are the clinical features of ectopic pregnancy?
|
4Ts and 1S
- Temperature > 38°C - Tenderness: abdominal (90%) +/- rebound - Tenderness on bimanual examination, CMT - Tissue: palpable adnexal mass - Signs of pregnancy: Chadwick's sign, Hegar's sign |
|
|
What are relevant investigations to do for ectopic pregnancy?
What is the management for a patient with ectopic pregnancy? |

|
|
|
What are some RFs for ectopic pregnancy?
|

|
|
|
What is the algorithm for a suspected ectopic pregnancy?
|
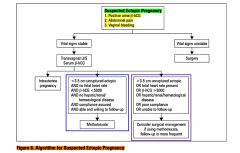
|
|
|
What is antepartum hemorrhage and what is the DDx?
|
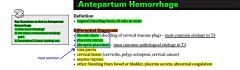
|
|
|
What is placenta previa?
What are the RFs? |
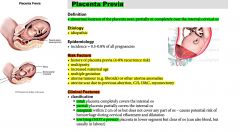
|
|
|
What is the classification of placenta previa?
|
TOTAL: placenta completely covers the internal os
PARTIAL: placenta partially covers the internal os MARGINAL: within 2 cm of os but does not cover any part of os - causes potential risk of hemorrhage during cervical effacement and dilatation LOW LYING (NOT A PREVIA): placenta in lower segment but clear of os (can also bleed, but usually in labour) |
|
|
What are the clinical features of placenta previa?
|
- PAINLESS bright red vaginal bleeding (recurrent)
(mean onset of bleeding is 30 wks GA, but onset depends on degree of previa (total previa - bleed earlier) |
|
|
What are some of the levels of placental invasion in placenta previa?
|
i. Placenta accrete - AT the myometrium (most common)
ii. Placenta increta - INTO the myometrium iii. Placenta percreta - PASSES myometrium |
|
|
T/F. One must NEVER perform a vaginal exam until placenta previa has been ruled out by U/S
|
True
If the patient is coming in with vaginal bleeding. It is important to do an U/S. And once placenta previa has been ruled out, then one can go ahead with a vaginal exam. Now information about a placenta previa would be revealed probably at the 18 wk U/S checkup....But if this has not been done, then must do one before vag exam. |
|
|
What is the most important investigation in someone with suspected placenta previa (painless bright red vaginal bleeding)?
|
ultrasound
|
|
|
What is the management of placenta previa?
|

|
|
|
What is the main clinical difference between placenta previa and abruptio placenta?
|
Placenta previa presents with PAINLESS vaginal bleeding
Abruptio placenta precents with PAINFUL vaginal bleeding (NOTE: bleeding may not occur if abruptio placenta is concealed) NOTE: Vasa previa presents as PAINLESS vaginal bleeding |
|
|
What is abruptio placenta?
What are the RFs? |
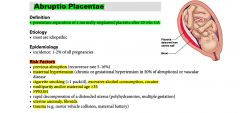
|
|
|
What are the clinical features of abruptio placenta?
|

|
|
|
What is the most common cause of DIC in pregnancy?
|
Abruptio placenta
Note in 20% of abruptio placenta, DIC occurs |
|
|
What is vasa previa?
|
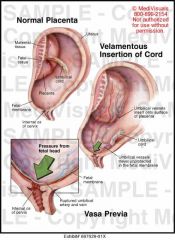
Vasa previa is present when fetal vessels traverse the fetal membranes over the internal cervical os. These vessels may be from either a velamentous insertion of the umbilical cord or may be joining an accessory (succenturiate) placental lobe to the main disk of the placenta. If these fetal vessels rupture the bleeding is from the fetoplacental circulation, and fetal exsanguination will rapidly occur, leading to fetal death.
Normally, the umbilical cord inserts into the middle of the placenta as it develops. In velamentous cord insertion, the umbilical cord inserts into the fetal membranes (choriamniotic membranes), then travels within the membranes to the placenta (between the amnion and the chorion). The exposed vessels are not protected by Wharton's jelly and hence are vulnerable to rupture. Rupture is especially likely if the vessels are near the cervix, in which case they may rupture in early labor, likely resulting in a stillbirth. |
|
|
What is the presentation in vasa previa?
- relevant investigations? - management? |

|
|
|
What is the management of abruptio placenta?
|

|
|
|
What investigations are relevant for abruptio placenta?
|
Abruptio placenta is a clinical diagnosis. u/s sensitivity is very low (15%)
|
|
|
What is the management of abruptio placenta?
|

|
|
|
T/F. OCP is safe to take during breastfeeding?
|
True
|
|
|
What medication can you give a mother who has inadequate milk production?
|
domperidone
|
|
|
What are some investigations that are useful in an Rh positive woman?
|
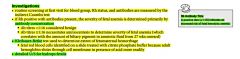
|
|
|
Explain the concept of Rh-neg women getting sensitized in pregnancy?
|
A woman is at risk when she has a neg Rh factor and her partner has a positive Rh factor. This combination can produce a child who is Rh positive. While the mother's and baby's blood systems are separate there are times when the blood from the baby can enter into the mother's system. This can cause the mother to create antibodies against the Rh factor, thus treating an Rh positive baby like an intruder in her body. If this happens the mother is said to be sensitized. A sensitized mother's body will make antibodies. These antibodies will then attack an Rh positive baby's blood, causing it to breaking down the red blood cells of the baby and anemia will develop. In severe cases this hemolytic disease can cause illness, brain damage and even death.
Sensitization can also occur during a: - blood transfusion - miscarriage - abortion - ectopic pregnancy - procedures such as amniocentesis. Since the antibodies do not disappear and rarely cause a problem in first pregnancies, it is very important to be screened thoroughly and give an accurate medical history to your doctor or midwife. Hemolytic disease can be prevented for many women, if they are not already sensitized. Rh immunoglobulin (RhIg = Rhogam) is a blood product given via injection to help the Rh negative mother by "minimizing her reaction to the Rh positive red cells. Since a small number of unsensitized women may have problems with the end of pregnancy, many practitioners recommend that she be given an injection of RhIg (also known as Rhogam) at 28 weeks gestation, to prevent the few cases of sensitization that occur at the end of pregnancy. |
|
|
List the scenarios under which Rhogam (Rh-IG) is given? (prophylaxis)
|
|
|
|
note
|
In any pregnant pt w/ vaginal bleeding, it is important to check and treat for hemodynamic instability; also important to do blood typing and screening and transfuse prn. Rhogam should be offered as well.
|
|
|
An Rh Antibody titre of ≥ 1:16 indicates what?
|
Increased risk of fetal hemolytic anemia
An antibody titre of ≥ 1:16 necessitates amniocentesis to determine the severity of fetal anemia |
|
|
What are the complications of anti-Rh antibodies on the fetus?
What are the treatment options if prevention was not done/hasn't worked? |

|
|
|
During a pregnancy, at what times is an U/S done and for what reason?
[pregnancy lmcc] |

|
|
|
In a woman with postmenopausal vaginal bleeding bleeding apart from bw, what would you do on physical exam and / or investigations?
|
physical exam:
- vitals (bp, pulse), fluid status - bimanual exam (pelvic) - pap test investigations: - u/s - endometrial biopsy - +/- ct scan note: this pt should be referred to gynecology |
|
|
What is a bone scan?
|
A bone scan is an imaging test that shows areas of increased or decreased bone turnover (metabolism).
A bone scan involves injecting a radioactive material (radiotracer) into a vein. The substance travels through your blood to the bones and organs. As it wears off, it gives off a little bit of radiation. This radiation is detected by a camera that slowly scans your body. The camera takes pictures of how much radiotracer collects in the bones. If a bone scan is done to see if you have a bone infection, images may be taken shortly after the radioactive material is injected and again 3 to 4 hours later, when it has collected in the bones. This is called a 3-phase bone scan. To evaluate metastatic bone disease, images are taken only after the 3 to 4 hour delay. The scanning part of the test will last about 1 hour. The scanner's camera may move above and around you. You may need to change positions. You will probably be asked to drink extra water after you receive the radiotracer to keep the material from collecting in your bladder. |
|
|
note
|
Postmenopausal bleeding is endometrial cancer until proven otherwise
|
|
|
Discuss an approach to vaginal bleeding.
|
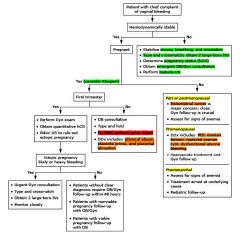
|
|
|
note
|
In a pt who is having vaginal bleeding, pelvic exam should NOT be done till placenta previa is ruled out!
|
|
|
What are some RFs for complicated urinary tract infections (UTIs)?
|
- male
- pregnancy - recent urinary tract instrumentation - indwelling catheter - functional / anatomical abnormality of urinary tract (incl. bph) - chronic renal disease - diabetes, immunosuppression |
|
|
What are some non-medical options for preventing UTIs?
|

|
|
|
What are the causes of dysuria?
What are the signs and symptoms of the different infectious causes of dysuria? |

|
|
|
What are some investigation options for dysuria?
|

|
|
|
What is the management of dysuria?
|

|
|
|
What are the most common pathogens involved in urinary tract infections?
|
KEEPS
- klebsiella sp. - e.coli (90%), other gram-negatives - enterococci - proteus, pseudomonas - s. saprophyticus |
|
|
What are more serious complications of urinary tract infections (uti)?
|
- sepsis
- pyelonephritis - infected nephrolithiasis - renal abscess |
|
|
T/F. In very young pts and elderly pts that present with abdo pain, fever, and/or delirium, one must rule out a urinary tract infection (uti) by doing appropriate workup.
|
True
|
|
|
note
|
In a pt w/ dysuria, exclude other causes (eg. STIs, vaginitis, stones, interstitial cystitis, prostatitis) through appropriate hx, physical examination, and investigation before diagnosing a urinary tract infection (uti).
note: ddx for dysuria includes: - uti - stones, stricture(s), bph - caffeine, interstitial - sti - trauma, fb, instrumentation - malignancy |
|
|
What are some RFs for urinary tract infections?
|

|
|
|
What is the ddx for dysuria?
|

|
|
|
What are some causes/RFs of recurrent uncomplicated UTIs?
|
- vaginal intercourse
- use of diaphragms or spermicides for contraception - atrophic vaginitis - onset of UTI before age 15 - urinary retention - urinary incontinence Others include: - structural abnormalities - poor hygiene |
|
|
What is the ddx for dizziness?
[vertigo] |
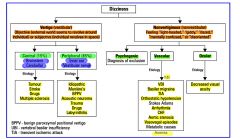
|
|
|
What are the 'vascular' causes of dizziness?
|
- arrhythmia
- vasovagal episodes - mi - aortic stenosis - chf - tia - vbi - basilar migraine - anemia |
|
|
What physical exams/investigations would you do for dizziness?
|

|
|
|
What is multiple sclerosis?
|
|
|
|
What are the clinical features of multiple sclerosis?
|
|
|
|
What investigations are relevant for multiple sclerosis?
What are some treatment options? |

|
|
|
For dizziness, discuss what questions you would ask on history?
|

|
|
|
note
|
In a pt who presents with lightheadedness or ‘dizziness’, it is always important to get postural vitals because they may have orthostatic hypotension.
|
|
|
note
|
In hypotensive dizzy patients, exclude serious conditions (eg. MI, abdominal aortic aneurysm, sepsis, GI bleeding) as the cause.
|
|
|
Dizziness is a non-specific terms that can be labeled as:
- vertigo - disequilibrium - presyncope - syncope Distinguish between these terms. |

|
|
|
What are the symptoms of acute bacterial prostatitis?
|
- lower back, rectal, perinel pain
- irritative and obstructive urinary Sx, hematuria, blood per ejaculate - fever (acute onset), chills, malaise On rectal exam: - enlarged, tender, and warm prostate Investigations: - cbc (wbc), Cr - urinalysis, urine c+s (if urinalysis pos.) |
|
|
What are some medications and substances that can cause dizziness?
|
Medications
- ototoxic drugs (asa, gentamicin) - lasix - nitrates - PDEi (eg. cialis) - antipsychotics - antihypertensives (any) Substances - caffiene - alcohol |
|
|
T/F. Status epilepticus is a medical emergency and can cause irreversible brain damage without treatment.
|
True
|
|
|
What are pseudoseizures?
|
Pseudoseizures are a physical manifestation of an emotional disturbance. They resemble epileptic seizures, but, unlike the seizures caused by epilepsy, they are not caused by electrical disruptions in the brain. People experiencing pseudoseizures often experience loss of consciousness, grand mal-like twitching or jerking, and aggravated emotional states. These episodes may last for 20 minutes or more.
Physicians believe that pseudoseizures are psychological defense mechanisms, and may be brought on by episodes of severe stress or emotional trauma. The seizures tend to occur when patients try to suppress the trauma, often taking the person suffering with them by surprise, as do epileptic seizures. The difference between epileptic seizures and pseudoseizures can be difficult to recognize, even for trained medical professionals. The physical appearances of epileptic seizures and pseudoseizures are virtually identical. Generally, a diagnosis of pseudoseizures is reached after a complete neurological work up is performed, thorough seizure history and description is obtained, and the results of an electroencephalogram (EEG) are analyzed to gauge differences in the brain's electrical activity from what would be expected of someone prone to epileptic seizures. One of the most common complications involved in the diagnosis and treatment of pseudoseizures is the misconception that people who suffer from the phenomena are hypochondriacs, hysterics, or "faking it." The name for the condition alone, "pseudoseizures," leads some people to think of the occurrences as medically suspect. Many patients who experience pseudoseizures are urged to seek counseling. This can be a good or bad therapeutic option, depending on the context. As pseudoseizures are a physical manifestation of intense emotional or psychological stress, or a physical response to a childhood trauma, counseling to work through the underlying cause of the pseudoseizures is certainly an important step toward resolving the concern. However, counseling alone will not resolve the pseudoseizures. The physical manifestation of the disorder will not resolve if the entirety of the phenomena is not considered and treated. Most importantly, it is crucial that patients and healthcare providers remember that pseudoseizures are seizures. There is a complete lack of control inherent in any seizure activity, and the potential ramifications of that loss of control can be just as devastating for people suffering from pseudoseizures as it can for those living with epileptic seizures. |
|
|
note
|
Anticonvulsants are teratogenic in a pregnant woman due to increased risk of oNTDs. It is important to advise patients planning pregnancy to take 5mg (not 0.5mg) folic acid. Also consider switching meds.
|
|
|
What is BPPV?
What is the etiology? How is Dix-Hallpike done? What is the management for this condition? |
|
|
|
What is Meniere's disease (endolymphatic hydrops)?
What are the clinical features? What is the management? |
|
|
|
What is vestibular neuronitis?
What are the clinical features What is the treatment? |
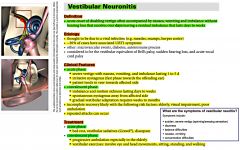
|
|
|
What is labyrinthitis?
What is the etiology? What are the clinical features? What investigations would you do? What is the treatment? |
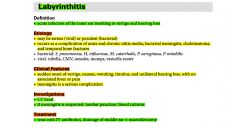
|
|
|
What is the classic triad of ruptured AAA?
|
i. pain
ii. hypotension iii. pulsative abdominal mass |
|
|
T/F. Repair of asymptomatic AAA is generally not justified for:
- Males <5.0cm - Females <4.5cm |
True
|
|
|
What is the management of ruptured AAA?
|
- ABCs
- no imaging - straight to OR (confirm diagnosis by laparotomy) - crossmatch 10 units packed RBCs |
|
|
Compare peripheral vs central vertigo.
|

|
|
|
Compare the following causes of vertigo:
bppv meniere’s disease vestibular neuronitis labyrinthitis acoustic neuroma |

|
|
|
note
|
When a parent elects to bottle feed, support their decision in a non-judgemental manner.
|
|
|
What is the most common cause of neonatal sepsis?
|
group b Streptococcus (GBS)
|
|
|
What are the causes and RFs for neonatal sepsis?
|

|
|
|
What are the signs of sepsis in the newborn?
|

|
|
|
For a newborn, discuss the discharge instructions to be given to the parents?
|
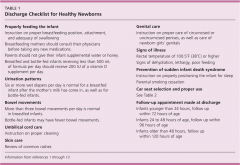
|
|
|
What is Sudden Infant Death Syndrome (SIDS)?
|
Sudden and unexpected death of infant <12 months in which the cause of death cannot be found by history, examination, or thorough postmortem and death scene investigation.
|
|
|
What can be done to prevent SIDS?
|
- place infant on back, NOT in prone position when sleeping
- allow supervised play time daily in prone position - alarms/other monitors not recommended - inc. anxiety and do not prevent life-threatening events - avoid overheating and overdressing - use appropriate infant bedding (firm mattress, avoid loose bedding and crib bumper pads) - no smoking |
|
|
What are some RFs for SIDS?
|
- prematurity
- sleeping on abdomen - smoking in household - minorities (Aboriginals and african americans) - socially disadvantaged |
|
|
Discuss the bmi classification.
|
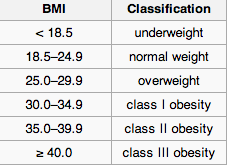
|
|
|
What are some co-morbidities associated with obesity?
|
co-morbidities:
- htn - dm - lipids elevated - cad - sleep apnea - osteoarthritis note: It is important to inquire about these conditions in obese pts as they are more likely to occur. |
|
|
note (99 objectives_obesity)
|
|
|
|
Guideline summary on prevention and management of obesity in children and adults.
|
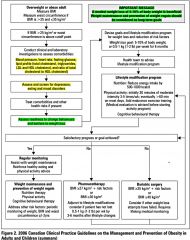
|
|
|
note (99 objectives_stress)
|
|
|
|
Illustrate the newborn resuscitation algorithm.
|
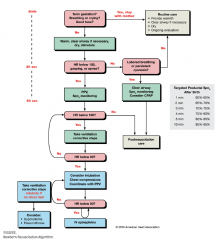
|
|
|
What does routine neonatal care involve?
|
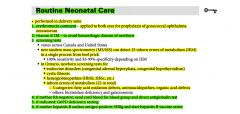
|
|
|
How would you diagnose a newborn in respiratory depression/distress? What would be the management for this newborn?
|
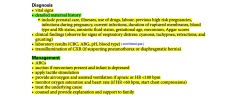
|
|
|
Explain assessment of neonate with APGARs?
|
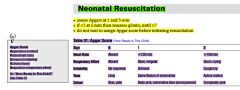
|
|
|
What are some interventions one can use in a depressed newborn?
|
EPINEPHRINE
- if HR<60 and not rising NALOXONE (NARCAN) - for newborns with respiratory depression and maternal narcotic use 4h before delivery FLUID BOLUS (NS, whole blood, ringer's lactate) - if there is evidence of hypovolemia |
|
|
What are the causes of respiratory depression in the newborn?
|
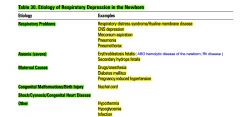
|
|
|
What characteristics would a depressed newborn have? How would you manage this patient (the newborn)?
|
One or more of the following: (just think of apgars)
- pulse < 100 - does not cry when stimulated - does not move all extremities - does not have a good strong cry - color pale, blue |
|
|
Which hemolytic causes of jaundice (inc. bilirubin production) are Coombs positive and which are negative?
|
COOMBS POSITIVE
- Isoimmune (Rh, ABO, other blood antigens)/Autoimmune (SLE) - Acquired cell defects (eg. drugs) COOMBS NEGATIVE - red cell membrane defects (elliptocytosis, spherocytosis) - RBC enzyme deficiencies (G6PD) - hemoglobinopathy (thalessemia) - microangiopathy (hemolytic-uremic syndrome) |
|
|
What is the difference between Gilbert's syndrome and Crigler-Najjar syndrome?
|
GILBERT'S SYNDROME:
- mild decrease in glucuronyltransferase activity (leading to defective conjugation of bilirubin) CRIGLER-NAJJAR SYNDROME: - complete deficiency of glucuronyltransferase enzyme |
|
|
Explain the classification of neonatal jaundice?
|
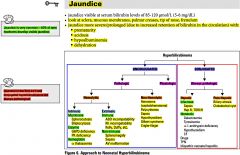
|
|
|
Explain the causes of neonatal jaundice by age?
|
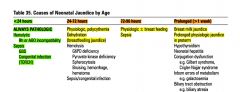
|
|
|
When must jaundice be investigated in the neonate? What investigations would you do in this patient (with jaundice that is not normal)
|

|
|
|
Children with _____________ syndrome are 15 times more likely to develop leukaemia
|
Down syndrome
|
|
|
What is cystic fibrosis?
|
Cystic fibrosis (also known as CF or mucoviscidosis) is an autosomal genetic disease affecting most critically the lungs, and also the pancreas, liver, and intestine. It is characterized by abnormal transport of chloride and sodium across epithelium, leading to thick, viscous secretions.[1]
The name cystic fibrosis refers to the characteristic scarring (fibrosis) and cyst formation within the pancreas, first recognized in the 1930s.[2] Difficulty breathing is the most serious symptom and results from frequent lung infections that are treated with, though not cured by, antibiotics and other medications. Other symptoms, including sinus infections, poor growth, diarrhea, and infertility affect other parts of the body. |
|
|
What is the management for someone with Cystic Fibrosis?
|
Nutritional counseling:
- high caloric diet - pancreatic enzyme replacement - fat soluble vitamin supplements Management of chest disease: - physiotherapy, postural drainage - exercise - bronchodilators - aerosolized DNAase - antibiotics: depends on sputum (C+S) - cephalosporin, cloxacillin, ciprofloxacin - lung transplantation Genetic counselling |
|
|
What is the presentation of someone with CF?
[cystic fibrosis] |
CF PANCRAS
- Chronic cough and wheezing - FTT - Pancreatic insufficiency (symptoms of malabsorption - steatorrhea) - Alkalosis and hypotonic dehydration - Neonatal intestinal obstruction (meconium ileus)/Nasal polyps - Clubbing of fingers/Chest radiograph with characteristic changes - Rectal prolapse - Electrolyte elevation in sweat, salty skin - Absence or congenital atresia of vas deferens - Sputum with Staph or pseudomonas ------------------------------------------------------------------------ Sx simplified: - chronic cough - absense/congenital atresia of vas deferens - salty skin - malabsorption (steatorrhea) - FTT |
|
|
What investigation would you do for suspected CF?
[cystic fibrosis] |
Sweat chloride test x 2 (>60mEq/L)
3 day fecal fat collection Genetics |
|
|
Discuss the difference between innocent and pathological murmurs in children.
|
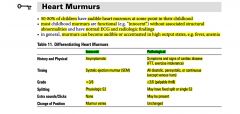
|
|
|
What is the difference between breastfeeding jaundice and breast milk jaundice?
|
breastfeeding jaundice:
common due to lack of milk production and subsequent dehydration, leading to exaggerated physiological jaundice breast milk jaundice: rare (1 in 200 breast-fed infants) inhibitor of glucuronyl transferase found in breast milk onset 7d of life, peak at 2nd and 3rd wk of life |
|
|
What is considered hypoglycemia in a newborn?
What are some of the causes? How would hypoglycemia present in the newborn? |

|
|
|
What is the management of hypoglycemia in the newborn?
|

|
|
|
What are some common medical problems to warn parents about who have just had a baby and are now discharged from the hospital?
|
- jaundice
- difficulty breastfeeding - minimal wet diapers/bm - sepsis (child toxic) - hypoglycemia - apneic spells - inconsolable crying - poor sleep |
|
|
note
|
When examining a newborn, systematically look for subtle congenital anomalies (e.g. ear abnormalities, sacral dimpling) as they may be associated with other anomalies and genetic syndromes.
|
|
|
What is Huntington's disease?
|
Huntington's disease is a disorder passed down through families in which nerve cells in certain parts of the brain waste away, or degenerate.
Huntington's disease is caused by a genetic defect on chromosome 4. The defect causes a part of DNA, called a CAG repeat, to occur many more times than it is supposed to. Normally, this section of DNA is repeated 10 to 28 times. But in persons with Huntington's disease, it is repeated 36 to 120 times. As the gene is passed down through families, the number of repeats tend to get larger. The larger the number of repeats, the greater your chance of developing symptoms at an earlier age. Therefore, as the disease is passed along in families, symptoms develop at younger and younger ages. There are two forms of Huntington's disease. The most common is adult-onset Huntington's disease. Persons with this form usually develop symptoms in their mid 30s and 40s. An early-onset form of Huntington's disease accounts for a small number of cases and begins in childhood or adolescence. |
|
|
Which heart defect is most commonly associated with Down syndrome?
|
AVSD
- should be repaired by age 6 months to prevent development of pulmonary HTN |
|
|
Compare trisomy 21 (Down syndrome) with trisomy 18 (Edwards syndrome)?
|

|
|
|
What are some general travel precautions and considerations
|
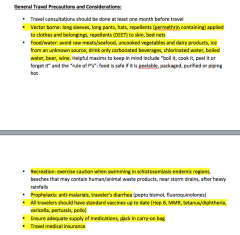
|
|
|
What are some potential travel related infectious diseases?
What are some destination related risks? |
travel related infectious diseases:
- chikungunya - dengue - malaria - hep a/b - measles, mumps, rubells - polio - travel’s diarrhea - yellow fever - rabies - schistosomiasis - tuberculosis destination related risks: - altitude illness - animal bites, insect stings - crime, assault - dvt - jet lag - motion sickness - environmental hazards - temperature extremes |
|
|
What are the 3Rs of immunizations?
|
Routine - adult and child immunizations
Required - crossing international borders Recommended - according to risk |
|
|
What are the vaccines in specific locations that are 'required' in the world?
|
yellow fever:
- required for travel to a country under International Health Regulations (2005) - multiple countries in Africa and S. America (risk generally higher in Africa) meningococcal meningitis - required by Saudi Arabia for religious pilgrims - risks: seasonal in sub-saharan Africa, S. Arabia (required) during Hajj, crowded student dormitory situations |
|
|
What are ‘recommended’ travel immunizations?
|
These vary based on the country travelling, but generally include:
hep a/b (twinrix) typhoid cholera poliomyelitis meningococcal meningitis japanese encephalitis rabies tick-borne encephalitis |
|
|
What is the most common vaccine preventable illness when traveling to developing countries?
|
Travelers Diarrhea
Dukoral is 57% protective against all-caused traveler’s diarrhea |
|
|
Discuss prevention strategies and management of travel’s diarrhea.
|
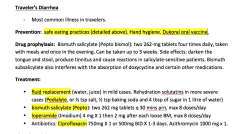
|
|
|
What are the signs/symptoms of altitude sickness?
What are some prevention and management strategies for altitude sickness? |
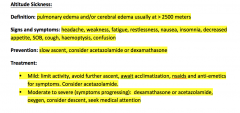
|
|
|
What is the ddx for fever in the returned traveller?
|
- malaria
- rabies - typhoid fever - hepatitis a/b - travel’s diarrhea - dengue fever - yellow fever - tuberculosis |
|
|
What are some travel related specific questions to ask a pt who developed fever after travelling outside of N. America?
|
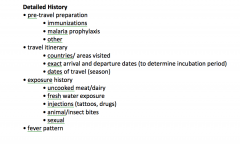
|
|
|
note (99 objectives_travel medicine)
|
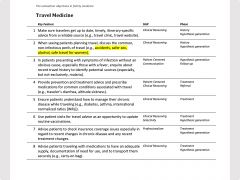
|
|
|
What are some secondary causes of hyperlipidemia?
|
- hypothyroidism
- dm - chronic liver disease - chronic kidney disease others: diet, alcohol |
|
|
Discuss the ddx for acute vs. chronic diarrhea.
|
|
|
|
What are some RFs for developing acute diarrhea?
|
- unsafe food handling
- contact w/ affected person - recent antibiotic use, recent hospitalization - hx of immunosuppression, malnutrition - extremes of age |
|
|
List 3 drugs that can result in diarrhea?
|
- laxatives
- abx - antacid |
|
|
A pt presents to your office with diarrhea that is >8d.
What are some things you would do on physical examination? What are some relevant investigations that you may consider? |
physical exam:
- vitals - fluid status: C BASE HOO - abdominal exam - (rectal exam) - (assessment of extra-intestinal manifestations of ibd if suspicious for this condition [oral ulcers, uveitis etc]) investigations: - cbc (wbc), lytes - stool c+s, o+p, (c. difficile toxin) - (tsh) - (esr, crp) - (celiac serology) - (abdo xray, ct) - (endoscopy, sigmoidoscopy/colonoscopy) |
|
|
What are the some RFs associated with c. difficile associated diarrhea?
|
- recent abx use (most common RF and modifiable)
- recent hospitalization - advanced age - severe illness, immunocompromised - gastric acid suppression - cancer chemotherapy |
|
|
note (99 objectives_diarrhea)
|

|
|
|
List some infectious agents that are associated with bloody diarrhea.
|
- e. coli
- salmonella - campylobacter - c. difficile |
|
|
What is the management of diarrhea?
|
- treat underlying cause
- rehydrate with electrolytes (eg. pedialyte) - imodium [loperamide] (anti-motility agent); pepto-bismol for traveler’s diarrhea - discontinue medications that may be causing diarrhea (eg. laxatives, antiacids) - Abx rarely used - unless targeted based on culture c+s - counseling re: contagiousness - return to work when symptoms resolve or negative culture results - f/u referral (acute diarrhea) -general surg (if peritoneal signs, perforation, or toxic megacolon - ID if unclear of treatment for confirmed infectious and invasive disease referral (chronic diarrhea) - GI if suspicious of ibd (endoscopic examination prn) - dietician for ibs or celiac disease |
|
|
note
|
A test with a low specificity will result in many false positives.
|
|
|
Discuss the quality of evidence for vs against mammograms as a screening tool for breast cancer.
|
|
|
|
What does the periodic health assessment include?
|
education and counselling:
- diet - exercise - sun exposure - sexual health - oral hygiene - personal safety - folic acid (if intending pregnancy) substances: - smoking - alcohol - rec drugs mental health - depression screen physical exam: - vitals + full physical screening tests: - bw_ahe, dm, lipids - ccc - bmd - prostate vs paps + mammogram |
|
|
What is the risk of perforation with colonoscopy?
|
1 in 1000
|
|
|
Compare fobt, sigmoidoscopy, and colonoscopy.
[colon cancer] |
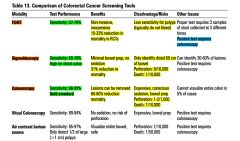
|
|
|
note (99 objectives_palliative care)
|
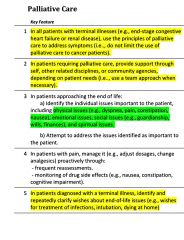
|
|
|
Discuss the main anti-emetics used in palliative care.
[nausea, vomiting] [palliative care] |
i. benedryl
50mg po/rectal/iv q4h prn ii. maxeran (metoclopramide) 5-20mg po/iv q6h prn (n/v due to gastroparesis) iii. zofran (ondansetron) 4-8mg po/iv q4h prn (n/v due to chemotherapy, metabolic (uremia, cirrhosis) iv. dexamethasone 2-8mg po/iv q4h prn (n/v due to inc. ICP, cns pain) |
|
|
Discuss the options for treatment of excessive respiratory secretions.
[palliative care] |
i. atropine drops 1%
1-2 drops orally or under tongue q8h ii. glycopyrrolate 1mg po or 0.2mg sc/iv q4h prn iii. scopolamine |
|
|
Discuss the commonly used opioids and grade then according to their potency.
[palliative care] [palliative care] |

|
|
|
A pt complains of ++ tiredness. He has very low energy levels. You've ruled out the organic causes of this. Write an order that may improve the pts energy levels?
[palliative care] |
ritalin 2.5mg qam +/- 2.5mg in the evening.
note: ritalin aka methylphenidate |
|
|
What is one medication that one can use for unintentional overdosing of an opioid?
[palliative care] |
naloxone (narcan) 0.01-0.04mg IV/IM q3-5 minutes, titrated to respiratory rate or mental status.
|
|
|
What is ESAS?
[palliative care] |

|
|
|
What is the PSS?
[palliative care] |
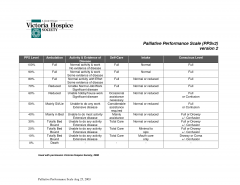
|
|
|
note
[palliative care] |
INVESTIGATIONS
- IN GENERAL, investigations should only be undertaken if their results will allow clinicians to make care decisions beneficial to the patient’s quality of life (eg. do not order CBCs if transfusions are not in keeping with patient’s goals of care). |
|
|
Discuss the multimodality approach to palliative care. i.e. who is/can be involved in the care of palliative pts?
[palliative care] |
- palliative team (doctor, nurses)
- sw - ccac - geriatrics - oncology (if cancer pt) - hospice - chaplain/faith minister |
|
|
In a palliative pt with muscle spasms, what is a medication that may be beneficial?
[palliative care] |
baclofen
|
|
|
Diagrammatically discuss the concept of total pain with regards to palliative care?
[palliative care] |

|
|
|
Discuss the difference between euthanasia and physician-assisted suicide.
|
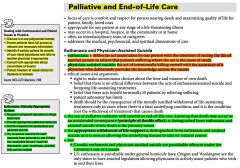
|
|
|
What is gout? What is the joint involvement?
What are the causes of gout? [joint pain] |

|
|
|
What are the signs and symptoms of gout? What investigations if any (gout is often a clinical diagnosis) would you do?
[joint pain] |

|
|
|
Compare gout with pseudogout?
[joint pain] |

|
|
|
What is rheumatoid arthritis?
[joint pain] |
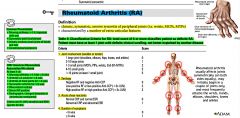
|
|
|
What are some joint deformities that occur in rheumatoid arthritis?
[joint pain] |

also:
- ulnar deviation of mcl; radial deviation of wrist joint - flexion contractures |
|
|
What are some extra-articular features of rheumatoid arthritis?
[joint pain] |

|
|
|
What are side effects of steroids (eg. prednisone)?
|
- weight gain
- osteoporosis, avascular necrosis (avn) - peptic ulcer disease (hence the use of PPIs) - easy bruising - susceptibility to infection - acne - htn, hyperlipidemia - hypokalemia, hyperglycemia - mood swings |
|
|
What are some poor prognostic features of rheumatoid arthritis?
[joint pain] |
- young age of onset
- high RF titre - elevated esr - involvement of >20jts - presence of EAF (extra-articular features) |
|
|
What is Cushing’s syndrome?
|

|
|
|
What are clinical features of Cushing’s syndrome?
|
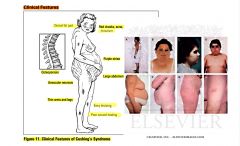
|
|
|
What is the treatment for hypercortisolism —> cushing’s syndrome?
|
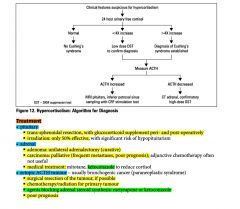
|
|
|
What is the management of rheumatoid arthritis?
[joint pain] |

|
|
|
What is the criteria for systemic lupus erythematous (SLE)?
[joint pain] |
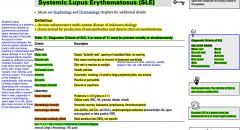
|
|
|
What are some investigations one could do to confirm systemic lupus erythematous (SLE)?
What is the management for SLE? [joint pain] |

|
|
|
What is the ddx for joint pain?
[joint pain, arthritis] |

|
|
|
What is the ddx for monoarthritis?
[joint pain] |

|
|
|
What is the ddx for oligoarthritis/polyarthritis?
[joint pain] |
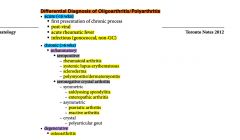
|
|
|
note
[joint pain] |
Septic arthritis is a medical emergency!
|
|
|
Generally compare inflammatory vs. degenerative arthritis.
[joint pain] |

|
|
|
For joint pain, discuss:
- physical exam - investigations [joint pain] |

|
|
|
For joint pain, discuss a relevant history (interview).
[joint pain] |

|
|
|
note
[joint pain] |
- In a pt presenting with a monoarthropathy, rule out infectious causes (eg. STDs such as gonorrhea).
- Clinically diagnose ligamentous injuries. Do NOT do an xray examination. In pts presenting w/ msk pain, include referred and visceral sources of pain in the ddx (eg. angina, slipped capital epiphysis as knee pain, neuropathic pain) In patients experiencing msk pain: - actively inquire about the impact of the pain on daily life - treat with appropriate dose of analgesics - arrange for community resources and aids (eg. splints, cane if necessary) |
|
|
List 3 systemic conditions that may result in joint pain.
[joint pain] |
- systemic lupus erythematous (sle)
- ulcerative colitis - wegener’s granulomatosis |
|
|
note
[joint pain] |
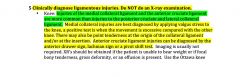
|
|
|
note
[joint pain] |
In assessing pts with a diagnosed rheumatological condition, search for disease-related complications (eg. extra-articular manifestations - iritis, oral ulcers, pleuritis, pericarditis, rash)
|
|
|
How do you estimate date of confinement (EDC)?
[pregnancy lmcc ii] |
Use Naegle's Rule:
1st day of lmp + 9 months + 7 days eg. lmp = April 1, 201 edc = Jan 8, 2012 Modify if cycle > 28days by adding number of days > 28 |
|
|
T/F: Tests for HIV, prenatal and genetic screening are voluntary and require proper counselling and informed consent before proceeding.
[pregnancy lmcc ii] |
True
|
|
|
What advice would you give a woman wanting to get pregnant with regards to folic acid?
[pregnancy lmcc ii] |
- folic acid 0.4-1mg daily in all women (8-12 wks preconception to avoid NTDs)
- folic acid 5mg if previous: NTD, anti-epileptic meds, DM, or if BMI > 35 - continue to take for T1 of pregnancy |
|
|
In pregnancy, with re: to nutrition, what should be the daily caloric increase?
[pregnancy lmcc ii] |
- 1st trimester: daily caloric increase of ~100cal/d
- 2nd trimester: daily caloric increase of ~300cal/d - 3rd trimester and during lactation: daily caloric increase of ~450cal/d Eg: if the total calories/day for a woman is 2200c/d, then during the 2nd trimester, she should be having 2500c/day |
|
|
What are some risk factors for neural tube defects?
[pregnancy lmcc ii] |
- prev. oNTD
- dm - dec. folate and zinc - anti-epileptics - bmi>35 (other answer) GRIMM - Genetics: family hx, consanguinity, chromosomal - Race: European Caucasians > African americans - Insufficient vitamins: zinc and folate - Maternal chronic disease (eg. diabetes) - Maternal use of anti-epileptic drugs |
|
|
How often should a woman come for prenatal visits?
[pregnancy lmcc ii] |
For uncomplicated pregnancies:
- q4-6 weeks until 28 weeks - q2 weeks from 28-36 weeks - weekly from 36 weeks to delivery |
|
|
When are fetal movements typically first noticed by the mother?
[pregnancy lmcc ii] |
at 18-20 weeks; can be earlier by 1-2 wks if multigravidas
|
|
|
Just read
[pregnancy lmcc ii] |
Compared to CVS, amniocentesis has a higher accuracy of prenatal cytogenetic diagnosis (99.8% vs 97.5%) and lower risk of spontaneous abortion (0.5% vs 1-2%)
|
|
|
A woman is intending to get pregnant. What would you discuss with her for pre-conceptual counselling?
[pregnancy lmcc ii] |
- diet (well balanced)
- exercise (prevent obesity) - maintain healthy weight - stop smoking - stop alcohol - avoid rec. drugs - stressors (dec./ avoid), domestic violence - take prenatal vitamins (incl. folic acid) - immunizations (uptodate) - optimize chronic disease (eg. diabetes) - medications contraindicated in pregnancy |
|
|
Routine Trimester 2 U/S at 18-22 weeks, helps determine?
[pregnancy lmcc ii] |
i. number of fetuses
ii. GA (if no prior U/S) iii. Location of placenta iv. fetal anomalies |
|
|
When should GBS screening be done in pregnancy? What are the risk factors of GBS (for neonatal disease) ?
What are some of the consequences of GBS to the baby? [pregnancy lmcc ii] |
at 35-37 weeks
RFs: - GBS bacteriruria during current pregnancy even if treated - previous infant with invasive GBS infection - preterm labour <37 weeks - ruptured membranes > 18 hrs before delivery - intrapartum maternal temperature ≥ 38C - positive GBS screen during current pregnancy CONSEQUENCES to BABY: - neonatal sepsis - meningitis - pneumonia |
|
|
What is the treatment for GBS in pregnancy?
[pregnancy lmcc ii] |
- treatment of GBS at the time of delivery with:
- penicillin G 5 million units IV then 2.5 million units IV q4h until delivery - if penicillin allergic but not at risk for anaphylaxis --> cefazolin - if penicillin allergy and risk for anaphylaxis --> clindamycin |
|
|
T/F. Preeclampsia prior to 20 wks of gestation is usually associated with a complete or partial molar pregnancy.
[pregnancy lmcc ii] |
True
|
|
|
What is the criteria for the diagnosis of pre-eclampsia?
[pregnancy lmcc ii] |
Systolic BP ≥ 140 or
Diastolic BP ≥ 90 AND Proteinuria ≥ 0.3 g in a 24-hr urine specimen |
|
|
For a pregnant patient that comes in suspicious for pre-eclampsia, what investigations would you do?
[pregnancy lmcc ii] |
- cbc, lytes, Cr, bun
- lfts, inr, aPTT, albumin - ldh, bilirubin - urine dip + 24h collection for total protein and creatinine clearance |
|
|
Which anti-hypertensives for the pregnant patient who is hypertensive are NOT appropriate. Which ones are appropriate?
[pregnancy lmcc ii] |
NOT APPROPRIATE (teratogens)
- ACEi - diuretics - propanolol APPROPRIATE: - labelalol 100-300mg bid/tid - α-methyldopa |
|
|
What is the difference between pre-existing HTN and gestational HTN?
[pregnancy lmcc ii] |

|
|
|
What are some complications of gestational HTN?
[pregnancy lmcc ii] |

|
|
|
What is the management for HTN in pregnancy (both preexisting and gestational)?
[pregnancy lmcc ii] |

|
|
|
What is preeclampsia?
|
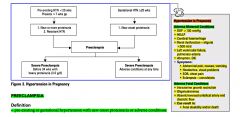
|
|
|
What are the RFs for pre-eclampsia?
[pregnancy lmcc ii] |

|
|
|
What is the management of pre-eclampsia?
[pregnancy lmcc ii] |

|
|
|
What are some risk factors for gestational diabetes mellitus (GDM)?
[pregnancy lmcc ii] |
- Age > 25
- obesity - ethnicity (aboriginal, hispanic, asian, african) - FHx of DM - previous hx of GDM - previous child with BW > 4.0 kg - PCOS - current use of glucocorticoids - essential hypertension or pregnancy-related HTN |
|
|
What is the definition of gestational diabetes mellitus (gdm)?
[pregnancy lmcc ii] |
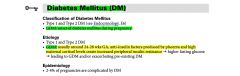
|
|
|
What is the management of dm (Type 1, 2, gdm) in a pregnant patient?
[pregnancy lmcc ii] |

|
|
|
What are some complications of dm/gdm in pregnancy - maternal, fetal, and neonatal?
[pregnancy lmcc ii] |

|
|
|
What is hyperemesis gravidarum?
[pregnancy lmcc ii] |

|
|
|
What weeks do the 3 trimesters comprise of?
[pregnancy lmcc ii] |
1st trimester (0-12 weeks)
2nd trimester (12-28 weeks) 3rd trimester (28-40 weeks) Normal pregnancy TERM: 37-42 weeks |
|
|
Explain the course of b-hCG levels in pregnancy?
[pregnancy lmcc ii] |
- bHCG levels in the plasma double q1-2 days, peak at 8-10 weeks, then fall to a plateau
- bHCG levels in serum appear 9 days post-conception, they appear in the urine 28 days after LMP |
|
|
What are the b-hCG Rule of 10s?
[pregnancy lmcc ii] |
i. 10IU at time of missed menses
ii. 100,000 IU at 10 wks (peak) iii. 10,000 IU at term |
|
|
In pregnancy, does transvaginal or transabdominal U/S detect pregnancy first?
[pregnancy lmcc ii] |
TRANSVAGINAL U/S:
- 5 wks: gestational sac visible (b-hCG > 1200-1500 mIU/mL) - 6 wks: fetal pole seen - 7-8 wks: fetal heart tones visible TRANABDOMINAL U/S: - 6-8 wks: intrauterine pregnancy visible (b-hCG>6500 mIU/mL) |
|
|
What are 4 signs of placental separation?
[pregnancy lmcc ii] |
i. Gush of blood
ii. Lengthening of the cord iii. Uterus becomes globular iv.. Fundus rises |
|
|
T/F. Routine oxytocin administration in 3rd stage of labour can reduce the risk of PPH by >40%.
[pregnancy lmcc ii] |
True
|
|
|
What is the effect of alcohol in pregnancy?
[pregnancy lmcc ii] |
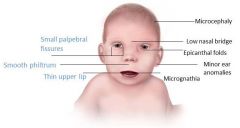
- increased incidence of abortion, stillbirth
- congenital anomalies fetal alcohol syndrome: - growth retardation - CNS involvement - facial anomalies |
|
|
What are the safest antibiotics to give during breastfeeding? What harmful effects can be caused by: erythromycin, tetracyclines, sulpha drugs, metronidazole, fluoroquinolones?
[pregnancy lmcc ii] |
SAFEST:
- ampicillin, cephalosporins DRUGS TO AVOID: - erythromycin: may cause maternal liver damage (acute fatty liver) - tetracyclines: stain infant's teeth, may affect long bone development - sulpha drugs: anti-folate properties, therefore risk in T1; risk of kernicterus in T3 - metronidazole: anti-metabolite, therefore theoretical risk in T1 - chloramphenicol (bone marrow suppression) - fluoroquinolones: risk of cartilage damage - psychotropic drugs - lithium |
|
|
What is the effect of cigarette smoking in pregnancy? What is the effect of cocaine in pregnancy?
[pregnancy lmcc ii] |
CIGARETTE SMOKING:
- dec. birth weight - placenta previa/abruption - spontaneous abortion - preterm labour - stillbirth COCAINE: - microcephaly - growth retardation - prematurity - mental retardation - placental abruption |
|
|
What is eclampsia?
[pregnancy lmcc ii] |
Eclampsia refers to the development of grand mal seizures in a woman with preeclampsia, in the absence of other neurologic conditions that could account for the seizure.
|
|
|
Just read
[pregnancy lmcc ii] |
The definitive treatment of preeclampsia is delivery to prevent development of maternal or fetal complications from disease progression. Timing of delivery is based upon gestational age, the severity of preeclampsia, and maternal and fetal condition.
Severe preeclampsia is generally regarded as an indication for delivery, regardless of gestational age, given the high risk of serious maternal morbidity. However, prolonged antepartum management in a tertiary care setting or in consultation with a maternal-fetal medicine specialist is an option for selected women remote from term (<34 weeks of gestation). For women with mild preeclampsia, we suggest expectant management with delivery at ≥37 weeks of gestation (Grade 2B). Expectant management of women with mild preeclampsia consists of frequent laboratory monitoring (platelet count, liver and renal function tests), assessment of maternal blood pressure and symptoms, and evaluation of fetal growth and well-being. For women with preeclampsia between 23 and 34 weeks of gestation, we recommend a course of antenatal glucocorticoids (betamethasone) (Grade 1A). For women with severe preeclampsia, we recommend seizure prophylaxis (Grade 1A). The benefit of seizure prophylaxis is less clear in mild preeclampsia; however, we suggest prophylaxis in these women (Grade 2B). We recommend use of magnesium sulfate rather than phenytoin for seizure prophylaxis (Grade 1A). |
|
|
In pre-eclampsia what is the proteinuria concentration. What is it in severe pre-eclampsia?
[pregnancy lmcc ii] |
PRE-ECLAMPSIA
- proteinuria >300mg/d SEVERE PRE-ECLAMPSIA - proteinuria 3-5g/d |
|
|
Which immunizations are safe, which ones are contraindicated?
[pregnancy lmcc ii] |
INTRAPARTUM:
- safe: tetanus toxoid, diphtheria, influenza, hep B - avoid live vaccines (risk of placental and fetal infection): polio, measles/mumps/rubella, varicella - contraindicated: rubella, oral typhoid POSTPARTUM: - rubella vaccine for all non-immune mothers - hep B vaccine should be given to infant within 12h of birth if maternal status unknown or positive - follow up doses at 1 month and 6 months |
|
|
What is the management of patients with severe pre-eclampsia?
[pregnancy lmcc ii] |
- ABCs
- treat HTN - seizure prevention and control - deliver fetus |
|
|
How are hypertensive disorders in pregnancy classified?
[pregnancy lmcc ii] |
1. Pre-existing (<20wks GA) - 90% are essential, 10% are secondary
2. gestational (≥20 wks GA) Pre-eclampsia can occur with either pre-existing or gestational HTN |
|
|
What is the management HTN with preeclampsia?
[pregnancy lmcc ii] |
HTN WITH PREECLAMPSIA
- Stabilize and deliver (only cure is to deliver) - Increase maternal and fetal monitoring i. Anti-convulsant therapy (raises seizure threshold) - give MgSO4 IV bolus, monitor for signs of Mg toxicity (depressed deep tendon reflexes, decreased RR, anuric, hypotonic, CNS or cardiac depression ii. Anti-hypertensive therapy: (lower BP lowers risk of stroke) - labetalol - hydralazine - nifedipene (2nd line) iii. Post-partum management: (risk of seizure is highest in the first 24 hrs postpartum) - continue giving MgSO4 for 12-24 hrs after delivery; vital q1h; consider HELLP syndrome in toxic patients |
|
|
What is Symphysis Fundal Height (SFH) at 12 weeks, 20 weeks, and 37 weeks?
[pregnancy lmcc ii] |
- at 12 weeks: uterine fundus is at pubic symphysis
- at 20 weeks: fundus is at the umbilicus. SFH should be within 2 cm of GA between 20 and 36 weeks - at 37 weeks: fundus at the sternum |
|
|
How does uterine rupture occur? How does it present? What is the management? What are the complications?
[pregnancy lmcc ii] |
- assoc. with previous uterine scar (~40% of cases)
- hyperstimulation with oxytocin - grand multiparity - previous uterine manipulation - generally occurs during labour, but can occur earlier with a classical incision PRESENTATION - prolonged fetal bradycardia (MOST COMMON PRESENTATION) - acute onset abdominal pain - hypotonic/hypertonic uterine contractions - vaginal bleeding MANAGEMENT - r/o placental abruption - immediately stabilize and deliver (may require hysterectomy) COMPLICATIONS: - maternal hemorrhage, shock, DIC - amniotic fluid embolus - fetal distress/mortality, maternal mortality SIDE NOTE: fetal bradycardia also occurs with cord compression |
|
|
What is dystocia? What are the causes of dystocia?
[pregnancy lmcc ii] |
Abnormal progression of labour:
- during active phase of 1st stage: >4 hrs of <0.5cm/hr - during 2nd phase: >1 hr with no descent during active pushing Causes of dystocia? i. power (leading cause): contractions (hypotonic, incoordinate), inadequate maternal expulsive efforts ii. passenger: fetal position, size, attitude, anomalies (hydrocephalus) iii. passage: CPD, maternal soft tissue masses iv. psyche: stress hormones released can bring about dystocia |
|
|
For shoulder dystocia, what
- are the RFs? - presentation? - management? [pregnancy lmcc ii] |
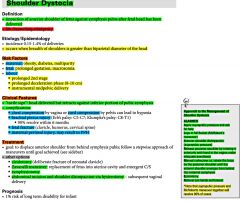
|
|
|
What is a Normal NST?[pregnancy lmcc ii]
What is the indication for NST? [pregnancy lmcc ii] |
normal nst:
2 accelerations, >15bpm from baseline, lasting >15s in 20 mins Indication for nst: Any suggestion of uteroplacental insufficiency or suspected fetal distress. |
|
|
What is a Non-stress test (NST)? What is a Normal (reassuring) NST? What is an abnormal (non-reassuring NST)?
|
- Fetal heart rate (FHR) tracing ≥20 mins using an external Doppler to assess FHR and its relationship to fetal movement
- It is indicated for any suggestion of uteroplacental insufficiency or suspected fetal distress. ------------------------------ - Normal NST: at least 2 accelerations of FHR > 15bpm from the baseline lasting > 15s, in 20 minutes - Abnormal NST: <2 accelerations of FHR in 40 minutes. If no observed fetal movement in the 1st 20 mins, stimulate fetus (fundal pressure, acoustic/vibratory stimulation) and continue monitoring for 30 minutes. If NST abnormal, then perform biophysical profile (BPP). |
|
|
What is a biophysical profile (BPP)? What are the indications? and what is a reassuring BPP?
[pregnancy lmcc ii] |
- U/S assessment of the fetus ± NST
INDICATIONS: - abnormal NST - decreased fetal movement - any other suggestion of fetal distress or uteroplacental insufficiency - post term pregnancy A BPP of 8/8 Pneumonic: LAMB - AFV 2cm x 2cm - Limb extension + flexion - Movement (3 discrete) - Breathing (one episode) x 30s |
|
|
What are some gestational dependent screening investigations and when do they occur?
[pregnancy lmcc ii] |

|
|
|
What is the management for pregnancy termination?
[pregnancy lmcc ii] |

|
|
|
What would you give to a patient who has Mg toxicity?
[pregnancy lmcc ii] |
calcium gluconate by IV
|
|
|
Differentiate true labour from false labour.
[pregnancy lmcc ii] |
TRUE LABOUR: regular, painful contractions of increasing intensity associated with PROGRESSIVE dilatation and EFFACEMENT of cervix and DESCENT of presenting part, or progression of station
- preterm (>20 but <37 wks) - term (37-42 wks) - post-term >42 wks) FALSE LABOUR: Braxton-Hicks contractions - irregular contractions, with unchanged intensity and long intervals, occur throughout pregnancy and not associated with any dilatation, effacement, or descent - often relieved by rest or sedation |
|
|
What is the approach to the management of abnormal FHR?
[pregnancy lmcc ii] |
- Ensure fetal tracing
- call for help - 100% O2 by mask - Stop oxytocin - correction maternal hypotension - fetal scalp pH/fetal scalp electrode - vaginal exam to r/o cord prolapse - rule out fever, dehydration, drug effects, prematurity - Amnioinfusion or tocolytics in selected cases - C/S when necessary |
|
|
Compare early, variable, and late decelerations? (Picture)
[pregnancy lmcc ii] |
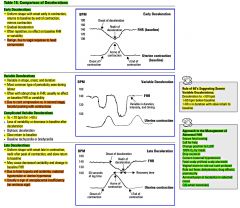
|
|
|
What is the classification of intrapartum EFM tracings?
[pregnancy lmcc ii] |

|
|
|
What is postpartum hemorrhage (PPH)? What is the DDx for early PPH and the DDx for late PPH?
[pregnancy lmcc ii] |
- Loss of >500mL of blood at the time of vaginal delivery, or >1000mL with C/S
- Early: within 1st 24 hrs - Late: between 24 hrs and 6wks DDx of Early PPH: i. Tone (atony - MOST COMMON CAUSE) ii. Tissue (retained placenta, clots) iii. Trauma (laceration, inversion) iv. Thrombin (coagulopathy) DDx of Late PPH: i. retained products ii. +/- endometritis iii. sub-involution of uterus |
|
|
Retained placenta is when the placenta is undelivered after 30 mins postpartum. What are the causes of this? What is the presentation? What exams/investigations would you do? Management?
[pregnancy lmcc ii] |
Causes:
- abnormal placental implantation (placenta accreta, increta, percreta) PRESENTATION: - incomplete placenta removed - risk of postpartum hemorrhage and infection INVESTIGATIONS: - explore uterus - assess degree of blood loss MANAGEMENT: - 2 large bore IVs, type and screen - Brant maneuver (firm traction on umbilical cord with one hand applying suprapubic pressure to avoid uterine tension by holding uterus in place) - oxytocin - manual removal if above fails - D&C if required |
|
|
What is endometritis?
What are RFs of endometritis? What is the treatment? [pregnancy lmcc ii] |
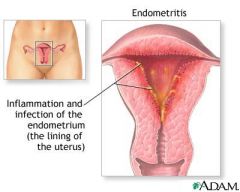
Infection of the uterus
Presents with: - fevers, chills - abdo pain, uterine tenderness, - foul-smelling discharge or lochia RFs: - C/S - intrapartum chorioamnionitis - prolonged labour - prolonged ROM - multiple vaginal examinations Treatment: - oral Abx if well - IV Abx with hospitalization in moderate to severe cases |
|
|
What is the puerperium period? What are some complications within this period?
[pregnancy lmcc ii] |
Its the 6 wk period of adjustment after pregnancy when pregnancy-induced anatomic and physiologic changes are reversed
COMPLICATIONS: - PPH - retained placenta - uterine inversion |
|
|
note
[pregnancy lmcc ii] |
In a breast-feeding woman, screen for and characterize dysfunctional breast-feeding (e.g. poor latch, poor production, and poor letdown)
|
|
|
Define the following terms: premature ROM, prolonged ROM, preterm ROM, PPROM. What are the risk factors for PROM?
[pregnancy lmcc ii] |
* Normally labour begins and then membranes rupture
premature ROM (PROM) - rupture of membranes prior to labour at any GA prolonged ROM: >24hrs elapsed between rupture of membranes and onset of labour preterm ROM: ROM occurring before 37 weeks gestation (assoc with PTL) preterm premature ROM (PPROM): rupture of membranes before 37 wks AND prior to onset of labour RISK FACTORS: MATERNAL (multiparty, cervical incompetence, infection (cervicitis, vaginitis, STI, UTI, family hx of PROM, low SES, poor nutrition; FETAL: congenital anomaly, multiple gestation |
|
|
What would be the management for a patient with premature rupture of membranes?
[pregnancy lmcc ii] |

|
|
|
How would you be sure that a pregnant women has membrane rupture?
[pregnancy lmcc ii] |
i. Pooling of fluid on speculum exam (in posterior fornix, may even fluid leak out of cervix)
ii. increased pH of vaginal fluid (nitrazine test) iii. ferning of fluid under light microscopy iv. decreased AFV on U/S NOTE: Nitrazine has low specificity as can be positive with blood, urine or semen |
|
|
What is uterine atony?
[pregnancy lmcc ii] |
Uterine atony is a loss of tone in the uterine musculature. Normally, contraction of the uterine muscle compresses the vessels and reduces flow. This increases the likelihood of coagulation and prevents bleeds. Thus, lack of uterine muscle contraction can cause an acute hemorrhage. Clinically, 75-80% of postpartum hemorrhages are due to uterine atony.
|
|
|
What drug should one use for augmentation of labour?
[pregnancy lmcc ii] |
oxytocin
|
|
|
Which 2 drugs can be given to enhance fetal lung maturity?
[pregnancy lmcc ii] |
i. Betamethasone valerate (Celestone)
ii. Dexamethasone both given IM |
|
|
What are some complications of PROM?
[pregnancy lmcc ii] |
- chorioamnionitits
- cord prolapse - premature delivery - limb contracture |
|
|
What is HELLP syndrome?
[pregnancy lmcc ii] |
HELLP syndrome is a life-threatening obstetric complication usually considered to be a variant or complication of pre-eclampsia.[1] Both conditions usually occur during the later stages of pregnancy, or sometimes after childbirth.
Hemolysis Elevated Liver enzymes Low Platelets |
|
|
What is the management of a pregnant patient undergoing preterm labour?
[pregnancy lmcc ii] |
A. INITIAL
- transfer to appropriate facility if stable - hydration - bed rest LLDP - sedation (morphine) - avoid repeat pelvic exams - U/S examination of fetus B. TOCOLYSIS (suppression of labour) - does not inhibit preterm labour completely but may buy time to allow for Celestone and/or transfer to appropriate facility - agents: Nifedipine, Indomethacin C. ENHANCEMENT OF FETAL LUNG MATURITY - betamethasone valerate (celestone) or dexamethasone D. Cervical cerclage (benefits mainly for prevention of preterm labour in a patient with an incompetent cervix) - usually placed at the end of the 1st trimester and removed in the 3rd trimester |
|
|
A pregnant woman comes in and is discovered to have asymptomatic bacteruria? What'll you do ?
[pregnancy lmcc ii] |
TREAT IT !
because in pregnancy, there is increased risk of progression to cystitis, pyelonephritis, and probable increased risk of PRETERM LABOUR UNCOMPLICATED UTI: - amoxicillin x 7 days or - TMP-SMX (Septra) or nitrofurantoin PYELONEPHRITIS - hospitalization - IV Antibiotics |
|
|
What is Virchow's Triad for venous thromboembolism (VTE)?
[pregnancy lmcc ii] |
1. Hypercoagulable state (incl. preg, use of ocp, malignancy)
2. Venous stasis 3. Endothelial damage |
|
|
What is the management in PPH?
[pregnancy lmcc ii] |
BASICS:
- ABCs, vitals, CBC, lytes, pRBC cross and type, coat profile, 2 large bore IVs and crystalloids, treat underlying cause MEDICAL THERAPY: - Oxytocin 20U/L in NS or RL (IV infusion) - Ergotamine IM or IV bolus - Carboprost (hemabate) LOCAL CONTROL: - bimanual compression: elevate uterus and massage through patient's abdomen - uterine packing: mesh with Abx treatment - intrauterine balloon tamponade SURGICAL (intractable PPH): - D&C (careful, b/c vigorous scraping may cause Asherman's syndrome) - laparotomy with bilateral ligation of uterine artery, ovarian artery or hypogastric artery - hysterectomy (last option) with angiographic embolization if post-hysterectomy bleeding |
|
|
What is uterine inversion? Etiology? Clinical Features? Management?
[pregnancy lmcc ii] |
Turning inside out (inversion) of the uterus through cervix +/- vaginal introitus. ETIOLOGY: often iatrogen (excess cord traction with fundal placenta), excessive tocolytics, more common in grand multiparous
CLINICAL FEATURES: - may cause profound vasovagal response with vasodilation and hypovolemic shock - shock may be disproportionate to maternal blood loss MANAGEMENT - ABCs, give IV crystalloids - can use tocolytic drug (eg. terbutaline) or nitroglycerin IV to relax uterus and aid replacement - replace uterus without removing placenta; remove placenta manually and withdraw slowly - IV oxytocin infusion (only after uterus replaced) - re-explore uterus - may require GA +/- laporotomy |
|
|
note (99 objectives_pregnancy)
|
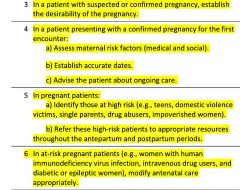
|
|
|
note (99 objectives_disability)
|

|
|
|
What are the causes of falls in the elderly?
What investigations would you do in this patient? What are some falls prevention strategies? |

|
|
|
What are the common causes/ddx of dementia?
|
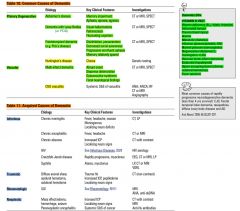
|
|
|
What is alzheimer's dementia (AD)?
|
Progressive cognitive decline interfering w/ social and occupational functioning characterized by:
i. anterograde amnesia (impaired ability to learn new info) ii. one of the following cognitive disturbances - aphasia (language disturbance) - apraxia (impaired ability to carry out motor activities despite intact motor function) - agnosia (failure to recognize or identify objects despite intact sensory function) - disturbance in executive function - impaired planning, organizing, sequencing, abstracting |
|
|
T/F. down's syndrome predisposes to early onset of alzheimer's disease.
|
True
|
|
|
What are some RFs for alzheimer's dementia?
|
- family hx of AD
- head injury - low education level - smoking - down's syndrome |
|
|
Discuss the cffm memory clinic clinical reasoning model.
|

|
|
|
Discuss the diagnosis of delirium on the basis of the 'confusion assessment method'.
|
- diagnosis of delirium requires criteria 1 and 2, plus either 3 or 4
1. acute onset and fluctuating course 2. inattention 3. disorganized thinking 4. altered level of consciousness |
|
|
What is the etiology of delirium?
|
I WATCH DEATH
infectious withdrawal (drugs) acute metabolic d/o trauma cns pathology hypoxia deficiency_vitamins endocrinopathies acute vascular insults toxins heavy metals SIMPLIFIED (common) - drugs - infection - metabolic imbalance - organ failure |
|
|
What are the 1st line drugs for delirium?
|
i. haldol
ii. risperidone note: ativan may make delirium worse |
|
|
Before diagnosis someone w/ dementia. One must always check for reversible causes of the pt's symptoms. What tests are indicated?
|
- bw: cbc, lytes, tsh, b12, Cr, glucose, Ca, albumin
- urinalysis (urine dip) - ct/mri |
|
|
How do you differentiate between:
- normal aging - mild cognitive impairment (mci) - dementia |
normal aging
- no objective cognitive loss - recalls w/ cueing - no impairment in ADLs mild cognitive impairment (mci) - cognitive loss - no impairment of ADLs dementia - cognitive loss - impairment of ADLs |
|
|
note
|
for pts w/ mild cognitive impairment you do not treat w/ cholinesterase inhibitors as their condition may worsen; however, in pts w/ dementia, cholinesterase inhibitors are used
|
|
|
For mild cognitive impairment (mci), one does not use cholinesterase inhibitors as a pt's condition may worsen. What are some non-pharmacological options for treatment of mci?
|
i. mediterranean diet
ii. exercise iii. social networking iv. mental stimulation |
|
|
Differentiate between ADLs and iADLs.
|
basic ADLs: (DEATH)
dressing eating ambulating toileting hygiene instrumental ADLs: (SHAFT) shopping housekeeping accounting food preparation transportation |
|
|
What is the difference between the mmse and the moca?
|
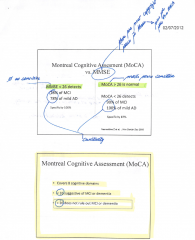
|
|
|
What is a mixed dementia?
|
alzheimer's + vascular dementia
|
|
|
What is frontotemporal dementia (FTD)?
|
DEFINITION
- progressive changes in behaviour/personality, or progressive decline in language or praxis (early decline in regulation of personal and social interpersonal conduct, early emotional blunting and loss of insight) - early onset: 45-65 (mean age 50) - early loss of executive function ---------------------------------------------------- 1°: picks, ALS, idiopathic 2°: huntingtons, etoh, nph, strokes, copd, sleep apnea 2 types: - behavioural varient - language variant: progressive nonfluent aphasia, semantic dementia |
|
|
What is the difference between parkinson's disease dementia (pdd) and lewy body dementia (lbd)?
|
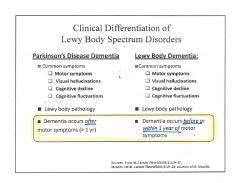
|
|
|
Discuss the prevalence rates of the different types of dementia.
|
alzheimer's (60-80%)
vascular (10-20%) mixed ftd (5-10%) lbd (5-15%) |
|
|
note
|
For pts w/ frontotemporal dementia, one can use SSRIs or trazodone for pharmacotherapy; however, one should avoid cholinesterase inhibitors as these can make pts worse. Pts can get agitated on cholinesterase inhibitors.
|
|
|
For which dementia types can cholinesterase inhibitors be used?
|
- alzheimers
- lewy body dementia - parkinson's disease dementia Not used in frontotemporal dementia |
|
|
What are some relative contraindications for cholinesterase inhibitors (note: these drugs are used in dementia)?
|
- lbbb
- 2° or 3° heart block - bradycardia <50 note: this is why its important to do an ekg prior to starting AchEIs |
|
|
When should one report a patient w/ possible dementia to the ministry of transportation (MOT)?
|
- ftd, dlb/pdd
- abnormal cognitive tests, esp. tests of visuospatial or executive functioning (trails b) - loss of 2 iADLs or 1 ADL |
|
|
List some cholinesterase inhibitors (AchEIs).
|
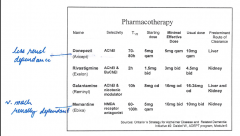
|
|
|
What are some common S/Es of cholinesterase inhibitors (AchEIs)?
|
- nausea
- diarrhea - wt loss - h/a - insomnia - dizziness |
|
|
When should one refer a dementia pt to a specialist?
|
- ftd
- dlb/pdd - rapidly progressing dementia - diagnosis/management not clear - to support decision not to drive |
|
|
A pt presents w/ symptoms of anxiety. It is always important to:
i. exclude serious medical pathology ii. identify other co-morbid psychiatric conditions What medical pathology may mimic anxiety; What are some co-morbid psychiatric conditions assoc. w/ anxiety disorders? |
medical pathology (that may mimic anxiety:
- cvs: mi, chf, pe, arrhythmias - resp: asthma, copd, pneumonia - endocrine/metabolic: hyperthyroidism, pheochromocytoma, vit b12 deficiency - neurological: neoplasm, encephalitis - substance induced: intoxication (caffeine, cocaine) and withdrawal (alcohol) co-morbid psychiatric conditions that are assoc. w/ anxiety disorders: - mood disorders - psychotic disorders - personality disorders - substance abuse NOTE: medical workup for anxiety disorder would include: bw_cbc, lytes, tsh, b12, urinalysis, urine drug screen, cxr, ecg |
|
|
What is panic disorder (w/o agoraphobia)?
|
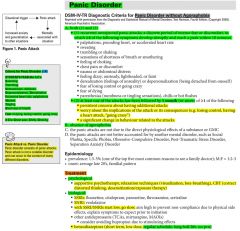
|
|
|
What is panic disorder (w/ agoraphobia)?
|

|
|
|
What is generalized anxiety disorder?
|
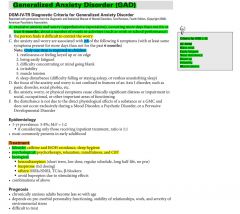
|
|
|
What is social phobia (social anxiety disorder)?
|

|
|
|
What is the management of obsessive-compulsive disorder (ocd)?
|
i. cbt
ii. medications: - SSRIs - atypical/typical antipsychotics (risperidone, haldol) |
|
|
What is the management of ptsd?
|
i. cbt
ii. medications: - SSRIs - benzodiazepines - atypical antipsychotics iii. emdr (eye movement desensitization and reprocessing) |
|
|
What is the diagnostic criteria for ptsd?
|
a) exposure to a traumatic event
b) re-experiencing the traumatic event c) avoidance of stimuli assoc. w/ the trauma d) symptoms of inc. arousal e) duration: ≥1 month f) impairment in social, occupational, or other important areas of functioning |
|
|
What are some risk factors for DVTs?
|
THROMBOSIS
trauma, travel hypercoagulable, hrt recreational drugs (ivdu) old (age>60) malignancy birth control pill obesity, obstetrics surgery, smoking immobilization sickness (chf, mi, nephrotic syndrome, vasculitis) |
|
|
What is the presentation of a dvt?
|
unilateral leg:
- pain - swelling, - erythema - warmth - palpable cord on palpation - can be asymptomatic (note: absence of physical findings does not rule out disease note: the classic 'Homan's sign' (sharp calf pain on passive dorsiflexion of foot) has proven to be insensitive and nonspecific, therefore it's not very useful. |
|
|
What is the ddx of a dvt?
|
- cellulitis
- arterial occlusive disease - muscle strain/tear - lymphangitis/lymph obstruction - ruptured popliteal cysts |
|
|
DVT of the lower extremity is subdivided into proximal (thigh) and distal (calf) thrombosis. Which is considered more clinically important?
|
Proximal vein thrombosis is considered more clinically important as it is commonly associated with serious disease and fatal outcomes.
|
|
|
What is the ddx for unilateral leg swelling?
|
i. vascular: dvt, venous insufficiency, chronic superficial thrombophlebitis
ii. lymphatic: lymphedema (chronic) iii. drugs (ccb) iv. msk: cellulitis, nec. fasciitis, knee injury, baker's cyst/rupture |
|
|
note
|
silent PE is present in approximately 40-60% of patients who present with a dvt.
|
|
|
What investigations would you do in someone with a suspicion of dvt?
|
i. d-dimer (only useful to r/o dvt if neg. and low clinical suspicion of disease); neg. predictive value >99%
ii. doppler u/s (most useful) iii. mri iv. venography (gold standard, but expensive, invasive, and higher risk) note: - doppler u/s sensitivity and specificity for proximal dvt is ~95% - sensitivity for calf dvt is ~70% note: under bw, you may also order: - pt - ptt - platelet count - others: protein S, protein C, fibrinogen, lupus anticoagulant |
|
|
What is the Well's criteria for calculating the pre-test probability of a dvt?
|
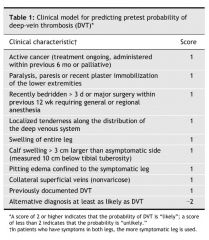
Those with Wells scores of two or more have a 28% chance of having DVT, those with a lower score have 6% odds. Alternatively, Wells scores can be categorized as high if greater than two, moderate if one or two, and low if less than one, with likelihoods of 53%, 17%, and 5% respectively.
SIMPLIFIED risk score interpretation: low: 0 moderate: 1-2 high: ≥3 depending on risk score, one should follow the diagnostic algorithm for dvt |
|
|
Discuss the diagnostic algorithm for dvts.
|
|
|
|
If a pt has a moderate-high probability of having a dvt and the u/s comes back negative, should one do a followup u/s?
|
yes in 5-7 days
|
|
|
What is the treatment for dvts?
|
1. LMWH for 7 days followed by PO warfarin (therapeutic INR 2-3). Recommended dose of enoxaparin is 1mg/kg q12h sc.
Recommended duration of anticoagulation: i. 3-6 mo for pts w/ reversible risk factors (low-risk group). Increased D-dimer level measured after 3 months of anticoagulation in pts w/ unprovoked DVT should favour a longer course. ii. at least 6 months for pts w/idiopathic venous thrombosis or medical risk factors for DVT (intermediate-risk group) iii. indefinite for pts w/DVT associated w/active cancer; pts w/inherited thrombophilia (e.g., deficiency of protein C or S Ab), antiphospholipid, and recurrent episodes of idiopathic DVT (high-risk group). 2. Long-term LMWH may be preferable to warfarin in pts w/cancer 3. Outpatient rx of DVT is appropriate for pts w/o prior DVT, thrombophilic conditions, or substantial comorbidity. 4. Exclusions from outpatient treatment of DVT include pts w/potential high complication risk (e.g., Hgb <7, platelet count <75,000, guaiac-positive stool, recent CVA or noncutaneous surgery, noncompliance). 5. Compression stockings are effective in decreasing the incidence of post-thrombtoic syndrome and should be started within one month of proximal DVT and used for at least 1 year after dx. 6. IVC filter to prevent PE is recommended for patients with contraindications to DVT. |
|
|
When is vte prophylaxis appropriate?
|
- acute mi, acute stroke
- general medical pts - immobilized, especially those with chf, resp failures, infections, nephrotic syndrome, IBD - cancer pts - when immobilized - surgical pts - general/gyne/ortho/trauma/urology/cardiothoracic/peripheral vascular surgery note: lmwh is contraindicated in neurosurgery pts, carries inc. risk of intracranial hemorrhage. |
|
|
What is post-phlebitic syndrome?
|
- occurs after dvt; persistent pain, heaviness, and swelling 2° incompetent valves
- complications: venous ulcers, dermatitis, purpura - treatment compression stockings Post-phlebitic syndrome can affect 23-60% of patients in the two years following DVT of the leg. Of those, 10% may go on to develop severe post-phlebitic syndrome, involving venous ulcers. |
|
|
note
|
Compression stockings are used in pts recovering from dvts to treat and prevent post-phlebitic syndrome.
|
|
|
In pts w/ dvt, which is unexpected (given their low risk factors), one must consider underlying coagulopathy. When should thrombophilia workup be done?
|
- age <45
- unprovoked situation - family hx (≥2 1st degree relatives - clot in unusual location - multiple events in the same pt - vte during pregnancy and/or prev. pregnancy complication |
|
|
Discuss the 4 stages of alcohol withdrawal and the symptoms assoc. with these stages.
|

|
|
|
What is the management of alcohol withdrawal?
|

|
|
|
What is Wernicke-Korsakoff Syndrome and what is the management of this condition?
|
- alcohol induced amnestic disorder due to thiamine deficiency. The thiamine deficiency occurs due to alcohol abuse in chronic alcoholics.
Main symptoms are: - impaired memory - ataxia (gross lack of coordination of muscle movements) - vision changes Note: these patients also tend to be malnourished. TREATMENT: thiamine supplements |
|
|
What are some management strategies of alcohol dependance?
|

|
|
|
What are cocaine withdrawal symptoms?
What is the management? |
- initial crash (1-48 hrs): increased sleep, increased appetite
- withdrawal (1-10 wks): dysphoric mood plus fatigue, irritability, vivid unpleased dreams, insomnia or hypersomnia, psychomotor agitation or retardation Management is supportive management |
|
|
T/F. For cocaine abuse, there aren't too many medical options to prevent or reduce abuse, rather psychotherapy, group therapy and behaviour modification may be helpful.
|
True
|
|
|
What are some things that happen with acute intoxication of opioids?
What is a toxic reaction to opioids? What is the treatment for a toxic reaction? What is the treatment for chronic abuse of opioids? |
Opioids directly effect the CNS resulting in:
- decreased pain perception, sedation - respiratory depression - nausea/vomiting, dec GI motility (constipation and anorexia) - decreased sex drive In a toxic reaction, patients may have shallow respirations, mitosis, bradycardia, hypothermia, decreased LOC Treatment of toxic reaction to opioids: - ABCs - IV glucose - naloxone (Narcan) - patient will need intubation and mechanical ventilation Treatment of chronic opioid abuse: - psychosocial (Narcotics anonymous) - methadone (relieves drug cravings and withdrawal symptoms) - naltrexone/naloxone |
|
|
What class of drugs do naloxone and naltrexone fall under?
|
opioid antagonists
|
|
|
note (99 objectives_substance abuse)
|
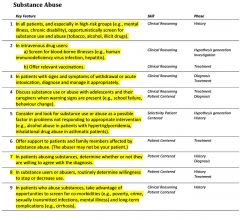
|
|
|
note
|
In adolescents:
− Screen for substance use in conditions known for comorbid association (anxiety, depression, ADHD, ODD, CD, PTSD) − Think of substance use when dealing with issues of poor performance in school, poor concentration, poor weight gain − Screen especially in families with poor social support, known parental substance abuse, or delayed development |
|
|
note
|
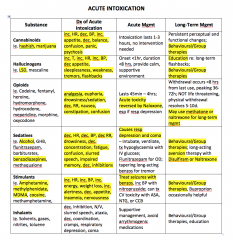
|
|
|
How would someone with cannabis/marijuana intoxication present?
|
CANNABIS INTOXICATION:
- tachycardia - conjunctival vascular engorgement - dry mouth - increased appetite - increased sense of well being - euphoria/laughter - muscle relaxation - impaired performance on psychomotor tasks including driving High doses can cause depersonalization, paranoia, and anxiety May trigger psychosis and schizophrenia in predisposed individuals V. minor withdrawal, not significant |
|
|
What is Delirium Tremens?
|
Alcohol withdrawal delirium, occurs 3-5 days after alcohol withdrawal. Symptoms include:
- Autonomic hyperactivity: tachycardia, tachypnea, diaphoresis - N/V - anxiety - hand tremor - tonic-clonic seizures - insomnia - visual/auditory/tacile hallucinations - persecutory delusions |
|
|
How would someone with amphetamine (includes amphetamine, methampethamine, street names: speed) intoxication present?
|
PRESENTATION
- euphoria - improved concentration - sympathetic and behavioural hyperactivity at high doses may cause coma Chronic use can produce a paranoid psychosis diagnostically similar to schizophrenia with agitation, paranoia, delusions and hallucinations - Withdrawal Sx include: dysphoria, fatigue, restlessness - antipsychotics useful in treatment of stimulant psychosis |
|
|
List some Hallucinogens. How would someone with LSD intoxication present?
|
HALLUCINOGENS: LSD, mescaline, psilocybin, PCP, cannabis, ecstasy, saliva
LSD is a highly potent drug: intoxication is characterized by tachycardia, HTN, mydriasis (dilated pupils), tremor, hyperpyrexia (fever), variety of perpetual and mood changes. High doses of LSD can cause depersonalization, paranoia, anxiety No specific withdrawal symptoms characterized |
|
|
What is the ddx for a breast lump/mass?
|
- fibrocystic changes
- fibroadenoma - fat necrosis - papilloma - galactocele - ductal hyperplasia - lipoma - neurofibroma - abscess - silicone implant - breast Ca* *malignant |
|
|
What is the most common cause of unilateral spontaneous blood nipple discharge?
|
intraductal papilloma
|
|
|
Compare breast fibrocystic changes vs. fibroadenoma.
|
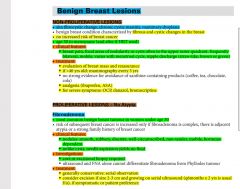
|
|
|
What are some of the RFs for breast Ca?
|
- gender (female)
- age - prior hx of breast Ca - previous breast biopsy (regardless of result) - 1st degree relatives w/ breast Ca - high breast density, nulliparity, 1st preg >30yrs old, menarche <12; menopause >55 - radiation exposure - >5 yrs HRT note: breast Ca is the 2nd leading cause of mortality in women (1st is lung cancer) note: gender followed by age are the two greatest RFs for breast Ca. |
|
|
What are investigation options for diagnosing breast cancer?
|

|
|
|
What are favourable vs. unfavourable features of breast cancer?
|

|
|
|
note
|
90% of breast cancers are sporadic; whereas 5-10% of breast cancers are due to mutations in the brca1 and brca2 genes
|
|
|
Is the clinical breast examination (cbe) still valid?
|
No, as per the 2011 CTFPHC guidelines, in asymptomatic women, the cbe is not recommended; neither is the breast self exam.
The self breast exam has no benefit w/ regards to survival; but instead is associated w/ inc. no. of physician visits and increased rate of biopsy results. |
|
|
What are the indications for genetic screening for the brca 1/2 genes (breast cancer)?
|
- pt diagnosed w/ breast and ovarian cancer
- strong family hx of breast/ovarian cancer (eg. Ashkenazi Jewish) - family hx of male breast cancer - young patient (<35 yrs old) - bilateral breast cancer in pts <50 yrs old |
|
|
Discuss frequency of follow-up post breast cancer treatment.
|
- visits should be q3-6mo x 2 yrs and annually thereafter (freq is controversial)
- annual mammography, no other imaging unless clinically indicated - psychosocial support and counselling |
|
|
What is the big risk w/ tamoxifen?
|
inc. risk of endometrial cancer; though, it is used to treat breast cancer.
|
|
|
Discuss management options for breast cancer.
note: for adjuvant/neoadjuvant section, after radiation and hormonal, add chemotherapy to notes |

|
|
|
note
|
There is no survival benefit of mastectomy over lumpectomy plus radiation for stage I and II disease.
|
|
|
T/F. For prostate cancer, screening with psa and dre reduces mortality.
|
False
|
|
|
What are some RFs for prostate cancer?
|
- age
- african american descent - high dietary fat - smoking - FMHx - IBD - adematous polyps |
|
|
What are signs/symptoms of prostate cancer?
|
FUND
frequency urgency nocturia dysuria OBSTRUCTIVE Sx hesitancy straining incomplete emptying intermittency post void dripping weak flow constitutional Sx +/- perineal pain +/- bone pain |
|
|
What is the ddx of a prostate nodule?
|
- prostate cancer (30%)
- bph - prostatitis - prostatic infarct - prostatic calculus - tuberculous prostatitis |
|
|
What are the clinical features of prostate cancer?
|

|
|
|
What are relevant investigations to consider for prostate cancer suspicion?
|
- dre
- psa - trus - transrectal u/s --> size and local staging - trus-guided prostate biopsy - bone scan (can be omitted in untreated CaProstate w/ psa<10ng/ml) - ct scanning to assess mets |
|
|
What are some treatment options for localized prostate cancer?
|
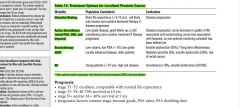
note: these are treatment options for localized prostate cancer. For more advanced cancer, treatment options include:
- chemotherapy - androgen deprivation therapy |
|
|
What are some causes of elevated psa?
|
- prostate cancer
- bph - prostatitis - prostatic ischemia/infarction - prostate biopsy / surgery - urethral catherization - prostatic massage - trus - strenuous exercise - perineal trauma - ejaculation - radiation therapy note: a normal dre does NOT significantly elevate psa |
|
|
What is prostate specific antigen (psa)?
|
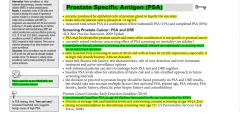
|
|
|
Discuss the benefits and harms of prostate cancer screening with respect to the European Trial and the PLCO trail.
|

|
|
|
With regards to prostate cancer screening, when should one send a pt to a urologist?
|

- abnormal dre
- if any of the psa abnormalities listed below, repeat the psa every 3 to 6 months for referring the patient to the urologist. This will ensure that the psa was really elevated and it's not just a falsely elevated value due to many other factors that may cause an elevated psa (bph, prostatitis, uti, sexual intercourse, urethral instrumentation etc.) - psa >10ng/ml - doubling time within two years - rapid rising velocity >0.75ng/ml per year - consistently elevated PSA demonstrated over 2 to 3 readings in a 1-2 yrs period (refer to cut-off for age and race) note: in a patient on an 5-α reductase inhibitors such as finasteride, their psa is reduced by 50% in 6 months and this is not dose dependent, therefore in these pts one should double their psa value to get their 'true' psa value |
|
|
Discuss monitoring of pts post-treatment for prostate cancer.
|
- the age and race specific psa levels are irrelevant if patient had prostatectomy or radiation therapy.
- if psa is detectable after prostatectomy, refer to specialist immediately. - if psa raises after any treatment (other than prostatectomy), refer to specialist. - if any signs or metastases, refer to specialist. Most common sites of prostate mets are bone, liver, and lung |
|
|
How is the AUA prostate symptom score calculated for benign prostatic hyperplasia (bph)?
|
FUNWISE
frequency urgency nocturia weak stream intermittency straining emptying, incomplete feeling of Each symptom is graded out of 5 0-7 mildly symptomatic 8-19 moderately symptomatic 20-35 severely symptomatic note: dysuria not included in score but is commonly associated w/ bph |
|
|
What are some relevant investigations if you're suspecting bph?
|

|
|
|
Discuss the management of someone who has bph.
|

|
|
|
For bph, how long does it take for the following drugs to take their effect: ?
i. flomax (tamsulosin - α-adrenergic antagonist) ii. proscar (finasteride - 5α reductase inhibitor) |
flomax (tamsulosin)
2-4 wks proscar (finasteride) 4-6 months |
|
|
Describe the three categories of prostatitis.
|
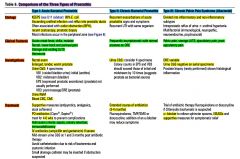
|
|
|
For prostate cancer, there are several treatment options. What are the complications from these treatment options?
|
brachytherapy: erectile dysfunction
radiation therapy: - radiation proctitis - erectile dysfunction (50%) radical prostatectomy: - urinary incontinence (10%) - erectile dysfunction (30%) - urethral stricture - bowel damage - anesthetic complications hormonal treatment (IM LHRH combined w/ anti-androgens) - dec. libido - gynecomastia - osteoporosis |
|
|
Cervical cancer is caused by?
|
hpv infection
|
|
|
Discuss the indications and benefits of the quadrivalent vaccine Gardisil?
|
- currently indicated for women 9-26 yrs for prevention of diseases caused by HPV 6, 11, 16, 18 (genital warts, cervical/vulvur/vaginal dysplasias and cancer)
- for optimal benefit of vaccine, should be given before onset of sexual activity - given IM at 0,2,6 months - not a treatment for active infections - it is still indicated for sexually active women as most women will not be infected with all 4 HPV types simultaneously - conception should be avoided until 30days after last dose of vaccination - side effects: pain, swelling, erythema, low grade fever - contraindications of Gardisil: pregnant women and nursing women |
|
|
The majority of cervical cancers occur in which part of the cervix?
|
transformation zone
|
|
|
What are 2 benign cervical lesions?
What are the 2 main types of cervical cancers? |

1. Squamous cell carcinoma (95%)
2. Adenocarcinoma (5%) |
|
|
note (99 objectives_colon cancer)
|
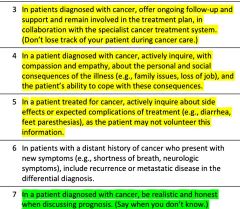
|
|
|
What are some of the clinical features of cervical cancer?
|

|
|
|
Discuss cervical cancer screening with respect to screening initiation, screening interval, and screening cessation.
|
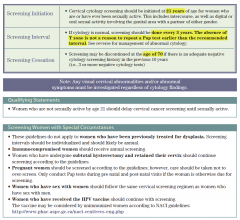
|
|
|
just read
[cervical cancer tests] |
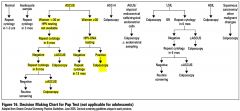
|
|
|
note
|
Any suspicious lesion of the vulva should be biopsied.
|
|
|
What do you do with abnormal paps in pregnancy?
|

|
|
|
What are some RFs of colon cancer?
|

|
|
|
note (99 objectives_cancer)
|
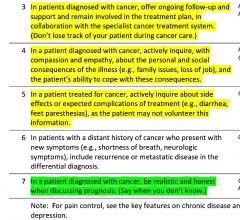
|
|
|
Where does breast cancer metastasize to typically?
|
bone>lungs>liver>brain
|
|
|
What is the ddx for abdominal pain per various locations of the abdomen?
|

|
|
|
A patient presents with acute abdominal pain. What investigations would you consider?
|
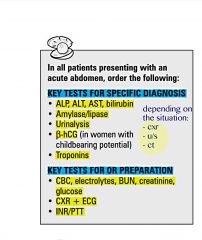
|
|
|
Discuss the location of referred pain for the following conditions
- biliary colic - renal colic - appendicitis - pancreatitis - ruptured aortic aneurysm - perforated ulcer - hip pain |
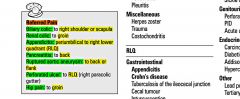
|
|
|
note
|
Pancreatitis can look like a surgical abdomen, but is rarely an indication for laparotomy.
|
|
|
What are some causes of chronic abdominal pain?
|

|
|
|
What are some causes of acute abdominal pain?
|
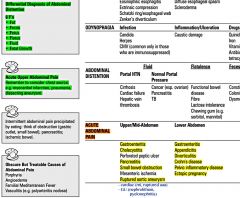
|
|
|
For peptic ulcer disease (pud), what are the:
- causes? - relevant investigations? - basic approach to the management? |
causes:
- h. pylori (most common cause 90% of duodenal and 60% of gastric) - nsaids - physiologic stress-induced - zollinger-ellison (ZE syndrome) ________________________________________________________ investigations: - H. pylori test (urea-breath test, serology) - endoscopy (most accurate) - can also take a biopsy during this procedure - upper GI series (barium swallow) - serum gastrin measurement if ZE syndrome suspected ________________________________________________________ management: i. Stop NSAIDs ii. eradicate H. Pylori iii. Acid neutralization (start PPI, other meds like H2-antagonists are less effective) iv. Quit smoking (inc. risk of ulcer, impairs healing, inc. risk of complications/death) |
|
|
A pt presents with gerd. Which investigations to consider?
|
Trial of PPI. GERD is usually a clinical diagnosis
Investigations - endoscopy (to r/o out conditions that mimic reflux such as cancer, PUD (+/-biopsy for h. pylori), esophagitis) - barium swallow (r/o strictures) - esophageal manometry - 24 hr pH |
|
|
Patients with PUD may present with which complications?
|
- bleeding
- perforation - gastric outlet obstruction |
|
|
GERD - Signs and Symptoms?
|
ESOPHAGEAL
i. Typical - heartburn and acid regurgitation ii. Atypical - chest pain, dysphagia (late), odynophagia (painful swallowing - rare) NON-ESOPHAGEAL i. Respiratory - cough, wheezing, aspiration pneumonia ii. non-respiratory - sore throat, hoarseness, dental erosions |
|
|
What are the complications of gerd?
|
- esophagitis
- Barett's esophagus --> esophageal cancer - strictures |
|
|
What is the most common cause of GERD?
|
- inappropriate transient relaxations of lower esophageal sphincter (LES)
|
|
|
What are the causes of dyspepsia?
|
Dyspepsia also known as upset stomach or indigestion, refers to a condition of impaired digestion.[1] It is a medical condition characterized by chronic or recurrent epigastric pain/discomfort, upper abdominal fullness and feeling full earlier than expected when eating. An organic aetiology is more likely if age >55, associated Sx, or taking medications (especially NSAIDs)
COMMON CAUSES: functional dyspepsia, drug s/e, peptic ulcers, GERD UNCOMMON CAUSES: angina, crown's disease, cancer, gallstones, aerophagia RARE CAUSES: giardia lamblia, malabsorption (celiac disease) |
|
|
T/F. Hiatus hernia worsens reflux, does not cause it
|
True
|
|
|
What are some clinical features of liver disease? (Read only)
|
EFFECTS of LIVER FAILURE:
- encephalopathy (coma), xanthelasma, scleral icterus, jaundice, spider angioma, gynecomastia, muscle wasting, bleeding tendency (bruising), loss of sexual hair/testicular atrophy, ankle edema, palmar erythema, dupuytren's contracture, asterixis, leuconychia, Terry's nails, clubbing EFFECTS of PORTAL HTN: - esophageal varices - splenomegaly - caput medusa, umbilical hernia - ascites - hemorrhoids |
|
|
What are the 3 top causes of small bowel obstruction?
|
ABC
Adhesions Bulge (hernias) Cancer |
|
|
note
|
In a woman with abdominal pain:
- always r/o pregnancy if she is of reproductive age - suspect gynecologic aetiology for abdominal pain - do a pelvic examination, if appropriate |
|
|
just read (common presentations of surgical abdominal pain).
|

|
|
|
What are some causes of acute abdominal pain in children?
|
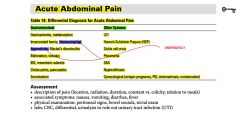
|
|
|
What are the classic features of intussusception?
How is the diagnosis made and what is the treatment? |

|
|
|
What are the causes of aaa?
What are the RFs for aaa? |
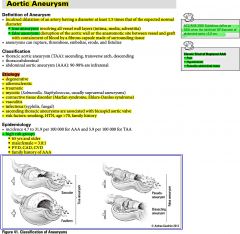
|
|
|
What are the guidelines of screening aaa and f/u? [just read]
|

|
|
|
What are the indications for surgical repair of an aaa?
|
- rupture
- symptomatic aneurysms > 5.5 cm - symptomatic aneurysms with rapid rate of expansion (> 0.5 cm/6 months) - aneurysms twice the size of the non-aneurysmal aorta |
|
|
note
|
Given a pt with established diabetes, advise about signs and treatment of hypoglycemia/hyperglycemia during an acute illness or stress (i.e. gastroenteritis, physiological stress, decreased intake)
|
|
|
Discuss the differences between DKA and HHS (hyperosmolar hyperglycaemia state).
|

|
|
|
Discuss some of the precipitants of dka.
|
[the 6 Is of dka]
- Infection - ischemia / Infarction - iatrogenic (glucocorticoids) - Intoxication - insulin missed - intra-abdominal process (eg. pancreatitis, cholecystitis) Can occur with lack of insulin (non-adherance, inadequate dosage, 1st presentation) or increased stress (surgery, infection, exercise). |
|
|
Discuss whats involved in diabetes assessment and monitoring.
|
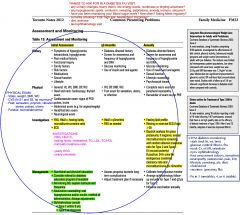
|
|
|
just read
|
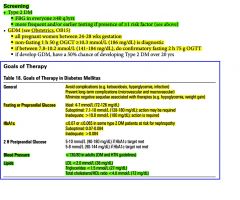
note: 2hr post prandial glucose target is 5-10M
|
|
|
Explain the different insulin regimens?
|

|
|
|
Describe the different insulin formulations
|
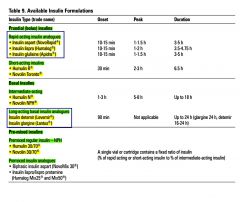
|
|
|
note
|
hyperosmolar hyperglycemic state (hhs) aka hyperosmolar non-kerototic state (honk)
|
|
|
What is frozen shoulder (adhesive capsulitis)?
- What is the mechanism? - What are the clinical features - What are relevant investigations? - What is the management? |
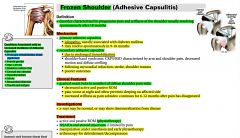
|
|
|
What is fibromyalgia?
|
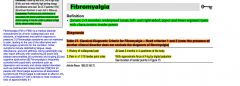
|
|
|
What is polymyalgia rheumatica (pmr)?
What is the criteria for diagnosis? signs / symptoms? What investigations would you do? Management? |
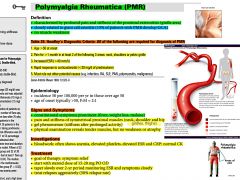
|
|
|
note
|
If a chronic pain patient is having paresthesias that may / may not be related to the pain site, it is worthwhile to check the Ca levels, and Vitamin B12 levels
|
|
|
What are some investigations that can be used to diagnose H. pylori?
|
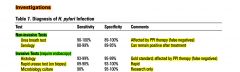
|
|
|
A patient comes in with symptoms typical of dyspepsia (early satiety, bloating, epigastric discomfort typically after a meal).
What investigations would you do? What are your treatment options? |
INVESTIGATIONS:
- BW - CBC, lytes, LFTs, amylase, bilirubin - non-invasive H. pylori testing (serology) ----------------------------------------------------------------------------- MEDICATION: - trial of PPI or H2 antagonist Prescription: pariet ec/nexium/tecta x 1 mo; if after 1 mo symptoms come back will consider ppi for long term - In the presence of any red flags (i.e. weight loss, dyshagia, persistent vomiting, 1st onset age >50, fatigue/anemia, palpable abdominal mass) --> consider GI referral (Dr. Bisonette (GI)) for a consult + endoscope |
|
|
What is gastritis?
- causes? - symptoms? - management? |
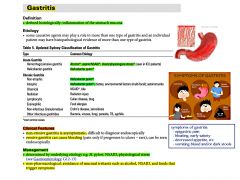
|
|
|
What is plantar fasciitis (heel spur syndrome)?
What are the symptoms/signs? What is the management? |
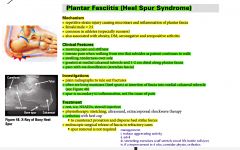
|
|
|
In children, what are the RED FLAGS for organic aetiology of chronic abdominal pain?
[pediatrics] |
- age < 5 yrs old
- fever - localizes pain away from midline - anemia - rectal bleeding - rash - pain awakens child at night - travel history - prominent vomiting, diarrhea - wt loss or failure to gain wt - joint pain |
|
|
What is the most common cause of seizures in children?
|
Fever (febrile seizures)
Febrile seizures occur from 6 mo - 6 yrs of age |
|
|
What is a febrile seizure?
|
A febrile seizure, also known as a fever fit or febrile convulsion, is a convulsion associated with a significant rise in body temperature. They most commonly occur in children between the ages of 6 months to 6 years.
The direct cause of a febrile seizure is not known; however, it is normally precipitated by a recent upper respiratory infection or gastroenteritis. The diagnosis is one that must be arrived at by eliminating more serious causes of seizure and fever: in particular, meningitis and encephalitis must be considered. However, in locales in which children are immunized for pneumococcal and Haemophilus influenzae, the prevalence of bacterial meningitis is low. If a child has recovered and is acting normally, bacterial meningitis is very unlikely. |
|
|
Differentiate between Simple/Benign febrile seizures and Complex/Atypical febrile seizures?
|

|
|
|
What are the causes of chronic abdominal pain in children?
|
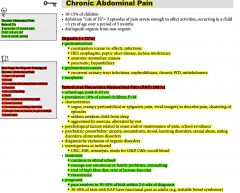
|
|
|
What investigations would you do in a child presenting with seizures?
|
- CBC, lytes, Ca, Mg, PO4
- Cr, BUN - glucose - tox screen - EEG, CT and LP if indicated note: If simple febrile seizure, then investigations only to determine the cause of the fever. |
|
|
What is the management of a child with febrile seizures?
|
- counsel and reassure patient and parents (febrile seizures do not cause brain damage, v. small risk of developing epilepsy)
- antipyretics (tylenol) and fluids (neither prevent seizures) - prophylaxis not recommended - if high risk of recurrent or prolonged seizures, have sublingual or rectal lorazepam (Ativan) at home. - treat underlying cause of fever (eg. otitis media) |
|
|
What sort of workup would you do in a child who presents with febrile seizures. What would be the management of this patient?
|

|
|
|
T/F. Term infant should gain 20-30g/day
|
True
|
|
|
Explain the management of fever in the pediatric population for <1 month, 1-3 months, and 3 months - 3 years
|
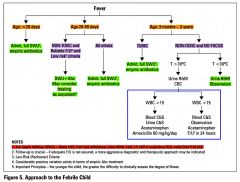
|
|
|
How would a toxic looking child present?
|
Toxic-appearing infants and children are:
- pale or cyanotic - lethargic - inconsolably irritable - In addition, they may have tachypnea and tachycardia with poor capillary refill. |
|
|
What does a full septic workup include:
|
FSWU:
- CBC + diff - blood C + S - urine C + S - LP CXR if respiratory Sx Stool C + S if GI Sx |
|
|
Discuss the classification of fever of unknown origin (fuo).
|

|
|
|
Discuss the causes of classic fever of unknown origin (fuo).
|

|
|
|
Discuss the approach to investigations in fever of unknown origin (fuo).
|

|
|
|
What are some physical findings in infective endocarditis?
[fever] |
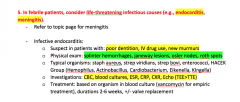
|
|
|
note
|
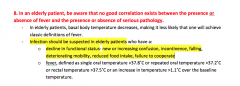
|
|
|
In a febrile pt, what are some other causes of hyperthermia other than infection?
|
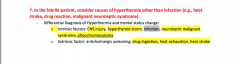
|
|
|
note
|
progressively worse:
systemic inflammatory response syndrome (SIRS) --> Sepsis --> Severe sepsis --> Septic shock --> MODS (multiple organ dysfunction syndrome) |
|
|
Discuss the definitions of: SIRS, sepsis, severe sepsis, septic shock.
What are the clinical features of septic shock? What is the management for septic shock? |
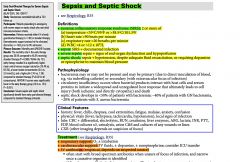
|
|
|
What is febrile neutropenia?
What is the most common organism involved Briefly discuss investigations and management? |

|
|
|
note
|
Aggressively and immediately treat pts who have fever resulting from serious causes before confirming diagnosis, whether these are infectious (eg. febrile neutropenia, septic shock, meningitis) or non-infectious (eg. heat stroke, neuroleptic malignant sydrome, drug reaction)
|
|
|
List some drugs commonly associated with drug-induced fever.
|
- penicillin, erythromycin (antibiotics)
- HCTz, methyldopa (anti-hypertensive) - allopurinol - heparin |
|
|
note
|
In a pt with multiple injuries, it is essential to first stabilize the pt (ABCs and life threatening injuries) before dealing with any fractures.
|
|
|
T/F. In a traumatic neck injury, one must always use the canadian c spine rules.
What are the canadian c spine rules? |
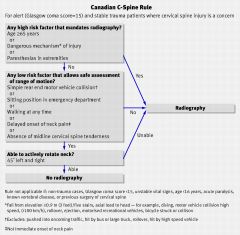
True
|
|
|
What is the ddx for neck pain?
|
- degenerative: OA, ddd (most common)
- myelopathy (spinal cord compression), radiculopathy (nerve root compression) - trauma - rheumatologic: pmr, gca, fibromyalgia - infection: meningitis, pharyngeal abscess, other infectious causes of lad - neoplastic: due to lad, bony mets, neuro compression - cvs: referred from MI, angina - msk: referred from shoulder pain, cervical muscular pain - vascular: vertebral or carotid artery dissection |
|
|
What would you do on physical exam in someone who presents with neck pain?
|
- masem
- palpation - neck rom +/- cn exam - u/e: sensation, motor, and reflexes (incl. shoulders) |
|
|
What are some possible investigations one can do with regards to neck pain?
|
- xray: c spine
- ct: c spine (better for facet oa, other bony changes - mri: c spine (better for disc herniations, foramen stenosis, tumour) - emg (suspected radiculopathy, esp. if Sx more prominent in u/e |
|
|
T/F. The risk of developing neuroleptic malignant syndrome is higher with typical antipsychotics versus atypical antipsychotics.
|
True
|
|
|
T/F. pseudotumour cerebri may present with neck pain.
|
Yes.
Idiopathic intracranial hypertension or pseudotumor cerebri (PTC), is a neurological disorder that is characterized by increased intracranial pressure (pressure around the brain) in the absence of a tumor or other diseases. The main symptoms are headache, nausea, and vomiting, as well as pulsatile tinnitus (sounds perceived in the ears, with the sound occurring in the same rhythm as the pulse), double vision and other visual symptoms. The pain may be felt in the neck and shoulders as well. If untreated, it may lead to swelling of the optic disc in the eye, which can progress to vision loss. IIH is diagnosed with a brain scan (to rule out other causes) and a lumbar puncture; lumbar puncture may also provide temporary and sometimes permanent relief from the symptoms. Some respond to medication (with the drug acetazolamide), but others require surgery to relieve the pressure. The condition may occur in all age groups, but is most common in young women, especially those with obesity. The most common symptom of IIH is headache, which occurs in almost all (92–94%) cases. It is characteristically worse in the morning, generalized in character and throbbing in nature. It may be associated with nausea and vomiting. The headache can be made worse by any activity that further increases the intracranial pressure, such as coughing and sneezing. |
|
|
How would you treat neck pain that is more msk / degenerative in nature?
|
- ice / heat
- tylenol / advil - physiotherapy, chirotherapy, massage therapy, accupuncture - +/- referal to neurologist |
|
|
When viewing a c spine xray, which 3 views would you want to observe?
|
i. lateral view
ii. anterioposterior view iii. open mouth odontoid view It is important to carefully observe each vertebrae and make sure that they are aligned (4 lines of alignment) |
|
|
What are the indications for open reduction?
[fractures] |
NO CAST
Non-union Open fracture C - neurovascular compromise A - intra - Articular fracture S - Salter-Harris 3,4,5 T - polytrauma |
|
|
What are the signs of basal skull fractures?
|
1. Battle's sign (bruised mastoid process)
2. Racoon eyes (periorbital bruising) 3. Hemotympanum 4. CSF Rhinorrhea/Otorrhea |
|
|
What are some early local and systemic fracture complications?
What are some late complications? |
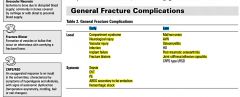
|
|
|
Discuss the management of fractures.
|

|
|
|
What is compartment syndrome?
What are the ‘Ps’ of compartment syndrome? What is the management? |

|
|
|
What are the 6Ps of vascular compromise?
[fracture] |
- pain
- pallor - polar - paresthesias - paralysis - pulselessness |
|
|
note
|
Crush injuries increase the risk of developing:
i. compartment syndrome ii. rhabdomyelolysis. |
|
|
note
|

|
|
|
What is a scaphoid fracture?
What are the clinical features? What investigations would you do? What is the treatment? |
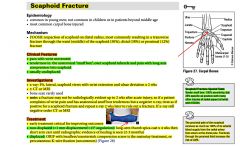
|
|
|
What is a colles’ fracture?
What is the mechanism of injury What are relevant investigations? What is the management? |
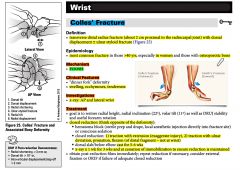
|
|
|
What is a smith’s fracture?
What is the mechanism of injury What is the management? |

|
|
|
just read
|
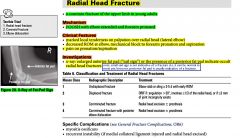
|
|
|
Discuss the salter-harris classification of fractures.
|
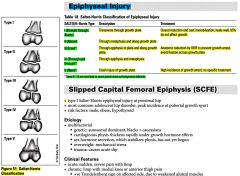
|
|
|
note (99 objectives_fractures)
|

|
|
|
note
|

|
|
|
Discuss the physical exam for a pt who presents with a fracture?
|
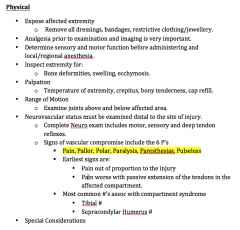
|
|
|
note
|
Ottawa Foot and Ankle rules only apply for ankle inversion injuries.
|
|
|
What is Osgood-Schlatter Disease?
What is the mechanism for this injury? What are the clinical features? What is the management? |

|
|
|
What is the difference between a greenstick fracture and a buckle (torus) fracture?
|

|
|
|
Discuss the different types of fracture patterns (diagrammatically).
|

|
|
|
Discuss the indications for doing bone mineral density testing. Note these indications are also risk factors for osteoporosis.
|
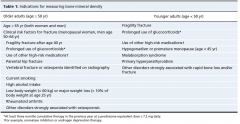
|
|
|
What is the management of osteoporosis?
|

|
|
|
Discuss the integrated management model for diagnosing and managing osteoporosis.
|
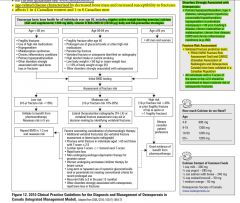
|
|
|
note:
|
Corticosteroid therapy is the 2nd most common cause of osteoporosis.
|
|
|
What is osteoporosis. Discuss the use of T scores in the diagnosis of osteopenia and osteoporosis.
|
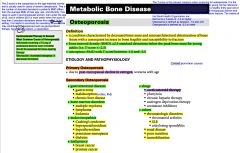
|
|
|
What are some physical signs of # / osteoporosis?
|
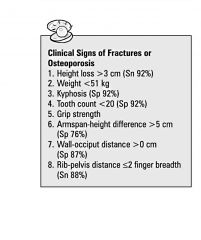
|
|
|
Diagrammatically discuss the wall-occiput test for thoracic fracture and rib-pelvis test for lumbar fracture.
|
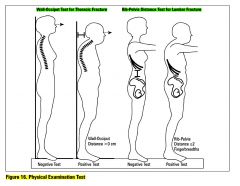
|
|
|
What are the recommended biochemical tests for pts being assessed for osteoporosis?
|
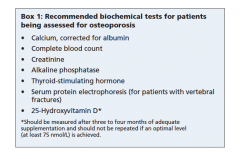
note: serum protein electrophoresis is to check for possible multiple myeloma.
apart from the biochemical tests, one can also order xray_thoracic, lumbar if suspicious of a vertebral fracture (midline tenderness); another test is bmd |
|
|
Name one online clinical assessment tool for assessing risk for osteoporotic fractures.
|
- FRAX (WHO fracture risk assessment tool)
- CAROC (canadian assoc. of radiologists and osteoporosis Canada) |
|
|
What is a fragility fracture?
|
fracture that occurs spontaneously or following a minor trauma, such as a fall from a standing height
|
|
|
note
|
In osteoporosis pts, it is important to avoid prescribing meds that may increase the risk of falls.
That is: caution must be applied with benzos, TCAs, antihypertensives, anti-anginal meds |
|
|
What is the epidemiology of osteoporosis?
|
osteoporosis:
- affects 1 in 8 older men - affects 1 in 4 older women - 13% men and 25% women have osteoporosis (canada) |
|
|
List some adverse effects of bisphosphonates.
|
- esophagitis
- GI symptoms - renal toxcity - arthralgias - flu like symptoms - uveitis - osteonecrosis of the jaw |
|
|
What is the indications for using calcitonin?
|
combination of back pain and compression fracture (osteoporosis)
|
|
|
What would be the presentation of a urinary tract infection (UTI) in an infant?
How is the urine sample collected for urine testing (i.e. dipstick, cultures) [suprapubic, catheterization] |
|
|
|
Depression may present differently in children and adolescents. What are some symptoms these groups may show when faced with depression?
|
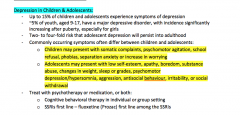
|
|
|
How might pneumonia present in children and youth?
|
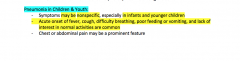
|
|
|
What is the ‘HEADSS’ assessment in adolescents?
|
- home
- education - activities - drugs - sexuality - suicide + mental health |
|
|
note (99 objectives_in children)
|

|
|
|
What are some preventative measures and risk factor reduction to address with a child (and / or parent) when they come in for the well child check?
|

|
|
|
In blunt chest trauma, if xray shows widened mediastinum, what is the most significant thing one should be suspicious for?
|
traumatic rupture of the aorta
|
|
|
Which investigation is most commonly used for diagnosis of a traumatic aortic rupture?
|
CT angiography
Although the gold standard is aortogram, this is difficult to do due to access and time availability |
|
|
In trauma, ‘disability' (of ABCDE) is measure either by the AVPU method or GCS. Discuss the classification of the GCS (glasgow coma scale).
|

|
|
|
Discuss the approach to trauma (including primary and secondary surveys, relevant investigations).
|
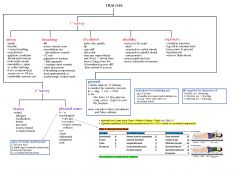
|
|
|
What are the different categories of shock?
Discuss the classification of hemorrhagic shock. |

|
|
|
note (99 objectives_trauma)
|
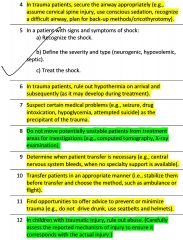
|
|
|
In trauma, what do the following terms mean:
- FAST - DPL |
FAST = focused assessment sonography in trauma
DPL = diagnostic peritoneal lavage note: Focused assessment with sonography for trauma (commonly abbreviated as FAST) is a rapid bedside ultrasound examination performed by radiologists, surgeons, emergency physicians and certain paramedics as a screening test for blood around the heart (pericardial effusion) or abdominal organs (hemoperitoneum) after trauma. |
|
|
note:
|
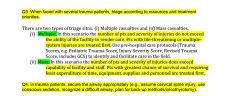
|
|
|
note:
[trauma, tension pneumothorax, needle thoracocentesis, chest tube] |

|
|
|
What is PCOS and what are the clinical features?
What is the diagnostic criteria? What are relevant investigations in a patient with PCOS? |
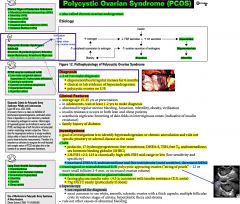
|
|
|
What are the long term health consequences of pcos?
|
- hyperlipidemia
- obesity - sleep apnea - DM - infertility - endometrial hyperplasia |
|
|
What is the management for PCOS?
|

|
|
|
What are some RFs for erectile dysfunction?
|
- dm
- htn - hyperlipidemia - smoking - advancing age - pelvic irradiation/surgery (inc. radical prostatectomy) - medications (antihypertensives like b-blockers and ccbs, psychotropics) - psychiatric illness: depression, anxiety, stress, marital conflicts) |
|
|
What is erectile dysfunction and what is the etiology?
Differentiate between organic and psychogenic erectile dysfunction? Discuss some of the questions to ask pts on history? |
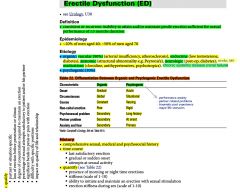
|
|
|
What is gender identity?
|
Individual’s innate sense of being male, female, or somewhere in between.
|
|
|
What is sexual orientation?
|
Individual’s pattern of physical and emotional arousal towards others; commonly dichotomized into heterosexual and homosexual.
|
|
|
note (99 objectives_sex)
|
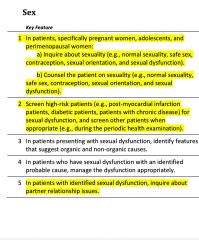
|
|
|
What are some male factors for infertility?
|

|
|
|
What are some female factors for infertility?
|

|
|
|
What are some investigations relevant to female infertility?
What is the management of infertility (related to females)? |
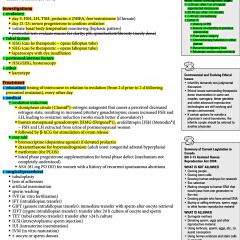
|
|
|
What is endometriosis?
|
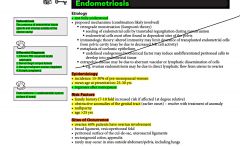
|
|
|
What is the classic triad in endometriosis?
|
i. dysmenorrhea
ii. dyspareunia iii. dyschezia (constipation) also assoc with infertility * vaginal bleeding - not typically abnormal in endometriosis |
|
|
What are the clinical features of endometriosis?
What are relevant investigations to do for a pt that presents with the symptoms of endometriosis? |
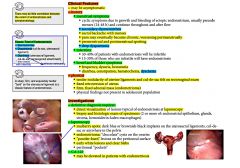
|
|
|
What are some female RFs for infertility?
What are some male RFs for infertility? |
female:
- age >35 (females) - history of STI / pelvic inflammatory disease - very high body fat - very low body fat - smoker - substance abuse male: - varicocele - cryptochidism - prior chemo or radiation - cystic fibrosis - klinefelter’s syndrome - retrograde ejaculion - history of STIs |
|
|
A female pt comes in to your office complaining of not getting pregnant for the last 2 years despite trying. You’ve taken a good sexual / gynaecological hx and have a set of investigations lined up. What are some things to look for on physical exam?
|
- bmi
- hirsuitism - acne - (acanthosis nigricans) - galactorrhea - pelvic exam |
|
|
note
|
Generally,
- 75% of couples achieve pregnancy in 6 months, - 85% within 1 yr - 90% within 2 years |
|
|
When should one begin doing investigations for infertility?
|

|
|
|
What is the difference between primary infertility and secondary infertility?
|
primary infertility:
infertility in the context of no prior pregnancy secondary infertility: infertility in the context of prior pregnancy |
|
|
What are some relevant investigations to do for male infertility?
What is considered a normal semen analysis? What would be the management of male causes of infertility? |

|
|
|
note (99 objectives_infertility)
|

|
|
|
What are the symptoms of a prolactinoma?
|
- galactorrhea
- visual changes - headaches |
|
|
Differentiate thought process from thought content?
|
- Thought process (coherent/incoherent, logical/illogical, circumstantial, tangential, flight of ideas)
- Thought content - (SI/HI, preoccupations, ruminations, overvalued ideas) |
|
|
What does the Mental Status Exam comprise of?
|
- Appearance + Behavior
- Speech - Mood - subjective emotional state - Affect - objective emotional state - Thought process (coherent/incoherent, logical/illogical, circumstantial, tangential, flight of ideas) - Thought content - (SI/HI, preoccupations, ruminations, overvalued ideas) - Perception (hallucination, delusion, depersonalization) - Cognition (level of consciousness, orientation to person, place, time; memory) - Insight (understand their degree of illness) - Judgement (Understands if their condition gets worse, they are to come back to the hospital |
|
|
Differentiate between different types of delusions: Persecutory, delusions of reference, erotomania, grandiose, religious, somatic, nihilistic
|
- Persecutory: belief that someone wants to harm you
- Reference: Message from the TV/celebrity intended for you - Erotomania - belief that someone is in love with you - Grandiose - belief of inflated self of self worth - Religious - belief of receiving instructions from a higher power - Somatic - belief that one has a physical disorder/defect - Nihilistic - belief that things do not exist; a sense that everything is unreal |
|
|
What are the 5 axes in Psychiatry?
|
Axis I: ddx of DSM psych clinical disorders
Axis II: Personality disorders, developmental delay Axis III: GMCs that are potentially relevant to the understanding or management of the mental disorder Axis IV: psychosocial and environmental issues Axis V: global assessment and functioning (GAF 0-100; 100= superior functioning, 0 is inadequate info; 1-10 persistent danger of severely hurting self or others) |
|
|
What is formication?
|
- tactile hallucination that insects or snakes are crawling over or under the skin. Especially associated with crystal meth use.
|
|
|
What is the difference between malingering and factitious disorder?
|
MALINGERING
- intentional production of false or grossly exaggerated physical or psychological symptoms motivated by external reward (e.g. avoiding work, obtaining financial compensation, or obtaining drugs) FACTITIOUS DISORDER - intentional production of feigning of physical or psychological signs of Sx in order to assume the sick role where external incentives (e.g. economic gain) are absent Unlike Somatoform disorders, these 2 are under conscious control |
|
|
What is nocturnal myoclonus?
|
- occurs in the middle-aged and elderly
- myoclonic jerks q20-40 seconds - bed partner complains TREATMENT: Benzos (clonazepam, nitrazepam) |
|
|
What is sexual orientation?
|
- the degree of a person's erotic attraction to people of the same sex, the opposite sex, or both sexes
- homosexuality - heterosexuality - bisexual |
|
|
What do pervasive developmental disorders comprise of?
|
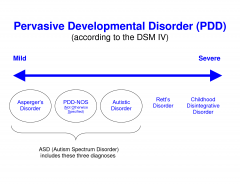
i. Autism
ii. Asperger's iii. childhood disintegrative disorder iv. Rett's disorder v. PDD NOS |
|
|
What is autism?
|
Autism is a disorder of neural development characterized by abnormalities in 3 areas:
1. Social interaction i. impaired non-verbal behaviours like eye contact, facial expression, hand gestures ii. failure to develop appropriate peer relationships iii. lack of social/emotional reciprocity 2. Communication i. delayed or absent speech or marked impairment to initiate or sustain a conversation ii. stereotyped/repetitive or idiosyncratic use of language iii. absence of appropriate make-believe play 3. Restricted and repetitive behaviours, interests, and activities i. inflexible adherence to specific non-functional routines eg. rocking At least 6 features before 3 years old (at least 2 from social interaction and 1 from the other two categories) |
|
|
What is Asperger syndrome/disorder?
|
Asperger syndrome, also known as Asperger's syndrome or Asperger disorder, is an autism spectrum disorder (ASD) that is characterized by significant difficulties in social interaction, alongside restricted and repetitive patterns of behavior and interests. It differs from other autism spectrum disorders by its relative preservation of linguistic and cognitive development. Although not required for diagnosis, physical clumsiness and atypical use of language are frequently reported.
NOTE: in Asperger's there is impaired social interaction and restricted repetitive patterns of behaviours or interests; HOWEVER no delay in language or cognitive development. Autism is worse than Asperger's in the spectrum of PDDs |
|
|
What is the difference between transference and countertransference?
|
In a therapy context, transference refers to redirection of a patient's feelings for a significant person to the therapist. Transference is often manifested as an erotic attraction towards a therapist, but can be seen in many other forms such as rage, hatred, mistrust, parentification, extreme dependence, or even placing the therapist in a god-like or guru status. The focus in psychodynamic psychotherapy is, in large part, the therapist and patient recognizing the transference relationship and exploring the relationship's meaning. Since the transference between patient and therapist happens on an unconscious level, psychodynamic therapists who are largely concerned with a patient's unconscious material use the transference to reveal unresolved conflicts patients have with childhood figures.
Countertransference is defined as redirection of a therapist's feelings toward a patient, or more generally, as a therapist's emotional entanglement with a patient. |
|
|
What is the difference between a tia and a stroke?
|
transient ischemic attack (tia):
sudden onset of neurological deficits of a vascular basis without infarction (prev. definition of tia was based on time duration of <24h; this has been changed as it was quite arbitrary) stroke: sudden onset of neurological deficits of a vascular basis with infarction of cns tissue; infarction is permanent tissue injury (confirmed by neuroimaging) |
|
|
What investigations would you do in someone who presents with symptoms of a tia/stroke?
|

|
|
|
What is the ddx for stroke?
|
- tia
- seizure / post-ictal - hypoglycemia - migraine - brain tumour - subdural hematoma - subarachnoid hemorrhage - encephalitis - sepsis - conversion disorder |
|
|
Discuss primary prevention for tia/stroke.
|
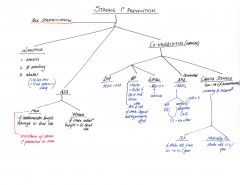
|
|
|
Discuss acute management of stroke.
|
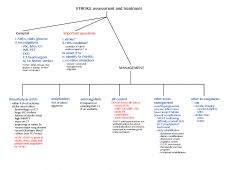
|
|
|
Discuss management of tia.
|

|
|
|
Discuss secondary prevention for tia/stroke.
|
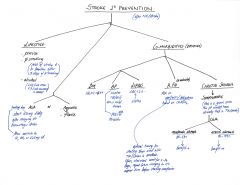
|
|
|
Discuss the abcd risk prediction tool of developing a stroke from a tia.
|

|
|
|
What are some RFs for tia/stroke?
|
- sedentary lifestyle
- smoking - alcohol (excessive) - htn - lipids_elevated - dm - atrial fibrillation - carotid stenosis - estrogen based therapy - tia (for stroke) |
|
|
What is the etiology of epistaxis (nose bleeds)?
|

|
|
|
What would you do on physical exam for someone who presents with epistaxis?
|
- vitals
- fluid status assessment - inspection: nasal flares - observe for masses, polyps, mucosa (dry), perforation, deviation - heent: for Sx of urti - general inspection for pallor - general inspection for bruising |
|
|
For epistaxis what investigations would you do/consider?
|
- bw: cbc, inr, ferritin
- lfts, type and cross, group and screen |
|
|
Discuss management of epistaxis.
|

|
|
|
List 3 situations where one should not delay antibiotic treatment.
|
- meningitis
- sepsis / septic shock - febrile neutropenia |
|
|
Discuss the approach (with respect to children 0-6months, 6mo-2yrs, >2yrs) of prescribing antibiotics in a child with suspicion of acute otitis media (aom).
|

|
|
|
note (99 objectives_infections)
|

|
|
|
note (99 objectives_antibiotics)
|
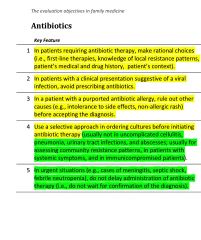
|
|
|
With respect to antibiotics, discuss the various cell wall inhibitors.
|

|
|
|
With respect to antibiotics, discuss the various protein synthesis inhibitors and topoisomerase inhibitors.
|

|
|
|
With respect to antibiotics, discuss the various anti-metabolites and anti-microbials.
|
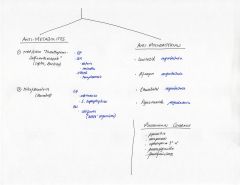
|
|
|
Discuss the classification of common bacteria.
|
|
|
|
What are the 4 main Parkinsonian features? What are some other parkinsonian findings?
|
TRAP
- tremor (resting, 4-5Hz pill rolling; usually unilateral, asymmetrical) - rigidity (lead-pipe, cogwheel) - akinesia/bradykinesia - postural instability other findings include: - shuffling gait w/ dec. arm swing - freezing - stooped posture - slow to think / respond - micrographia - masked facies - dysarthria - hypophonia - personality changes, depression, anxiety, sleep disturbances - constipation, urinary retention, sexual dysfunction (late findings) |
|
|
What is the diagnostic criteria for parkinson's disease (PD)?
|

|
|
|
What are the signs and symptoms of Parkinson's disease?
|
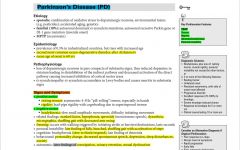
|
|
|
What are the feature's of atypical Parkinson's disease?
What is the ddx for Parkinson's disease? |
- early age of onset <50yrs
- early cognitive impairment - abrupt onset of symptoms - rapid progressions - early falls - symmetric symptoms at onset - poor response to L-dopa - s/e of typical antipsychotics (eps symptoms) - FHx of psychiatric/dementing disorders - recent diagnosis of psychiatric disease - hx of encephalitis - unusual toxic exposure -------------------------------------------- DDx: - dementia w/ lewy bodies - multiple system atrophy - corticobasal degeneration - normal pressure hydrocephalus - essential tremor - tremor from hyperthyroidism or b-agonists - cerebellar disorder |
|
|
What is the triad of symptoms in normal pressure hydrocephalus?
|
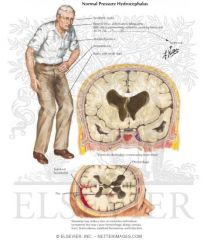
- confusion
- urinary incontinence - gait instability |
|
|
note
|
In a pt w/ parkinson's disease, it is important to check their functional status. i.e. their ADLs and iADLs
|
|
|
What test can one do for assessing gait instability in Parkinson's disease?
|
|
|
|
What investigations do you do in someone who has the symptoms typical of Parkinson's disease?
|
Investigations are done only if there are features of an alternative diagnosis. eg.
ct/mri head is done if suspecting: - brain lesion - neurodegenerative disorder or nph - stroke tsh (tremor of hyperthyroidism or general slowing of hypothyroidism) |
|
|
As part of a Parkinson's disease management, it is best to involve other health care professionals to enhance the pt's functional status. Which health care professionals might you consult?
|
i. physiotherapy: improve speed, initiation, balance, reduce risk of falls
ii. OT: improve home safety iii. slp: speech and decrease risk of aspiration iv. +/- geriatrician: optimizing medications as needed v. +/- dietician: no specific diet influences the course of parkinson's disease, but a high fiber diet and adequate hydration can help reduce constipation. Also some of these pts may have difficulty swallowing, so they may need liquid food rather than solids. |
|
|
In a pt w/ Parkinson's disease, why must anti-parkinson's medications never be abruptly stopped?
|
due to the risk of neuroleptic malignant syndrome (nms)
|
|
|
What is the medical management for Parkinson's disease?
|

|
|
|
What is epiglottitis?
|
Epiglottitis is an inflammation of the epiglottis — the flap at the base of the tongue that keeps food from going into the trachea (windpipe). Due to its place in the airway, swelling of this structure can interfere with breathing, and constitutes a medical emergency. Infection can cause the epiglottis to obstruct or completely close off the windpipe. With the advent of the Hib vaccine, the incidence of epiglottitis has decreased, but the condition has not been eliminated.
Its a rare condition that occurs in children typically 2-6 yrs of age. Causative agents include: H. influenza and beta-hemolytic Streptococcus. Children present as: Toxic looking, rapid progression, severe airway obstruction, drooling, stridor, tripod position, sternal recession, ANXIOUS. Diagnosis is usually clinical. One should avoid examining the throat to prevent further exacerbation; also may require intubation and Abx; prevented by Hib vaccine |
|
|
What is bacterial tracheitis? What are the causative agents?
|
Tracheitis is an inflammation of the trachea. Bacterial tracheitis is a bacterial infection of the trachea and is capable of producing airway obstruction.
One of the most common causes is s. aureus and often follows a recent viral upper respiratory infection. It is the most serious in young children, possibly because of the relatively small size of the trachea that gets easily blocked by swelling. The most frequent sign is the rapid development of stridor. It is occasionally confused with croup. Similar symptoms as croup, but more rapid deterioration, high fever, toxic appearance, DOES NOT respond to croup treatments. Diagnosis is clinical but definitive diagnosis can be made by endoscopy. Other causative agents include: H. influenza, streptococcus, pneumococcus. MANAGEMENT: start therapy for croup, usually required intubation and antibiotics |
|
|
note
|
Pulling on the pinna may be extremely painful in otitis externa, but is usually tolerated in pts with otitis media. This may be helpful in differentiating otitis externa from otitis media, unless both conditions exist.
|
|
|
What is otitis externa?
What are some RFs? What are the clinical features? What is the management? |
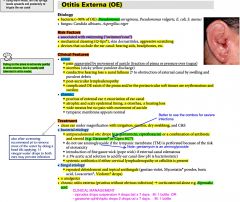
|
|
|
note (99 objectives_urti)
|

|
|
|
just read
|
COMPARISON OF VIRAL VS. BACTERIAL URTI
i. bacterial infections are associated with moderate to high fevers (typically >38.5C), whereas viral infections may be associated with low grade fevers ii. more common to have rhinorrhea, sneezing, sore throat with viral infections compared to bacterial infections. iii. hoarseness is typically of viral etiology iv. H/A and chills are more severe in bacterial causes of urti v. cough tends to be more productive in bacterial infections |
|
|
note
|
- influenza vaccine is recommended annually for everyone.
- Tami-flu is an anti-viral that has very little evidence of benefit in treating influenza A + B. Must be taken <48hrs of symptoms, otherwise no benefit. Some evidence of reduction of symptoms by 24 hours. |
|
|
What are the clinical features of peptic ulcer disease?
|
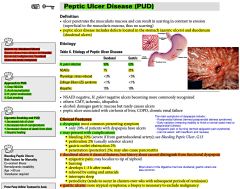
|
|
|
What is rosacea? What are the different types
- what is the clinical presentation? |

|
|
|
What is the management of rosacea?
|

|
|
|
A 67M comes in for a general assessment. You update the ccc, bmd, prostate, bw. He’s had a tetanus shot 4 years ago. Is there any other vaccine(s) to discuss with him?
|
- flu shot (depending on the time of the year)
- pneumovax (pneumococcal 23-valent) - zostavax (shingles vaccine) note: pneumovax should be given in all pts >65 and it is covered under ohip |
|
|
A pt presents with epistaxis. You've taken care of the ABCs; the pt is stable. How would you determine the site of bleeding and control the bleeding? (note you've already done the lean forward and apply firm pressure technique)
|
determine site of bleeding:
- insert cotton pledget (w/ 4% lidocaine) ± topical decongestant (otrivin) - use speculum to visualize nasal cavity and aspirate excess blood and clots control site of bleeding: - 1st line: topical vasoconstrictor (otrivin) - if this fails and bleeding site visible: silver nitrate (do not cauterize both sides of septum (perforation risk)) i. anterior hemorrhage treatment: - gauze strips 1/2 inch (soaked w/ vaseline) or - absorbable packing (gelfoam) or - merocel / nasal tampons or - floseal ii. posterior hemorrhage treatment: - foley catheter or - gauze pack or - epistat balloon * if anterior/posterior packs fail to control epistaxis: - arterial ligation - elective embolization - ± septoplasty |
|
|
Write a prescription for treatment of vulvar lichen sclerosis.
|
dermovate 0.05% ointment
apply to affected area qhs M: 30g repeats: 4 [treat qhs for 6wks]; then twice weekly for maintenance note: ointment should be used instead of cream as cream may contain irritants not present in the ointment |
|
|
Colles fracture (diagram)
|

|
|
|
note
|
It is important to warn parents of infants getting the rotateq vaccine that they may have loose stools for up to 2 wks; as long as they don't have a fever, bloody stools, or look unwell no need to bring them in
|
|
|
note
|
Adults should get one adacel (Tdap) booster, if not received in the past. After this they can keep getting the tetanus shots.
|
|
|
List some maternal complications of abruptio placenta.
|
- dic (20% of abruptions)
- amniotic fluid embolus - hemorrhagic shock - pituitary necrosis (Sheehan syndrome) - acute renal failure |
|
|
What is Neuroleptic malignant syndrome (NMS)?
Presentation? What is the management? |
Neuroleptic malignant syndrome (NMS) is a life-threatening neurological disorder most often caused by an adverse reaction to neuroleptic or antipsychotic drugs. It is a psychiatric EMERGENCY.
Presentation of NMS includes (FARM): - Fever - Autonomic changes (inc. HR/BP, sweating) - Rigidity (muscle) - Mental status change (e.g. confusion) These symptoms develop over 24-72 hrs. Labs show: inc CPK, myoglobinuria, and leukocytosis MANAGEMENT: - discontinue drug, hydration, cooling blankets - dantrolene (muscle relaxant - dec. rigidity), bromocriptine (DA agonist) |
|
|
What is serotonin syndrome?
|
Serotonin syndrome is a potentially life-threatening adverse drug reaction that may occur following therapeutic drug use, inadvertent interactions between drugs, overdose of particular drugs, or the recreational use of certain drugs. It occurs when theres serotonin excess.
The symptoms are often described as a clinical triad of abnormalities: - Cognitive effects: headache, agitation, hypomania, mental confusion, hallucinations, coma - Autonomic effects: shivering, sweating, hyperthermia, hypertension, tachycardia, nausea, diarrhea. - Somatic effects: myoclonus (muscle twitching), hyperreflexia (manifested by clonus), tremor. MANAGEMENT - discontinue medication, give serotonin antagonists, provide supportive care, including control of agitation, control of autonomic instability, and control of hyperthermia. Agitation can be control by benzos. Also hyperthermia can be treated with benzodiazepine. |
|
|
How does NMS (neuroleptic malignant syndrome) differ from SS (serotonin syndrome)?
|
- NMS severe global rigidity whereas SS involves twitchy, shivering, and restlessness
- NMS: pallor; whereas SS: flushed and sweaty - NMS: no GI Sx; whereas SS: vomiting, diarrhea, abdominal pain |
|
|
Discuss the variables involved in the calculation of coronary vascular disease based on the framingham calculator.
|
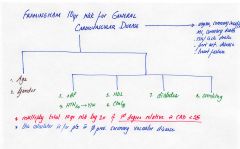
|
|
|
A pt comes to your office with 4 sinus infections over the last 6 months. You decide that the pt needs to go to ent. What investigation would you do before the pt is referred to ent?
|
ct face
|
|
|
note
|
A patient who develops cirrhosis needs screening endoscopy to check for esophageal varices. Once a pt is diagnosed w/ cirrhosis, it's best to refer them to the GI specialist. They'll probably look after the screening. If not, then the GP should look after the endoscopy screening.
|
|
|
note
|

Voltaren gel is a good option as a topical nsaid. It is available otc as emulgel. This is a 1% cream that is to be applied bid.
|
|
|
You have just diagnosed a pt w/ htn. What are standard htn investigations to do?
|
- cbc, lytes, Cr
- fasting glucose, fasting lipids - urinalysis - ekg note: may also consider tsh (though not part of the guidelines) note: If an ekg has been done within the last 1-2yrs, no need to do another one. The reason for an ekg is to check for ventricular hypertrophy. |
|
|
note
|
For a pt who has had a vasectomy, it is important to check if they still have post-vasectomy sperm; this is typically checked by the urologist within 3 months. No further need to recheck.
|
|
|
What are comedones?
|

A comedo is a clogged hair follicle (pore) in the skin. Keratin (skin debris) combines with oil to block the follicle. A comedo can be open (blackhead) or closed by skin (whitehead), and occur with or without acne. The word comedo comes from Latin to suggest the worm-like look of a blackhead that has been secreted. The plural of comedo is comedones.
|
|
|
What are the 6 clinical features of duodenal ulcers?
|
i. epigastric pain
ii. burning iii. 1-3 hrs post prandial iv. relieved by eating, antacids v. interrupts sleep vi. periodicity |
|
|
Discuss indications for bmd testing.
[osteoporosis] |
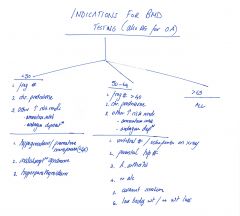
|
|
|
What investigations do you order on suspicion of mononucleosis?
|
i. cbc
ii. monospot note: both of these can be put on the bw requisition form note: avoid ordering ebv titres |
|
|
note
|
If a pt is on allopurinol for gout prophylaxis and develops and acute gouty flare, it is important to warn the pts to stop taking allopurinol during an acute gouty episode as this can make things worse.
|
|
|
List the two main interventional procedures used for treating tension pneumothorax.
|
i. needle thoracocentesis [immediate treatment] (2nd intercostal space midclavicular line)
ii. chest tube [definitive treatment] (5th intercostal space midaxillary line) |
|
|
What is the management of vasomotor rhinitis?
|
nasonex 50mcg/spray
2 sprays in each nostril od |
|
|
What can you recommend for a pt who has mild epistaxis 2' scoughing of the nasal mucosa due to rhinorrhea from a urti?
|
i. secaris (lubricating nasal gel)
ii. nasogel (lubricating nasal gel) note: both are otc |
|
|
note
|
When a patient or pt's parent comes in for allergy testing, there are 3 important pts to consider:
i. antihistamines ii. pinpoint allergy (may require allergist) iii. allergy shots (will require allergist) |
|
|
Write a prescription for insulin, needle tips, glucometer, and test strips.
|
insulin prescription
1. lantus/levermir S: 3cc cartridge M: 3 boxes R: 99 2. needle tips M: 1 box R: 99 3. glucometer x 1 (glucometer M:1) 4. test strips M: box of 100 R: 99 –------------------------------------------------------- note: * 100u/cc therefore 300u/cartridge 5 cartridges / box S = sig = dose Victoza cost $300/month (costco cheapest pharmacy: no costco membership required) |
|
|
Would you choose amoxicillin or would you choose biaxin for 1st line management of community acquired pneumonia?
|
biaxin is a better option as it will cover atypical organisms
|
|
|
A pt is dx w/ depression and wants to quit smoking. Write the prescription for the ideal medication in this situation.
|
wellbutrin xl
take 150mg od M: 60 tablets |
|
|
What is Bell's palsy?
What is the ddx? |

Bell's palsy is a form of facial paralysis resulting from a dysfunction of the cranial nerve VII (the facial nerve) causing an inability to control facial muscles on the affected side. Several conditions can cause facial paralysis, e.g., brain tumor, stroke, myasthenia gravis, and Lyme disease. However, if no specific cause can be identified, the condition is known as Bell's palsy. Bell's palsy is the most common acute mononeuropathy (disease involving only one nerve) and is the most common cause of acute facial nerve paralysis (>80%).
Bell's palsy is defined as an idiopathic unilateral facial nerve paralysis, usually self-limiting. The hallmark of this condition is a rapid onset of partial or complete paralysis that often occurs overnight. In rare cases (<1%), it can occur bilaterally resulting in total facial paralysis. It is thought that an inflammatory condition leads to swelling of the facial nerve. The nerve travels through the skull in a narrow bone canal beneath the ear. Nerve swelling and compression in the narrow bone canal are thought to lead to nerve inhibition, damage or death. Corticosteroids have been found to improve outcomes, when used early, while anti-viral drugs have not. Most people recover spontaneously and achieve near-normal to normal functions. Many show signs of improvement as early as 10 days after the onset, even without treatment. Often the eye in the affected side cannot be closed. The eye must be protected from drying up, or the cornea may be permanently damaged resulting in impaired vision. In some cases denture wearers experience some discomfort. |
|
|
What are the indications for imaging in a child with a urinary tract infection (uti)?
|
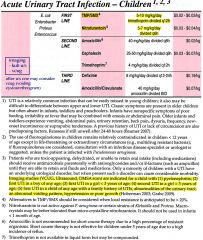
|
|
|
note
|
It is important to warn patients that acne when treated with medication will often get worse before getting better so its important to give it a fair trial.
|
|
|
T/F. Weight gain is NOT a side effect of OCPs.
|
True
|
|
|
A pt presents w/ a bartholin cyst ~3cm across. What would you do for management?
|
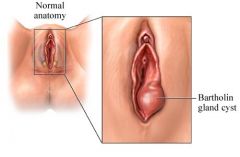
- chlorhexadine + 2% lidocaine
- needle aspiration (18 gauge); throw collection into garbage - abx: cipro 500mg bid x 7d and flagyl 500mg bid x 7d - tylenol #3 q4h prn x 15 tablets - refer to gynecology; may have to get marsupialization +/- biopsy |
|
|
note
|
caution / contraindications to oral steroids include (but not limited to):
- severe renal failure - severe liver disease - osteoporosis - elderly pts - HTN, CHF |
|
|
note
|
It is best to be cautious in ordering shoulder ultrasounds in elderly pts as most of them will have tears anyways. Then you end up chasing your tail.
|
|
|
note
|
For lactose intolerance, symptoms typically improve within days of not having any milk products. This is because you are removing the agent that cannot be digested from the gut. No agent = no GI upsets.
|
|
|
note
|
There is no point ordering the celiac serology in a pt who has been on a non-celiac diet. The patient needs to be on celiac diet in order for the test to be useful.
If a patient has celiac disease and they get symptoms of GI upset, then likely their villi are destroyed. They need to abstain from celiac products for weeks (~1 month) before noticing an improvement in sx. |
|
|
T/F. Statins are contraindicated in pregnancy.
|
True
Other drugs that are contraindicated in pregnancy are: - prednisone - ACEi, diuretics, propanolol (teratogens) |
|
|
What is the management of status asthmaticus?
|
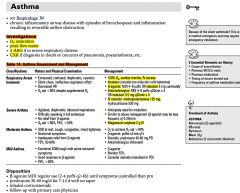
|
|
|
Discuss specific htn (hypertension) investigations related to 2' causes.
|

|
|
|
Discuss the interpretation of hepatitis b serology.
|

|
|
|
A patient asks you when she should start the OCP. What do you tell her?
[oral contraceptive pills] [OCPs] |
- quick start is best
- just start it that day It does not have to be related to when your periods are. |
|
|
Discuss an approach to pregnancy.
|
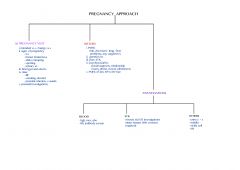
|
|
|
Discuss genetic screening in pregnancy.
|
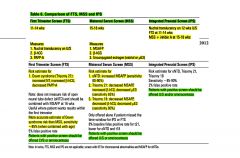
|
|
|
Discuss the difference between amniocentesis and cvs.
[chorionic villus sampling] |

|
|
|
What is preterm labour? What are some RFs and how do you predict it?
|
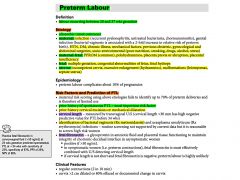
|
|
|
What is infantile colic and what is the management?
|

|
|
|
What is necrotizing enterocolitis (NEC)?
|
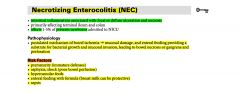
|
|
|
For necrotizing enterocolitis, discuss clinical presentation, investigations, and treatment.
|

|
|
|
What is your ddx in a crying /fussing child?
|
- infantile colic
- constipation, diarrhea, anal fissure - intussusception, volvulus - meningitis, sepsis, necrotizing enterocolitis - pneumonia, chf - shaken baby syndrome, fracture |
|
|
Discuss the etiology of acute otitis media (aom).
|
|
|
|
What is scarlet fever? What is the treatment?
|

|
|
|
What is roseola? What is the treatment? What are some complications?
|

|
|
|
What is enuresis and what is the management?
|

|
|
|
Discuss the various fracture descriptions and patterns.
|
|
|
|
What are 2 drugs that can be used to treat long term opioid addiction?
|
i. methadone
ii. buprenorphine |

