![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
245 Cards in this Set
- Front
- Back
|
Parietal-Occipital Association Areas
|
5-7, 18-19
|
|
|
Occipital-Temporal Association Areas
|
37, 20-21
|
|
|
Speech Areas Association Areas
|
22, 39-40, 42*, 44-45
|
|
|
Prefrontal Association Areas
|
9,10,11, 46-47
|
|
|
Parieto-temporal association cortex
|
(non-dominant hemisphere)
Parietal: mediates spatial relationships, attention; Temporal: object and face recognition (in both hemispheres) |
|
|
Parieto-temporal-frontal association cortex
|
(dominant hemisphere)
mediates language comprehension (Wernicke’s area) and expression (Broca’s area); also reading, writing. |
|
|
Prefrontal association cortex
|
mediates planning, judgment, intellect: so called executive functions leading to goal-directed behaviors. Connections with limbic areas integrate cognition with emotions
|
|
|
Limbic cortex
|
mediates emotions, memory
|
|
|
ventral Intraparietal cortex (VIP)
|
integration of multimodal information for constructing a spatial representation of the external world (in relation to the body or parts thereof)
|
|
|
Optical Ataxia
|
Misreaching (loss of visual guidance)
caused by anterior intraparietal sulcus lesion (dorsomedial parietal cortex) |
|
|
Inferotemporal cortex
|
the P system visual pathway: the “what”; object, face recognition
|
|
|
prosopagnosia
|
an inability to recognize faces of specific persons
|
|
|
Posterior parietal cortex
|
the M system visual pathway: the “where”, spatial integration, location
|
|
|
Apperceptive Agnosia
|
imparied ability to match or copy complex visual shapes or objects. Damage to posterior inferior temporal cortex
|
|
|
Associative Agnosia
|
Patients can match or copy an object, but their ability to identify the object is impaired. Damage to the anterior inferior temporal cortex
|
|
|
Frontal Lobe Series
|
Orbitofrontal-Ventromedial Prefrontal Cortex (OF)
Dorsolateral Prefrontal Cortex (DLPFC) Premotor Cortex (PM) Primary Motor (M1) |
|
|
Ventrolateral PFC Areas
|
47, 45, 44
|
|
|
Dorsolateral PFC Areas
|
46, 8
|
|
|
Ventromedial PFC Areas
|
32
|
|
|
Medial PFC Areas
|
9
|
|
|
Orbitofrontal PFC Areas
|
11, 12, 13
|
|
|
Dorsolateral Prefrontal Cortex
|
receives multi-sensory input via parietal association cortex. Outputs are to suppl. motor areas and basal ganglia. Encodes behaviors related to spatial relationships, working memory, shifting cognitive sets. (Wisconsin card sorting)
|
|
|
Ventrolateral Prefrontal Cortex
|
receives temporal lobe visual association input. Encodes behavior specific to object recognition tasks, relational (deductive) reasoning, ability to form analogies (“I am going to be a dinosaur if I don’t make this sale”)
|
|
|
Orbitofrontal and Medial Cortex
|
connected to medial temporal limbic areas related to affect and motivation. Encodes behaviors that have emotional significance; requires restraint and delay in gratification
anticipated reward |
|
|
Dorsolateral PFC Testing
|
Verbal fluency decreases
Delayed Response task Wisconsin Card Sort Test |
|
|
Verbal fluency test
|
Patient asked to write down 5-letter words that start with an “R”.
|
|
|
Delayed Response Task
|
Animal allowed to watch while food is placed under one of the two objects and a curtain is drawn. After delay the curtain is raised and animal must chose the container to get food. Low success in dlPFC (BA 48) lesion
|
|
|
Wisconsin Card Sort Test
|
Patient must learn from feedback which sorting scheme is correct
|
|
|
Anterior Cingulate Cortex
|
ACC monitors behavioral conflict, influencing the preparation or organization of the behavior in the dlPFC
|
|
|
Orbitofrontal and Ventromedial PFC Test
|
Gambing Test - those with damaged areas will continue with losing strategy
|
|
|
Reward Pathway
|
Dopamine:
VTA -> N. accumbens -> PFC |
|
|
Deductive Reasoning
|
Inferior PFC
|
|
|
Inductive Reasoning
|
Dorsolateral PFC
|
|
|
dMPFC in Theory of Mind
|
Cognitive Empathy
|
|
|
vMPFC in Theory of Mind
|
Attribution of emotional empathy
|
|
|
TPJ in Theory of Mind
|
Recognizing the mental state of a person
|
|
|
pSTS in Theory of Mind
|
Understanding intention or goal of a person
|
|
|
extrastriate body area (EBA) in Theory of Mind
|
Detecting presence of a person
|
|
|
Absolute indicators for immediate further evaluation
|
No babbling by 12 months
No gesturing (pointing, waving good bye) by 12 months No single words by 16 months No two-word spontaneous (not just echolalic) phrases by 24 months ANY loss of ANY language or social skills at ANY age |
|
|
Alzheimer's Risk Factors
|
ApoE polymorphisms
Age Hypercholesterolemia Diet |
|
|
The person may feel as if he or she is having memory lapses — forgetting familiar words or the location of everyday objects. But no symptoms of dementia can be detected during a medical examination or by friends, family or co-workers.
|
Stage 1 Very mild cognitive decline (may be normal age-related changes or earliest signs of Alzheimer's disease)
|
|
|
Friends, family or co-workers begin to notice difficulties. During a detailed medical interview, doctors may be able to detect problems in memory or concentration. Common stage 3 difficulties include:
Noticeable problems coming up with the right word or name Trouble remembering names when introduced to new people Having noticeably greater difficulty performing tasks in social or work settings Forgetting material that one has just read Losing or misplacing a valuable object Increasing trouble with planning or organizing |
Stage 2 Mild cognitive decline (early-stage Alzheimer's can be diagnosed in some, but not all, individuals with these symptoms)
|
|
|
At this point, a careful medical interview should be able to detect
clear-cut symptoms in several areas: Forgetfulness of recent events Impaired ability to perform challenging mental arithmetic — for example, counting backward from 100 by 7s Greater difficulty performing complex tasks, such as planning dinner for guests, paying bills or managing finances Forgetfulness about one's own personal history Becoming moody or withdrawn, especially in socially or mentally challenging situations |
Stage 3 Moderate cognitive decline (Mild or early-stage Alzheimer's disease)
|
|
|
Gaps in memory and thinking are noticeable, and individuals begin to need help with day-to-day activities. At this stage, those with Alzheimer's may:
Be unable to recall their own address or telephone number or the high school or college from which they graduated Become confused about where they are or what day it is Have trouble with less challenging mental arithmetic; such as counting backward from 40 by subtracting 4s or from 20 by 2s Need help choosing proper clothing for the season or the occasion Still remember significant details about themselves and their family Still require no assistance with eating or using the toilet |
Stage 4 Moderately severe cognitive decline (Moderate or mid-stage Alzheimer's disease)
|
|
|
Memory continues to worsen, personality changes may take place and individuals need extensive help with daily activities. At this stage, individuals may:
Lose awareness of recent experiences as well as of their surroundings Remember their own name but have difficulty with their personal history Distinguish familiar and unfamiliar faces but have trouble remembering the name of a spouse or caregiver Need help dressing properly and may, without supervision, make mistakes such as putting pajamas over daytime clothes or shoes on the wrong feet Experience major changes in sleep patterns — sleeping during the day and becoming restless at night Need help handling details of toileting (for example, flushing the toilet wiping or disposing of tissue properly) Have increasingly frequent trouble controlling their bladder or bowels Experience major personality and behavioral changes, including suspiciousness and delusions (such as believing that their caregiver is an impostor)or compulsive, |
Stage 5 Severe cognitive decline (Moderately severe or mid-stage Alzheimer's disease)
|
|
|
In the final stage of this disease, individuals lose the ability to respond to their environment, to carry on a conversation and, eventually, to control movement. They may still say words or phrases.
At this stage, individuals need help with much of their daily personal care, including eating or using the toilet. They may also lose the ability to smile, to sit without support and to hold their heads up. Reflexes become abnormal. Muscles grow rigid. Swallowing impaired. |
Stage 6 Very severe cognitive decline (Severe or late-stage Alzheimer's disease)
|
|
|
Cellular factors affecting ABeta production
|
LRP1
SORL1 |
|
|
Factors that affect ABeta aggregation and clearance
|
LRP1
RAGE Nerilysin IDE CSF/ISF Flow |
|
|
Presenilin-1 (PS-1)(PSEN1 gene)
|
second gene with mutations found to cause early-onset of Alzheimer's. Variations in this gene are the most common cause of early-onset Alzheimer's.
|
|
|
Presenilin-2 (PS-2)(PSEN2 gene)
|
is the third gene with mutations found to cause early-onset Alzheimer's.
|
|
|
Apolipoprotein E-e4 (APOE4)
|
first gene variation found to increase risk of Alzheimer's and remains the risk gene with the greatest known impact. Having this mutation, however, does not mean that a person will develop the disease.
|
|
|
Stage a Alzheimer’s Disease Histology
|
Cellular processes of brainstem nerve cells (e.g. caeruleus neurons) are the earliest structures that display AT8-immunoreactive pretangle material (Stage a).
|
|
|
Stage b Alzheimer’s Disease Histology
|
The material fills the soma and dendritic processes of a few neuromelanin-containing caeruleus neurons
|
|
|
Stage c Alzheimer’s Disease Histology
|
pretangle material occurs in nerve cells of other nonthalamic brainstem nuclei with diffuse cortical projections (upper raphe nuclei, magnocellular nuclei of the basal forebrain, hypothalamicn tuberomammillary nucleus).
|
|
|
Stage 1a Alzheimer’s Disease Histology
|
portions of neuronal processes containing pretangle material appear in the transentorhinal region. These processes may represent pathologically altered terminals of caeruleus axons.
|
|
|
Stage 1b Alzheimer’s Disease Histology
|
isolated pyramidal cell somata of the transentorhinal region together with their cellular processes become filled with pretangle material and, thereafter, increase in number.
|
|
|
Order of AD Symptoms/Signs
|
decrease in CSF ABeta42
increase in ABeta Fibrils increase in CSF tau hippocampal atrophy hypometabolism cognitive decline |
|
|
Neuroprotectin D1 (NPD1)
|
Reduced in CA1 region of AD Brain
Shifts APP Processing from Amyloidogenic to Non-Amyloidogenic Pathway Reduced COX-2 and B94 Positive Cells in Ab-Stressed HN Cells |
|
|
Docosahexaenoic acid (DHA)
|
Attenuates Abeta Secretion with Concomitant NPD1 Biosynthesis
|
|
|
Neural Growth Factor (NGF)
|
Excreted by Schwann Cells in peripheral nerve injuries
regrowth and prevents the presynaptic cell (not shown) from withdrawing |
|
|
glial scar
|
myelin fragments and astrocytes and macrophages fill the site of injury in the CNS
|
|
|
Ciliary neurotrophic factors (CNTF)
|
activate GP130 receptors causing growth. But, cytokine suppressor SOCS3 inhibits the regrowth pathway
|
|
|
SOCS3
|
cytokine suppressor that inhibits the regrowth pathway
|
|
|
BDNF (brain derived neurotrophic factor)
|
released along with NGF to guide the axon back to NMJ sites
|
|
|
Agrin
|
promotes or maintains AChR clustering
|
|
|
MuSK
|
transmembrane protein version of tyrosine kinase. Functions as an agrin receptor critical to AchR clustering
|
|
|
Neuregulin-1
|
protein responsible for transcription of AChRs at post-synaptic site
|
|
|
secreting oligodendrocyte transcription factor 2 (OLIG2)
|
inhibits axonal growth in the CNS
|
|
|
Bcl-2: (B-cell lymphoma 2)
|
anti-apoptosis protein
|
|
|
Two regions that retain neurogenesis capabilities in mammals
|
(1) the subgranular zone (SGZ) of the hippocampal dentate gyrus
(2) the subventricular zone (SVZ), which contributes interneurons to the olfactory bulb |
|
|
the subgranular zone (SGZ)
|
hippocampal dentate gyrus area that regenerates
|
|
|
subventricular zone (SVZ)
|
contributes interneurons to the olfactory bulb
|
|
|
rostral migratory stream (RMS)
|
an intricate path of migration that neuroblasts (from astrocytes) follow towards the olfactory bulb
|
|
|
opioid effect on environmentally induced neurogenesis
|
negates
|
|
|
A heterogeneous group of related, early-onset, chronic disorders that share the essential feature of a disturbance in the acquisition of cognitive, motor, language, or social skills.
|
Developmental Disabilities
|
|
|
children under the age of 5 years who are 2 or more standard deviations below the mean on age-related, standardized developmental assessments.
operationally defined as significant delay in two or more developmental domains (gross motor, fine motor, cognition, speech/language, personal/social, activities of daily living) |
Global Developmental Delay
|
|
|
children over 5 years of age who demonstrate “significant” (greater than -2 SD’s) sub-average general intellectual functioning existing with concomitant deficits in adaptive behavior.
Full Scale IQ of less than 70 along with commensurate disabilities within the realms of adaptive functioning. |
Mental Retardation
|
|
|
Average Intelligence
|
85-115
|
|
|
Borderline Intelligence
|
70-84 (one SD)
|
|
|
Mild Mental Retardation
|
50-69 (two SD’s)
|
|
|
Moderate Mental Retardation
|
35-49
|
|
|
Severe Mental Retardation
|
20-34
|
|
|
Profound Mental Retardation
|
<20
|
|
|
AAP Recommended Screening Tools
|
Ages and Stages Questionnaire
Parental Evaluation of Developmental Status (PEDS) Brigance Screen not Denver II |
|
|
Static Encephalopathy Course
|
linear incline in milestones with age but below normal
|
|
|
Neurodegenerative Disease Course
|
plateau and decline in milestones achieved
|
|
|
Global Developmental Delay: Significant delay
|
>2 SD below the mean on the basis of standardized testing in two or more developmental domains:
Gross/Fine Motor Language Social Adaptive This term is reserved for children under the age of 5 years |
|
|
Pervasive Developmental Delay
|
Significant delay in the following developmental domains:
Language/Communication Social Restricted/Repetitive patterns of behavior |
|
|
“Neuromuscular” Developmental Delay
|
Significant delays in gross motor skills
Normal “cognitive” developmental skills Language skills Social skills Suggests possible neuropathy, myopathy, or neuromuscular junction disorder |
|
|
Cerebral Palsy
|
A non-specific term pertaining to non-progressive changes in tone and posture resulting from a “one-time” injury or malformative process to the developing central nervous system
Considered a static encephalopathy The term does not include an evaluation of intelligence! |
|
|
Cerebral Palsy Signs & Symptoms
|
Spastic
Choreoathetotic Dystonic Ataxic Hypotonic Mixed |
|
|
Prenatal Etiologies of Developmental Disabilities
|
Congenital Malformations of the CNS
Genetically-determined abnormalities of brain structure/function Maternal illness/injury during pregnancy Maternal exposure to exogenous toxins/drugs Maternal/fetal infection Prematurity |
|
|
Perinatal Etiologies of Developmental Disabilities
|
Perinatal Trauma
Hypoxic Ischemic Encephalopathy |
|
|
Postnatal Etiologies of Developmental Disabilities
|
Inborn errors of metabolism
Abnormal postnatal growth or nutrition Endogenous toxins (eg. renal or liver failure, endocrine abnormalities) Exogenous toxins (eg. lead) Acquired postnatal infection Acquired CNS trauma CNS Tumors Neurocutaneous Disorders |
|
|
Adenoma Sebaceum, Cortical Tuber, Ash Leaf Macule, Giant Cell Astrocytoma
|
Tuberous Sclerosis
|
|
|
Fibroma Molluscum, Café-au-lait macules, Lisch Nodules, Optic Nerve Glioma
|
Neurofibromatosis Type I
|
|
|
port-wine stain birthmark (usually on the face) and nervous system problems
|
Sturge Weber Syndrome
|
|
|
Caudal Regression Malformation
|
secondary to maternal Diabetes Mellitus
|
|
|
Spasticity
|
velocity dependent resistance to stretch in a passive limb
|
|
|
Dystonia
|
sustained muscle contractions causing twisting and repetitive movements, abnormal postures or both
|
|
|
Associated with Prematurity
IVH at 24-32 Weeks Periventricular leukomalacia Lower Extremity > Upper Extremity Primary Problem : Lack of selective motor control |
Spastic Diplesia Cerebral Palsy
|
|
|
Full Term Infants- related to vascular injury or maldevelopment
Cortical – A>L Dominate hand ? May be missed early |
Hemiparesis Cerebral Palsy
|
|
|
Usually occurs in small Full Term infants or VLBW Infants
Early hypotonia or spasticity All four extremities Involved Usually a combination of Spasticity and Dystonia |
Spastic Quadriparesis Cerebral Palsy
|
|
|
Usually full term
Generally hypotonic at birth may be opisthotonic Persistent Moro and ATNR reflex Classic movement pattern emerges by 18 months |
Dyskinetic Cerebral Palsy
|
|
|
BoNT-A
|
established to reduce spasticity in the u and l extremities
|
|
|
Agitation, confusion, poor concentration and orientation, misperception of sensory stimuli, visual or tactile hallucinations
Alertness intact but disturbed content of consciousness Generalized or multifocal process affecting both cerebral hemispheres |
Delerium
|
|
|
Refers to the awareness of self and environment
|
Consciousness
|
|
|
Unarousable Unresponsiveness
Consciousness: None Eyes: Do not open to any stimulus Vocalization: None Motor: No purposeful movements |
Coma
|
|
|
Patients who have survived coma without gaining higher cognitive function
Consciousness: None Eyes: Spontaneous eye opening and closure Vocalization: Groans and Grunts, no formed words or purposeful communication Motor: Postures or withdraws to noxious stimulus, occasional nonpurposeful movement EEG: Preserved sleep and wake cycles |
Vegetative State
|
|
|
Severely altered consciousness but with definite behavioral evidence of awareness of self and environment
Follows simple commands Gestural or verbal “yes/no” responses Intelligible verbalization Movements and affective behaviors occur in contingent relation to relevant environment stimuli and not attributable to reflexive activity |
Minimally Conscious State
|
|
|
Loss of voluntary motor control and vocalizations with preserved consciousness
Bilateral injury to the cortic-spinal and cortical-bulbar tracts Pontine hemorrhage, tumor, demyelination |
Locked-In Syndrome
|
|
|
Consciousness: Preserved
Eyes: No lateral movements, blink and vertical eye movements preserved, vision intact Vocalizations: Aphonic/Anarthric Motor: Quadriplegic EEG: Normal awake background |
Locked-In Syndrome
|
|
|
Supratentorial Lesions
|
affecting Bilateral Cerebral Hemispheres/Thalamic Nuclei
|
|
|
Infratentorial Lesions
|
Affecting the Brainstem Reticular Activating System
|
|
|
Subdural Hematoma
|
Subfalcine and Transtentorial Herniation
|
|
|
Intraventricular Hemorrhage
|
Hydrocephalus, and Central Herniation
|
|
|
Apnea Test
|
No CNS Depressants or NMJ Blockade
Ventilate with 100% FiO2 for 20 minutes Disconnect Ventilator and Continue O2 ABG until PCO2 > 60mmHg Watch for any signs of ventilation |
|
|
Irriversible cessation of all cerebral activity, including that of the brainstem
|
Brain Death
|
|
|
Irreversible deep coma and lack of spontaneous respiration
|
Brain Death
|
|

|
|
|

|
|
|

|
|
|

|
|
|

|
|
|

|
|
|

|
|
|

|
|
|

|
|
|

|
|
|

|
|
|

|
|
|

|
|
|
|
|
|

|
|
|

|
|
|

|
|
|
|
penumbra
|
surrounding traumatized zone with the dead and the living, apoptosis can be substantial
|
|
|
Left superior MCA infact
|

|
|
|
Left Inferior MCA Infarct
|

|
|
|
Left deep MCA Infarct
|
|
|
|
Left MCA Stem Infarct
|

|
|
|
Right superior MCA Infarct
|
|
|
|
Right Inferior MCA Infarct
|

|
|
|
Right deep MCA Infarct
|
|
|
|
Right MCA Stem Infarct
|
|
|
|
Left ACA Infarct
|

|
|
|
Right ACA Infarct
|

|
|
|
Left PCA Infarct
|
|
|
|
Right PCA Infarct
|
|
|
|
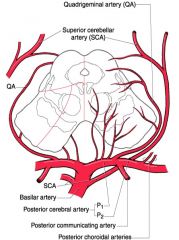
ipsilateral ataxia, vertigo, nystagmus, nausea decrease ipsi pain/temp (face), contra pain/temp (body), hoarseness, dysphagia, ipsilateral Horner’s syndrome
|
Lateral medullary (Wallenberg) syndrome: PICA
|
|
|
contralateral paresis, decreased sense of touch, position, vibration (contra body), ipsilateral tongue weakness
|
Medial medullary syndrome
|
|
|
contra paresis, face weakness, dysarthria
contralateral and/or ipi ataxia ipsilateral horizontal gaze palsy contralateral touch, sense, vibration |
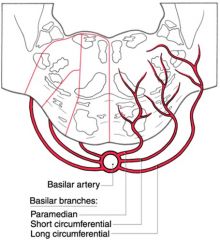
Pontine infarct of paramedian branches of basilar artery
|
|
|
ipsilateral ataxia, vertigo, nystagmus, decreased pain, temp (face), decreased pain, temp (contra body)
|
AICA Syndrome
|
|
|
ipsilateral ataxia, possible: vertigo, nystagmus
|
SCA Infarct: dorsolateral rostral pons
|
|
|
3rd nerve palsy
contralateral hemiparesis contra ataxia ataxia, tremor, involuntary movements |
Midbrain Infarct: branches of PCA,
top of basilar arteries |
|
|
Acquisition of novel behavior through experience. Or, an enduring change in the underlying mechanisms of behavior resulting from experience with stimuli and responses to the stimuli
|
Learning
|
|
|
a change in the animal's behavior as a function of experience with (usually) a single stimulus. It does not rely on learning a specific temporal relationship between different stimuli
|
Non-associative Learning
|
|
|
Learn the relationship between multiple stimuli
|
Associative Learning
|
|
|
the progressive decrease in responding to a stimulus when that stimulus is repeatedly presented.
|
Habituation
|
|
|
the partial or complete restoration of a habituated response following presentation of another, novel stimulus.
|
Dishabituation
|
|
|
the enhancement of a response following the presentation of a novel (typically strong or noxious) stimulus
|
Sensitization
|
|
|
Modulatory Neurotransmitter in Dishabituation
|
Serotonin (5-HT)
|
|
|
Molecular Action in Dishabituation
|
Output K+ channel closes lengthening the depolarization and increased intracellular Ca++
|
|
|
temporary maintenance and manipulation of information not currently available to the sense but necessary for successfully achieving shor-term behavioral objectives
|
Working Memory (traditionally called short-term memory)
|
|
|
refers to remembering personal events, cultural history, semantic information, and other facts that we can be explicitly aware of
|
Declarative Memory
|
|
|
retrieval of old memories happens here
|
Posterior lateral parietal and posterior midline regions
|
|
|
a heterogeneous category that covers several different forms of memory that are expressed through performance without the requirement of conscious content
|
Nondeclarative memory
|
|
|
Location of neural activation related to semantic priming
|
Anterior temporal cortex
|
|
|
MTL Pathology in Vascular Disease
|
CA1 shows the most reliable loss of neurons
|
|
|
MTL Pathology in Alzheimer's Disease
|
the pattern of cell death and other histological findings suggests that the entorhinal cortex is prominently affected, that CA1 and the subiculum are also heavily involved, and that the dentate gyrus and CA3 are relatively preserved
|
|
|
MTL Pathology in Temporal Lobe Epilepsy
|
cell death occurring predominantly in the dentate gyrus and CA subfields — one finding distinguishes it from AD: entorhinal cortex cell death is observed in both diseases, but is more pronounced in Alzheimer's disease, in which it starts in layer II, whereas in TLE it seems to be confined to layer III neurons
|
|
|
Some retrograde memory deficits
Diminished intellectual faculties Obvious psychiatric symptoms, including tendency for fabrication, apathy Severe anterograde amnesia Involves damage to mammillary bodies, + dormosomedial nu, and disrupted circuitry to anterior nucleus-cingulate gyrus. Seen in chronic alcoholics with B1 thiamin vitamin deficiency |
Korsakoff Psychosis
|
|
|
Loss of intellectual skills sufficient to impair social or occupational function.
Memory impairment. Impaired abstraction Impaired judgement Aphasia Agnosia Visuospatial difficulty Personality changes No impairment of consciousness |
Dementia
|
|
|
TREM2
|
risk variant for Alzheimers
|
|
|
Fluctuation in cognition and attention
Recurrent well-formed visual hallucinations Parkinsonism Supportive Features: repeated falls, syncope, neuroleptic sensitive, delusions |
Dementia with Lewy Bodies
|
|
|
Donepezil
|
Reversible acetylcholinesterase inhibitor
treats dementia |
|
|
Razadyne (galantamine)
|
Reversible cholinesterase inhibitor
treats dementia |
|
|
Exelon® (rivastigmine tartrate)
|
Reversible cholinesterase inhibitor
treats dementia |
|
|
Namenda (memantine)
|
NMDA receptor antagonist
Treats moderate to severe dementia |
|
|
NMO autoantibody
|
for AQP4
|
|
|
involves the optic nerves and spinal cord: spinal cord lesions tend to be longitudinally extensive
|
Neuromyelitis Optica
|
|
|
Neurobiological function that produces dynamic selection of stimuli for increased or more effective neural processing
|
Attention
|
|
|
Allocation of processing resources to the analysis of certain stimuli or aspects in the environment, generally at the expense of resources allocated to other stimuli or aspects
|
Selective Attention
|
|
|
Endogenous Attention Areas
|
Intraparietal Sulcus
Frontal Eye Field |
|
|
Exogenous Attention Areas
|
right temporo-parietal junction (JPT)
right ventral frontal cortex amygdala |
|
|
P1 visual peak
|
low-level extrastriate visual cortex (V2,3,4)
|
|
|
N1 visual area
|
parietal visual areas
|
|
|
failure to report, orient, sometimes even
to deny one side of the body. Often confined to the left side of body = deficit of attention (because right hemisphere is non-dominant). difficulty with complex tasks such as drawing, dressing. Loss of an integrated spatial gestalt. deficits in spatial relationships such as block construction = “constructional apraxia” defects of affect - humorless, with lack of appropriate concern; loss of prosody of speech; and often a decrease in alertness. |
Contralateral Neglect Syndrome from Right PC (non-dominant)
|
|
|
Simultanagnosia: inability to attend to more than one visual object at a time
Optic ataxia: inability to reach for an object in space under visual guidance (VIP lesion likely) Oculomotor apraxia: difficulty directing gaze toward objects using saccades |
Bilateral Brain lesions: Balint’s syndrome
|
|
|
Alexia (can’t read)
Anomia (can’t name objects) contructional Apraxia (can’t construct simple figures) Agraphia (inability to write) Finger agnosia (inability to name individual fingers Confusion of left and right personal/extrapersonal space |
damage to angular gyrus (BA 39)
|
|
|
Alexia (can’t read)
Anomia (can’t name objects) contructional Apraxia (can’t construct simple figures) Agraphia (inability to write) Finger agnosia (inability to name individual fingers Confusion of left and right personal/extrapersonal space Acalculia finger agnosia right/left disorientation |
Gerstmann syndrome (also area 39)
|
|
|
Methylphenidate (Ritalin)
|
DA reuptake inhibitor
|
|
|
Blood supply to cingulate cortex
|
Anterior Cerebral Artery (ACA)
|
|
|
Blood supply to motor strip (representation of lower extremities)
|
Anterior Cerebral Artery (ACA)
|
|
|
Blood supply to ant limb of int capsule
|
Anterior Cerebral Artery (ACA)
|
|
|
Blood supply to caudate head
|
Anterior Cerebral Artery (ACA)
|
|
|
Blood supply to lateral aspects of parietal lobe
|
Middle Cerebral Artery (MCA)
|
|
|
Blood supply to basal ganglia
|
Lenticulostriate aa. via Middle Cerebral Artery (MCA)
|
|
|
Blood supply to internal capsule
|
Lenticulostriate aa. via Middle Cerebral Artery (MCA)
|
|
|
Blood supply to lateral aspects of frontal lobes
|
Middle Cerebral Artery (MCA)
|
|
|
Blood supply to lateral aspects of superior temporal lobe
|
Middle Cerebral Artery (MCA)
|
|
|
Blood supply to Putamen
|
Anterior Cerebral Artery (ACA)
|
|
|
Blood supply to Posterior Globus Pallidus
|
Anterior Choroidal aa. via Internal Carotid Artery (ICA)
|
|
|
Blood supply to Thalamus
|
Thalamoperforator (anterior) & Thalamogeniculate (posterior) aa. via Posterior Cerebral Artery (PSA)
|
|
|
Stria Terminalis Pathway
|
Visceral Emotion (hypothalamus)
|
|
|
Ventral Amygdalofugal pathway
|
Emotional Memory Instrumental Action (targets include, NA, septum, cortex)
|
|
|
Aversion systems
|
septum
amygdala posterior hypothalamus (produce fear, anxiety, rage) |
|
|
Gratification Systems
|
nu. accumbens
anterior hypothalamus brainstem nu (elicit sensations of pleasure and reward) |
|
|
Emotional Memory systems
|
hippocampus
dorsal medial thalamus amygdala (areas concerned w short-term memory associated with emotion) |
|
|
Visual agnosia - loss of object recognition
Hypermetamorphosis - object obsession Oral tendencies - placing inedible objects in the mouth. Hyper-appetitive - overeating Hypersexuality Loss of emotional valence Tame, docile behavior |
Klϋver-Bucy Syndrome
Bilateral lesions of the anterior temporal lobe (including amygdala) |
|
|
Chronic effects of SSRIs
|
Downregulation of 5HT Autoreceptor
Reduction in 5HT2A postsynaptic receptors |
|
|
How do antidepressants affect synaptogenesis?
|
increased BDNF translation
|
|
|
BDNF transduction pathway end-product
|
bcl-2
|
|
|
Subgenual area 25
|
upregulated in depression
|
|
|
dFr 9 and 46
|
downregulated in deppression
|
|
|
phenothiazines (thorazine, chlorpromazine)
|
block DA receptors
|
|
|
the mesolimbic dopaminergic system in schizophrenia
|
arising from the VTA projects to areas that are abnormal in schizophrenics. Over-activity in this system may produce positive symptoms.
|
|
|
mesocortical dopaminergic system in schizophrenia
|
reduced activity produces negative symptoms (lack of emotional responsiveness, thought disorder)
|
|
|
BDNF receptor
|
trk
|
|
|
SSRI mechanism of action
|
blocks SERT -> inc. 5-HT
|
|
|
ketamine mechanism of action
|
NMDA receptor antagonist -> inc. Glutamate
|
|
|
APP chromosome
|
21
|
|
|
PSEN1 chromosome
|
14
|
|
|
PSEN2 chromosome
|
1
|
|
|
ApoE4 chromosome
|
19
|
|
|
TREM2 chromosome
|
6
|
|
|
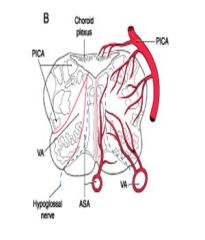
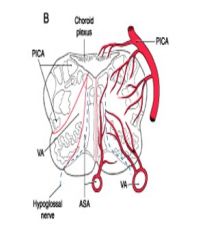
effects the pyramidal tract, medial lemniscus, hypoglossal nucleus. Produced by block of paramedian branches of and anterior spinal arteries
|
Medial Medulla = Medial medullary syndrome
|
|
|
effects the inf. cerebellar peduncle, vestibular nu, sp. trigeminal nu., anterolateral system, nucleus
ambiguus, nu. solitarius, descending sympathetic fibers. Produced by block of PICA. |
Lateral Medulla = PICA or Wallenberg syndrome
|
|
|
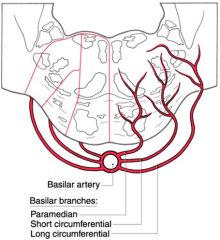
effects corticospinal and corticobulbar trs, facial colliculus (also abducens nu, medial lemniscus). Produced by block of paramedian branches of basilar artery, ventral and dorsal territories.
|
Medial Pontine Basis-Tegmentum = Foville’s syndrome
|
|
|
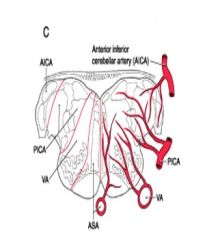
effects middle cerebellar peduncle, vestibular nu, trigeminal nu., anterolateral system, cochlear nuclei, descending sympathetic fibers. Produced by block of AICA.
|
Lateral Caudal Pons = AICA syndrome
|
|
|
effects oculomotor nerve or fascicles produced by block of branches of PCA and top of the basilar artery.
|
Midbrain Basis = Weber’s syndrome
|
|
|
effects oculomotor nerve, red nucleus, and sup. cerebellar penduncle. Produced by block of branches of PCA and top of the basilar artery
|
Midbrain Tegmentum = Claude’s syndrome
|
|
|
effects oculomotor nerve or fascicles, red nucleus, sup. cerebellar penduncle, plus substantia nigra, and cerebral peduncle produced by block of branches of PCA and top of the basilar artery.
|
Midbrain Basis+Tegmentum = Benedikt’s syndrome
|
|
|
Dermatome for shoulders
|
C4
|
|
|
Dermatome for thumb
|
C6
|
|
|
Dermatome for middle finger
|
C7
|
|
|
Dermatome for little finger
|
C8
|
|
|
Dermatome for nipples
|
T4
|
|
|
Dermatome for xiphoid
|
T6
|
|
|
Dermatome for umbilicus
|
T10
|
|
|
Dermatome for just above patella
|
L3
|
|
|
Dermatome for medial malleolus
|
L4
|
|
|
Dermatome for great toe
|
L5
|
|
|
Dermatome for lateral malleolus
|
S1
|
|
|
Dermatome for peri-anal
|
S4-5
|

