![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
62 Cards in this Set
- Front
- Back
|
location of the testis, epididymis and spermatic cord and their coverings
|
-
|
|
|
descent of the testis and relate this to anomalies associated with this process
|
-
|
|
|
blood supply, lymphatic drainage and nerve supply of the testis
|
-
|
|
|
location, function and innervation of the dartos and cremaster muscles
|
-
|
|
|
origin, course and termination of the ductus deferens
|
-
|
|
|
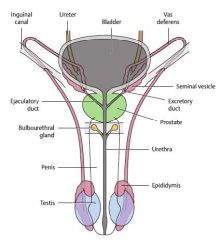
male internal genitalia, their location and function
|
-
|
|
|
anatomy of the penis and its associated muscles
|
-
|
|
|
neurovascular supply of the testis, internal genitalia and penis
|
-
|
|
|
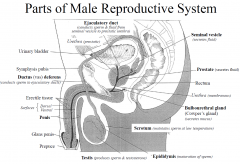
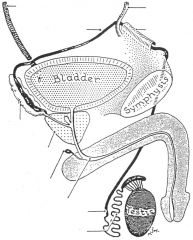
Parts of the male reproductive system
|
|
|
|
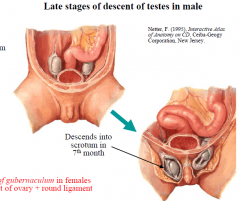
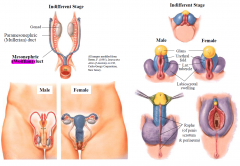
Descent of the Testes /Ovaries
|
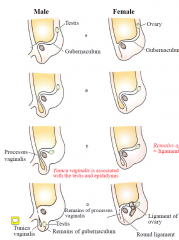
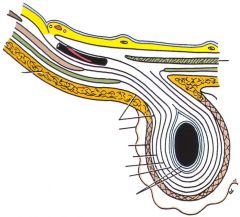
-Gubernaculum guides descent of testes through the abdominal wall (inguinal canal) into scrotum
-Processus vaginalis (a downward extension of the peritoneum) is drawn front of gubernaculum -Part of the processus vaginalis in spermatic cord later obliterates leaving tunica vaginalis |
|
|
Late Stage testes Descent
|
|
|
|
Cryptochidism
|
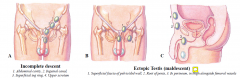
Failure of descent of one or both testis into scrotum (cryptorchidism) associated with increased risk of malignancy.
|
|
|
Congenital Anomalies
|

|
|
|
Male and Female - Development
|
|
|
|
Male Development (penis)
|

|
|
|
Forms of Hypospadias
|

|
|
|
|
|
|
Scrotum Function
|
-maintains sperm at ~3o below body temperature
|
|
|
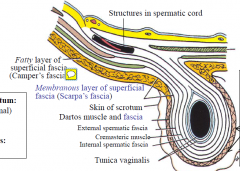
Dartos Muscle
|
-smooth muscle, sympathetic control
-contracts in response to cold & brings testis closer to body -relaxes in response to warmth continuation of the camper's fascia |
|
|
Cremaster Muscle
|
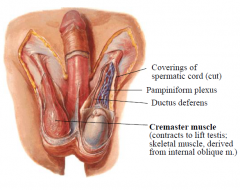
-skeletal muscle; lifts testis;
-protective reflex, active in very young -Cremasteric reflex: stroke medial upper thigh reflex retraction of testis (L1/2) |
|
|
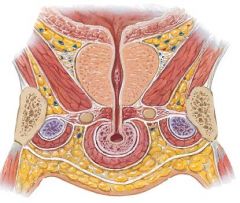
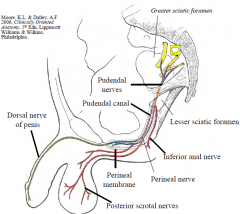
Sensory to scrotum and penis
|
Sensory supply to skin of scrotum:
-anterior 1/3rd via L1 (ilioinguinal) -post 2/3rd via S3 (pudendal) Sensory supply to skin of penis: - pudendal nerve |
|
|
-
|
|
|
The processus vaginalis
|
The processus vaginalis is a downward extension of the peritoneum and later obliterates leaving the tunica vaginalis (in males).
|
|
|
Wolffian duct.
|
The male reproductive system originates from the Wolffian duct.
|
|
|
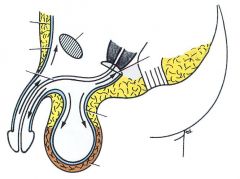
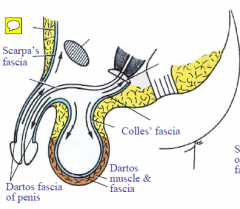
Scarpas Fascia
|
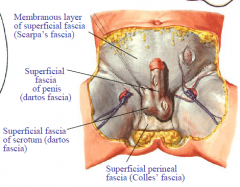
Scarpa’s fascia is continuous with Colles fascia, dartos fascia of penis and dartos fascia of scrotum.
|
|
|
Spermatic Cord Cntents
|
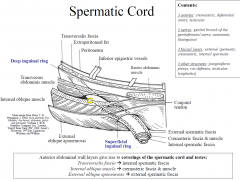
|
|

|
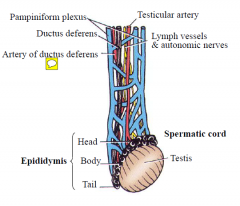
|
|
|
Testicular torsion
|
Testicular torsion cuts off blood supply to testis and epididymis testicular infarction (urgent surgery)
|
|
|
Epididymis
|
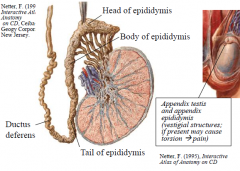
-maturation of sperm
-superior & posterior to testes -transmits sperm to the vas deferens |
|
|
Testis
|
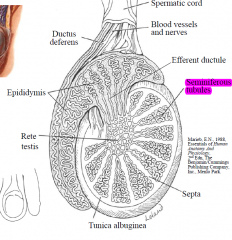
-Ovoid, mobile; 4 x 2.5 x 2 cm, 25g
-2 poles (superior, inferior), 2 surfaces (medial, lateral), 2 borders (anterior, posterior) -Thick outer covering (tunica albuginea) sends in septa dividing it incompletely into lobules -Sperm produced in walls of seminiferous tubules -Testosterone produced in interstitial cells (of Leydig) |
|
|
Neurovascular Supply: Scrotum vs. Testis
|
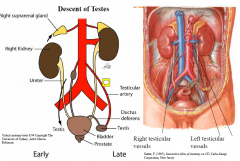
Neurovascular supply reflects early development; each testis descends into the scrotum and drags its blood supply with it
Testicular artery from abdominal aorta (below origin of renal arteries). Artery of ductus deferens (from internal iliac) supplies ductus deferens & provides collateral supply to the testis (both arteries are obstructed with testicular torsion) Testicular vein - from pampiniform plexus of spermatic cord Right testicular vein IVC Left testicular vein left renal vein (left pampiniform plexus more commonly forms varicocoele) Nerve supply to testis via sympathetic (T10 level spinal cord, descend as plexus on artery), probably mainly vasomotor |
|
|
lymphatic drainage of testis vs. scrotum
|
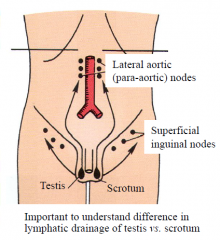
|
|
|
Scrotal Swellings
|
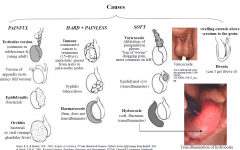
|
|
|
Appendix of testis
|
The appendix testis (or hydatid of Morgagni) is a vestigial remnant of the Müllerian duct, present on the upper pole of the testis and attached to the tunica vaginalis. It is present about 90% of the time.
|
|
|
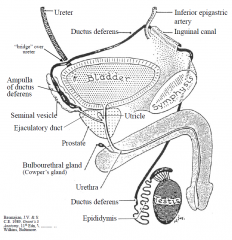
Ductus (vas) Deferens
|
-Carries spermatozoa from epididymis to ejaculatory duct
-45 cm long, smooth muscle, (sympathetic stimulation) -Starts at tail of epididymis -Runs in posterior part of spermatic cord, through deep inguinal ring (lateral to inferior epigastric artery) -Turns into pelvic cavity -Expands behind bladder as the ampulla of ductus deferens -Joins with duct of seminal vesicle to form ejaculatory duct |
|
|
|
|
|
Seminal Vesicles
|
-Contributes to seminal fluid
-5 cm long containing a tube ~15cm long folded on itself -Smooth muscle of wall contracts with sympathetic stimulation (emission) |
|
|
Ejaculatory duct
|
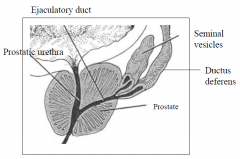
-Pathway by which sperm & seminal vesicle secretions reach urethra
-2-2.5cm long, passes through prostate close to median plane -Opens into prostatic urethra. |
|
|
Prostate Gland
|
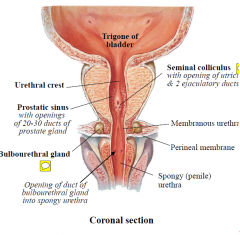
-Secretions contribute to seminal fluid, 20-30 ducts drain into prostatic sinus of prostatic urethra
-Firm, dense, fibromuscular gland, ~4cm long -Palpation (digital rectal exam): firm to palpation, triangular-shape posteriorly with median groove -Prostatitis – inflammation of prostate (often bacterial) tenderness to palpation |
|
|
Lobes of the prostate
|
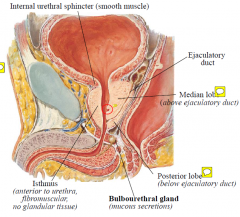
The prostate gland has 3 lobes. The isthmus is anterior to the urethra. The median lobe lies above the ejaculatory duct. The posterior lobe is the most common site of cancer.
|
|
|
Prostate Blood Supply
|
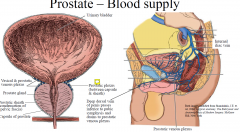
Arterial supply - branches of internal iliac artery
Venous drainage - prostatic venous plexus, around sides and base of prostate drains mainly to internal iliac vein. Also communicates posteriorly with internal vertebral venous plexus of Batson metastatic spread from prostate to vertebral column and elsewhere Lymphatic drainage - mainly to internal & external iliac nodes |
|
|
Bulbourethral gland
|
sits onto of the perineal memrbrane but its duct pierce the membrane and enters into the penile urthera
|
|
|
Complications of Prostatic Hyperplasia
|
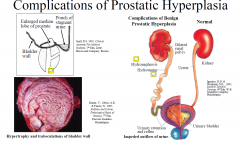
Prostatism
-Constellation of symptoms associated with bladder outlet obstruction: weak urinary stream, hesitancy, terminal dribbling, intermittency, sensation of incomplete bladder emptying, straining (at times) to urinate -Retention of urine can result in bacterial proliferation -Symptoms of irritation include urinary urgency, frequency, nocturia, and incontinence (at times) |
|
|
Penis
|
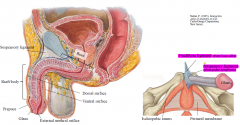
-Skin forms prepuce (foreskin) around glans; circumcision = removal of prepuce
-Frenulum is skin fold on ventral (urethral) surface -Phimosis - foreskin cannot be retracted over glans, Paraphimosis - foreskin cannot be brought back to original location -Parts: Root is the attached part (to ischiopubic ramus and perineal membrane) Body/shaft Is the free part (comprised of corpus spongiosum and paired corpora cavernosa) Glans penis |
|
|
How is penile enlargement surgery performed?
|
cut the suspensory ligament
|
|
|
Penis – Erectile Tissue
|
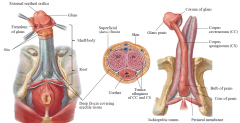
3 bodies of erectile tissue covered by deep fascia, superficial fascia and skin
Bulb of penis, continues as corpus spongiosum and enlarges distally as glans penis; it transmits the spongy urethra Left & right crus (attached to ischiopubic ramus and perineal membrane) continue in shaft as as the corpus cavernosum: they are connected distally too. Tunica albuginea surrounds the erectile tissue |
|
|
Penis – Associated Muscles
|
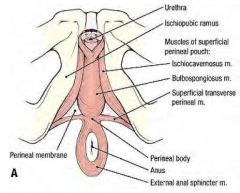
Bulbospongiosus
Ischiocavernosus |
|
|
Bulbospongiosus muscle
|
covers the bulb of the penis and aids in emptying residual urine & sperm. Contracts reflexly at ejaculation. Anterior fibres aid erection by compressing the deep dorsal vein
MAINTAIN: only! |
|
|
Ischiocavernosus
|
Ischiocavernosus muscle covers crura of penis, forces blood from crura into corpus cavernosum aiding in erection. It also compresses tributaries of the deep dorsal vein of the penis, thus restricting venous outflow from the penis and helping to maintain erection.
- MAINTAIN with tributaries - INITATE: push blood into cavernousum |
|
|
Penis – Arterial Supply
|
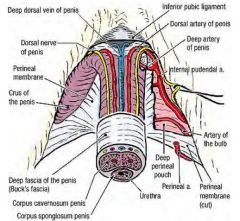
|
|
|
Penis – Arterial Supply
|
Arterial supply from internal pudendal artery; its branches form the deep artery which dilate in the corpora cavernosa in response to parasympathetic stimulation (relaxes smooth muscle in erectile tissue) blood fills cavernous spaces engorgement of corpora cavernosa
Main venous drainage of erectile tissue is via deep dorsal vein of penis which drains into prostatic venous plexus |
|
|
Penis Venous Drainage
|
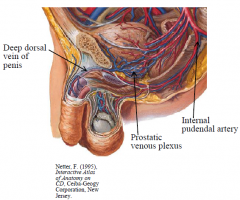
|
|
|
Nerve Innervation in Male
SENSORY |
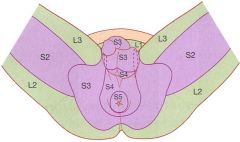
Sensory innervation to perineum is mainly via the pudendal nerve:
supplies skin of shaft and glans of penis supplies posterior 2/3 of scrotal skin (anterior 1/3 supplied by L1 level – ilioinguinal & genitofemoral nerves) |
|
|
Nerve Innervation in Male
MOTOR |
Motor supply to skeletal muscles in perineum also via pudendal nerve, including:
bulbospongiosus and ischiocavernosus muscles external anal sphincter and external urethral sphincter |
|
|
Nerves in males
|
|
|
|
Erection
|
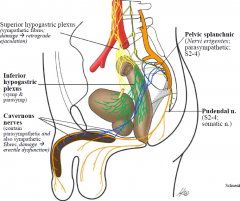
Erection (vasodilatation of aa. in corpora cavernosa) – parasympathetic (S2-4)
|
|
|
Emission
|
Emission (sperm & secretions to prostatic urethra) - smooth muscle contracts in epidid, dd, sv, & prostate to move sperm and seminal fluid into prostatic urethra– sympathetic (L1-2)
|
|
|
Ejaculation
|
(expulsion to exterior) – coordinated autonomic + somatic nn; internal urethral sphincter (smooth m.) contracts to prevent retrograde ejaculation into bladder (sympathetic L1-2); relaxation of external urethral sphincter & rhythmic contraction of bulbospongiosus m. (around bulb of penis) via pudendal nerve (somatic; S2-4)
|
|
|
Remission/Detumescence
|
(return to flaccid state) – vasoconstriction of helicine arteries in erectile tissue – sympathetic nn.
|
|
|
Composition of seminal fluid
|
Composition of seminal fluid (2-5ml ejaculate) ~ 65-75% seminal vesicle secretions,
~ 25-30% prostatic secretions, ~ 2-5% testes (200-500million spermatazoa). |
|
|
Pre-Ejaculate
|
Bulbourethral glands (pre-ejaculate) – mucus-like
|
|
|
Peyronies Disease
|
plaques, strands of dense fibrous tissue in corpus cavernosum producing curvature of penis (especially in the erect state)
|

