![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
308 Cards in this Set
- Front
- Back
|
What is the percent of incidence of breast cancer in each region of the breast?
|
• Upper outer - 50%
• Nipple - 18% • Upper inner - 15% • Lower outer - 11% • Lower inner - 6% |
|
|
What part of the breast tissue is the most common site of breast cancer?
|
• Tail of Spence - part of the upper outer breast tissue extending into axillae
|
|
|
What are the three tissue type of the breat?
|
• Adipose tissue - majority of the breast tissue
• Glandular tissue - secretes milk • Suspensory or Cooper's ligaments - fibrous bands that attach breast tissue to chest wall muscles |
|
|
How does breast cancer effect the suspensory ligaments of the breast?
|
Cancer may cause the ligaments to contract, causing pits or dimples in the overlying skin
|
|
|
Name the location and drainage area of the regional lymph nodes around the breasts.
|
• Pectoral - behind anterior axillary fold, drains anterior chest wall and breast
• Subscapular - located along lateral edge of the scapula just inside posterior axillary fold, dains posterior chest wall and arm • Lateral - along the humerus inside the upper arm, drains the arm • Central axillary - high middle axillae, drains all axillary nodes |
|
|
Where does the lymph drainage of the breast go?
|
• 75% of drainage goes to infraclavicular and supraclavicular nodes on the SAME side
• 25% of drainage will go to the OPPOSITE breast, abdomen, or deep into breast – a problem for metastatic disease, increases spread to the other side |
|
|
What are the developmental considerations regarding breasts in the newborn?
|
Estrogen causes white nipple fluid in both sexes, but it resolves in few days to few weeks
|
|
|
What are the developmental considerations regarding breasts in the adolescent?
|
• Estrogen stimulates breast development
• Breast development – onset 8-8.5 to 13 years, average 10 – 11, duration of 3 years • Precocious (before 8y/o) or delayed (after 13.5y/o) puberty needs an endocrine evaluation • Breasts may normally be asymmetric – teen may need reassurance |
|
|
What are the developmental considerations regarding breasts in the pregnant female?
|
• Nipples enlarge, darken, and become more erect
• Increased venous pattern over skin (superficial vessels) • Elevated Montgomery glands • Colostrum forms in the 4th month – precursor to milk, thick yellow fluid |
|
|
What are the developmental considerations regarding breasts in the lactating female?
|
• Colostrum changes to milk 3 days postpartum
• Frequent nursing relieves sensation of tenderness, engorgement • Mastitis – inflammation or infection of breast tissue after childbirth; red, swollen, hot, painful, breasts |
|
|
Mastitis
|
• inflammation or infection of breast tissue after childbirth
• red, swollen, hot, painful, breasts |
|
|
What are the developmental considerations regarding breasts in the aging female?
|
• Menopause – glandular tissue atrophies, decreased breast size
• Decreased elasticity – related to decreased adipose, causes pendulous, flattened, sagging breasts • Axillary hair decreases |
|
|
Gynecomastia
|
• nub of breast tissue under areola, feels like a large grape
• Adolescence males - normal, unilateral, temporary, excess testosterone converted to estrogen • Elderly males - normal, unilateral or bilateral, testosterone drops and estrogen is unopposed, possibly from • Possibly due to medication effects (Cimetadine) or a pituitary tumor |
|
|
What is the lifetime risk of breast cancer in females and males?
|
• Females - 1 in 8
• Males - 1 in 1,000 |
|
|
Fibrocystic Lumps
|
• Non-cancerous
• May enlarge and become more tender prior to the menstrural period or with caffeine |
|
|
Types of Nipple Discharge
|
• Always needs evaluation, possibly via prolactin levels
• Clear discharge – may be due to a pituitary tumor or meds • Galactorrhea – milky discharge, associated with a pituitary tumor • Bloody discharge or thick yellow with blood – always significant, especially when associated with a lump, may indicate ductal cancer |
|
|
Paget's disease
|
• Advanced ductal cancer
• starts as a small crust on the nipple with surrounding erythema |
|
|
Mammograms
|
• Women with breast implants and males can get mammograms
• Young women don’t get mammograms b/c tissue is too dense for scan to mean anything • 10% failure rate – 10% of the time, it won’t find breast cancer when it’s present • Recommended yearly starting at age 40 |
|
|
How often is recommended to receive a clinical breast exam?
|
• 20-30 years old – very 3 years
• 40+ years old – yearly |
|
|
Self Breast Exam
|
• Perform 5-7 days after onset of menses - decreased nodularity
• The most nodularity occurs mid-cycle until the last half of the cycle • Postmenopausal – examine at same time each month |
|
|
Risk Factors of Breast Cancer
|
• Female – 100 x more common in female than males
• Age – 1 in 8 before age 45 and progressively increases with age • Breast cancer in one breast – increases risk 3-4 x in other breast • Abnormal breast cells on previous biopsy • Family History – especially if occurrence before age 50 and/or in 1st degree relative, seen in 20-30% of incidences • BRACA 1 or BRACA 2 – these gene mutations are also a risk factor for men • Radiation to chest – especially if before age 30; treatment for Hodgkin’s lymphoma • Current use of oral contraceptives • First child after 30-35 y/o • Never having a child or breast fed • Menses before age 12, menopause after age 55 • Hormone replacement therapy (HRT) – estrogen and progesterone • Caucasian • Mammograms showing dense tissue – more glandular, less fat • Overweight or obese, physical inactivity • Alcohol – over one drink per day increases risk x1-1.5 • DES exposure (diethylstilbesterol) in persons taking it and their daughters (1940s anti-miscarriage drug) |
|
|
Peau d'Orange
|
• Orange peel skin
• Caused by blocked lymph ducts • Common with Cancer • Edema may exaggerate hair follicles causing bumpy texture and large pores appearing like an orange peel |
|
|
How does breast cancer change the appearance of nipples?
|
• Asymmetry
• Inverted nipples - change from normal and/or unilateral • Dry scaling, fissures, ulcerations, bleeding |
|
|
Supernumerary nipple
|
• Two nipples along the mammary ridge at the mid-clavicular line
• Occurs in 1% of men and women • Appears like a nevus (mole) |
|
|
Retraction Maneuvers
|
• Observe changes in contour, symmetry, retraction, and dimpling
• Hands at side • lift arms overhead • Push hands on hips • Push palms together • Lean forward |
|
|
Clinical Breast Exam
|
• Use a bimanual technique to palpate breast, especially for women with larger breasts
• Place pillow or towel roll under shoulder of side to be examined • Have patient place hand behind head on side to be examined • Palpate in vertical strips using pads of 3 fingers from the mid-axillary line to the sternal border, including Tail of Spense – never raise fingers, may miss a spot • Premenstrual – breasts are engorged due to estrogen, feels fuller, more nodular • Use same examination technique for those who have had surgical procedures, mastectomy, breast augmentation • Assess the nipples for lumps, discharge, and color • Inspect the supraclavicular and infraclavicular areas |
|
|
Galactorrhea
|
• Lactation when not breast feeding, usually due to a pituitary tumor
|
|
|
Characteristics of Breast Lumps
|
• Location – quadrant, cm from nipple, clock position (i.e. 3 o’clock position)
• Size – length, width, depth • Shape – round, oval, indistinct • Consistency – soft, hard, firm • Tenderness • Borders – defined, irregular • Retraction/dimpling – present or absent • Mobility – mobile indicates fibrocystic, fixed indicates cancer |
|
|
Five Key Clinical Characteristics of Breast Cancer
|
• painless
• ulceration • fixed • retraction • nipple discharge |
|
|
Dizziness vs Vertigo
|
• Dizziness = lightheadedness; unsteadyness
• Vertigo = true rotational spinning, problem w/ cerebellum or inner ear, sense of movement, whirling sensation, staggering gait |
|
|
Paresthesia
|
• Decreased sensation
• Numbness, tingling |
|
|
Paresis
|
• Weakness
• Neurologic motor problem |
|
|
Four Causes of Lumps/Swelling in the Neck
|
• Recent injury, infection – tonsillitis, dental infection, eye infection
• Throat cancer – increased cancer risk with alcohol and smoking • Oral cancer – increased cancer risk with smokeless tobacco and pipes • Environmental exposure – radiation, toxic chemicals • Thyroid problems – goiter, cancer |
|
|
Dysphagia
|
• Difficulty swallowing
|
|
|
How does HYPERthyroidism affect the following systems:
• Cardiovascular • Gastrointestinal • Integumentary • Neurological • Heat tolerance • Weight |
• Cardiovascular – Tachycardia
• Gastrointestinal – Diarrhea • Integumentary – Fine, silky, soft hair • Neurological – Nervousness • Heat tolerance – Hot • Weight – Weight loss |
|
|
How does HYPOthyroidism affect the following systems:
• Cardiovascular • Gastrointestinal • Integumentary • Neurological • Heat tolerance • Weight |
• Cardiovascular – Bradycardia
• Gastrointestinal – Constipation • Integumentary – Dry skin, brittle hair • Neurological – Fatigue • Heat tolerance – Cold • Weight – Weight gain |
|
|
What are the developmental considerations regarding the face in the child?
|
• Habits of mother (alcohol, drugs), delivery problems
• Fetal Alcohol Syndrome • Developmental milestones – is the child's growth on schedule? |
|
|
How do you document inspection and palpation of a normal head?
|
• Normocephaic – round and symmetric head
• NCAT – normocephalic, atraumatic |
|
|
Bones of the Face
|
• Fused bones, non-moveble joints
• Frontal • Zygomatic • Lacrimal – eye orbit • Sphenoid – behind eye • Maxilla • Mandible - only moveable joint of skull, connects to temporal bone at Temporal Mandibular Joint (TMJ) |
|
|
Seizures
|
• Sudden, excessive electrical discharge in brain
|
|
|
Syncope
|
• Temporary unconscious event
• Aka fainting |
|
|
Goiter
|
• Thyroid gland enlargement
• Associated with HYPERthyroidism • Check for convex, protruding base of neck – when the thyroid enlarges, it protrudes anteriorly since it can't grow posteriorly |
|
|
Cataracts
|
• Opaque lens in eye
|
|
|
Diplopia
|
• Double vision
|
|
|
Epiphora
|
• Excessive tearing or watering of the eye
• May be due to irritants, allergies, infection, or obstruction of lacrimal ducts |
|
|
Floaters
|
• Temporary, translucent protein fragments in visual field
|
|
|
Glaucoma
|
• Increased intraocular pressure (IOP) that causes atrophy of the optic nerve
• Results in loss of peripheral vision, night blindness |
|
|
Hyperopia
|
• Far-sightedness
|
|
|
Macular Degeneration
|
• Loss of pigmentation at the visual focus of the retina
• Loose center of visual field, but keep peripheral |
|
|
Myopia
|
• Near-sightedness
|
|
|
Presbyopia
|
• Permanent loss of near-sighted focus
• Decreased power of accommodation with aging – decreased ability of the lens to change shape to accommodate for near vision |
|
|
Photophobia
|
• Eye's intolerance of or pain from light
|
|
|
Ptosis
|
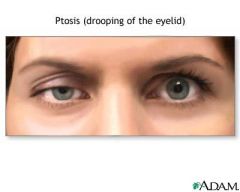
• Drooping of upper eyelid
• May involve CN 3, 5, and/or 7 |
|
|
Scotoma
|
• Black spot in visual field
• Seen in glaucoma, visual pathway disorders |
|
|
Palpebral Fissure
|
• Space between upper and lower eyelid
• Upper lid covers part of the iris when eyes are open • Lower lid is at the limbus – border between cornea and sclera |
|
|
Nasolabial Fold
|
• Fold from nose to mouth
• Asymmetric or absent w/ stroke |
|
|
Deafness
|
• Loss of hearing
|
|
|
Otalgia
|
• Ear pain or ache
• May be referred from teeth, throat, TMJ • Sinus problems and upper respiratory infection – microorganisms may migrate from nose to middle ear via eustachian tube, which explains why colds are often associated with ear infections |
|
|
Otitis externa
|
• Infection or inflammation of the external ear
• Gentle movement of pinna and press on tragus causes pain • Watery discharge, sometimes serosanguineous or pruritic • Commonly due to pseudomonus and fungus • Aka swimmer's ear |
|
|
Otitis media
|
• Infection or inflammation in middle ear or tympanic membrane
• Press on mastoid (mastoiditis) causes pain • Bright red TM, loss of landmarks • Increased incidence of otitis media in Native Americans, Alaskan, Canadian Eskimos, Downs syndrome, bottle feed babies (lying down with bottle increases reflux through eustachian tube to middle ear), premature infants |
|
|
Tinnitus
|
• Ringing, buzzing, whistling in ear
• Often first sign of hearing loss • Worse at night – described as "white noise" when room is quiet |
|
|
Allergies
|
• Immune reaction to foregin antigens
• Seasonal rhinitis |
|
|
Allergic Rhinitis
|
• Pale Mucosa
• Assc. w/ itchy eyes, sneezing, etc. • Look for allergic salute in children |
|
|
Epistaxis
|
• Nose bleed
|
|
|
Post nasal drip
|
• Sinus drainage down back of throat
|
|
|
Rhinorrhea
|
• Runny nose
• Clear nasal discharge |
|
|
Sinusitis
|
• Inflammation of sinus
|
|
|
Bruxism
|
• Grinding of teeth
|
|
|
Caries
|
• Gradual decay of a tooth
• Aka cavity |
|
|
Hoarseness
|
• Rough quality a voice
|
|
|
How does Parkinson's disease affect facial expression?
|
• Mask-like facial expression
|
|
|
Hirsutism
|
• Excessive facial hair due to an endocrine problem
|
|
|
Sensory Assessment of Cranial Nerve 7 (Facial)
|
• Test sweet and salty to anterior 2/3 of tongue
|
|
|
What is TMJ? What is the clinical assessment for TMJ disorder?
|
• Temporal Mandibular Joint
• Anterior to tragus of ear • Inspect while opening and closing mouth – abnormal if opens in a zig zag pattern • Palpate while opening and closing mouth - abnormal if pain, crepitus, disrupted, decreased ROM, locking • Caused by bruxism • NURSES have the highest incidence of TMJ disorder |
|
|
What are the three salivary glands called?
Where are they located? What is each duct called? |
• Parotid gland – embedded in cheeks over mandible, anterior and inferior to ear; Stenson's duct in cheek
• Submandibular – beneath mandible at the angle of the jaw; Wharton's duct at each side of frenulum under tongue • Sublingual – located on the floor of the mouth; many small, non-visible openings along sublingual fold of tounge |
|
|
What is the function of the salivary glands?
|
• Secrete saliva containing salivary amylase (ptyalin) to start digestion
|
|
|
What is the vertebral prominens?
|
• C7 vertebrae
• Felt when head is flexed • If a second bump is felt, that's T1. That is not the vertebral prominens. |
|
|
In relation to the Sternocleidomastoid muscle, where are the carotid artery, internal jugular vein, and external jugular vein?
|
• Carotid and internal jugular - beneath SCM muscle
• External Jugular - above, on top of SCM muscle |
|
|
What are the accessory muscles of respiration in the neck?
What does an enlargement of these accessory muscles indicate? |
• Sternocleidomastoid muscle (SCM) – rotates the head side to side
• Trapezius – shrugs the shoulders, rotates the head to the side, extends head backward • Enlargement of accessory muscles indicate a breathing disorder, difficulty breathing |
|
|
What are the "two triangles" in the neck?
|
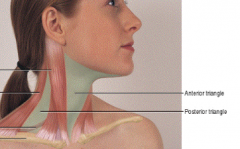
• Anterior Triangle - formed by the anterior aspect of both SCM muscles and the line of the jaw
• Posterior Triangle - formed by the posterior aspect of the SCM muscle, the anterior aspect of the trapezius, and the superior aspect of the clavicle • There is only one Anterior Triangle, found on the front of the neck. There are two Posterior Triangles, one on each side of the neck. |
|
|
What are the midline neck structures in descending order?
|
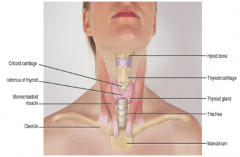
• Hyoid bone – at floor of mouth
• Thyroid cartilage – prominent notch, aka Adam’s apple • Cricoid cartilage – aka upper tracheal ring, site of emergency cricoidotomy • Thyroid gland – endocrine gland • Tracheal rings |
|
|
What two hormones does the thyroid gland secrete? What is main function of these hormones?
|
• T3 – triiodothyronine
• T4 – thyroxine • Main function of T3 and T4 – metabolic rate |
|
|
What is the basic anatomy/structure of the thyroid gland?
|
• Contains two lobes and an isthmus
• Shaped like a butterfly • Each lobe is 5cm x 3cm x 2cm (ht, width, depth) |
|
|
What does asymmetry of the midline neck structures, especially the trachea and SCM muscles, indicate?
|
• Tension Pneumothorax
• Pulls midline neck structures to the good, unaffected side |
|
|
Normal Neck Range of Motion
|
• Stop for pain, movements should be smooth and controlled
• Flexion (head to chin, nod "yes") = 45 degrees • Lateral flexion (ear to shoulder) = 40 degrees • Rotation (turn right and left, shake "no") = 70 degrees • Extension (backwards, look to ceiling) = 55 degrees |
|
|
How do you assess a traumatic neck injury?
|
• Do not manipulate or examine the cervical spine
• Stabilize the spine until further evaluation can be performed |
|
|
What is the immune/lymph function of the spleen?
|
• Produces antibodies
|
|
|
Where are the thymus, tonsils, and adenoids located?
|
• Thymus – located in chest
• Tonsils – located in the throat • Adenoids – located in the nasopharynx |
|
|
What is a Peyer's patch?
|
• An accumulation of lymph tissue in the intestines
|
|
|
What is the immune/lymph function of the bone marrow?
|
• Produces WBCs
|
|
|
All tissue supplied by blood vessels have lymph vessels except ______, _____, and ______.
|
• Cornea of the eye
• CNS • Placenta |
|
|
What is the basic function of lymph system?
|
• Lymph vessels collect interstitial fluid that surrounds the cells and drain into specific nodes
• Lymphocytes within lymph nodes filter and engulf bacteria, RBCs, toxins, microorganisms, and abnormal/Cancerous cells |
|
|
Where does the drainage of the lymph system enter the circulatory system?
|
• Right side of body (right head and neck, right arm, thorax, lungs and pleura, heart, and upper liver) drains into the Right Lymphatic Duct, which drains into the Right Subclavian Vein
• Rest of the body drains into the Thoracic Duct, which drains into the Left Subclavian Vein • That means if an abnormal cell (infectious, Cancerous) gets past lymph node, it will eventually enter the circulatory system and disperse throughout the body (i.e. metastatic Cancer) |
|
|
What four areas of the lymph system are accessible for inspection and palpation?
|
• Head and neck – majority (~75 nodes on each side)
• Arms • Axillae • Inguinal |
|
|
Where are the superficial and deep lymph nodes located?
|
• Superficial nodes – lie in sub-q tissue; may be palpable
• Deep nodes – lie in muscle, fascia or body cavities; non-palpable |
|
|
What does the consistency and mobility of the lymph nodes tell the examiner?
|
• Soft, mobile nodes are typical of infection
• Firm/hard, fixed nodes are typical of Cancer |
|
|
What does tender lymph nodes indicate?
|
Infection
|
|
|
Lymphadenopathy
|
• Enlarged lymph nodes over 1 cm
• Malignancy – hard, fixed, unilateral, nontender node • Infection – bilateral, mobile, warm, tender nodes • Allergies |
|
|
How do you palpate the lymph nodes?
|
• Use systematic approach to prevent missing any areas
• Touch lightly with fingertips – excessively hard pressure may compress nodes into underlying tissue, making them inaccessible • Palpate bilaterally to compare the two sides • Palpate the deep cervical nodes by bending ipsilaterally (same side) to relax muscles • Assess for supraclavicular nodes – hunch shoulders to relax muscles, allowing you to slip fingers behind clavicle |
|
|
Why is it important to assess the supraclavicular lymph nodes?
|
• Supraclavicular nodes are in a metastatic site, so enlargement here may indicate a neoplasm in the thorax, breast or abdomen
|
|
|
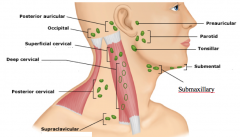
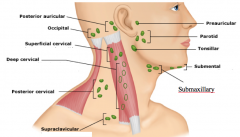
Name the location and area of drainage of this lymph node: Preauricular
|
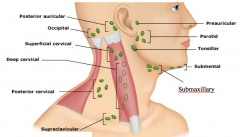
• Location – anterior to tragus of ear
• Drainage – scalp, forehead, lateral eyelids, eyes, upper face and external auditory canal • Ex – adenopathy with eye infection |
|
|
Name the location and area of drainage of this lymph node: Postauricular
|
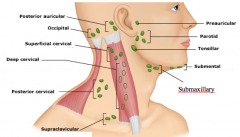
• Location – behind ear on mastoid process
• Drainage – parietal area of scalp and external auditory canal • Ex – adenopathy with otitis externa |
|
|
Name the location and area of drainage of this lymph node: Occipital
|
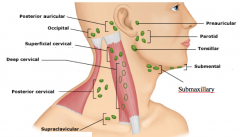
• Location – base of the skull
• Drainage – parietal region of scalp • Ex – adenopathy with scalp lesion |
|
|
Name the location and area of drainage of this lymph node: Submental
|
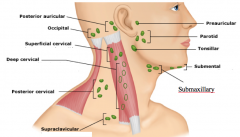
• Location – midline, behind the tip of the mandible
• Drainage – outh, lips and tongue • Ex – adenopathy with oral cancer |
|
|
Name the location and area of drainage of this lymph node: Submaxillary (aka Submandibular)
|
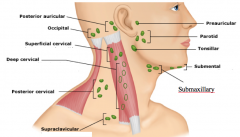
• Location – half way between jaw angle and tip of mandible
• Drainage – lips, mouth, tongue, and submaxillary glands • Ex – adenopathy with oral cancer |
|
|
Name the location and area of drainage of this lymph node: Tonsillar (aka retropharyngeal, jugulodigastic)
|
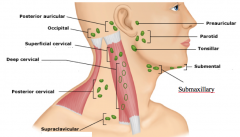
• Location – at the angle of the jaw
• Drainage – eyelids, frontotemporal skin, external auditory meatus, tympanic cavity, tonsils, posterior palate, floor of mouth and thyroid • Ex – adenopathy with tonsillitis |
|
|
Name the location and area of drainage of this lymph node: Superficial Cervical (aka Anterior Cervical)
|
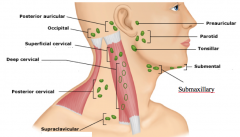
• Location – overlying the SCM muscle
• Drainage – skin of ear and neck |
|
|
Name the location and area of drainage of this lymph node: Deep Cervical Chain
|
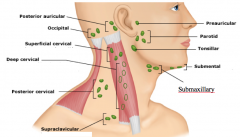
• Location – under the SCM muscle
• Drainage – ear, larynx, thyroid, trachea and upper part of esophagus • Ex – adenopathy with laryngeal cancer |
|
|
Name the location and area of drainage of this lymph node: Posterior Cervical Chain
|
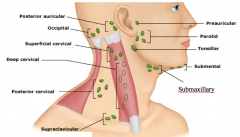
• Location – in the posterior triangle along the edge of the trapezius muscle
• Drainage – posterior scalp, posterior skin of neck and thyroid • Ex – adenopathy with thyroid cancer, mononucleosis |
|
|
Name the location and area of drainage of this lymph node: Supraclavicular
|
• Location – above and behind the SCM muscle
• Drainage – upper abdominal, lungs, breast and arm • Important to rule out neoplasm – adenopathy here is usually really bad |
|
|
What are the developmental considerations regarding the head and neck in the newborn and infant?
|
• Record head circumference up to 2 y/o
• Be aware of the fontanels of the fetal skull |
|
|
What is the function of the fetal skull's fontanels?
What are the shapes and closure ages of the fetal skull's fontanels? |
• Fontanels allow for growth
• Posterior fontanel – triangle shape, closes at 2 months • Anterior fontanel – diamond shape, closes at 24 months |
|
|
Craniocynostosis
|
• Premature closure of one or more cranial sutures while brain growth continues
|
|
|
What do sunken fontanels in a fetal skull indicate?
What do buldging fontanels in a fetal skull indicate? |
• Sunken fontanels – Dehydration
• Buldging fontanels – increased Intracranial Pressure |
|
|
What are the developmental considerations regarding lymphadenopathy in the child?
|
• Lymphadenopathy is common with minor infection
|
|
|
What are the developmental considerations regarding the lymph system and the head/neck in the pregnant female?
|
• Chloasma – facial discoloration
• Palpable thyroid is normal |
|
|
What are the developmental considerations regarding the head/neck in the aging adult?
|
• Change in the curve of the neck to compensate for kyphosis
• Prominent facial bones due to decreased tissue elasticity |
|
|
Lymphedema
|
• Excessive collection of fluid in the interstitial spaces due to blocked or infected lymphatic channels
• Acquired secondary to lymph duct trauma – surgery or metastasis • Congenital (Milroy disease) – mal-development of the lymph system • Never take BP, give injection, or draw blood in this area due to compromised local immune system |
|
|
Acute Lymphangitis
|
• Inflammation of lymph vessels usually 2o to strep infection of an extremity
• S/S – red streaks extending to axilla or groin, fever, chills |
|
|
Acute Lymphadentitis
|
• Inflammation of lymph nodes, secondary to systemic neoplastic disease (Cancer), bacterial infection, or other inflammatory condition
• S/S – enlarged, tender, firm nodes, surrounding edema, erythema • Ex – cat scratch disease |
|
|
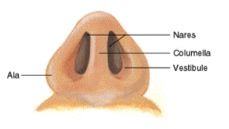
Locate on the nose:
• Ala • Vestibule • Columella • Nares |
|
|
|
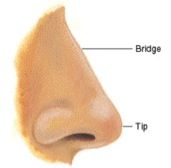
Locate on the nose:
• Bridge • Tip |
|
|
|
What are the two types of hair in the nose? Why is it dangerous to pluck nose hairs?
|
• Vibrissae – coarse hairs that line anterior edge of nose
• Ciliated mucous membrane - hair-like structures that lines the remainder of the nasal cavity and filters fine dust and bacteria • Plucking nasal hairs may result in brain abscess – nose is direct pathway to brain |
|
|
Kiesselbach's Plexus
|
• Anterior portion of nasal septum
• Common site for nosebleeds (aka epistaxis) |
|
|
Locate the following lymph nodes of the head and neck:
• Preauricular • Postauricular • Occipital • Submental • Submaxillary (aka submandibular) • Tonsillar (aka retropharyngeal, jugulodigastic) • Superficial cervical (Anterior cervical) • Deep cervical chain • Posterior cervical chain • Supraclavicular |
|
|
|
Nasal Turbinates
|
• Located on the lateral walls of each nasal cavity
• Superior, middle & inferior turbinates – 3 bony projections covered by mucous membrane • Superior never visible, middle and inferior may be visible • Increases surface area to warm, humidify & filter air |
|
|
Nasal Meatus
|
• Cleft under each turbinate
• Sinuses drain into middle meatus – sinusitis may occur if duct is blocked • Sinus openings are narrow & occlude easily • Nasolacrimal duct drains into inferior meatus |
|
|
Olfactory Receptors
|
• Aka hair cells
• Positioned in roof of nasal cavity and upper third of septum • Receptors transmit sensation to the olfactory nerve (CN I) and to temporal lobe of brain |
|
|
Sinuses
|
• Four sets - mxillary, frontal, ethmoid, sphenoid
• Air filled pockets in skull bones • Helps to resonate sound • Provides mucus to drain into nasal cavity, keeps nares moist) |
|
|
Vermilion Border of Lips
|
• Outer edge of lips
• Transition from outer skin to inner mucous membranes |
|
|
What are the two sections of the roof of the mouth?
|
• Hard palate – anterior, mucous membrane over bone, whitish, behind front teeth
• Soft palate – posterior, mucous membrane over muscle, pink, soft, mobile |
|
|
Parts of the Tongue
|
• Dorsal Surface – contain papillae, with taste buds surrounding the paillae
• Ventral surface - shinny with prominent veins • Frenulum - connects tongue to floor of mouth |
|
|
Teeth and Gums:
• Parts of the tooth • Number of permanent and deciduous teeth |
• The tooth consists of crown, neck, and root
• 32 permanent teeth – 16 teeth in each arch, including 3rd molars (wisdom teeth) • 20 deciduous (baby) teeth – erupt between 6 mo and 30 mo, lost between 6 and 12 y/o starting with central incissors • Gingiva (gums) - thick fibrous tissue covered with mucous membranes |
|
|
Oropharynx
|
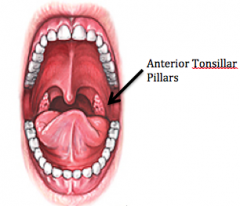
• Anterior tonsillar pillars separate mouth from oral pharynx
• Contains the palatine tonsils – lymphoid tissue, appear granular with deep crypts, located between anterior and posterior pillars |
|
|
Nasopharynx
|
• Above oropharynx, behind nasal cavity
• Contains the pharyngeal tonsils (aka adenoids) and the eustachian tube outlet |
|
|
Anosmia
|
• Loss of sense of smell
• Can be either a nose receptor problem or a brain problem • Can be due to smoking, cocaine, rhinitis, temporal lobe lesion |
|
|
Allergic Salute
|
• Crease on top of nose
• Caused by repetitive wiping upward of nose due to allergies |
|
|
What are the clinical manifestations of a foreign body occlusion in the nose?
|
• Purulent, unilateral discharge
• No Upper Respiratory Infection (URI) symptoms |
|
|
Nasal Septum Deviation
|
• Asymmetric nares
• Due to trauma → septum deviates toward smaller nares |
|
|
Nasal Septum Perforation
|
• Shine light in one nares and look for light on other side
• related to cocaine use and chronic nose picking |
|
|
Nasal Polyps
|
• Smooth
• Pale gray • Avascular • Mobile • Common with allergies • Often found in middle meatus |
|
|
What does pallor and cyanosis of the lips indicate?
|
• Pallor – anemia
• Cyanosis – central hypoxia |
|
|
Cheilosis
|
• Aka angular stomatitis
• Cracking at the corners of the mouth • May be caused by riboflavin and niacin deficiency |
|
|
Clinical Manifestations of Oral Herpes Simplex
|
• Aka cold sore, fever blister
• Viral lesion that may break the vermilion border • Exacerbations with stress |
|
|
What conditions are associated with loss of tooth enamel?
|
• Bruckism
• Bulemia |
|
|
What causes the following teeth discolorations:
• Brown teeth • Yellow teeth • Dark Brown |
• Excessive fluoride
• Tobacco • Tetracycline during last trimester |
|
|
Maloclusion
|
• Misalignment of teeth, bad bite
• Upper teeth should protrude slightly over lower teeth • Often related to sucking thumb |
|
|
Gingivitis
|
• Swelling, hypertrophy of gums
• Usually related to poor dental hygiene • Major cause of tooth loss |
|
|
Gingival Hyperplasia
|
• Overgrowth of gum tissue
• Cause by pregnancy, puberty, leukemia, long use of Dilantin |
|
|
What does a smooth, glossy tongue indicate?
|
• Iron, B12, or folic acid deficiency
|
|
|
Leukoplakia
|
• white patch on tongue
• non-painful precancerous lesion • does NOT scrape off |
|
|
Candidiasis
|
• Aka monilial infection, or thrush
• Antibiotics may destroy normal bacterial flora, causing a proliferation of fungus • Fungus may cause white cheesy patches or black hairy tongue • Does scrape off |
|
|
What effect can bismuth (PeptoBismal) have on the tongue?
|
• May cause blackened tongue
|
|
|
Aphthous Ulcers
|
• Aka canker sores
• Cause unknown – may be acidic food, autoimmune |
|
|
Torus Palatinus
|
• Common, midline bony ridge in hard palate
• Normal finding, insignificant • More common in Native American and Asians |
|
|
Cleft Lip/Cleft Palate
|
• Incomplete fusion of maxillary process
• Affects sucking • More common in Native American and Asians |
|
|
Bifid Uvula
|
• Partial or complete split of uvula
• Not significant, but contributes to snoring • More common in Native Americans and Asians |
|
|
Grading Scale for Tonsil Size
|
1+ barely visible
2+ halfway to uvula 3+ touching or nearly touching uvula 4+ touching each other |
|
|
What are the S/S of acute tonsillitis?
|
• Bright red, swollen tonsils, with exudate
• May occlude airway |
|
|
What does tonsilar exudate or large white spots possibly indicate?
|
• Mononucleosis
• Leukemia • Diphtheria |
|
|
Assessment of Cranial Nerves 9 (Glossopharyngeal) and 10 (Vagus)
|
• Test the gag reflex – press on tongue or posterior oral pharynx
|
|
|
Halitosis
|
• Bad breathe odor
|
|
|
Choanal Atresia
|
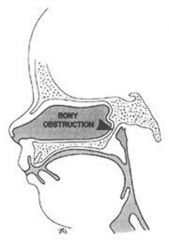
• Congenital bony or membranous septum between nose and pharynx
|
|
|
Ankyloglossia
|
• Impaired mobility of tongue due to a short frenulum
• May impair speech, “tongue tied” |
|
|
At what age does the nose develop in females and male?
|
• Females - around 10 y/o
• Males - around 18 y/o |
|
|
What are the developmental considerations regarding the nose and gums in the pregnant female?
|
• Nasal stuffiness and epistaxis – very common, due to increased vascularity
• Gums may normally hypertrophy – may bleed with normal brushing |
|
|
What are the developmental considerations regarding the nose and mouth in the aging adult?
|
• Larger appearing nose – due to decreased elastic and sub-Q tissue
• Longer nasal hairs • Decreased sense of smell – begins as early as 6th and 7th decades (50s and 60s) • Xerostomia • Receding gums • Teeth may be worn down • Tooth loss – some bony reabsorption • Malocclusion due to tooth loss – the opposing tooth with move up, causing altered bite • TMJ arthritis |
|
|
Xerostomia
|
• Dry mouth
• Often due to medications – diuretics, antihistamines, antidepressants, antipsychotics • Also caused by dehydration |
|
|
What disease causes central visual field loss?
What disease causes peripheral visual field loss? |
• Central – macular degeneration
• Peripheral – glaucoma |
|
|
What do "halos around lights" in the visual field possibly indicate?
|
• Acute narrow angle glaucoma
• Digoxin toxicity |
|
|
What does night blindness possibly indicate?
|
• Optic atrophy – age related
• Glaucoma • Vitamin A deficiency |
|
|
Strabismus
|
• Eye cannot point in same direction, cross eyed
• Includes esotropia and exotropia |
|
|
What does redness or swelling of the eye possibly indicate?
|
• Infection
• Allergies • Dryness • Mechanical – i.e. foreign body |
|
|
How can a vaginal infection in the mother affect the infant's eyes during child birth?
|
• Vaginal infection in the mother can transfer to the infant's eyes during child birth
• I.e. gonorrhea, herpes |
|
|
How does Diabetes Mellitus, hypertension, and hyperthyroidism affect the eyes?
|
• Diabetes Mellitus – diabetic retinopathy, leading cause of blindness
• Hypertension – when uncontrolled, hypertensive retinopathy • Hyperthyroidism – changes eye size and shape, lids may not close tightly |
|
|
How does the chronic use of steroids affect the eyes?
|
• Chronic use of steroids, often used for chronic inflammatory diseases, can cause premature cataracts
|
|
|
What do the following abbreviations mean:
• OD • OS • OU |
• OD – Oculus Dexter, right eye
• OS – Oculus Sinister, left eye • OU – Oculus Unites, both eyes • These abbreviations are no longer used in the hospital b/c of miscommunications |
|
|
What is the difference between:
• Ophthalmologist • Optometrist • Optician |
• Ophthalmologist – medical doctor
• Optometrist – highly train, not a MD • Optician – technician, fills Rx, not a MD |
|
|
What visual acuity is considered normal?
What visual acuity is considered legally blind? |
• Normal – 20/20
• Legally blind – 20/200 after correction |
|
|
How is visual acuity for far vision tested?
How is visual acuity for near vision tested? |
• Far vision – Snellen chart from a 20 ft distance, test each eye individually
• Near vision – Jaegar, Rosenbaum, newsprint, etc. |
|
|
How is visual acuity documented?
|
• What can you see at 20 ft / Distance the normal or average eye can see the same thing
• Ex – 20/20 means what you can see at 20 ft, the normal or average eye can also see at 20 ft • Ex – 20/50 means what you can see at 20 ft, the normal or average eye can see at 50 ft |
|
|
Do you test vision with or without vision correction (glasses, contacts)?
|
• To determine level of visual acuity, test without vision correction
• To determine how well the vision is corrected, test with vision correction |
|
|
How do you test peripheral vision?
|
• Confrontation test
• Face patient, 2 ft away • Assess when patient can see finger at periphery • Test each eye individually for all fields |
|
|
How do you document a normal eye exam?
|
• Visual fields are full by confrontation, no field cuts, CN 2 intact
|
|
|
Extraocular Muscles (EOMs)
|
• Six muscles are attached to the eyeball for straight and rotary movement
• Each muscle is coordinated with the same muscle in the other eye so that the eyes move in parallel, or conjugate, movement • Superior rectus, inferior rectus, lateral rectus, medial rectus, superior oblique, inferior oblique |
|
|
Which three cranial nerves are responsible for eye movement?
|
• CN 3 (oculomotor)
• CN 4 (trochlear) • CN 6 (abducens) |
|
|
Which eye muscles are innervated by which cranial nerves?
|

|
|
|
What movement is associated with each eye muscle?
|

• Superior rectus – up and temporal
• Inferior rectus – down and temporal • Lateral rectus – horizontal and temporal • Medial rectus – horizontal and nasal • Superior oblique – down and nasal • Inferior oblique – up and nasal |
|
|
How do you test Extra Ocular Movements (EOMs)?
|
• Hold chin to avoid movement
• Follow a moving object through the 6 cardinal positions of gaze • Detect any non parallel movements by comparing both eyes |
|
|
Nystagmus
|
• Involuntary movement of eyeballs
• Normal nystagmus – initial 1 - 2 beats of nystagmus in extreme lateral gaze • Abnormal nystagmus – any beats in other positions of gaze |
|
|
Corneal Light Reflex
|
• Tests the parallel alignment of the eyes
• Instruct patient to look straight ahead • Direct a light source towards the nasal bridge • Note the position of the light reflection on each cornea • The light should fall on the same spot of each eye |
|
|
Esotropia
|
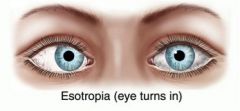
• Form of strabismus
• Eyes turn inward |
|
|
Exotropia
|
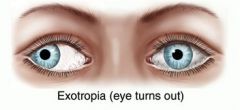
• Form of strabismus
• Eyes turn outward |
|
|
Cover Test
|
• Detects eye muscle weakness
• Ask pt to focus on a fixed object while covering one eye • A weak eye will drift into a relaxed position once the eye is covered • Quickly remove the cover from the eye • If the covered eye moves to reestablish fixation, then eye muscle weakness is present • Repeat procedure for the other eye • Document presence/absence of eye drift when eye is covered |
|
|
Meibomian Gland
|
• Gland inside the eyelid
• Lubricates lids • Prevents evaporation of tears • Provides an air tight seal when eyes are closed |
|
|
Hordeolum
|
• Aka sty
• Localized staph infection of hair follicle at lid margin • Painful |
|
|
• Chalazion
|
• Infection or retention cyst of a meibomian gland
• Swelling with non-tender, firm, discrete nodule on lid • Not painful |
|
|
Blepharitis
|
• Inflammation of eyelids secondary to staph infection or seborrheic dermatitis
|
|
|
Entropion
|
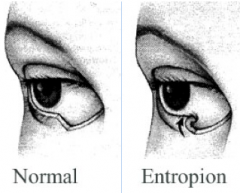
• Inward turn of eyelid
• Lashes irritate conjunctiva • Occurs with weak muscles and normal aging |
|
|
Ectropion
|
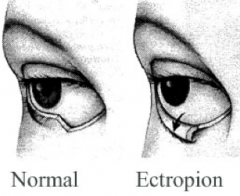
• Outward turn of eyelid
• Most prominent on medial side • Causes increased tearing, loss of tears, and dry eyes • Occurs with muscle loss • Common with normal aging • Can cause conjunctivitis due to to exposure of palpebral conjunctiva |
|
|
Exophthalmos
|

• Lid lag
• Visible white rim of sclera between the upper lid and iris during downward movement of the eyes • Occurs with hyperthyroidism, facial paralysis |
|
|
Where is the following located on the eye:
• Lateral canthus • Medial canthus • Caruncle • Limbus • Conjunctiva |
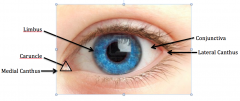
• Lateral canthus – outer corner of eye
• Medial canthus – inner corner of eye • Caruncle – small fleshy mass of the inner canthus containing sebaceous glands • Limbus – border of sclera and iris, bulbar conjunctiva merges with cornea |
|
|
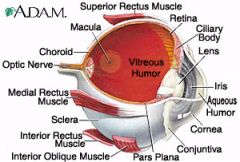
What are the layers of the eye?
|
|
|
|
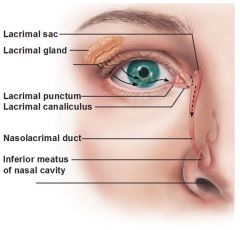
Lacrimal Apparatus
|
• Lacrimal glands, ducts, and sac
• Forms tears to irrigate conjunctiva and cornea to keep eye moist and lubricated • Lacrimal glands, located in upper outer corner or eye, secretes tears that drain across eye into puncta • Tears then drain into the lacrimal sac, through nasolacrimal duct, and empty into the inferior meatus in the nose |
|
|
Enophthalmos
|
• Posterior displacement of eyeballs, eyes are sunken into body orbit
• Opposite of exophthalmos |
|
|
Sclera
|
• Tough, fibrous
• White • Outer covering under transparent bulbar conjunctiva • Scleral redness – called an "injected eyes" • Scleral icterus - yellowed sclera, characteristic of jaundice |
|
|
Bulbar Conjunctiva
|
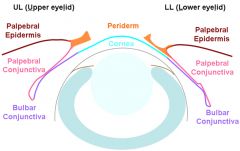
• Protective thin mucous membrane covering the sclera
• Not the cornea • Translucent |
|
|
Conjunctivitis
|
• Aka pink eye
• Mechanical (foreign object), allergic, viral, bacterial • S/S – itching, burning, foreign body sensation, eyes appear red and irritated (red at periphery, clear around iris) • Assess adenopathy |
|
|
Subconjunctival Hemorrhage
|
• Not a serious condition
• Red sclera secondary to increased intraocular pressure (IOP), possibly caused by coughing, sneezing, weight lifting, childbirth, straining with BM, trauma |
|
|
Pinguecula
|
• Yellowish nodules on bulbar conjunctiva at 3 & 9 o'clock-
• Due to thickening secondary to sun, wind, and dust exposure, chronic irritation • Not serious, no treatment |
|
|
Pterygium
|
• Overgrowth of conjunctival tissue
• Starts at inner canthus and progresses towards cornea in a triangular shape • May affect vision if extends to pupil • Treatable via lasar to prevent vision loss |
|
|
Palpebral Conjunctiva
|
• Continuation of mucous membrane that covers inner eyelid
• Check for palpebral pallor of lower lid • Eye pain or foreign body sensation – evert by rolling lid on Q-tip and inspect upper lid |
|
|
How do you test the corneal reflex?
|
• Corneal reflex – blink reflex, protects eye
• Touch cotton wisp to eye • Should blink if CN 5 and 7 intact – CN 5 carries afferent sensation to brain, CN 7 carries efferent message that stimulates the blink reflex |
|
|
Astigmatism
|
• The spherical curve of the cornea is asymmetric around the eye
• Light rays are spread over a diffuse area rather than on a focal point on the retina • Causes blurred vision, but may be corrected with glasses |
|
|
Keratitis
|
• Inflamed cornea
|
|
|
Cornea
|
• Transparent
• Covers and protects the pupil and iris • Helps refract (bend) light rays to focus on the inner retina – damaged cornea affects vision • Shine a light across the cornea from the side – normally smooth and clear, abnormally if cloudy |
|
|
Cataract
|
• Lens opacity
• Pupil may appear cloudy |
|
|
Mydriasis
|
• Dilated pupils
|
|
|
Miosis
|
• Constricted pupils
|
|
|
Anisocoria
|
• Unequal pupil dilation
• Normal in ~5% of population |
|
|
Which crancial nerves are responsible for the dilation and constriction of the pupils?
|
• CN 2 Sensory and 3 Motor
|
|
|
How do you tests for pupillary light reflex?
|
• Shine a light into the eye
• Direct response – pupil of stimulated eye should constrict • Consensual – pupil of unstimulated eye should also constrict • Documentation – R 3/1 = 3/1 L |
|
|
How does the autonomic nervous system affect pupil size?
|
• Sympathetic NS – pupil dilation
• Parasympathetic NS – pupil constriction |
|
|
How do you test for accommodation of the eyes?
|
• Accommodation – ability to adjust vision from far to near
• Focus on a distant object – pupils dilate • Then, look at an object moving towards the nose – pupils constrict and converge |
|
|
How do you document normal pupils?
|
• PERRLA – Pupils are Equal and Round, React to Light, and Accommodation
|
|
|
Lens of the Eye
|
• Transparent
• Posterior to the pupil • Ciliary body controls lens thickness by changing its shape to accommodate for near and far objects |
|
|
Retina
|
• Contains the optic disc, retinal vessels, backgrounds and macula
• Contains transparent vitreous body |
|
|
Fundoscopic (Ophthalmoscopic) Exam
|
• Use the ophthalmoscope for examining the internal eye – use the small aperture for undilated
pupils • Use your right eye to examine the patient's right eye • Begin approximately 10 inches from patient, 15 degrees lateral • Find the Red Reflex (red glow in pupils) – reflection off retina • Adjust diopters to bring structures into focus |
|
|
Anterior Chamber of the Eye
|
• Between cornea and lens
• Contains aqueous humor – produced continually by the ciliary body • Look for abnormalities (opacities, dark shadows, or black dots) – may occur with cataracts or hemorrhages of vitreous humor |
|
|
Intraocular pressure
|
• Normal = 13 - 22 mm Hg
• Determined by the amount of aqueous solution produced and the resistance to its outflow at the angle of the anterior chamber |
|
|
Intraocular Pressure of Glaucoma
|
• IOP > 22 mm Hg
• Chokes the blood supply to the retina • Measured by tonometry • Can cause blindness |
|
|
Fundus of the Eye
|
• Interior surface of the eye, opposite the lens, including the retina, optic disc, and macula
• Color varies depending upon skin color • Grounds should be clear • Abnormal (hemorrhages, exudates, microaneurysms) – seen in hypertension, diabetes, hyperthyroidism |
|
|
Optic Disc
|
• Area of eye where fibers from the retina converge to form the optic nerve (CN 2)
• Located on the nasal side • Yellow to pink, round to oval, distinct margins (may have normal variation of slight fuzziness at nasal border) • Abnormal (fuzzy margins due to papilledema, or disc edema) – seen in hyptertension, increased ICP |
|
|
Retinal Vessels
|
• Consist of a paired arteries (light red, smaller) and veins (dark red, larger)
• Present in four quadrants of retina |
|
|
Macula
|
• Responsible for central vision
• Difficult to find in undilated eyes • Color is dark • Located on temporal side • Contains rods and cones • Contains fovea centralis – center of macula, area of sharpest vision |
|
|
Rods and Cones of the Eye
|
• Rods – responsible of motion detection and night vision
• Cones – detailed vision and color |
|
|
If a pt has glaucoma and macular degeneration, what area(s) of the visual field are lost?
|
• Glaucoma affects peripheral vision
• Macular Degeneration affects central vision • Together, blindness occurs |
|
|
What type of blindness is caused by a blockage of the optic nerve?
|
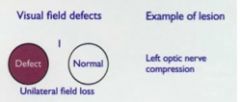
• Unilateral blindness
|
|
|
What type of blindness is caused by a blockage of the optic chiasm?
|
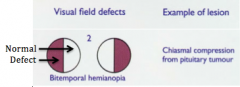
• Bitemporal hemianopsia
|
|
|
What type of blindness is caused by a blockage of the optic tract?
|
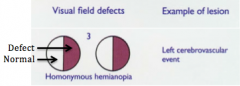
• Homonomous Hemianopsia
|
|
|
Right and Left Optic Tract
|
• Left Optic Tract – fibers from the left half of each retina
• Right Optic Tract – fibers from the right half of each retina |
|
|
Optic Chiasm
|
• Location where fibers from both temporal visual fields cross over
|
|
|
What are the developmental considerations regarding the eye in the infant and child?
|
• At birth – test light perception by observing the blink reflex
• After 2-4 weeks, complete by 4 y/o – observe for tearing • By 3 weeks – test pupillary light reflex • By 1 month – should fixate on yellow, bright object • By 4 months – should fixate on an object with both eyes, vision approx 20/200 • Around 2 y/o – screen vision using picture cards, vision approximately 20/40) • By 3 y/o or preschool – check visual fields • Between 4 and 8 y/o – check color vision (X linked) via Ishirara's test • Extra Ocular Muscle Function - must dx strabismus by 6 y/o, otherwise poor prognosis b/c results in disuse of deviated eye • Setting sun sign • Iris color – permanently differentiates by 6 to 9 months • Check for bilateral red reflex |
|
|
Ishirara's Test
|
• Series of polychromatic cards that have numbers imbedded in different colors
• Tests for color blindness |
|
|
Amblyopia
|
• Loss of vision or blindness due to disuse
|
|
|
How is Extra Ocular Muscle Function tested?
|
• Corneal light reflex
• Cover test • Test for EOMs |
|
|
Setting Sun Sign
|
• Eyes deviate downward with rim of sclera showing above iris (eye point to floor)
• May indicate hydrocephalus |
|
|
What are the developmental considerations regarding the eyes in the aging adult?
|
• May normally have decrease in eyebrow cover on temporal side
• Xanthelasma, pseudoptosis, ectropion, entropion, arcus senilus, floaters, presbyopia, glaucoma, macular degeneration • Dry eyes and burning due to decreased function of lacrimal gland and entropion • Decreased pupil size – creates problems with night vision and night driving • Senile cataract – lens opacifies by age 70, everyone will develop cataracts if they live long enough • Visual acuity may gradually diminish, but central visual acuity generally (85%) remains intact |
|
|
Xanthelasma
|

• Lipid deposits at inner canthus
|
|
|
Pseudoptosis
|
• Lids may droop and cover eyes
• Secondary to loss of elasticity, fat, and muscle atrophy, thus loose skin |
|
|
Arcus senilus / Corneal Arcus
|
• Collection of broken down lipids forming a gray/white circle around the limbus
• Seen in hyperlipidemia |
|
|
Floaters
|
• Occurs in the vitreous due to condensed vitreous fibers or exudates
|
|
|
Presbyopia
|
• Decreased ability of lens to change shape to accommodate for near vision
|
|
|
What are the three primary causes of vision problems in the aging adult?
|
• Cataracts – lens opacity, pupil may appear cloudy
• Glaucoma – loss of peripheral vision • Macular degeneration – loss of central vision, leading cause of blindness • Emphasize regular eye exams and glaucoma testing |
|
|
Locate the following on the ear:
• Auricle/Pinna • External Auditory Canal • Helix • Antihelix • Tragus • Antitragus • Lobe |
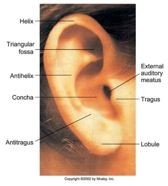
|
|
|
External Auditory Canal (EAC)
|
• 2.5 to 3 cm long
• Terminates at the Tempanic Membrane • Lined with cilia • Glands in the EAC secrete cerumen – yellow waxy substance that lubricates and protects the ear |
|
|
Tympanic Membrane
|
• Ear drum
• Separates external ear canal from middle ear • Normal color – translucent, pearly gray • Anchored in center by malleus • Normally slightly concave – bulding indicates increased pressure (otitis media), retraction indicates vacuum (blocked eustachian tube or serous otitis media) |
|
|
Middle Ear
|
• Air cavity inside temporal bone
• Structures – malleus, incus, stapes • Equalizes pressure by opening eustachian tube to nasopharynx – path for infection • Conducts sound vibrations to inner ear |
|
|
Inner Ear
|
• Contains sensory organs for equilibrium and hearing
• Structures – vestibule, semicircular canals, cochlea • Cochlea contains the Organ of Corti, which transmits sound impulses to the CN 8 |
|
|
Pathway of Sound thru Ear
|
• Sound is transmitted through the external auditory cannel to the Tympanic Membrane
• Vibrations of the TM are transmitted by the middle ear bones to the oval window • Sound is then transmitted to the sensory organs of the inner ear where the round window disperses the vibrations • Lastly, vibrations are converted to nerve impulses which are conducted by the 8th cranial nerve to the temporal lobe of the brain for interpretation of sound |
|
|
Air Conduction (AC) of Sound
|
• Vibrations reach sensory organ of ear through air
• Usual mechanism of hearing, most effective |
|
|
Bone Conduction (BC) of Sound
|
• Comduction via vibration of skull bones
• Transmits sound directly to inner ear and CN 8 • Alternate route of sound |
|
|
Conductive Hearing Loss
|
• Obstruction in the external or middle ear
• Can be blocked by cerumen, foreign body, perforated TM, fluid in middle ear, otosclerosis |
|
|
Sensorineural or Perceptive Hearing Loss
|
• Pathology in the inner ear, CN 8, or auditory areas of the temporal lobe
• Common w/ aging (~40s, 5th decade) • Ex - presbycusis |
|
|
Presbycusis
|
• Gradual nerve degeneration
• Occurs with aging – begins when a person is in the 40s • Type of sensorineural/perceptive hearing loss • High frequency sounds are lost 1st – shouting increases high frequency and makes hearing worse • Harder to hear consonants – speech may sound garbled) • Hearing difficulty increases with background noise |
|
|
Mixed Hearing Loss
|
• Combination of conductive and sensorineural
• Ex – presbycusis and ear wax |
|
|
Equilibrium
|
• Vestibular branch of CN 8
• Labyrinth constantly sends info regarding body position to the brain • Inflammation causes vertigo |
|
|
What are the developmental considerations regarding the ears in the fetus?
|
• Inner ear develops by 4th week
• Rubella during the 1st trimester damages the Organ of Corti, causing hearing loss or deafness in the child – decreased risk with immunizations |
|
|
What are the developmental considerations regarding the ears in the infant and young child?
|
• Newborn – Moro (startle) reflex
• 3-4 months – acoustic blink reflex (infant stops movement and appears to listen) • 6-8 months – turns head to localize sound • Preschool – screen with audiometry, especially if no speech by age 2 • Children have an increased risk of ear infections due to a shorter and wider eustachian tube • Two episodes of ear infections in the first year are predictive of future problems • Use pneumatic insufflator (puff of air) – should vibrate the TM, cone of light flickers |
|
|
Signs of Hearing Loss in Children
|
• Delayed speech
• Reacts more to movement and facial expression than to sound • Speech is monotonous or garbled, mispronounces sounds • Appears shy and withdrawn |
|
|
What are the developmental considerations regarding the ears in the aging adult?
|
• Decreased hearing related to increase coarseness of cilia lining ear canal and drier, more occlusive cerumen (atrophy of the apocrine glands)
• Presbycusis • Auditory reaction time is delayed after age 70 – increases driving risk |
|
|
S/S of Hearing Loss
|
• Inattentive in casual conversation
• Lip reading – watching lips rather than eyes • Facial expression is strained or puzzled • Posturing head – to hear sounds with the better ear • Misunderstanding questions – confuses words that sound alike • Frequently asks to have statements repeated • Speech sounds garbled, vowel sounds distorted • Inappropriately loud voice • Flat monotonous tone of voice • Hears better when the environment is quiet |
|
|
Ototoxic Medications
|
• Salicylates (Aspirin)
• Aminoglycoside antibiotics – streptomycin, gentamycin, kanamycin, neomycin, vancomyosin • Others – furosemide (lasix), indocin, quinine • May need to stop medications if tinnitus occurs |
|
|
Microtia
|
• Small ears
• < 4 cm |
|
|
Macrotia
|
• Large Ears
• > 10 cm |
|
|
Cauliflower Ear
|
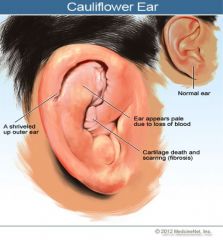
• Abnormal shape of the ear
• Due to repeated rauma to underlying cartilage |
|
|
What is the normal position of the ear?
|
• Top of the pinna should touch or be above an imaginary line drawn from the inner canthus of the eye to the most prominent area of the occipital bone
• Tilt of the pinna should be within 10 degrees of vertical • Abnormal positioning may indicate a chromosomal abnormality and genitourinary problems |
|
|
Darwin's Tubercle
|
• Painless nodule on helix
• Normal abnormality |
|
|
Tophi
|

• Yellow, non-tender nodules on helix
• Secondary to gout • Contains uric acid crystals |
|
|
Mastoiditis
|
• Painful, swollen, erythematous mastoid region
• Assc. w/ otitis media |
|
|
How do you hold the ear of an adult during an otoscope exam?
How do you hold the ear of a child during an otoscope exam? |
• Adult – hold ear up and back
• Child – hold ear down |
|
|
Cerumen
|
• Ear wax
• Two types of ear wax – genetically determined • Moist/honey colored – Af-Amer, Caucasians • Dry/flaky – Asians & Nat-Amer • Ear wax does not indicate poor hygiene |
|
|
What might clear, watery exudate from the ear after head trauma indicate?
|
• Exudate may be CSF from basilar skull fracture
• Test fluid for glucose via test strip – if it is positive glucose, it's CSF • Needs immediate attention – increased risk of bacterial meningitis |
|
|
Furuncle
|
• Boil from infected hair follicle
|
|
|
Aural Atresia
|
• Absence or closure of ear canal
|
|
|
Exostosis
|
• Small, hard bony nodules in ear canal, hypertrophic bone
• More common in cold water swimmers • Benign, doesn’t require treatment |
|
|
Landmarks of Tympanic Membrane:
• Cone of Light • Pars Flaccida • Pars Tensa • Short Process of Malleus • Manubrium/Handle of Malleus • Umbo • Annulus |
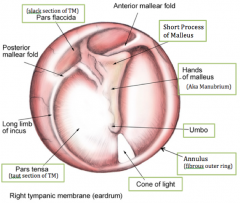
|
|
|
Cone of Light (Triangular Reflection)
|
• Right Ear – 5 o'clock
• Left Ear – 7 o'clock |
|
|
S/S of Acute Tympanic Membrane Perforation
|
• Pain > Pop > Relief
• Ear pain • Loss of landmarks • Purulent drainage seen in ear canal • Current perforation is a dark oval, old perforation is a white oval • Important not to let any fluid enter inner ear after perforation • Conductive hearing loss |
|
|
Hearing Tests
|
• Whisper or Voice Test – occlude one ear, whisper behind pt to evaluate hearing
• Weber Test – place activated tuning fork on top of hear, sound should equalize bilaterally • Rinne – place activated tuning fork on mastoid process (BC), then at external auditory canal (AC); AC should be greater than BC • |
|
|
What is indicated when a Weber Test is only heard in one ear?
|
• Only heard in "bad" ear – this is a GOOD thing, this means there is only a conductive loss (i.e. obstruction, TM perforation, otitis media), not sensorineural/perceptive problem; CN intact
• Only heard in "good" ear – this is a BAD thing, this means there is a sensorineural/perceptive and conductive loss; CN impaired |
|
|
If BC > AC, what type of hearing loss?
If AC > BC, what type of hearing loss? |
• BC > AC – Conductive Loss
• AC > BC – Sensorineural Loss |
|
|
Romberg Test
|
• Vestibular test
• Stand with feet together, arms at sides, eyes closed approx 20 sec. • Observe balance • Tests cerebellum and proprioception (vestibular apparatus in inner ear) • Positive Romberg – unsteady balance, falling out of stance |
|
|
Give the name, function, and test for cranial nerve 1
|
• Name – Olfactory
• Sensory Fxn – smell • Test – close eyes, occlude one nares, test smell with a familiar aromatic substance |
|
|
Give the name, function, and test for cranial nerve 2
|
• Name – Optic
• Sensory Fxn – vision • Test – test visual acuity by snellen, visual fields by confrontation, fundoscopic exam |
|
|
Give the name, function, and test for cranial nerve 3
|
• Name – Oculomotor
• Motor Fxn – eye muscles • Test – PERRLA, EOMs, lid lag, ptosis |
|
|
Give the name and the function of cranial nerve 4
|
• Name – Trochlear
• Motor Fxn – eye muscles • Test – EOMs, lid lag |
|
|
Give the name, function, and test for cranial nerve 5
|
• Name – Trigeminal
• Sensory Fxn – general sensation from face, eyes, mouth • Sensory Test – test 3 zones of sensation (ophthalmic, maxillary, manibular) bilaterally with cotton ball • Motor Fxn – skeletal muscles of mastication • Motor Test – assess temporal and massester muscle strength while clenching teeth, lateral jaw strength or chin strength against resistance • Corneal reflex requires intact CN 5 |
|
|
Give the name, function, and test for cranial nerve 6
|
• Name – Abducens
• Motor Fxn – eye muscles • Test – EOMs (lateral eye movement), lid lag |
|
|
Give the name, function, and test for cranial nerve 7
|
• Name – Facial
• Sensory Fxn – taste from anterior tongue • Test – sweet and salty taste from anterior tongue • Motor Fxn – muscles of facial expression, salivary glands • Test – assess facial movement, expresseion (smile, frown, puff cheecks against resistance, raise eyebrows, close eyes against resistance), and symmetry • Corneal reflex requires in tact CN 7 |
|
|
Give the name, function, and test for cranial nerve 8
|
• Name – Vestibulocochlear
• Sensory Fxn – hearing, equilibrium • Hearing Test – whisper test, Weber's, Rinne • Equilibrium Tests – Romberg |
|
|
Give the name, function, and test for cranial nerve 9
|
• Name – Glossopharyngeal
• Sensory Fxn – taste from posterior tongue, general sensations from middle ear and throat, BP and gas content within major blood vessels • Motor Fxn – swallowing muscles, salivary gland • Test - say "ahhh," uvula should rise midline; gag flex; test sour/bitter from posterior tongue |
|
|
Give the name, function, and test for cranial nerve 10
|
• Name – Vagus
• Sensory Fxn – general sensations from thoracic and abdominal viscera • Motor Fxn – larynx, swallowing muscles, thoracic and abdominal viscera • Test - say "ahhh," uvula should rise midline (deviation can indicate tonsilar abscess, nerve damage, polio, diphtheria); gag flex |
|
|
Give the name, function, and test for cranial nerve 11
|
• Name – Accessory
• Motor Fxn – swallowing muscles, sternocleidomastoid and trapexius • Test - shoulder shrug against resistance |
|
|
Give the name, function, and test for cranial nerve 12
|
• Name – Hypoglossal
• Motor Fxn – tongue muscles • Test – movement and strength of tongue by sticking out tongue and pushing against resistance; position (midline vs deviation towards paralyzed side) |
|
|
Otorrhea
|
• Ear discharge
|
|
|
Pharyngitis
|
• Soar Throat
|
|
|
Otosclerosis
|
• 3 middle ear bones harden and stop moving
• Common in middle aged men • Conductive loss |

