![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
33 Cards in this Set
- Front
- Back
|
Ataxia |
Comes from greek a-taxis: without order or without coordination Incoordination during voluntray movement without paresis, spasticity or involuntary movement Ataxia is usually associated with a wide base stance and incoordination of the limbs Cerebellar ataxia = abnormal rate, range, or force of movement with intact strength Vestibular ataxia = loss of balance; animal often lists or falls to one side Proprioceptive ataxia = decreased awareness of limb position and often results in scuffing of toes, crossing oflimbs, and standing on the dorsum of paws |
|
|
Causes of Ataxia and specific signs |
1. Abnormal proprioception (sensory ataxia)-any Dz causing compression of SC or otherwise affecting proprioceptive tracts in SC or brain CSx: absent or reduced knuckling respons, postural responses (ie hopping reaction) may also be abnormal. May see additional signs of Sc dysfunction (paresis etc) 2. Cerebellar dysfucntion: may arise from many Dz's (congenital malformation, infection, abiotrophy) CSx: typically assoc with symmetric ataxia, dysmetria (eg goose stepping gait), intention tremors (esp of head) 3. Vestibular Dz: common in dogs and cats and may be idiopathic, associated with middle/inner ear Dz or associated with brain stem Dz CSx: asymmetric ataxia, head tilt, nystagmus and falling or rolling to one side |
|
|
Paresis and paralysis |
Paresis is the partial loss of voluntary motor actvity (ie reduced ability to initiate motor activity) Paraylsis or plegia is the complete loss of voluntary motor activity |
|
|
Mentation classification |
Depression: Lethargy with decreased activity but normal mental status Obtundation: Dull mentation with decreased consciousness and response to mild stimulus Stupor: Decreased consciousness and response only to noxious stimulus Coma: Unconscious and no response to even noxious stimulus |
|
|
Causes of altered mentation |
The RAS in the rostral midbrain controls the level of consciousness, and any Dz process affecting this area of uts connections to the cerebral cortex will alter consciousness Coma or stupor results from one of three Dz processes: 1. Encephalopathy (metabolic or toxic) 2. Diffuse cerebral cortical Dz 3. Dz in the midbrain or pons (compression, destructive lesions) Most important aetio: increased ICP, cerebral oedema, herniation of brain tissue |
|
|
Proprioception |
From Latin proprius, meaning "one's own", "individual," (think of "to appropriate an object"; ad + proprius-->to make ones own) and capio, capere, to take or grasp, is the sense of the relative position of neighbouring parts of the body and strength of effort being employed in movement Means "sense of position" Clinical sign of loss of proprioception is ataxia (in coordination) |
|
|
Spasticity |
Increase in muscle tone due to hyperexcitable stretch (myotactic) reflexes Descending UMN pathways normally attenuate the myotactic reflex. Lesions in the UMN pathway cause changes in the excitability of motor neurons, interneuronal connections and local reflex pathways that over time lead to hyperexcitable myotactic reflexes and spasticity |
|
|
Tetany |
Sustained muscle contraction that is worsened by stimulation It occurs with: strychnine poisoning, some congenital conditions |
|
|
Tremor |
Rhythmic oscillation of the body or body part due to alternating contractions of antagonistic muscles Can be: intention tremor, resting tremor, fine fast action tremor or static tremor |
|
|
Peripheral Vestibular Dz SIgns |
No signs of altered mental status or proprioceptive positioning deficits No positional nystagmus (nystagmus is always in the same direction) and is either horizontal or rotatory NOT vertical Head tilt towards affected side Ipsilateral ataxia Fast phase of nystagmus AWAY from affected side |
|
|
Central Vestibular Dz Signs |
Changes in mental status (most commonly somnolence) and deficits in proprioceptive positioning and/or hopping Nonambulatory tetraparesis common vertical or positional nystagmus may be seen |
|
|
Cerebellar Ataxia |
Characterized by dysmetria (inability to control the rate and range of stepping movements) which is usually manifested as hypermetria (exaggerated step-hyperflexion) Diff from spasticity: spasticity causes thoracic limbs to appear rigid or spastic while hypermetria is manifested by prolonged flexion of the step (protraction) Other signs: truncal sway, head/whole body tremors, intentional tremors, wide pelvic limb stance and gait Other signs: coexisting vestibular (possible), mentation WNL, tone/reflexes generally WNL (sever signs->increased tone), proprioception normal to delayed (ipsi) |
|
|
Spinal Cord Segments |
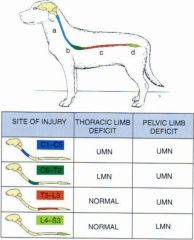
|
|
|
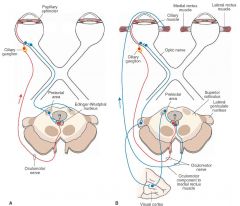
SNS Innervation eye |

|
|
|
PSNS and SNS Innervation of eye |
|
|
|
PLR and conscious vision |
|
|
|
Panniculus reflex (cutaneous trunci reflex) |
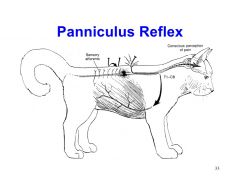
|
|
|
Menace response |

|
|
|
Meningitis causes |
Septic: Non septic Idiopathic: |
|
|
Seziures causes |
Intracranial Extracranial |
|
|
Steps for localizing lesions causing cranial nerve signs (ie WITHIN the brain) |
1. Gait normal or abnormal? Normal: 2. Postural reactions: Deficits-->Cerebrum/diencephalon Normal-->neuropathy of cranial nerves Abnormal Gait: 2. Type of gait abnormality Tetraparesis/hemiparesis *UMN signs-->Brainstem *LMN signs-->generalized LMN disorder Asymmetric ataxia, head tilt, proprioception normal, direction of nystagmus doe snot change, facial paresis, Horner's syndrome -->Peripheral vestibular Dz |
|
|
Brainstem Dysfunction |
For these puposes functional brainstem; midbrain, pons, medulla oblongata UMN signs in all four limbs (tetraparesis) or hemiparesis (depends on site) Paresis/paralysis caused by brainstem dysfunction is obvious in gait and postural reactions good for cf with forebrain elsions-->minimal gait abnormalities (have postural deficits/walking or circling) CN signs (III-XII) with larger or extensive brainstem lesions. Help localize lesion Mental status may be altered (esp if there are lesions in midbrain or pons)-dullness to coma CN dysfunction will be ipsilateral to lesions Motor dysfunction (ie gait) can be contraletral or ipsilateral depdning on pathways affected |
|
|
Diencephalon DYsfunction |
May produce UMN signs in all 4 limbs (tetraparesis) or hemiparesis Gait is not severly afafcted but postural deficits may be seen May circle in eitehr direction depending on lesion CN II may be affected-visual and PLR deficits SOL of dinecephalon may also affect CN III, IV and VI CN signs are ipislateral to lesion Postural dfeicits are ontarletarl to lesions or ipislateral to lesion Characteristic abnormality-->hypothalamic problem May have generalized hyperesthesia (rare) due to thalamic central role in sensory pathway projection to the cerebral cortex Altered level of consciousness (stupor or coma) due to interference with ARAS |
|
|
Vestibular Dysfunction |
May be central (brainstem-affecting the nuclei, cerebllum (vestibulocerebellum), sinal cord (vestibulospinal tracts)) or peripheral (affecting the nerve or labyrinth->old dog vestibular Dz) CANNOT rule out central vestib Dz on neuro exam, can only RULE IN (eg vertical nystagmus, paradoxical head tilt, extra-vestibular signs assoc with brainstem) Any sign of of brainstem Dz in assoc with vestibular signs indicate that central involvment is present. Most important differentiating feature->deficit in postural reactions Peripheral vestibular dysfunctio does not cause paresis or loss of proprioception whereas central Dz freq does |
|
|
Cerebellar Dysfunction Signs |
May be unilateral or bilateral Spastic ataxia, wide-based stance, dysmetria, intention tremor, no obvious signs of weakness Cerebellar ataxia is often characetrized by dysmetria (stride lengths that are too short-hypometria, stride lengths that are too long-hypermetria) Nystagmus may occur-usually more of a tremor of the globe than the slow-quick movemnts assoc with evstibular Dz Is most pronounced when animal shifts its gaze and focuses on annew field (intention tremor) ACute injury to cerebllum can cause decerebellate posture: extensor hypertonus in TL and flexion in PL Lesions to floculonodular node causes vestibular signs Diffuse cerebellar lesion-->loss of menace response |
|
|
Cerebral Dysfunction signs |
Alteration in behaviour or mental status Seziures Loss of vision with intact PLR Contarletral decrease in facial sensation Mild contarleteral hemiparesis Deficits in postural reactions Only one or two of these signs may be present Signs are generally contraletarl to lesion Behavioural changes-->often lesion in limbic system/frontal/temporal lobes Frontal lobe lesion-->disinhibition-->excessive pacing Pacing will often continue until a barrier is reached and head pressing will occur If there is an asymmetric lesion ciricling may occur (ipsilateral to lesion) and head TURN (not tilt) towards side of lesion may be seen Dullness, stupor or coma Mentation abnormalities usually more severe with brainstem injuries |
|
|
Brain regions to Localize to |
1. Telencephalon 2. Diencephalon 3. Brainstem (mesencephalon, pons, myelencephalon) 4. Vestibular system 5. Cerebellar |
|
|
Decerebrate rigidity |
Extensor rigidity of all limbs; secondary to severe cortical/midbrain lesion; patient usuallycomatose |
|
|
Decerebellate rigidity |
Extensor rigidity of the thoracic limbs with flexion of pelvic limbs and dorsal extension ofthe head; associated with acute cerebellar lesions including herniation |
|
|
Hyperaesthesia, anaesthesia, hyperalgesia, analgesia |
Hyperesthesia: increased sensitivity to sensory stimulus Anaesthesia: absent response to sensory stimulus Hypalgesia: decreased sensitivity to painAnalgesia: absent pain perception |
|
|
Spinal Cord Disease |
GAIT->UMN/GP Ataxia -slow strided gait -prolonged swing phase to gait ("floating" end to swing phase) -knuckling/scuffing -crossing limbs Mentation, CN WNL +/- pain at site of lesion Proprioception->normal to reduced Tone->decreased (LMN), normal to increased (UMN) Reflexes->decreased (LMN), normal to increased (UMN) |
|
|
Idiopathic Vestibular Disease |
Peripheral vestibular Dz Dogs->most commonly eriatric, GSD Cats->any age DDx: peripheral-neoplasia, otitis media/interna, ototoxicity central-malformation, inflamm/infctn, neoplasia, CVA Investigate well, then provide supportive care (fluids if not drinking, anti emetic to counter motions sickness, keep in hospital to avoid self harm) If there is gradual or complete improvement within 72 hours, it is likely idiopathic vestibular disease and additional diagnostic testing is not necessary. If there is no improvement or progression of signs, it is likely something much more serious |
|
|
Prosencaphelic Disease Gait and CP |
Gait: normal gait with postural reaction deficits (contralateral to lesion) NO ataxia, NO weakness Propulsive gait (constantly pacing, aimless), circling (towards lesion) Postoral reactions->normal to delayed Other signs: CN often abnormal, contralateral visual deficit with NORMAL PLR, contrlateral facial hypalgesia, facial/tongue paralysis, ALTERED MENTATION, ALTERED BEHAVIOUR (lack of recognition of environ, may be more aggressive or more docile, propulsive, SEZIURES) |

