![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
108 Cards in this Set
- Front
- Back
|
Heart Failure
(HF) |
--Abnormal condition involving impaired cardiac pumping
--HF (aka CHF) is not a disease but a “syndrome” Associated with long-standing HTN & CAD --Results from the heart’s inability to pump amt of oxygenated blood needed to meet metabolic requirements of body |
|
|
Statistics
(HF) |
--Affects about 5.7 million people (AHA,2012)
--Most common reason for hospitalization in adults older than 65 --About ½ of all people who have heart failure die within 5 years --Heart Failure costs the nation $34.4 billion each year Incidence hasn’t ↓ in 2 decades but overall survival ↑ |
|
|
Risk Factors
(HF) |
--Age
--Hypertension ----To compensate for ↑ B/P the heart muscle thickens ----Over time force of heart muscle contraction weakens preventing normal filling of heart with blood --High cholesterol --African American descent ----Related to the higher incidence of HTN & DM ----Have a 30% higher mortality rate |
|
|
Etiology & Pathophysiology
(HF) |
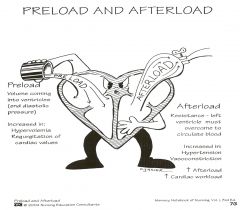
--May be caused by an interference with normal mechanisms regulating cardiac output (CO)
----CO = HR X SV (amt of blood pumped from LV with each contraction) CO influenced by: --Preload = Volume of blood in ventricle at end of diastole --Afterload = Force ventricle must develop to eject blood into circulatory system --Myocardial contractility --Heart rate --Metabolic state of individual |
|
|
Types of HF
|
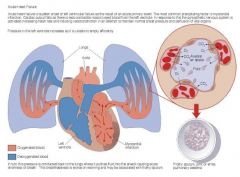
Left-sided failure
--Most common form --Blood backs up through left atrium into pulmonary veins --Pulmonary congestion & edema Right-sided failure --Backflow to right atrium & venous circulation --Results from diseased right ventricle --One-sided failure eventually leads to biventricular failure |
|
|
Left-Sided Heart Failure
|
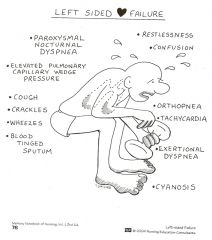
|
|
|
Right-Sided Heart Failure
|
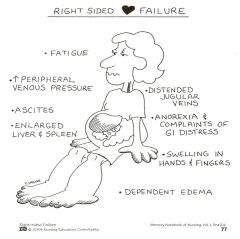
|
|
|
Clinical Manifestations
(acute HF /CHF) |
Pulmonary edema
--Agitation --Pale or cyanotic --Cold, clammy skin --Severe dyspnea, crackles, cough (hacking, productive, dry), “frothy” secretions --Tachypnea --Tachycardia Signs & symptoms of low cardiac output: --Think “head-to-toe” assessment & abnormal heart sounds (e.g. S3, S4, murmur) Fatigue --Earliest symptoms, after activities which are normally not tiring ----Related to decreased CO Dyspnea (PND) or SOB --Cause by alveolar edema --PND – reabsorption from dependent areas when patient is sleeping --Pt c/o suffocation feelings Tachycardia --Compensatory mechanism from SNS Heart murmur, S3, S4 Heaves/Lift --3rd to 5th intercostal spaces using ball of your hand Edema/Anasarca --Legs, liver, abdomen Nocturia --Related to recumbent position ↑ renal blood flow Chest pain --Related to decreased coronary perfusion from ↓ CO & ↑ work of heart --Can be anginal pain Weight changes --Multifactoral Skin changes --Dusky appearance Many patients suffer from sleep obstructive apnea Behavioral changes --Restlessness, confusion, ↓ attention span, some (impaired cognition), sleepiness |
|
|
Complications
(HF) |
--Pleural effusion
--Arrhythmias --Left ventricular thrombus --Hepatomegaly --Pulmonary hypertension |
|
|
Symptom Classification System
(HF) |
I - No symptom limitation with ordinary physical
activity II - Ordinary physical activity somewhat limited by dyspnea (ie, long distance walking, climbing 2 flights of stairs) III - Exercise limited by dyspnea at mild work loads (ie, short distance walking, climbing one flight of stairs) IV - Dyspnea at rest or with very little exertion |
|
|
Classification of Chronic Heart Failure
|
A
- High risk for developing heart failure
--Hypertension, diabetes mellitus, CAD, family history of cardiomyopathy B - Asymptomatic heart failure --Previous MI, LV dysfunction, valvular heart disease C - Symptomatic heart failure --Structural heart disease, dyspnea and fatigue, impaired exercise tolerance D - Refractory end-stage heart failure --Marked symptoms at rest despite maximal medical therapy |
|
|
Diagnostics
(HF) |
--Primary goal to determine underlying cause
--History & physical exam --ABGs, serum chemistries --Chest X ray --12-Lead ECG --Hemodynamic assessment/monitoring --Echocardiogram (determines LVEF) --Stress testing --Nuclear imaging studies --Cardiac catheterization --Laboratory tests; CBC, BMP, HBA1C, Lipid profile, thyroid levels, cardiac enzymes and B type natriuretic peptide level (BNP) |
|
|
Nursing & Collaborative Management
(AHF) |
Primary goal is to improve LV function by:
↓ intravascular volume ↓ preload (venous return) ↓ afterload Improving gas exchange & oxygenation Improving cardiac function Reducing anxiety |
|
|
HCP Orders
(AHF) |
--Oxygen 2L/min via nasal cannula
--Lasix 40 mg IV push STAT and every 12 hours --Insert peripheral IV D5W at 5 ml/hr --Insert Foley catheter |
|
|
In-Depth Nursing & Collaborative Management
(AHF) |
1. ↓ preload
--Reduce the amount of volume returned to the LV --Diuretics --Nutritional therapy --High Fowler’s position 2. ↓ afterload --↓ pulmonary congestion --ACE inhibitors/ARBs --Nesiritide (Natrecor) – both afterload & preload reducer 3. Improving gas exchange & oxygenation --↓ pulmonary congestion --IV Morphine --Administer oxygen --Possible intubation 4. Improving cardiac function --Digoxin (Lanoxin) (enhance contractility) --Newer inotropics --e.g., PDE III inhibitor: Milrinone (Primacor) --Beta-blockers --Hemodynamic monitoring 5. ↓ anxiety |
|
|
Nursing & Collaborative Management
(Chronic HF) |
--Treat underlying cause
--Maximize (optimize) cardiac output --Alleviate symptoms --Rest --Biventricular pacing (Generic: Cardiac Resynchronization Therapy or CRT) --Oxygen treatment --Mechanical hearts --Heart transplantation |
|
|
Drug Therapy
(Chronic HF) |
--ACE Inhibitors
--Angiotensin-II Receptor Blockers (ARB) --Inotropic drugs --Digoxin --PDE III inhibitor --Vasodilators --Beta Blockers --Diuretics --Anticoagulants (e.g.,Warfarin) --Antidysrhythmic drugs |
|
|
Nutrition Therapy
(Chronic HF) |
Fluid restrictions not commonly prescribed
Sodium restriction --1.5 gm sodium diet (AHA 2010) Daily weights --Same time each day --Wearing same type of clothing Teach patients on how to read food labels |
|
|
Discharge Teaching
(Chronic HF) |
MAWDS
--Medications --Activity --Weight --Diet --Symptoms Follow-up Appointment |
|
|
Nursing Management
(chronic HF) |
Nursing ASSESSMENT
--Past health history --Medications --Functional health problems --Objective sx: cold, diaphoretic skin, tachypnea, tachycardia, crackles, abdominal distention/pain (feel bloated), restlessness --(See detailed list of sx, Chapter 34) Nursing DIAGNOSES --Activity intolerance (remember NYHA functional Class) --Excess fluid volume --Disturbed sleep pattern --Impaired gas exchange --Anxiety PLANNING Overall Goals: --↓ peripheral edema --↓ SOB --↑ exercise tolerance --Compliance with medications, diet, clinic appointments --No complications IMPLEMENTATION Acute Intervention: --Establishment of quality of life goals --Symptom management --Conservation of physical/emotional energy --Support system Ambulatory & home care: Teaching: --Psychological changes --Exercise-saving behaviors --Medications --Diet --Relaxation techniques --Support groups (as needed) --Social services referral as needed EVALUATION --Tissue perfusion --Respiratory status --Sleep --Fluid balance --Activity intolerance --Anxiety control --Knowledge: Disease process --Support system |
|
|
Healthy People 2020 Objectives
(Breast Disorders) |
--↓ female deaths from breast cancer
--↑ proportion women who receive a breast cancer screening based on most recent guidelines --↓ deaths from prostate cancer --↑ proportion of men who have discussed with their HCP whether or not to have a prostate-specific antigen (PSA) test to screen for prostate cancer |
|
|
Benign Breast Disorders
|
Fibroadenoma
Fibrocystic Breast Changes |
|
|
Fibroadenoma
(Benign Breast Disorders) |
Solid, slowly enlarging, benign mass; round, firm, easily movable, nontender, and clearly delineated from surrounding tissue
Usually located in upper outer quadrant of breast |
|
|
Fibrocystic Breast Condition
(Benign Breast Disorders) |
--Fibrocystic changes of breast (may involve lobules, ducts, stromal tissues)
--Common in premenopausal women between 20 and 50 years of age --Possibly caused by imbalance in normal estrogen-to-progesterone ratio --Rubbery, ill-defined --Painful/Tender --Increased tenderness & size prior to menstruation --Symptoms increase in the *premenstrual phase* |
|
|
Collaborative Care
(Fibrocystic Breast Changes) |
Diagnostic studies:
--Aspiration or needle biopsy --Mammography or ultrasound --Surgical removal --Supportive undergarments --OTC pain relievers --Caffeine --Vitamins --Low Na+ diet or diuretics --Hormones |
|
|
Breast Cancer
|
Types
Complications: --Invasion of lymph channels causing skin edema --Metastasis to lymph nodes --Bone, lungs, brain, liver—sites of metastatic disease from breast cancer --Ulceration of overlying skin |
|
|
Clinical Manifestations
(Breast Cancer) |

--Single lump, mass, or mammographic abnormality
--Painless, hard, irregular edges > likely to be cancerous --Can also be tender, soft or rounded --Orange peel appearance --Swelling of all or part of a breast --Skin irritation or dimpling --Breast or nipple pain --Nipple retraction (turning inward) --Redness, scaliness, or thickening of nipple or breast skin --A discharge other than breast milk, e.g., clear or bloody |
|
|
Men
(Breast Cancer) |
--Of all breast cancers, only 1% occur in men
--Usually presents as hard, painless, subareolar mass --Often widely spread disease because it is usually detected at a later stage than in women |
|
|
Screening
(Breast Cancer) |
--American Cancer Society Guidelines for the Early Detection of Cancer
--The American Cancer Society recommends these screening guidelines for most adults. Breast cancer --Yearly mammograms are recommended starting at age 40 and continuing for as long as a woman is in good health --Clinical breast exam (CBE) about every 3 years for women in their 20s and 30s and every year for women 40 and over --Women should know how their breasts normally look and feel and report any breast change promptly to their health care provider. Breast self-exam (BSE) is an option for women starting in their 20s. |
|
|
Screening: The United States Preventative Service Task Force (USPSTF)
(Breast Cancer) |
--The USPSTF recommends biennial screening mammography for women aged 50 to 74 years.
--The decision to start regular, biennial screening mammography before the age of 50 years should be an individual one and take patient context into account, including the patient's values regarding specific benefits and harms. --The USPSTF concludes that the current evidence is insufficient to assess the additional benefits and harms of screening mammography in women 75 years or older. --The USPSTF recommends against teaching breast self-examination (BSE). --The USPSTF concludes that the current evidence is insufficient to assess the additional benefits and harms of clinical breast examination (CBE) beyond screening mammography in women 40 years or older. |
|
|
Diagnostics
(Breast Cancer) |
--Same as fibrocystic breast disease
--Ploidy status ----Tumor differentiation (abnormality) ----Correlates with tumor aggressiveness --Axillary Lymph Node vs. Sentinel Lymph Node Dissection --Tumor size: Larger the tumor, the poorer the prognosis --Stages: TNM classification |
|
|
Surgical Therapy
(Breast Cancer) |
Lumpectomy
--Conserves the breast, nipple --Removal of tumor with small amts of normal tissue --Radiation post removal --ALND vs. SLND Modified radical mastectomy --Removal of breast & axillary nodes but conserves the pectoralis muscle |
|
|
Radiation Therapy
(Breast Cancer) |
--Radiation Therapy (Breast Cancer)
--Primary treatment (5-6 weeks) --Shrink a large tumor size to operable size --Palliative treatment for pain --Brachytherapy |
|
|
Chemotherapy (Breast Cancer)
|
--Cytotoxic drugs to destroy cancer cells
--Administered pre- & post-op --Pre-op (neoadjuvant): Shrink tumor, < extensive surgery --Suppresses tumor growth & prolongs survival |
|
|
Prophylactic Oophorectomy
(Breast Cancer) |
If BRCA gene mutation
|
|
|
Hormonal Therapy (Breast Cancer)
|
--Tamoxifen Citrate (Novaldex) – blocks estrogen
--Post-menopausal women w/out lymph node involvement, BRCA 2 mutation, or ↑ risk breast cancer --Prevention in individuals in high risk category --Side effects: Hot flashes, nausea, vomiting, blood clots, & endometrial cancer |
|
|
Post Op Nursing: Surgical Management
(Breast Cancer) |

--LOC, V/S
--Bleeding (dsg, drains) --Infection --Avoid BP, injections, phlebotomy affected arm --Ambulation & diet --Postmastectomy exercises --Breast reconstruction --Adjuvant therapy |
|
|
Discharge Teaching
(Breast Cancer) |
--Psychosocial
--Infection --Incisional & drain care --Exercises --Lymphedema --Health promotion --Follow up care --Sexuality |
|
|
Benign Prostatic Hyperplasia (BPH)
|
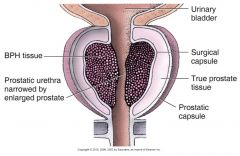
Glandular units in the prostate that undergo an increase in number of cells, resulting in enlargement of prostate gland
|
|
|
Symptoms
(BPH) |
--Hyperirritable bladder
--Urgency and frequency --Hypertrophied bladder wall muscles --Cellules and diverticula --Hydroureter --Hydronephrosis --Overflow urinary incontinence |
|
|
Potential Complications
(BPH) |
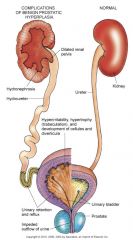
|
|
|
Surgical Procedures
(BPH) |
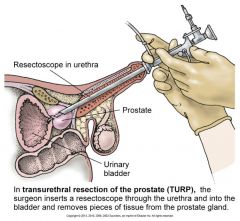
Transurethral resection of prostate (TURP)
Prostatectomy --Suprapubic --Retropubic --Perineal |
|
|
Postoperative Care
(Prostatectomy Procedures, BPH) |
Urinary catheter with retention balloon placed into bladder
Traction via taping to patient’s abdomen or thigh Uncomfortable urge to void continuously |
|
|
Diagnostics
(BPH) |
--Digital rectal exam
--Urine analysis and culture --Serum creatinine and BUN --PSA (Prostate Specific Antigen) --Urodynamic flow studies --Cystourethroscopy |
|
|
Treatment Goals
(BPH) |
Restore bladder drainage
Relieve symptoms Treat complications |
|
|
Drug Therapy
(BPH) |
Hormonal manipulation (androgen)
--Proscar Alpha-adrenergic blockers --Minipress, Cardura, Hytrin --Side effects: orthostatic hypotension, dizziness |
|
|
Conservative Therapy
(BPH) |
Stents, prostatic balloon
Foley catheters |
|
|
Invasive Therapy
(BPH) |
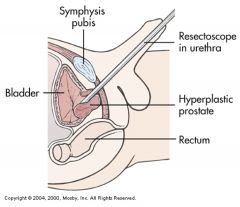
TURP
Indications: --Decrease in urine flow sufficient to cause discomfort --Persistent residual in urine --Acute urinary retention --Hydronephrosis Transurethral Resection of Prostrate (TURP) --Choice for debilitating patient with moderate prostatic enlargement --No incision, less likely to cause erectile dysfunction --Does not completely remove the prostate tissue --Bleeding is common (What medications to check pre-op?) |
|
|
Pre-operative: Assessment/Nursing Diagnoses
(TURP) |
--Pre-operative: Assessment/Nursing Diagnoses (TURP)
--Pain (? Anxiety) --Fear related to sexual dysfunction --Possible diagnosis of cancer --Knowledge deficit (surgery) --Risk of infection |
|
|
Pre-operative Nursing Interventions
(TURP) |
--Urethral catheter – to restore urinary drainage
--Coude catheter (curved tip catheter) --Filiform (rigid) --Treat urinary infection --High fluid intake (2-3 L/day) |
|
|
Post-operative: Assessment/Nursing Diagnoses
(TURP) |
--Pain related to bladder spasms
--Urge incontinence related to poor sphincter control --Potential for hemorrhage --Hyponatremia |
|
|
Post-operative Nursing Interventions
(TURP) |
--CBI: Use of 3 way foley catheter; removes clots, urinary drainage
--Observe for hemorrhage --24-36 hours, normal blood clots --Avoid activities that increase intra-abdominal pressure --Relieve bladder spasms --Belladonna, opium, suppositories, antispasmodics --Promote sphincter tone --Kegel’s exercise --Monitor for signs and symptoms of infection --Dietary interventions, stool softeners |
|
|
Patient Teaching
(TURP) |
--Catheter care
--Managing incontinence --Maintain adequate oral intake (2-3 L/day) --Sexual counseling ----Erectile dysfunction ----Retrograde ejaculation |
|
|
Prostate Cancer
|
--Malignant tumor of the prostate gland
--Most common form of cancer in men (1 in 5 men) ----Lifetime risk 15.9% (Howlader et al., 2011) --2nd leading cause of cancer death in men after lung cancer --Higher incidence in men > 65 years & majority of deaths after age 75 --High risk: African American men --Research: Possible link to high-fat diet & environmental factors --Androgen-dependent adenocarcinoma ----Slow growing & usually begins in the posterior or lateral portions of the prostate ----Spread to pelvic bones, femur (bones), lymph, lower spine, liver and lungs |
|
|
Clinical Manifestations
(Prostate Cancer) |
Asymptomatic in early stage
Symptoms are similar to BPH --Dysuria, dribbling, frequency, hematuria, nocturia and retention --Prostate feels hard, enlarged, and fixed on rectal exam --Pain in the lumbosacral area with radiation down the hips and legs are indicative of metastasis (? Renal calculi symptoms) --Distant metastasis & pain management issues |
|
|
Diagnostic Studies
(Prostate Cancer) |
Digital rectal exam
--Abnormal findings on rectal examination include areas of firmness, either localized (nodules) or generalized. Bogginess and asymmetry may also be noted. (+) elevated prostate-specific antigen (PSA) --Normal (0.2 – 4 ng/mL) --Mild elevation with other disorders, e.g. BPH, UTI -- > PSA » >tumor mass Trans-rectal ultrasound Prostate biopsy – confirms diagnosis CT or MRI to assess metastasis *Elevated alkaline phosphatase* indicates bone metastasis Grading & Staging (TNM classification) |
|
|
Surgical Options
(Prostate Cancer) |

Suprapubic Prostatectomy:
--Pt has co-existing problems --Suprapubic catheter & Foley catheter is inserted ----Foley catheter is removed 2-4th postoperative day ----Suprapubic tube has a greater risk for bladder spasms ----Monitor frequently for urine on dressing --Post-op CBI ----Watch for hyponatremia & seizures Retropubic Prostatectom: --No bladder incision --Catheter care ----Clean urethral meatus with soap and water ----Secure catheter --Wound serosanguinous for 4-5 days --Discharge with catheter for 3-5 days --Urinary incontinence – Kegel’s exercises --Discharge Teaching: ----No lifting heavy objects, no driving, no sex, drink 2-3 liters/day, stool softeners, high fiber in diet, walk, question about impotence |
|
|
Erectile Dysfunction
|
Inability to achieve or maintain erection for sexual intercourse
Organic vs. functional ED Assessment: --Medical, social, sexual history --Complete physical examination --Duplex Doppler ultrasonography test |
|
|
Healthy People 2020
(Cancer) |
↓ overall cancer rate
↑ proportion of cancer survivors living 5 yrs or > after dx ↑ mental & physical health-related quality of life of cancer survivors |
|
|
Urinary Tract Infection (UTI)
|
Most common health care acquired infection
Most common cause of sepsis in hospitalized patient --“Urosepsis” --Most common organisms are from GI tract --E. coli (most common) --Common source of hospital-acquired UTI (CAUTI) |
|
|
Classification
(UTI) |
Upper tract: renal parenchyma, pelvis, ureters
--Signs and symptoms: fever, chills, flank pain Lower tract: lower urinary tract --No usual systemic manifestations (localized symptoms) Sites of Infection --Pyelonephritis --Cystitis --Urethritis |
|
|
Predisposing Factors
(UTI) |
Factors increasing urinary stasis
--Intrinsic obstruction, extrinsic obstruction, urinary retention Foreign bodies --Urinary calculi, urologic instrumentation (CAUTI) Anatomical factors --Congenital defects leading to obstruction or urinary stasis, fistula exposing urinary stream to skin, vagina, or fecal stream, shorter urethra Sexual intercourse Immunosuppression Functional disorders (constipation, voiding dysfunction) |
|
|
Clinical Manifestations
(UTI) |
Symptoms
--Dysuria, frequent urination (> every 2 hours), urgency, suprapubic discomfort or pressure --Hematuria, or sediment in urine, cloudy urine --Flank pain, chills, and fever indicate pyelonephritis Older adult: --Could be asymptomatic --Non-localized abdominal discomfort rather than dysuria --May have cognitive impairment --Less likely to have fever Significant bacteriuria may have no symptoms or nonspecific symptoms like fatigue or anorexia |
|
|
Diagnostics
(UTI) |
Urinalysis (clean-catch is preferred, or catheterization or suprapubic needle aspiration)
Urine culture and sensitivity Imaging studies in some cases --IVP or abdominal CT when obstruction suspected |
|
|
Drug Therapy
(UTI) |
Trimethoprim-sulfamethoxazole or nitrofurantoin
--Used to treat empiric uncomplicated UTI ) Pyridium --OTC, provides soothing effect on urinary tract mucosa --Stains urine reddish orange Prophylactic or suppressive antibiotics --Patients with repeated UTIs --Prevent recurrence, or a single dose prior to events likely to cause UTI |
|
|
Health Promotion
(UTI) |
--Avoid unnecessary catheterization & early removal of indwelling catheters
--Aseptic technique must be followed during instrumentation procedures --Handwashing --Wear gloves for care of urinary system --Routine & thorough perineal care for all hospitalized patients --Avoid incontinent episodes by answering call light & offering bedpan at frequent intervals |
|
|
Acute Care Intervention
(UTI) |
--Instruct patient about drug therapy & side effects
--Emphasize taking full course despite disappearance of symptoms --Second or reduced drug may be ordered after initial course in susceptible patients --Instruct patient to watch urine for changes in color & consistency and decrease or cessation of symptoms --Counsel on persistence of lower tract symptoms beyond treatment or onset of flank pain or fever should be reported immediately |
|
|
Ambulatory and Home Care
(UTI) |
--Emphasize compliance with drug regimen
--Maintain adequate fluid intake --Regular voiding --Void after intercourse --Temporary discontinue use of diaphragm --Instruct on follow-up care with urine culture --Recurrent symptoms typically occur in 1-2 weeks after therapy |
|
|
Evaluation
(UTI) |
--Use of nonanalgesic relief measures
--Appropriate use of analgesics --Pass urine without urgency --Urine free of blood --Adequate intake of fluids |
|
|
Glomerulonephritis
|
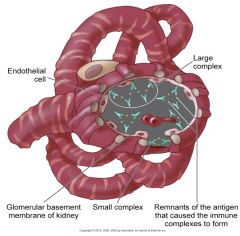
--Immunologic processes involving the urinary tract predominantly affect the renal glomerulus
--Inflammation of the renal glomeruli Classifications: --Extent of damage (Diffuse or focal) --Initial cause of the disorder (SLE, scleroderma, strep infection) --Extent of changes (Minimal or widespread) --Accumulation of antigen, antibody and complement in the glomeruli, results to tissue injury |
|
|
Acute Glomerulonephritis
|
--Patient assessment
----Connection with sore throat? ----Proteinuria --Physical assessment --Clinical manifestations --Laboratory assessment --Other diagnostic tests |
|
|
Collaborative Care
(Acute Glomerulonephritis) |
--Management of infection
--Prevention of complications --Dialysis --Plasmapheresis --Patient education |
|
|
Chronic Glomerulonephritis
|
Develops over period of 20 to 30 years or longer
Assessment Interventions: --Slowing progression, preventing complications --Diet changes --Fluid intake --Drug therapy --Dialysis, transplantation |
|
|
Urinary Tract Calculi
|

Nephrolithiasis – kidney stone disease
--Majority of cases caused by calcium stones (oxalate, phosphate) --Caucasian, 20-55 years old men Risk factors: --Metabolic --Climate --Urinary stasis --Urinary retention --Immobilization --Dehydration --Genetic --Lifestyle |
|
|
Clinical Manifestations
(Urinary Tract Calculi) |
Manifestations result from obstruction of urinary flow
--Ureterovesical junction (UVJ), common site of complete obstruction Symptoms: --Abdominal or flank pain (usually severe), hematuria, renal colic --Nausea & vomiting --Pain may be absent if stone unobstructing --Cool, moist skin --Stone near UVJ: lateral flank, testicles, labia, or groin --UTI signs and symptoms, fever, vomiting, nausea and chills |
|
|
Diagnostics
(Urinary Tract Calculi) |
Urinalysis, urine culture, IVP, retrograde pyelogram, ultrasound, cystoscopy, CT scan
Serum BUN, creatinine H & P: Use of OTC medications and dietary supplements, previous history, family history |
|
|
Endourologic, Lithothripsy or Open Surgical Stone Removal (Nephro or Pyelolithotomy)
(Urinary Tract Calculi) |
Indications:
--Stones are too large for spontaneous passage --Stones associated with bacteriuria or symptomatic infection --Stones causing impaired renal function --Stones causing persistent pain, nausea, or ileus --Inability of patient to be treated medically --Patient with one kidney |
|
|
Nursing Management
(Urinary Tract Calculi) |
Assessment
--Clinical manifestations --Subjective and objective data Nursing Diagnoses --Acute pain/Anxiety --Impaired urinary elimination --Ineffective therapeutic regimen management --Risk for infection Goals --Relief of pain --No urinary tract obstruction --Understanding of measures to prevent further recurrence of stones Implementation --Adequate fluid intake (goal: 2 L/day UO) --Measures to alleviate risk factors --Fluid intake should be advised according to persons’ activity, underlying illness, etc --Normal Ca++ diet, low animal protein, salt or both --Pain management & comfort measures --Teach patient to report spontaneous passage of stone --Encourage mobility --Safety measures, for patients experiencing acute colic, particularly if using opioid analgesics --Ice packs for bruising with lithotripsy |
|
|
Bladder Cancer
|
--Most frequent malignant tumor of the urinary tract is transitional cell carcinoma of the bladder
--Most common in men, between 60-70 years Risk factors: --Cigarette smoking --Exposure to dyes used in rubber and cable industries --Chronic abuse of certain analgesics (phenacetin) --Women treated with radiation for cervical cancer --Cylophosphamide (Cytoxan), unknown mechanism --Chronic recurrent bladder stones and chronic lower urinary tract infections --Chronic indwelling catheters (long periods) |
|
|
Clinical Manifestations & Diagnostics
(Bladder Cancer) |
--Gross painless hematuria (common finding)
--Bladder irritability with dysuria, frequency, and urgency Diagnostic studies: --Urine for cytology --Detects exfoliated cells from the bladder --IVP, ultrasound, CT or MRI --Cystoscopy- biopsy confirms diagnosis --TNM staging --Low-stage, low-grade bladder cancers are most responsive to treatments and more easily cured |
|
|
Nursing & Collaborative Care
(Bladder Cancer) |
--Prepare patient for diagnostic procedures
--History and Physical exam --Pre and post-op care --Surgical therapy ----Transurethral resection ----Laser photocoagulation ----Open loop resection ----Cystectomy ----Segmental ----Partial ----Radical --Radiation and Chemotherapy --Intravesical therapy ----Immunotherapy ----Chemotherapy |
|
|
Urinary Diversion
(Bladder Cancer) |
Performed with & without cystectomy
Indications: --Cancer of the bladder --Neurogenic bladder --Congenital anomalies --Strictures --Trauma to the bladder --Chronic infections with deterioration of renal function Types of urinary diversion surgery requiring collection devices --Ileal conduit --Cutaneous ureterostomy --Nephrostomy |
|
|
Incontinent Urinary Diversion
(Bladder Cancer) |
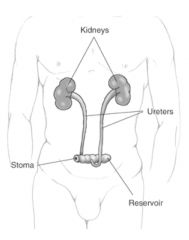
--Ileal conduit (ileal loop), most common type: 6-8 inches of ileum are converted into a conduit for urinary diversion
--Ureters are anastomosed into one end of the conduit, and other end of the bowel is brought out to the abdominal wall to form a stoma --Urine flows continuously --Requiring external collection device, requires frequent emptying --Risk for infection Teaching --Care of stoma & appliance --Increase fluid intake --Signs and symptoms of infection |
|
|
Continent Urinary Diversion
(Bladder Cancer) |
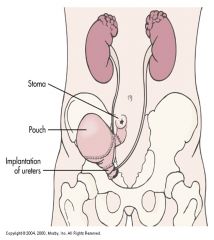
--Intra-abdominal reservoir that is catheterizable or has an outlet controlled by anal sphincter
--Internal pouches created similar to ileal conduit --Reservoirs from ileum, ileocecal segment or colon, e.g., Kock pouch --Continence mechanism formed between large, low pressure reservoir and the stoma by intussuscepting a portion of the bowel Patient Teaching --Self catheterization using strict sterile aseptic technique, every --4 to 6 hours --No external pouch |
|
|
Pre-operative: Nursing Management
(Bladder Cancer) |
--Patient teaching
--Recognize anxiety level, and fear --Patient’s family should be involved during teaching process --Social aspects of living with stoma should be included --Self-catheterization and irrigation of pouch --Explain problems of incontinence --Concerns about sexual activities should be discussed Consult enterostomal therapy RN |
|
|
Post-operative: Nursing Management
(Bladder Cancer) |
Early postoperative period priorities:
--Prevention of surgical complications such as atelectasis and shock, thrombophlebitis, paralytic ileus and small bowel obstruction --NPO --NGT may be required for 3 to 5 days --Prevention of injuries and maintaining urine output --Increase fluid intake – to “flush” the continent diversion --Explain to patient that “mucus –like” appearance in the urine is a normal occurrence Meticulous skin care around the stoma --Keep urine acidic to prevent alkaline encrustations --Stoma is expected to shrink within the first few weeks postoperatively Change appliance as needed Psychosocial support: altered body image Discharge planning/teaching --Proper fitting of appliance --Information where to purchase supplies, emergency telephone numbers, location of ostomy clubs, and follow-up visits --Measures to prevent complications and renal function deterioration |
|
|
Acute Kidney Injury (AKI)
|
Pathophysiology
Types: --Prerenal --Intrarenal --Postrenal Prerenal azotemia Causes: --Hypovolemic shock --Heart failure |
|
|
Phases of AKI
|
Rapid decrease in kidney function lead to collection of metabolic wastes in the body
Phases: --Onset --Oliguric --Diuretic --Recovery Acute syndrome may be reversible with prompt intervention |
|
|
Chronic Kidney Disease (CKD)
|
--Progressive, irreversible kidney injury; kidney function does not recover
--End-stage kidney disease (ESKD) --Azotemia --Uremia --Uremic syndrome |
|
|
Stages of CKD
|
Reduced renal reserve
Reduced GFR ESKD |
|
|
Stages of CKD Changes
|
Kidney changes
Metabolic changes --Urea and creatinine Electrolyte changes --Sodium --Potassium --Acid-base imbalance --Calcium and phosphorus Cardiac changes: --Hypertension --Hyperlipidemia --Heart failure --Pericarditis Hematologic changes GI changes |
|
|
Clinical Manifestations
(CKD) |
--Neurologic
--Cardiovascular --Respiratory --Hematologic --Gastrointestinal --Skeletal --Urinary --Skin |
|
|
Assessments
(CKD) |
--Psychosocial
--Laboratory --Imaging |
|
|
Priority Nursing Care
(CKD) |
--Dietary restrictions
--Uremic frost --Muscle strength, energy --Family members --Excess fluid volume --Decreased cardiac output --Recombinant human erythropoietin --Interdisciplinary team |
|
|
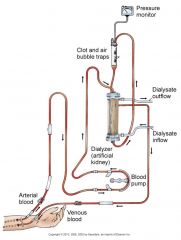
Hemodialysis
(CKD) |
--Patient selection
--Dialysis settings --Procedure --Anticoagulation |
|
|
Subclavian Dialysis Catheters
|

|
|
|
Hemodialysis Circuit
|
|
|
|
Vascular Access
(Hemodialysis) |
--Arteriovenous (AV) fistula or graft for long-term permanent access
--Hemodialysis catheter, dual or triple lumen, or AV shunt for temporary access --Precautions Complications: --Thrombosis or stenosis --Infection --Aneurysm formation --Ischemia --Heart failure |
|
|
Nursing Care
(Hemodialysis) |
--Drugs
--Postdialysis assessment --Hypotension --Headache --Nausea, vomiting --Malaise, dizziness --Muscle cramps or bleeding |
|
|
Complications
(Hemodialysis) |
--Dialysis disequilibrium syndrome
--Infectious disease --Hepatitis B & C --HIV |
|
|
Peritoneal Dialysis
(CKD) |
--Involves siliconized rubber catheter placed into abdominal cavity for infusion of dialysate
Types: --Continuous ambulatory (CAPD) --Automated --Intermittent --Continuous-cycle --Peritoneal Dialysis Exchange --Continuous Ambulatory Peritoneal Dialysis (CAPD) |
|
|
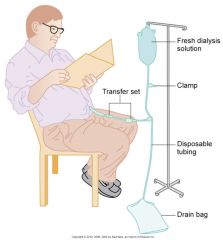
Continuous Ambulatory Peritoneal Dialysis (CAPD)
(CKD) |

|
|
|
Automated Peritoneal Dialysis
(CKD) |
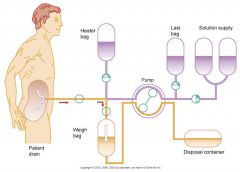
|
|
|
Complications
(Peritoneal Dialysis) |
--Peritonitis
--Pain --Exit site/tunnel infections --Poor dialysate flow --Dialysate leakage --Other complications |
|
|
Nursing Care
(Peritoneal Dialysis) |
--Before treatment—evaluate baseline vital signs, weight, laboratory tests
--Continually monitor patient for respiratory distress, pain, discomfort --Monitor prescribed dwell time, initiate outflow --Observe outflow amount and pattern of fluid |
|
|
Kidney Transplantation
|
--Candidate selection criteria
--Donors --Preoperative care --Immunologic studies --Surgical team --Operative procedure |
|
|
Transplanted Kidney
|
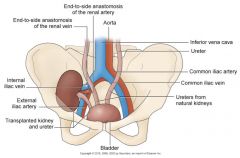
|
|
|
Postoperative Care
(Kidney Transplant) |
--Urologic management
--Assessment of hourly urine output x 48 hr Complications: --Rejection --Acute tubular necrosis --Thrombosis --Renal artery stenosis --Other complications --Immunosuppressive drug therapy --Psychosocial preparation |

