![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
54 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
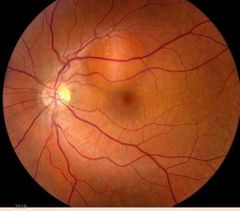
What is the diameter of the macula? |
5 mm |
|
|
|
Where is the macula located? |
4mm temporal 0.8mm inferior to the disc |
|
|
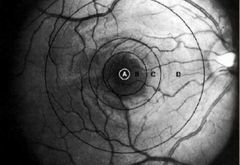
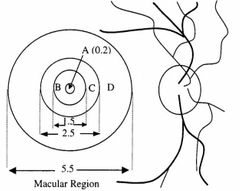
Macula region |
Macula region |
|
|
|
What is the prevalence of AMD for those aged 65-74 yrs? |
11% |
|
|
|
What is the prevalence of AMD for those aged 75-85 yrs? |
28% |
|
|
|
What are the risk factors for AMD? |
• Smoking • Diet • Aspirin • Race- whites>blacks • Gender- F >M • Age • Hypertension • Sun • Nutrition |
|
|
|
What are the ocular risk factor for AMD? |
• Refractive error • Len opactities • Aphakia |
|
|
|
What are the two forms of AMD? |
• Non- exudative/ atrophic DRY • Exudative WET |
|
|
|
What is/describe dry AMD? |
• Most common (85-90%) • Geographic atrophy • Usually Bilateral, slower • Choriocapillaris, RPE, Photoreceptors |
|
|
|
What is/describe wet AMD? |
• Neo-vascularisation • Causes more devastating and sudden vision “loss”’ aggressive, more quickly • Choroidal NV ,Serous or haemorrhagic neurosensory or RPE detachment |
|
|
|
What is the pathogenesis of AMD? |
• Genetic predispositions • Lipofuscinogenesis (with its linkage to oxidative stress) • Drusogenesis • Inflammation • Neovascularization (wet form) |
|
|
|
Give a summary of how drusen can lead to AMD? |
• Age-related thickening of Bruch’s membrane • Interferes with photoreceptor/RPE metabolism • Causing deposition of metabolites / formation of drusen • Damage to overlying RPE/photoreceptors and underlying choriocapillaris |
|
|
|
What is drusen? |
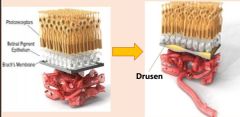
• Earliest clinical sign (AMD)
• Lipid or collagen deposits (metabolic waste)
• Lie between Bruch’s membrane and RPE
|
|
|
|
What does drusen cause/do? |
• Further disruption of RPE/photoreceptor metabolism
• Cause variable amount of depigmentation and eventually atrophy of overlying RPE |
|
|

What is HARD drusen? |
• Small localised collection of hyaline material within or on Bruch’s membrane
• Sharp, well demarcated boundaries |
|
|
What is SOFT drusen? |
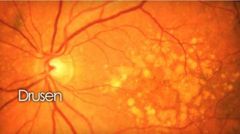
• Involve overlying focal RPE detachment • Poorly demarcated boundaries >63 um (fluffy) • Larger/commonly become confluent |
|
|
|
What are the sizes of small, intermediate and large drusen? |
• Small: <63 µ (usually Hard)
• Intermediate: 63-124 µ (usually soft)
• Large: >125 µ |
|
|
|
What does membranous drusen look like? |
• 63-175 µ • Pale, shallow appearing drusen
|
|
|
|
How does Granular drusen appear?
|
• About 250 µ • Solid appearing drusen
|
|
|
|
How does Serous drusen look like?
|
• >500 µ • Serous fluid • Blister like appearance |
|
|
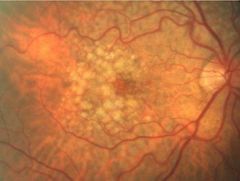
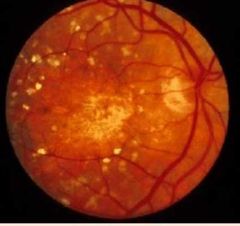
What is this? |
Confident drusen |
|
|
|
What is confident drusen? |
Associated with soft drusen • Widespread RPE abnormality • Increase risk of vision loss |
|
|
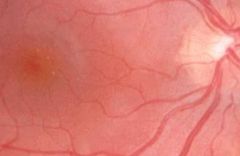
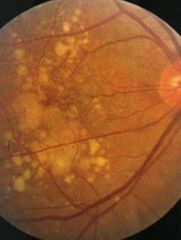
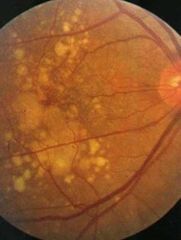
What is this? |
Calcified drusen |
|
|
|
What is calcified drusen? |
• sharply demarcated, glistening, refractile lesions associated with RPE atrophy. |
|
|

What is this? |

RPE degeneration |
|
|
|
What is RPE degeneration? |
•Focal areas of hypo- and hyper- pigmentation (‘stippling’)
•Leads to neurosensory atrophy revealing underlying choriocapillaris
|
|
|
|
What is the end stage of RPE degeneration? |
Geographic atrophy |
|
|
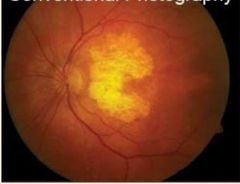
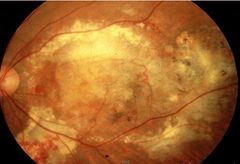
What is this? |

Geographic atrophy |
|
|
|
What is geographic atrophy? How can it arise? |
• Soft drusen present in early stages (significant risk factor for GA – due to RPE detachment)
• Decreased retinal thickness and increased visualisation of choroidal vessels
• Sharply demarcated pale area
• Choroidal vessels sometimes white |
|
|
|
What ia non-exudative AMD? |
Gradual mild to moderate impairment over months or years |
|
|
|
What is the cause of non-exudative AMD? |
• Slow/progressive atrophy of RPE and photoreceptors or • Collapse of an RPE detachment overlying soft drusen |
|
|
|
What is an advanced form of non-exudative AMD? |

Geographic atrophy |
|
|

What is this? |
Exudative AMD |
|
|
|
What is exudative AMD? |
•Choroidal neo-vascularisation •Exudative detachment of RPE and/or retina •Disciform scar |
|
|
|
What is Choroidal neo-vascularisation? |
• Proliferations of fibrovascular tissue from choriocapillaris through defects in Bruch’s membrane
• Formation of a subretinal/choroidal neovascular membrane (SRNVM/CNVM) • Fibrous tissue proliferation – scar development (Disciform scar) - Permanent vision loss |
|
|
|
What do SRNVM tend to do? |
Tendency to leak • Serous and blood • Distorted or blurred vision • Red if sub-retinal, darker if sub-RPE • Rarely vitreous haemorrhage |
|
|
|
What occur from leaking SRNVM? |
Retinal detatchments |
|
|
|
CNV lesion is well demarcated & its location may be determined by what? |
closest point to the foveal avascular zone (FAZ) |
|
|
|
State the CNV lesion location classifcation. |
• Subfoveal: under the centre of FAZ • Juxtafoveal: 1-199 µm from the centre of FAZ • Extrafoveal: >200 µm & <2500 µm from the centre of FAZ |
|
|

What are the types of CVN? |
Type I: CNV beneath RPE Type II: CNV above RPE |
|
|
|
Membrane terminology- Classic |
Classic – Early leakage from edge of membrane |
|
|
|
Membrane terminology- Occult type 1 |
Occult type 1 - fibrovascular. |
|
|
|
Membrane terminology- Occult type 2 |
Occult type 2- Undetermined leakage |
|
|
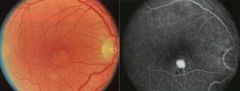
What is exudative AMD Classic CNVM? |
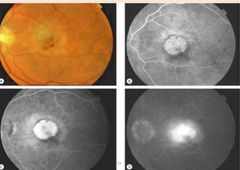
(30% of CNVM) • Pattern is mainly differentiated by FA findings • Early phase reveals staining of a well demarcated lesion. •Late phase reveals leak, at times beyond the lesion borders. |
|
|
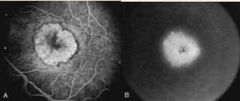
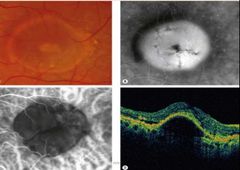
What ia this? |
Exudative AMD Ocult CNVM Type I Fibrovascular |
|
|
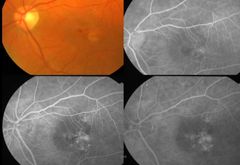
What is this? |
Exudative AMD Ocult CNVM Type II late leakage of undetermined source |
|
|
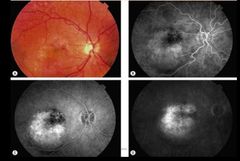
What is this? |
Wet disciform AMD |
|
|
|
Name the types of PED (Pigment epithelium detachment). |
• Drusenoid • Serous • Fibro vascular • Haemorrhagic |
|
|
|
What is AREDS? |
To evaluate the effect of high-dose vitamins C and E, beta-carotene and zinc formulations on age-related macular degeneration (AMD) progression and visual acuity. |
|
|
|
What is the main treatment for wet ARMD? |
Antiangiogenic drugs (VEGF) |
|
|
|
What is Vascular endothelium growth factor (VEGF)? |
• A naturally occurring protein • Stimulates angiogenesis • Proinflammatory |
|
|
|
What role does (VEGF) play on exudative AMD? |
• Stimulates angiogenesis of choroidal blood vessels into the retina beneath the macula. • Angiogenesis begins with vasodilatation and increases in vascular permeability, followed by activation and proliferation of vascular endothelial cells. |
|
|
|
What does Anti-VEGFs do? |
reduce the growth of new blood vessels, decrease the leakage through them. |
|
|
|
Name some anti-VEGF drugs. |
• Bevacizumab (Avastin) • Ranibizumab (Lucentis) • Pegaptanib sodium (Macugen) • Aflibercept (Eylea) • Anecortave acetate (Retaane) - (modified steroid) |
|

