![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
115 Cards in this Set
- Front
- Back
|
Name 5 steps of passage of oxygen from the air to the tissues.
|
1. The air goes from the air into the lungs.
2. Air goes out of the lungs and into the blood. 3. Transport of oxygen by the haemoglobin. 4. Getting oxygen off the haemoglobin into the tissue. 5. Oxygen enters the cell specifically into the mitochondria and peroxisomes. |
|
|
What does Boyle's law states?
|
Boyle's law states that lungs have to change their volume in order to change pressure and perform respiration. So during breathing out the volume of lungs decreases and therefore the pressure in them increases to a bit higher than atmospheric one (to 761mmHg), and the air flows out of the lungs (from higher to lower pressure). The opposite happens during inspiration. Lungs volume increase, pressure inside decrease to 759 mmHg, the air flows in.
|
|
|
Name four basic pressures involved in respiration of the lungs.(Two pressures pull the lungs away from the thoracic wall and two others prevent lungs from collapsing.)
|
Atmospheric pressure (760mmHg);
Intrapulmonary pressure (759-761mmHg); Intrapleural pressure (4 mmHg less than intrapulmonary pressure); Transpulmonary pressure (intrapulmonary pressure - intrapleural pressure) - it offsets elasticity and surface tension in lung. |
|
|
Name restrictive disorders of the lungs, difficulties in pressure change.
|
Scar tissue,
Mucous, Fluid, Reduced surfactant. Inability to contract lung - emphysema. |
|
|
Name obstructive disorders, difficulties in flow.
|
Tumours and asthma.
|
|
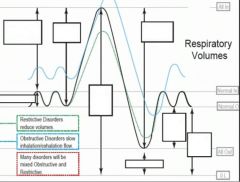
Label the respiratory volumes in the graph.
|
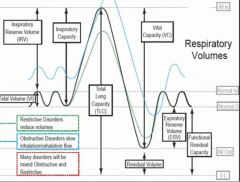
|
|
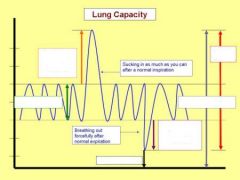
Label the lung volumes graph.
|
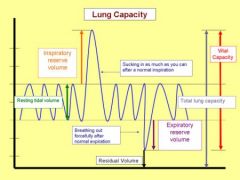
|
|
|
What is tidal volume and its typical value?
|
Tidal volume is the lung volume representing the normal volume of air displaced between normal inspiration and expiration when extra effort is not applied. Typical values are around 500ml.
|
|
|
Which lung volumes can be measured directly with a spirometer?
|
The tidal volume, vital capacity, inspiratory capacity and expiratory reserve volume can be measured directly with a spirometer.
|
|
|
What is Expiratory reserve volume?
|
expiratory reserve volume the maximal amount of gas that can be exhaled from the resting end-expiratory level. Abbreviated ERV.
|
|
|
What is Inspiratory reserve volume?
|
Inspiratory reserve volume the maximal amount of gas that can be inhaled from the end-inspiratory position.
|
|
|
What is minute volume?
|
minute volume (MV) the quantity of gas exhaled from the lungs per minute; tidal volume multiplied by respiratory rate.
|
|
|
What is the name of the amount of gas remaining in the lung at the end of a maximal exhalation.
|
Residual volume.
|
|
|
What is the name of the volume of gas inhaled and exhaled during one respiratory cycle.
|
Tidal volume.
|
|
|
What is the name of the volume of air remaining in the lungs after a maximal expiratory effort.
|
Residual volume.
|
|
|
What is the name of the volume of air present in the lungs, specifically the parenchyma tissues, at the end of passive expiration.
|
Functional Residual Capacity (FRC).
|
|
|
What is the name of the maximum amount of air a person can expel from the lungs after a maximum inspiration.
|
Vital capacity.
|
|
|
What gives us the power to expire?
|
Expiration is mainly due to the natural elasticity of the lungs, which tend to collapse if they are not held against the thoracic wall. This is the mechanism behind lung collapse if there is air in the pleural space (pneumothorax).
|
|
|
What controls breathing?
|
Ventilation occurs under the control of the autonomic nervous system from parts of the brain stem, the medulla oblongata and the pons.
|
|
|
What is RQ?
|
Respiratory quotient Co2 output/O2 uptake.
|
|
|
what does the spirometer measure?
|
Static volumes of the lungs.
|
|
|
what does the tidal volume include?
|
The air that fills the the alveoli plus the air in the airways.
|
|
|
How large is usual inspiratory reserve volume?
|
About 3 L.
|
|
|
How large is usual ERV?
|
1,2 L
|
|
|
How large is usual RV?
|
1,2 L
|
|
|
Name lung volumes.
|
TV, IRV, ERV, RV.
|
|
|
Name lung capacities and what each of them includes (which lung volumes).
|
IC = TV+IRV (3,5L)
FRC = ERV+RV (2,4L) VC = IC+ERV = TV+IRV+ERV (4,7L) TLC = VC+RV (5,9L) All the lung volumes put together. |
|
|
Name and explain two methods of measuring FRC.
|
1. Helium dilution. Person breaths in known amount of helium, which is insoluble in blood. After some time the amount of helium in the lungs equals the amount of helium in the spirometer, which can be measured. The amount of helium that was added to the spirometer and its concentration in the lungs are used to back-calculate the lung volume.
2. The body plethysmograph. Uses the Bayle's law about the constancy of gas' pressure vs. volume. If the volume increases, the pressure decreases, and visa versa. So the subject is connected to the plethysmograph (large airtight box) and inspires, the pressure in the box is calculated and from it FRC is calculated. |
|
|
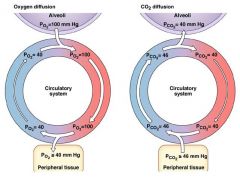
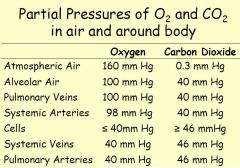
What is the normal values for PaO2? Partial pressure of oxygen in the arterial blood?
|
100 mmHg
|
|
|
What is the normal values for PaCO2?
|
40 mmHg
|
|
|
What is the normal values for PvO2?
|
40 mmHg
|
|
|
What is the normal values for PvCO2?
|
46mmHg
|
|
|
What is the normal values for partial pressure of oxygen in dry inspired air?
|
160mmHg
|
|
|
What is the normal values for partial pressure of CO2 in dry inspired air?
|
0 mmHg
|
|
|
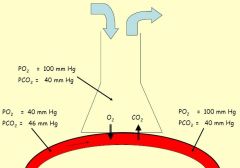
What is the normal values for partial pressure of oxygen in alveolar air? PAO2
|
100mmHg
|
|
|
What is the normal values for partial pressure of CO2 in alveolar air? PACO2
|
40mmHg
|
|
|
What is the capacity of the Physiologic dead space?
|
150 ml
|
|
|
What is the volume of FVC expired in 1 second?
|
- None
|
|
|
What is the value for the water vapour pressure?
|
47mmHg (in 37 degrees temperature)
|
|
|
What is the solubility of oxygen in blood?
|
0.003ml/100ml blood/mmHg
|
|
|
What is the solubility of CO2 in blood?
|
0.07ml/100ml blood/mmHg
|
|
|
What is the concentration of haemoglobin per 100 ml of blood?
|
15 g
|
|
|
What is the normal value of oxygen binding capacity of haemoglobin?
|
1.34 ml O2/ g haemoglobin
|
|
|
What is the normal value of oxygen consumption per minute time?
|
250 ml/min
|
|
|
What is the normal value of CO2 production per minute time?
|
200 ml/min
|
|
|
What is the normal value of respiratory exchange quotient (CO2 production/O2 consumption)?
|
0.8
|
|
|
Give a formula of how to calculate the residual volume (RV) using He dilution.
|
FRC = [V of spirometer x (He at the start - He at the end)]/He end.
Because: He at the start x V spirometer = He at the end x (V spirometer +FRC). And RV = FRC-ERV |
|
|
What is a dead space?
|
Is the volume of the airways that does not participate in gas exchange.
|
|
|
What is anatomical dead space?
|
The volume of the conducting airways, includes nose, trachea, bronchi, bronchioles.
|
|
|
What is the volume of the anatomical dead space?
|
150 ml
|
|
|
Why to sample the alveolar air one has to sample end-expiratory air?
|
Because first air of expiration is the air of the anatomical dead space, which has not undergone the gas exchange.
|
|
|
What is a physiological dead space?
|
Total volume of the lungs that does not participate in the gas exchange. Includes the anatomical dead space plus the functional dead space in the alveoli. Can be thought of as ventilated alveoli that do not participate in the gas exchange. usually because of ventilation/perfusion defect - ventilated alveoli are not perfused by pulmonary capillary blood.
|
|
|
How large is usual physiological dead space?
|
Usually it is nearly equal to anatomical dead space.
|
|
|
How to calculate the volume of physiological dead space? Bohr method.
|
Vd/Vt = (PACO2 - PECO2)/PACO2
where: Vd - Physiological dead space Vt - Tidal volume PACO2 - PCO2 of arterial blood PECO2 - PCO2 of mixed expired air. |
|
|
What is the ventilation rate?
|
Ventilation rate is the volume of air moved in and out of lungs per unit time.
|
|
|
How can the ventilation rate be expressed? Two ways.
|
The alveolar ventilation rate and the minute ventilation.
|
|
|
What is the minute ventilation? And how is it calculated?
|
The total rate of air movement into and out of lungs.
Minute ventilation = Tidal volume x breaths per minute. |
|
|
What is a alveolar ventilation?
|
The rate of air movement into and out of lungs excluding physiological dead space.
V'A = (VT - VD) x Breaths/min: Alveolar ventilation = (Tidal volume - Psysiologic dead space) x breaths per minute. |
|
|
How many percent of the vital capacity can be expired in the first second of the forced expiration by a healthy person?
|
80%, this is
FEV1/FVC = 0.8 |
|
|
What is FVC?
|
Forced vital capacity - the total volume of air that can be forcibly expired after a maximal inspiration.
|
|
|
Which muscles are used in breathing?
|
Inspiration: diaphragm, accessory muscles, external intercostal muscles;
Expiration (usually passive process, but during desease and exercise active): internal intercostal muscles, abdominal muscles. |
|
|
Describe the compliance in respiratory system.
|
Compliance is the measure of how volume changes as a result of a pressure change in the lungs and the chest. Thus, lung compliance describes the change in lung volume for a given change in transpulmonary pressure. Compliance = volume change per unit of force.
|
|
|
The compliance of the lungs and chest wall is inversely correlated with the elastic properties. Explain what that means.
|
The greater the amount of elastic tissue in the lungs and chest wall, the greater the elastic recoil force, but the lower the compliance.
|
|
|
What does the compliance of the lungs depend on?
|
The elasticity of the lungs and the surface tension of fluid lining the alveoli.
|
|
|
What is the surface tension of the lungs caused by?
|
The air-liquid interface formed by a thin layer of liquid of fluid lining the surface of alveoli.
|
|
|
State the law of LaPlace about the the air pressure, surface tension relationship and alveolus radius.
|
The air pressure within the alveolus is directly proportional to the surface tension and inversely proportional to the alveolus radius.
|
|
|
The law of LaPlace states that the air pressure within the alveolus is directly proportional to the surface tension and inversely proportional to the alveolus radius. That means that if the surface tension in small and big alveoli would be the same, the small ones would simply collapse into the big ones. What mechanisms prevents that from happening?
|
The alveoli walls the surfactant is present. It is more concentrated in the walls of smaller alveoli, so the surface tension there is lower than in the big ones.
|
|
|
What depends on the lung compliance and the transpulmonary pressure?
|
Lung volume.
|
|
|
In which part of the respiratory system does laminar/turbulent/transitional air flow occurs?
|
Laminar - low flow rate, occurs in the small airways;
Transitional - slightly higher flow rate, occurs in bronchial tree; Turbulent - high flow rates, occurs in the trachea (esp. in exercise). |
|
|
Give formula of calculating airway resistance.
|
R=8nl/pi r4;
where: R - resistance n - viscosity of the inspired air l - length of the airway r - radius of the airway. |
|
|
Name O2, CO2 and N2 percentage concentrations in inspired, alveolar and expired gas.
|
Inspired gas:
O2 - 20.9% CO2 - 0.03% N2 - 78% Alveolar gas: O2 - 14% CO2 - 5.6% Expired gas: O2 - 16% Co2 - 4.5% |
|
|
How to calculate the partial pressure of the dry gas?
|
Pgas = Ptotal x Fgas
e.g. if Ptotal = 760mmHg and O2 is 20.9% then PO2 = 760 x 0.209 = 159mmHg |
|
|
How to calculate the partial pressure of a gas saturated with a water vapour?
|
Pgas = (Ptotal - PH2O) x Fgas.
PH2O at body temperature = 47mmHg e.g. if Ptotal -760mmHg, O2 is 14%, then: PO2 = (760-47) x 0.14 = 100mmHg |
|
Fill in numbers.
|
|
|
Fill in numbers.
|
|
|
Fill in numbers.
|
|
|
|
What is the Perfusion?
|
Blood flow through the pulmonary capillaries.
|
|
|
State the equation for calculation of O2 uptake.
|
O2 uptake = (V insp - FO2 insp) - (V exp - FO2 exp)
If Ve=Vi=5000ml/min, FO2i=0.209 and FO2e=0.16, then O2 uptake = 5000 x (0.209 - 0.16) = 245 ml/min |
|
|
State the formula for calculating CO2 production.
|
CO2 output = (V exp x FCO2 exp) - (V insp x FCo2 insp).
F CO2 insp is usually zero. So: CO2 output = 5000 x 0.045 = 225ml/min. |
|
|
What is respiratory quotient?
|
Respiratory quotient = CO2 output/O2 uptake.
|
|
|
What is normal respiratory quotient?
|
0.8, because for 200ml CO2 produced, 250 ml O2 consumed: 200/250=0.8.
|
|
|
How can CO2 be transported in blood?
|
In solution, as a bicarbonate, and as carbamino compounds.
|
|
|
How can O2 be transported in blood?
|
In solution and in combination with Haemoglobin.
|
|
|
How much Hb is there in blood? Expressed in g/100ml of blood.
|
15 g per 100ml of blood.
|
|
|
How to calculate the amount of O2 transported in 100ml of blood? Give the equation and approximate numbers for a healthy adult.
|
O2 content = (1.34 x Hb x % saturation) + (0.003 x PO2) ml O2/100ml blood.
Hb is 15g/100 ml blood PaO2 = 100 mmHg So for arterial blood = (1.34 x 15 x 0.99) + (0.003 x 100) = 20.2 ml/100 ml blood. |
|
|
How does the upload of O2 to Hb changes if the affinity of Hb for O2 increases?
|
Affinity increases - upload increases.
|
|
|
How does the unload of O2 from Hb changes with the decrease in affinity og Hb for O2?
|
Decrease in affinity - unload increase.
|
|
|
Which factors affect the affinity of Hb for O2?
|
Affinity decreased by an increase in:
Temperature [H+] CO2 * Changes that occur in the metabolically active tissue. |
|
|
What is hypoxia and what causes it?
|
Hypoxia is a pathological condition in which the body as a whole (generalized hypoxia) or a region of the body (tissue hypoxia) is deprived of adequate oxygen supply.
Caused by: A low PO2 in the blood; A reduced ability of blood to carry O2 (e.g. anaemia); A reduction in tissue blood flow by local abstraction; Loss in ability of the tissue to utilise available O2 (e.g. cyanide). |
|
|
In which state the most of CO2 is carried in the blood?
|
In the state of HCO3-, almost 90% of total CO2.
|
|
|
Present the production of HCO3- from CO2.
|
CO2 + H2O <=>H2CO3 <=> H+ + HCO3-
First reaction is catalysed by the enzyme carbonic anhydrase. Both reactions are reversible. |
|
|
Name four ways of control of respiration.
|
Automatic control, basyc respiratory rhythm;
Voluntary control; Mechanisms that adapt breathing rate to the needs of the body; Reflexes. |
|
|
Where does the basic respiratory rhythm arise?
|
In the medulla.
|
|
|
What does suppress activity of inspiratory neurones?
|
Expiratory neurones.
|
|
|
What are inspiratory neurones?
|
Neurones that stimulate motor neurones and nerves that cause contraction of the inspiratory muscles.
|
|
|
What is the ventilation/perfusion ratio?
|
It is the ratio of alveolar ventilation / pulmonary blood flow: V'/Q'. Usually 0.8.
|
|
|
Which respiratory group is involved primarily in inspiration?
|
Dorsal respiratory group.
|
|
|
Which respiratory group is involved in both inspiration and expiration?
|
Ventral respiratory group.
|
|
|
Name two parts of the medulla which are associated with respiration.
|
Ventral and dorsal respiratory groups.
|
|
|
Which parts of the brain are involved in control of respiration?
|
Pons and the medulla.
|
|
|
Which two centres are there in the pons of the brain?
|
Apneustic and pneumotaxic centres.
|
|
|
What is the work of apneustic centre of the pons in respiration?
|
Apneustic centre of the pons stimulates the dorsal respiratory group, that is inspiration.
|
|
|
What is the work of pneumotaxic centre of the pons in respiration?
|
Pneumotaxic centre acts on apneustic centre to inhibit it;
it controls inhalation time. |
|
|
Name two zones of respiratory system.
|
Conducting zone and respiratory zone.
|
|
|
Which structures does respiratory zone of the respiratory system include? (3)
|
Respiratory bronchioles, alveolar ducts, alveolar sacs.
|
|
|
Which structures does conducting zone of the respiratory system include? (7)
|
Nose, nasopharynx, larynx, trachea, bronchi, bronchioles, terminal bronchioles.
|
|
|
Breathing is controlled by the levels of what?
|
CO2 and H+ in the blood.
|
|
|
Where are the levels of H+ and CO2 measured in the body for controlling respiration?
|
Chemoreceptors in the carotid arteries in the neck and in the aorta.
|
|
|
Breathing is controlled by the levels of what?
|
CO2 and H+ in the blood.
|
|
|
How large is total lung capacity in a healthy adult human?
|
6 L
|
|
|
Where are the levels of H+ and CO2 measured in the body for controlling respiration?
|
Chemoreceptors in the carotid arteries in the neck and in the aorta.
|
|
|
How large is total lung capacity in a healthy adult human?
|
6 L
|
|
|
What is the ideal ventilation/perfusion ratio?
|
1
|
|
|
What are the differences in ventilation/perfusion ratios between different parts of the lung?
|
In the apex of the lung the V'/Q' ratio is highest, and in the base of the lung it is lowest.
|
|
|
What are the differences in blood flow in different parts of the lung?
|
Blood flow in the apex of the lung is lowest and is highest in the base of the lung.
|

