![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
21 Cards in this Set
- Front
- Back
|
How is blood hypovolemia relieved? |
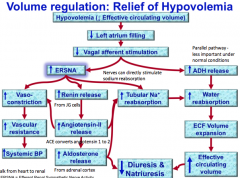
- Decreased vagal afferent pathway stimulates efferent renal sympathetic nerve activity (ERSNA) - ERSNA stimulates vasoconstriction; renin release and subsequent AT-II and aldosterone release; and acts directly on the tubular epithelium to increase sodium absorption |
|
|
How is blood hypervolemia relieved? |
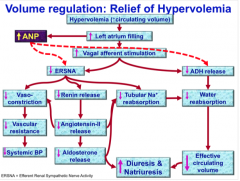
- Key difference is release of ANP from left atrium - ANP acts to decrease efferent renal sympathetic nerve activity and decrease ADH release |
|
|
What are some differences between osmoregulation and volume regulation? |
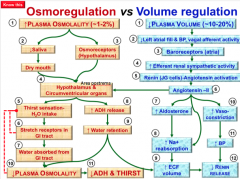
- One detects plasma osmolality, the other plasma volume - Osmolality is detected in the hypothalamus and circumventricular organs, while volume is detected by baroreceptors in the atria and carotid - Osmolality uses aldosterone and thirst to fix it - Volume uses sympathetic NS, RAAS and ANP to fix - Osmoregulation affects water excretion, thirst - Volume regulation affects sodium excretion and ECF volumes |
|
|
Where is glucose reabsorbed? |
In the PCT |
|
|
How does the PCT pick up proteins? |
Endocytosis |
|
|
How does the PCT pick up glucose? |
Sodium glucose like transporter (SGLT1) (Absorption of AAs and other stuff is also paired with sodium) |
|
|
What is the renal threshold? |
When reabsorption reaches the tubular capacity for glucose (Tm) and glucose starts appearing in the urine (osmotic diuresis - polyuria - a sign of diabetes mellitus)
It is about 180mg/dL |
|
|
What stimulates and inhibits HCO3- reabsorption/proton secretion in the PCT? |
Stimulate: Angiotensin-II Inhibit: Acetozolamide (diuretic) |
|
|
Which transporter is unique to the ascending limb? What can act on this transporter? |
The triple transporter of Cl-, Na + and K+ on the apical side.
Stimulation: Angiotensin II and ADH Inhibition: Furosemide and Bumetanide (=diuretics) |
|
|
Is the ascending limb permeable to water? |
No |
|
|
Why is K unique in the tubular epithelium? |
It is freely reabsorbed or secreted. (However, this in under the influence of aldosterone.) |
|
|
What is the counter current multiplier? |
Henle's loop: creates a gradient for urine concentration - Water reabsorbed in descending limb: concentrates urine - NaCl reabsorbed on its way back up: deconcentrates urine again |
|
|
What is the counter current exchanger? |
The vasa recta - slow blood flow and permeable to both solutes and water - helps maintain gradient |
|
|
How does urea get recycled in the kidney? |
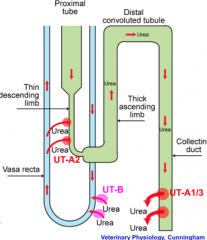
1. Urea is reabsorbed at IMCD (inner medullary collecting duct) via UT-A1 and UT-A3 2. Urea diffuses down concentration gradient into descending vasa recta via UT-B 3. Urea diffuses into descending loop of Henle via UT-A2 4. Ascending limb, DCT and cortical/outer medullary CD are all impermeable to urea - so urea from descending loop recycled to IMCD 5. ADH stimulates urea reabsorption by IMCD to increase medullary osmotic pressure and increase water reabsorption |
|
|
Where would you find type A urea transporters? Type B? |
Type A: nephrons Type B: vessels |
|
|
What do angiotensin II and aldosterone target in the DCT? |
They stimulate Na/Cl importer. |
|
|
Why is it important in the ascending limb, DCT and collecting duct to reabsorb lots of ions/electrolytes/etc? |
Because then lots of water will come when it gets to the collecting duct.
Water comes in via aquaporin 2, in principle cells |
|
|
Where does ADH target on the collecting duct principle cell? |
The aquaporins - encourage water uptake by making more aquaporins go to the membrane. |
|
|
What is the mechanism of diabetes insipidus regarding aquaporins? |
Aquaporins are under the influence of ADH, so if there is a ADH deficiency or problems with ADH receptors, not enough water can be taken up. This would cause polyuria.
Central DI: partial or complete lack of ADH secretion from the hypothalamus Nephrogenic DI: - Primary: ADH receptor dysfunction - Secondary: decrease in number of functioning nephrons, or resistance to ADH
|
|
|
What are the types of intercalated cells in the collecting duct? |
Type A: secrete protons (acid) Type B: secrete bicarbonate |
|
|
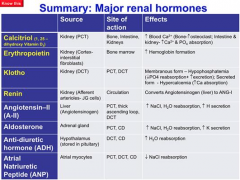
What are the major renal hormones? What are their functions? |
|

