![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
139 Cards in this Set
- Front
- Back
|
what does it seem like sex hormone binding globulin prefers to bind to? Why?
|
testosterone- why it is low in males and high in females
high in males- feminization low in females- masculinization |
|
|
what will antagonize DA besides PRL?
How do you know? |
estrogen because it inhibits it during pregnancy when you need milk production
|
|
|
What explanation would you give for magnesium's effect on PTH?
|
Mg likes to hog Ca's spot in transporters --> not as much Ca goes into parathyroid glands --> PTH is raised --> hypercalcemia
|
|
|
why do we give magnesium to coding pts?
|
to prevent Ca from going into cells and causing damage
|
|
|
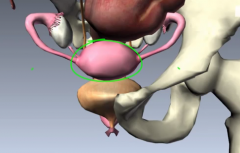
2 parts of the gonads: enclosure and endocribe cells.
role of each? what is it for males and females? |
enclosures- protects the germ line and provides selective barrier
males- seminiferous tubules females- follices endocrine- secrete hormones for germ cell dvlpmt and secondary sex characteristics Males- leydig and sertoli Females- Theca and granulosa |
|
|
besides sex hormones, what other hormones do the gonads produce?
|
inhibin and mullerian inhibiting hormone
|
|
|
what is the steroid product of sertoli cells? how do you know?
|
estrogen because they are analogius to granulosa cells
|
|
|
is there anything between the outer and inner cells?
|
YES A BASEMENT MEMBRANE BETWEEN THE 2 TYPES
|
|
|
is the main product of theca and leydig cells the same?
|
yes,
|
|
|
what is the outer cell product specifically?
|
it is androgens - androstenedione specifically
|
|
|
another name for theca cels?
|
interstitial cells
|
|
|
What enzyme is unique to the inner vs outer cells?
|
outer- 17-a hydroxylase
inner- aromatase |
|
|
3 main types of gonadal steroid? most powerful version of each?
|
progestins- progesterone
androgens- DHT estrogens- estradiol |
|
|
What is DHEA and it's strength?
|
weak androgen
|
|
|
Are post menopausal women dvoid of estrogen? what do they have? from where?
|
no, they still have estrone production from fat cells
|
|
|
what androgens are made in the ovaries? 2
|
androstenedione and DHEA
|
|
|
What enzyme does LH pump up? how do yu figue?
|
17-a hydroxylase
it stimulates theca and leydig cells which only produce up to androstenedione, meaning they have 17, but lack aromatase |
|
|
what hormone stimulates aromatase synthesis?
|
FSH
|
|
|
how is hCG able to keep the CL alive? molecularly speaking!
|
it is very similar in shape (same alpha subunit) as FSH, LH, and TSH so it can bind to the receptors on the CL
|
|
|
why do women living together tend to cycle together?
|
our GNRH neurons originated from the olfactory bulb and is influenced by phermones
|
|
|
why was this advantageous?
|
if we has a polygamist household, you can impregnate all females at once
|
|
|
pattern of GnRH release?
|
pulsatile
|
|
|
what happens if GnRH is continuous?
|
the AP gets tolerance and destroys GnRH receptors
|
|
|
what hapens if we have high vs low freq GnRH pulses?
why is this good? |
high- prfer LH
low- prefer FSH good for LH surge when estrogen is positively feeding back on the hypothalamus |
|
|
what do activin and inhibin do?
|
activin- positive feedbalk of FSH
inhibit- neg feedback |
|
|
are LH, FSH, and TSH proteins?
|
no, they are glycoproteins
|
|
|
in addition to creating aromatase, what else does FSH do in females?
|
increases maturation of the folicle
|
|
|
in addition to creating aromatase, what else does FSH do in the males? transcription
|
synthesizes androgen binding prteins to secure testosterone for spermatogensis
|
|
|
relationship of testosterone and estradiol to GnRH? 2
|
it inhibits it's efects on the AP
and it's release from the hypothalamus |
|
|
how does it inhibit GnRH in the hypothalamus?
|
it recruits endorphins which supress GnRH
|
|
|
How do most BCP's work?
|
by providing low doses of estrogen/progesterone to have a constant inhibition of GnRH so that there is never enough to ovulate with LH surge
|
|
|
if you take BCP's, will yo delaymenopause? what is the research?
|
research is conflicted? some say yes and some say no.
|
|
|
reasoning for possible delay and possible acceleration of menospuase with BCP?
|
delay- you keep your eggs
acceleration- no FSH means that fre radicals are allowed to build up |
|
|
why don't we get menses when we are young? do we have sex hormone?
|
our negative feedback is very sensitive to the low levels of sex hormones present
|
|
|
2 changes that happen to cause puberty?
|
hypothalamic neurons mature and become less sensitive to neg feedback
the pituitary is more responsive to GnRH |
|
|
do we get 2nd sex xharacteristics at puberty?
what causes it? organ? hormone? |
no, we get them several years prior when adrenal androgens go up?
|
|
|
what do gonadotropin levels look like in old age?
Why? 2 |
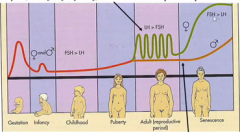
AP decrease sensitivity to neg feedback and secrete a lot
we lose follicles and thus inhbin |
|
|
what determines embryologically if you display male or female sex? why?
|
the Y chromosome because it codes for the testis determining factor
|
|
|
What does the X chromosome do for males?
|
it codes the gene for an androgen receptor which will sensitize reproductive parts to T and DHT
|
|
screw podolin and her stupid lecture style. Let's move onto DIT embryology and anatomy.
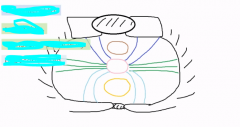
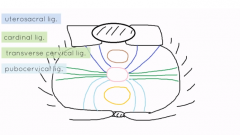
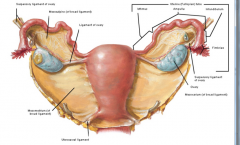
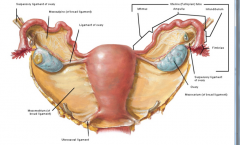
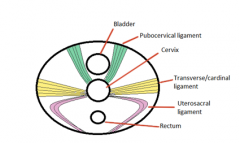
what connects the cervix to the back, side, and front of the pelvic cavity? |
|
|
|
mnemonic for cardinal ligament?
|
just imagine a bird outstretching it's wings at the cervix
|
|
|
what is the role of all these ligaments?
|
to hold up the vagina, cervix, and uterus
|
|
|
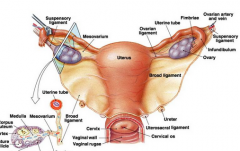
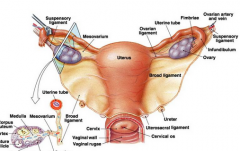
how can you think about the broad ligament?
in relation to the tubes, uterus, and ovaries? |
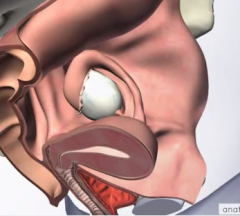
it is just the bottom of the peritoneum that the uterus and fallopian tubes rise out of like sheet
the ovaries drop down on it from above |
|
|
what other function does the broad ligament serve besides a sling?
|
it carries vessels, lymph, and nerves to the strcutures
|
|
|
where does the ureter pass in relation to the broad ligament? why does this make sense?
|

below because it is retroperitoneal!!!!
|
|
|
what are the 2 things in "water under the bridge"?
|
the ureter (water) is under the uterine artery (bridge) that is in the broad ligament
|
|
|
where is the round ligament and where does it connect?
|
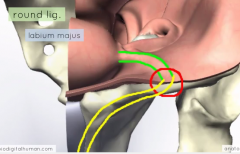
connects fundus of uterus to the inguinal canalto lead outside to the labia majoris
|
|
|
what structure in the male follows the same course as the round ligament?
|
the spermatic cord
|
|
|
how many ligaments does the ovary have?
|
2
|
|
|
which ligament is in cahoots with the round ligamanet? show and explain. what is in it?
|
just a ligament
the ovarian ligament connecting the tip of the ovary to the cornu of the uterus |
|
|
whihc side of the broad ligament does the ovary connect to?
|
the posterior side
|
|
|
What is the other ligament of the ovary and what fxn does it serve?
2 names |
the infundibulopelvic ligament/suspensory ligament of the ovary to provide lymph drai and vessels to the ovary
|
|
|
which pole of the ovary is superior vs inferior? what ligament are here?
how to visualize |
look at reproductive tract like an angry ant with ovary eyes
superior pole- lateral- suspensory ligament inferior pole- ovarian ligament |
|
|
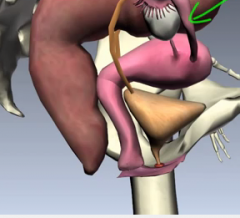
are the fallopian tubes anterior or posterior to the ovaries?
how can you tell from the broad ligament sides? |
anterior because it is on the superior surface of the broad ligament whereas the ovries rest on the posterior surface
|
|
|
where on the uterus do the tubes come out of? how do you know?
anterior or posterior? |
the fundus corners- sperm needs to travel to the far corners of the overies to get here
most anterior since uterus tilts forward |
|
|
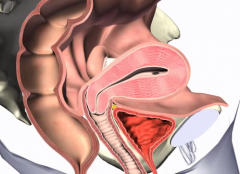
what shape is the bladder?
|
triang;e
|
|
|
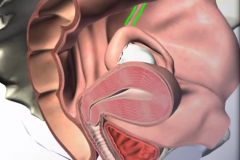
what does the pouch of douglas vs vesicouterine pouch look like?
mnemonic for how to name them |
douglas- verticle
vesiouterine- horizontal uterus is always at the second word |
|
|
why do you need to drink a lot of water before a uterine ultrasound?
|
when bladder is empty, you only see the fundus anteriorly
|
|
|
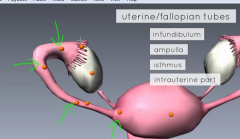
name the 4 parts of the fallopian tube in order from the ovary
|
|
|
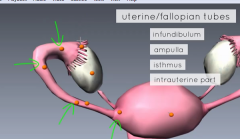
what does each term translate to? how do they relate to the anatomy and function?
|
infundibulum- funnel
ampulla- flask that funnel goes in isthmus- the narrow connecting strip after ampulla thins intrauterine- arrived indside uterus |
|
|
where does the egg get fertilized usually? why is this ideal and likely? 2 reasons
|
ampulla where you have lot of room
also it is the longest part |
|
|
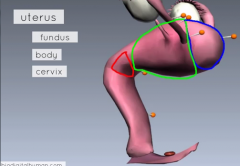
3 parts of the uterus?
|
|
|
|
what does cervix mean?
|
neck
|
|
|
is the cervix just the junction between the uterus and the vagina?
|
NO it is the bottom part of the uterus that sticks out into the vagina!
|
|
|
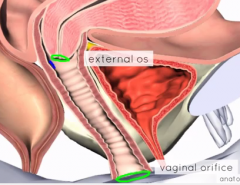
what are the 2 openings of the cervix?
|
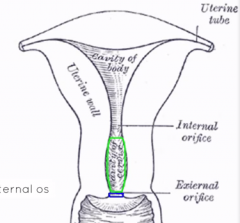
internal and external os
|
|
|
what are the fornixes created by?
how many are there? |
the recesses where the cervix goes into the vagina
roughtly 4 on all sides |
|
|
3 layers of the uterus?
|
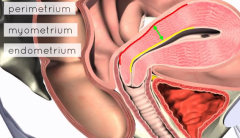
|
|
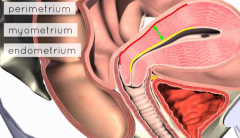
what is each layer comprised of?
|
CT
SM endothelial cells |
|
|
what happens to the layers in menses?
|
the endometrial layers thickens then sheds
|
|
|
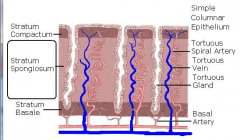
layers of the endometrium?
do they all grow and shed? which ones? |
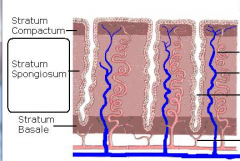
only stratum spongiosum and compactum grow and shed
|
|
|
what happens if you lose the stratum basalis layer?
some possible causes of this? |
then you get scarring and no regrowing. maybe difficult to get pregnant.
D/C can do this |
|
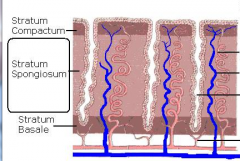
what is on the right of this?
what epithelial cell type is in the endotheium? |
|
|
|
what epithelial cell type is in the vagina?
|
stratified dsquamous into sratified squamous
|
|
|
what is it advantageous to have simple columnar in the endometrium?
|
they need to be very active (esp if there is implantation) and thus need quick access to the spiral arteries
|
|
|
what is at the ends of the vagina?
|
|
|
|
what is the vaginal vault?
|
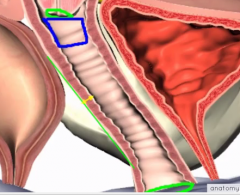
|
|
|
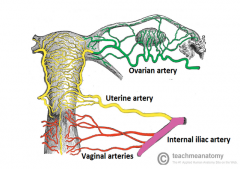
where do the ovarian arteries come fro relative to the renal arteries? left and right
what level are the renal arteries |
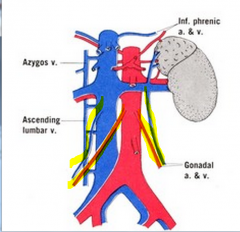
renal arteries at the transpyloric L1 level
ovarian arteries come out right below that both on the aorta |
|
|
where do the ovarian arteries come fro relative to the renal veins? left and right
|
right- IVC
left- left renal vein |
|
|
why does the left ovarian vein drain into the left renal vein?
|
the IVC is on the right
|
|
|
what structure grants safe passage of the ovarian vessels?
|
the suspensory igament
|
|
|
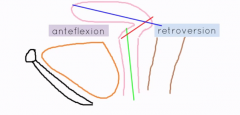
what is the axis of the cervix vs the uterus?
what angle should they make? (name and degree) |
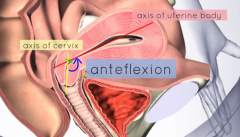
anteflexion is normally 125 degrees
|
|
|
what about the axis of the vagina and cervix?
|

anteversion- 90 degrees (more wide in the diagram)
|
|
|
what is retroflexion?
|
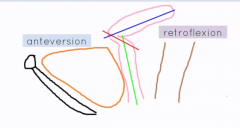
when the uterus flips toward the rectum
|
|
|
what does retroversion with anteflexion look like?
|
|
|
|
what angles are normal?
|
ante on both flexion and version
|
|
|
what vessel supplies the uterus?
what does it come off of? what ligament is it on? |
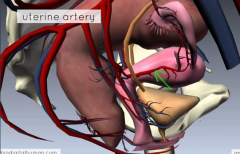
the uterine artery off the anterior division of the internal iliac artery
broad ligament |
|
|
water under the bridge imagination
|
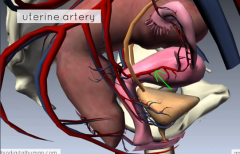
ureter passes lateral and under
|
|
|
3 parts of the broad ligament? imagine them.
|

|
|
|
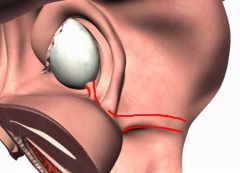
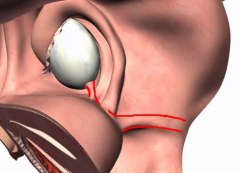
what hold up the superior, middle, and inferior uterus?
|
superior- broad ligaments inclusing suspensory and round
middle- front, back and side: uterosacral, pubocervical, and cardinal ligaments inferior-levator ani |
|
|
show how the levator ani support the lower uters/vagina
|
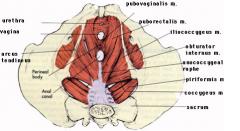
|
|
|
what did the round ligament do in embryo?
|
it was the gubenaculum pulling stuff down
|
|
|
what are the uterine horns?
|
the places where the ubes insert into the uterus
|
|
|
are the middle uterine ligaments in the back and front singulatr? how do you know?
|
no they are bilateral to get around the anus and urethra
|
|
|
at what level of the pelvis do the cardinal ligaments insert?
|
ischial spine
|
|
|
what structures are usually also removed in a hysterectomy? WHy?
|
cardinal ligaments because they house cancerous cells (resevoir) typically
|
|
|
define a secondary and primary sex organ?
|
primary- been there from birth
secondary- grow under influence of primary sex organs |
|
|
what type is the uterus?
|
secondary
|
|
|
imagine the borders of the 3 parts of the uterus
|
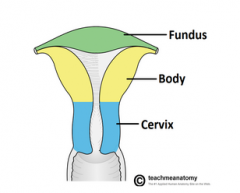
|
|
|
where does implantation tend to happen? fertilization?
|
body of uterus
ampulla of fallopian tube |
|
|
does positioning of the uterus, cervix, and vegina matter to pregancy much?
|
no
|
|
|
what kind of positioning should you be wary of and why?
|
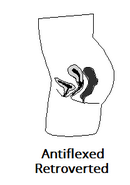
anything that places the uterus directly on top of the vagina because the excess pressure can cause prolapse under conditions of increased abdominal pressure
this or opposite, but this is more common |
|
|
how many layers is the broad ligament? why?
|
2 because it is just like the mesentary
|
|
|
does the myometrium change with the menstrual cycle?
|
no
|
|
|
when does the myometrium change and why? and how?
|
hyperplasia and hypertrophy during pregnancy to keep the baby from bursting through and to push it out in labor
|
|
|
function of stratum basalis?
|
it provides stem cels to regrow the other layes after menses
|
|
|
what effect does estrogen vs prgesterone have on the endometrium??
|
estrogen- makes it thicken
progesteron- makes it secrete stuff |
|
|
what space is infront and behind the broad ligament
|
the pouches
|
|
|
how can you imagine the emergence of the uterus to the peritoneum and the fallopian tube positions?
|

a swimmer launching straight out of the water and then coming down in front, but with broken arms tilting bacl
|
|
|
what does this explain about the vesicouterine puch?
|
why it is horzontal
|
|
|
what ligament helps to maintain the uterus in anteflexion?
|
round ligament
|
|
|
what struture carries the uterine artery and vein?
|
the cardinal ligaments
|
|
|
why would a woman get a hysteerectomy? 2
|
usually because of uterine or cervical cancer
|
|
|
major precaution to take with hysterectomies?
|
don't injure the ureters when clamping off the uterine arteries because they are super close
|
|
|
what ligament does the uterine artery travel though? kinda 2, but one definitively
|
the cardinal ligament
but it travels very close to the bottom of the broad |
|
|
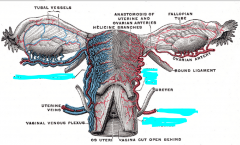
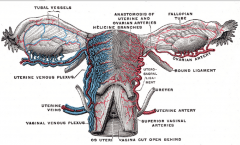
what do the capillary systems of the uterus look like? relationship with other arteries?
|
it anastamoses with the ovarian, but not vaginal
|
|
|
where is the ovarian vein? ligament and drange vein.
|
cardinal ligament again
going back to the internal iliac veins |
|
|
how do you remember what vessels come to and from the internal iliac?
|
internal iliac provide everything in the pelvic cavity above the levator ani except the ovary
|
|
|
why not the ovaries?
|
becasue the ovaries descended from above
|
|
|
what do the venous plexuses look like in the uterus/vagina? what goes into them?
|
they are very extensive and span the uterus and the top vagina
the ovaries, uterus, and vagina drain here |
|
|
|
|

what is this giant space?
|
rectouterine pouch
|
|
|
what is the most common 3 places for endometriosis?
|
fallopian tubes, ovaries, and ligaments of the uterus
|
|
|
what is a painful complication of endometrisis?
a emergency surgical one? why? |
dysmenorrhea
cysts where the ectopic lining has bled into |
|
|
can endometriosis cause infertility? how do you know?
|
yes because our pt had it.
|
|
|
what is the transformational zone? where?
|
it is the line in the cervix where the endocervical simple columnar turns into the ectocervical stratified squamous
|
|
|
cells in the ovary? epithelial
|
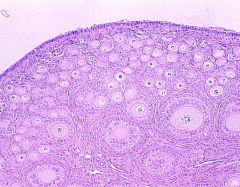
simple cubpoidal
just look at those cute little follicles! |
|
|
generally, which testicle sits higher? why?
|
right because it goes straight into the IVC and is drawn upwards with more negative pressure
|
|
|
where would ovarian and testicular cancer spread? why?
|
para aortic lymph nodes because their blood supply comes from up top there
|
|
|
what nodes would each 1/3rd of the vagina drain to?
|
outer third- inguinal nodes
inner two thirds- hypogastric, external iliac, and obturator |
|
|
describe the overall organization and connection of the lumbo-sacral plexus briefly
|
there is the lumbar and the sacral plexuses composed of the ventral and dorsal rami of each section
they are connected by the lumbosacral trunk |
|
|
describe the path of the lumbosacral trunk. show too
|
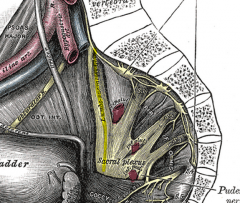
it cmes from the bottom roots of the lumbar plexus and comes down to join with the top of the sacral plexus
|
|
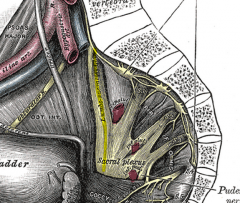
what is that up top with the lines? explain why it is there
|
the sympathetic trunk to give sympathetic stimulation to the sacral region carrying axons down from T1-L2 or something
|
|
|
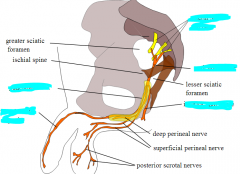
what plexus innervates the genitals? nerve?
|
sacral- pudenal nere
|
|
|
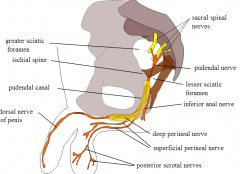
list the 3 main nerves off the pudendal from anterior to posterior. explain what each does
|
1. dorsal nerve of the penis/clitoris
2. perineal nerve- innervates posterior scrotum and posterior labia 3. inferior rectal/anal nerve- the anus and all it's glory |
|
|
|
|
|
another name for pudenddal nerve
|
alcot's canal
|
|
|
where does the lumbar vs sacral plexus innervate
|
lumbar- the front of the thighs
sacral- butt, pelvis, and back of thigh, lower leg |
|
|
other than a epidural, how could you help relieve pain of labor?
|
do a pudendal nerve block
|
|
|
how would you do a pudendal nerve block? landmarks?
|
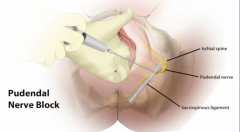
find the ischial spine through the vegina and inject an anesthetic there
|

