![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
188 Cards in this Set
- Front
- Back
|
What do the following embryological structures develop into in male and female?
1. Genital tubercle 2. Urogenital sinus 3. Urogenital folds 4. labio-scrotal swelling |
1. Genital tubercle
male: Glans penis, corpus cavernosum/spongiosum female: vestibular bulb 2. Urogenital sinus male: bulbourethral glands (of Cowper), prostate gland female: greater vestibular glands (or Bartholin), urethral and paraurethral glands (of skene) 3. Urogenital folds male: ventral shaft of penis (penile urethra) female: labia minor 4. labio-scrotal swelling male: scrotum female: labia majora |
|
|
Define CIN III in terms of dysplasia.
|
correlate with severe dysplasia and carcinoma-in-situ
|
|
|
Low risk HPV causes what? What types are low risk HPV?
|
Causes genital warts (condyloma acuminatum)
type 6, 11 |
|
|
What is koilocytosis? Where do you see this?
|
perinuclear vacuolization due to HPV cytopathic effect
seen in condyloma cuminatum |
|
|
Describe microscopic morphology of condyloma cuminatum.
|
hyperkeratosis, koilocytosis, parakeratosis of the external genitalia and perianal area.
|
|
|
What are 4 original sites of ovarian tumor? Which is most common?
|
Surface epithelial cells (Mullerian): most common
Germ cells sex-cord stroma metastasis to ovary |
|
|
List 6 mullerian epithelial ovarian tumors. Which one is most common?
|
serous: most common
mucinous Endometriod clear cell brenner tumor cystadenofibroma |
|
|
List 4 ovarian germ cell tumors
|
teratoma
dysgerminoma endodermal sinus tumor choriocarcinoma |
|
|
List 3 sex cord stromal tumors in ovary.
|
Fibroma, thecomas
Granuloca-theca cell tumor Leydig-Sertoli cell tumor |
|
|
What is the name of the ovarian tumor containing signet ring cells?
Where is it commonly from? Unilateral or bilateral? prognosis? |
Krukenberg tumor
metastasis from GI; most commonly stomach bilateral 80% poor diagnosis; most die within 2 years |
|
|
What embryological structure develops into male internal genitalia? What are they?
What transcription factors are responsible for this? (4) |
Wolffian duct
Seminal vesicles, epididymis, ejaculatory duct, ductus (vas) deferens mainly SRY; SF1, DAX1, and SOX9 |
|
|
What embryological structure develops into female internal genitalia? What are they?
|
Mullerian duct
fallopian tube, uterus, upper 1/3 vagina |
|
|
What is the clinical significance of mesothelial cysts?
|
many tumors arise from the epithelial cells of the cyst.
|
|
|
borderline ovarian Serous cystaadenoma progressing to low grade carcinoma is associated with what oncogene?
|
K-RAS oncogene
|
|
|
What is the most common invasive malignant tumor of the female genital tract?
What is endometriosis? |
endometrial adenocarcinoma (type II serous carcinoma)
Endometriosis is the presence of endometrial tissue outside the uterus. |
|
|
Describe the gross histology of endometriosis.
What cancer is commonly associated with it? |
Characterized by cyclical bleeding from ectopic endometrial tissue resulting in blood-filled "chocolate cyst"
associated with endometriod tumors (15-20%) |
|
|
A 70 YO woman with obesity presents with abnormal vaginal bleeding. Her Hx reveals infertility, menopause at 65. A biopsy of the uterine tissue reveals histology of well-differentiated, superficially invasive endometrial cancer.
What type of endometrial cancer is it? prognosis? why? What genes can be mutated in this cancer? |
Type 1 (endometrioid) endometrial adenocarcinoma
good prognosis b/c the tumor is estrogen dependent and sensitive to progesterone therapy PTEN, K-RAS, DNA mismatch repair |
|
|
Which type of endometrial adenocarcinoma has poorly differentiated histology?
Which gene can be mutated? prognosis? why? |
type II endometrial adenocarcinoma (serous carcinoma)
mutation in p53 poor prognosis due to Estrogen-independent tumor and unresponsive to progestin therapy |
|
|
what is the most important prognostic factor in endometrial cancer?
|
Invasion of the myometrium
|
|
|
How is the prognosis and histology different b/t adenocarcinoma with squamous differentiation and adenosquamous carcinoma of the uterus?
|
adenocarcinoma with squamous differentiation: the presence of benign squamous cells; better prognosis
adenosquamous carcinoma: presence of malignant squamous cells; poorer prognosis |
|
|
What is the most common "pure" ovarian germ cell tumor?
"Pure" ovarian germ cell malignancy? Is "pure" neoplasm more common than mixed tumor in the ovary? |
"pure" ovarian germ cell neoplasm? mature (benign) cystic teratoma or dermoid cyst
"Pure" ovarian germ cell malignancy? dysgerminoma yes, "pure" neoplasms are more common than mixed tumors in the ovary. |
|
|
What is the most common "pure" testicular germ cell tumor?
Which is more common tumor in the testes? mixed or pure? |
seminoma
mixed tumors are more common in the testis |
|
|
What tumor contains mature hair, sebum, teeth and located int he ovary? In what age group is this tumor common?
|
Mature (benign) cystic teratoma or dermoid cyst
in reproductive age group |
|
|
How is the behaivor of mature solid teratoma vary depending on the age group?
|
adults: malignant
children: benign |
|
|
What is struma ovarii? What type of tumor is this? What hormone is increased in the serum?
What is the name of a similar condition that secretes serotonin? |
It's a monodermal teratoma that has mature thyroid tissues and secrete thyroid hormones
Ovarian carcinoid. |
|
|
This tumor is most common ovarian germ cell malignancy and contains large, clear cells with mild dysplasia. What tumor is this? What other cells are commonly present?
|
dysgerminoma
presents with stromal septal T lymphocytes |
|
|
A tumor shows histomorphology of Schiller-Duval bodies. What tumor is this? What is elevated in the serum?
|
Yolk sac tumor
AFP is elevated |
|
|
What are 2 cytological components of germinal choriocarcinoma? prognosis?
|
Cytotrophoblasts and syncytiotrophoblasts
poor prognosis and does not respond well to chemotherapy |
|
|
What Mullerian epithelial derived ovarian tumor is 65% bilateral? mostly unilateral (2)?
|
bilateral: serous tumors
unilateral: Mucinous tumors and Brenner tumor |
|
|
What are 2 types of functional cysts of the ovary? Where do they develop from?
|
Follicular cystsfrom graafian follicles
Corpus luteum cysts from the corpus luteum |
|
|
A 40 YO female presents with abdominal mass. The biopsy and hisotlogy reveals mutilobulated tumor with pseudomyxoma peritonei?
What is the dx? is the tumor most likely to be benign or malignant? Unilateral or bilateral? |
Mucinous tumor (mullerian epithelial derived)
most likely to be benign and unilateral. |
|
|
What is androblastoma? Where is it seen?
|
Sertoli-Leydig cell tumor of ovary
|
|
|
What are crystalloids of Reinke? What tumor is it found in?
What hormones does this tumor secrete (3)? What are clinical manifestations in young boys? adult males? |
They are cytoplasmic crystals in Leydig cells found in Leydig cell tumor.
can secretes androgen, estrogens, and/or corticosteroids. Young boys: precocious puberty adult males: gynecomastia |
|
|
What are Call-Exner bodies and what tumor is it found in?
Describe the behavior and malignant potential of this tumor. |
They are formed by granulosa cells surrounding eosinohpilic material and resemble immature follicles.
They produce estrogen (potential large amount) and can be malignant 5-25% of the time. |
|
|
Name 3 tumors of ovary/testis that can secrete estrogen.
|
Granulosa cell tumor
Leydig cell tumor Thecomas |
|
|
What is Meig's syndrome? What tumor is it associated with?
|
Associated with fibroma or fibroma-thecoma
Defined as the triad of benign ovarian tumor, ascites, and pleural effusion. |
|
|
what hormone promotes early division of the spermatogonia?
|
growth hormone
|
|
|
What cell secretes androgen-binding protein (ABP)?
|
Sertoli cells
|
|
|
How does your body protect sperm from autoimmune attack?
|
Sertoli cells form blood-testis barrier.
|
|
|
What hormone is most effective in development of male external genitalia? What enzyme is involved in the final step of making this hormone?
|
Dihydrotestosterone (DHT)
5 alpha reductase |
|
|
What type of spermatogonia goes through mitosis only?
What type becomes mature sperm? |
type A: mitosis only, self-renewing
type B: becomes spermatocytes |
|
|
Clinically, how long do you wait to be infertile after vasectomy? why?
|
90 days because it takes about 90 days for sperm to mature
|
|
|
What is the major component of the ejaculate?
|
secretion from seminal vesicle (60% of total volume)
|
|
|
What are smegmas? What a potential complication of smegma?
|
they are desquamated epitheilial cells, sweat and debri b/t glans and prepuce; often associated with poor hygiene
can be carcinogenic or trap carcinogens --> penile carcinoma |
|
|
What are Bowen disease and Bowenoid papulosis?
How are they different, clinically? |
Bowen disease and Bowenoid disease: plaque or papule on male external genitalia.
Bowen disease has a 10% risk of developing carcinoma Bowenoid papulosis has no risk of developing carcinoma |
|
|
What is the greatest risk factor for penile squamous cell carcinoma?
|
lack of circumcision
|
|
|
A 30 YO presents with a mass in the testis. What is the most likely tumor do you suspect?
What if the pt is 65 YO? |
for 30YO: seminoma
for 65 YO: testicular lymphoma |
|
|
Diagnose the testicular tumor:
A painful, malignant mass with glandular/papillary morphology. High serum levels of AFP, hCG. |
embryonal carcinoma
|
|
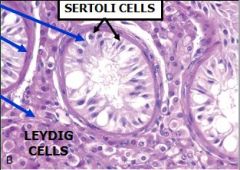
A 2 YO boy has bilateral masses in the lower abdomen. Physical exam reveals empty scrotal sac. A bx shows the following histologically.
What is dx? describe 4 morphologies. Complication? |
Cryptoorchism
4 morphologies: 1. arrest in development of germ cells 2. thickening of basement membrane of the seminiferous tubules 3. increased interstitial stroma 4. sparing of Leydig cells Higher risk of germ cell tumor in the testis |
|
|
Dx the following testicular tumor:
Morphology shows Schiller-Duval bodies and increased AFP. |
yolk sac tumor
|
|
|
What is the Most aggressive testicular germ cell tumor? What does this tumor secrete?
least aggressive? |
most aggressive: choriocarcinoma; secretes hCG
least aggressive: seminoma |
|
|
What is the least common testicular germ cell tumor?
|
choriocarcinoma
|
|
|
What does HMWk stain in the prostate? What does incomplete layer of HMWK stain indicate? What is the clinical significance?
|
HMWK stains the basal cell layer of prostate glands.
Incomplete layer indicates high grade prostatic intraepithelial neoplasia. This is precancerous to adenocarcinoma of the prostate |
|
|
What zone of the prostate is the associated with BPH? adenocarcinoma?
|
transitional zone: BPH
Peripheral zone: adenocarcinoma |
|
|
What is the most common risk factor for BPH?
|
old age, which increases serum dihydrotestosterone level --> hyperplasia of the prostate
|
|
|
A 70 YO male pt complains of increased urinary frequency, urgency, and urgency incontinence. He is diagnosed with BPH. What morphological change is responsible for the clininical symptoms?
|
stromal hyperplasia in the transitional zone, which obstructs the urethra.
|
|
|
How are glands of prostate cancer different form normal glands histologically?
Does BPH increase the risk of prostate cancer? |
Small glands with mild anaplasia, enlarged nuclei, 1 type of epithelial cell (instead of 2 types in normal)
NO |
|
|
What is the Gleason grading system? what grade is most common?
|
The grading system for prostate cancer based on histomorphology. Grade 3 is most common
|
|
|
A cancerous mass is detected in the lumbar spine. What do you suspect first?
|
metastasis from prostate cancer
|
|
|
What category of testicular germ cell tumor is most associated with necrosis and hemorrhage? What is the clinical significance?
|
Non-seminomatous germ cell tumor (NSGCT)
they tend to be more malignant and have poor prognosis. |
|
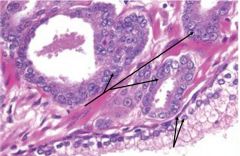
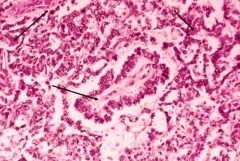
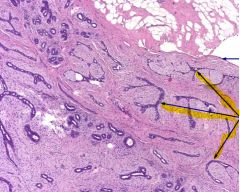
The picture shows a section of prostate carcinoma. What do the upper arrows indicate? bottom arrows?
|
Upper arrows indicate malignant epithelial cell layer, which consist of only one type of cells.
The bottom arrows indicates normal epithelial cell layers, which consist of 2 types of cell layers. |
|
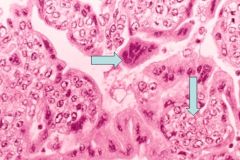
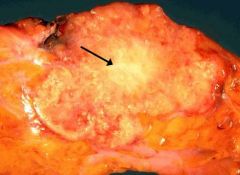
The pictures is from a prostate specimen with adenocarcinoma.
What are they? How are they clinically significant? |
A is perinueral invasion and B is Holmes crystals
they raise the suspicion of malignancy, especially in difficult cases. |
|
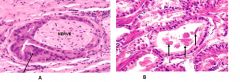
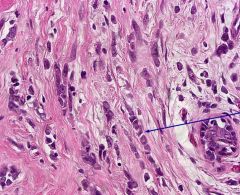
A 30 YO male with testicular mass shows the following morphology.
What is the most likely dx? Upper arrows indicate? lower arrows? |
Dx is seminoma
upper arrows are neoplastic germ cells with clear, large cytoplasm. Lower arrows indicate T cells |
|
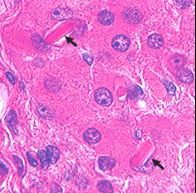
This is bx of a testicular mass in a 3 YO male. What do 2 upper arrows pointing at?
Bottom arrow? Dx? |
Upper 2 arrows indicate hyaline globules that secrete AFP.
Bottom arrow is pointing at Schiller-Duval body. Dx is yolk sac tumor; most common testicular tumor in children <4 YO |
|
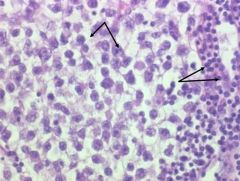
this is the most aggressive testicular tumor.
What are the cells indicated by the top arrow? bottom arrow? |
Choriocarcinoma
top arrow: syncytiotrophoblast bottom arrow: cytotrophoblast |
|
This is a section from testis. What are the arrows pointing at? What tumor is associated with these structures?
|
Reinke crystalloids
Leydig cell tumor |
|
|
What are 3 common risk factors for prostate cancer? which one is most important?
|
old age: most important
smoking fatty diet |
|
|
How is the dx of prostatic cancer made commonly?
|
transrectal ultrasound guided needle biopsy.
|
|
|
list 4 methods to improve predictive value of PSA.
|
1. age adjusted PSA level
2. PSA density: ratio of serum PSA to volume of PSA gland 3. PSA velocity: rate of change of PSA value over time 4. free PSA/total PSA ratio; <15% of free PSA increases the risk |
|
|
What imaging technique is commonly used to dx a testicular mass?
|
scrotal ultrasound
|
|
|
List 3 factors associated with early menopause.
List 3 factors associated with late menopause. |
early menopause: smoking, low body weight, poor nutrtion/chronic infection
Late menopause: obesity, diabetes, endometrial/breast cancer (anything that increases estrogen) |
|
|
What hormone is used to confirm menopause?
|
an increase in serum FSH
|
|
|
List 6 post-menopausal sxs.
|
"HHAVOC" +CNS sxs
Hirsutism Hot flashes Atrophy of vagina Osteopenia --> osteoporosis Coronary artery disease and HTN CNS sxs: mood swings, anxiety, depression, insomina |
|
|
What is the indication of progesterone in post-menopausal women on estrogen replacement therapy? how about for testosterone?
|
Progesterone: if uterus is intact b/c estrogen increases the risks of endometrial cancer.
Testosterone is indicated for females with lethargy and decreased libido. |
|
|
Estrogen hormone therapy increases risk in what diseases?
|
DVT, CHD, stroke, breast cancer and endometrial cancer
|
|
|
What is the MOA for Raloxifen? Why is it preferred over tamoxifen?
|
Selective estrogen receptor modulator (SERM)
antagonists at breast and endometrium and agonists at bone and lipids (increase HDL) Tamoxifen is a partial agonist at endometrial lining and can increase the risk of endometrial cancer. |
|
|
What is the MOA for Prolia?
|
RANK ligand inhibitor.
Rank ligand --> promotes osteoclastic action |
|
|
What is the pathogenesis behind supine hypotensive syndrome in pregnancy?
|
uterine hypertrophy can compress inferior vena cava causing decreased venous return and syncope in supine position.
|
|
|
List 4 cardiovascular physiologic changes during pregnancy.
|
1. increased cardiac output
2. increased heart size (increased LV wall mass --> slight left axis deviation on EKG) 3. AV O2 difference drops due to increased CO and alveolar ventilation oxygen consumption 4. increased venous distensibility --> varicose vein to dispose heat |
|
|
Is Dyspnea a normal change in pregnancy? why or why not?
|
Yes
higher tidal volume --> lower Pco2 (paradoxical dyspnea) the marked change or marked decline in Pco2 results in the sensation of dyspnea |
|
|
What accounts for mild renal hydronephorosis in pregnancy?
|
partial obstruction of ureters at the pelvic brim can cause fluid to back up in the ureter and cause dilated calyces, renal pelves and ureters.
|
|
|
What hormone dictates anti-insulin environment in pregnancy? What physiological changes are seen?
|
HPL (humal placental lactogen)
increases type 1 IGF --> Increase lipolysis and gluconeogensis --> increase in FFA, AA, and glucose |
|
|
What is the cause of chloasma, abdominal linear nigra and pigmentation in pregnancy?
|
increased MSH due to placental CRH and E3, which stimulate secretion of POMC hormones
|
|
|
What causes bile stone and pruritis during pregnancy?
|
impaired gall bladder contraction, promotion of bile tract stasis --> stones and pruritis due to high bile level.
|
|
|
What hormone stimulate synthesis of TBG during pregnancy? how about T4/T3?
|
TBG synthesis is increased by estrogen.
T4/T3 synthesis is increased by hCG but the mother remains euthyroid. |
|
|
Where is the principal site of estrogen and progesterone synthesis during the first trimester of pregnancy?
how about in 2nd and 3d trimesters? |
1st trimester: both progesterone and estrogen are synthesized by corpus luteum.
2nd and third trimesters: both are synthesized by the placenta. |
|
|
Describe Estriol (E3) syntehsis during 2nd and third trimester of pregnancy.
Describe E1 and E2 synthesis during 2nd/3rd trimesters. |
E3 synthesis:
Pregnenolone from mother --> converted to progesterone in the placenta --> converted to DHEA in fetal adrenal gland --> hydroxylated in the fetal liver --> aromatized in the placental --> E3 transferred to maternal circulation E1 and E2: DHEAS from adrenal glands (50% mother and 50% fetal) --> aromatized in the placenta |
|
|
When does hCG level peak during pregnancy?
What cells secrete hCG? What else do these cells secrete? What does extremely high hCG indicate? |
peaks at week 10 of pregnancy
secreted by syncyotrophoblast; also secretes HPL extremely high hCG indicates pathology (e.g. choriocarcinoma) or multiple pregnancy |
|
|
Compare and contrast fasting state vs fed state in terms of insulin sensitivity during pregnancy.
|
fed state --> low HPL --> insulin increases and promotes fat storage
fasting state --> high HPL --> insulin resistance |
|
|
How does the fetus increase Ca transfer from the mother during pregnancy.
|
increased production of fetal 1,25 OH vitamin D --> increase GI Ca/PO4 absorption in mother and decreased maternal PTH --> increased placental productin of PTHrP --> increased Ca transfer against the gradient into the fetus
|
|
|
What pituitary hormones are increased during pregnancy? decreased?
|
Increased prolactin due to hypertrophy and hyperplasia of pit gland.
Increased ACTH, endorphin, and MSH due to high placental CRH and E3. decreased GH |
|
|
Describe the thyroid status in pregnancy.
|
Euthyroid even though total T4/T3 increases due to an increase in TBG (estrogen-induced). Free T4/T3 remain the same.
Increased thyroid gland due to hCG |
|
|
What 3 hormones are increased during parturition?
|
prostaglandin, E1, and E3
|
|
|
What 4 factors inhibit parturition?
|
1. anencephaly
2. sulfatase deficiency 3. inadequate adrenal development 4. no PG, E1, and E3 |
|
|
What are 2 differential dx in pregnant pts with the following sxs:
dilated left atrium pulmonary congestion pulmonary HTN |
mitral stenosis and aortic stenosis
|
|
|
what type of delivery is preferred in pregnant pts with aortic stenosis? why?
|
vaginal delivery
C-section has too much risk of volume loss. Volume loss cannot be fixed by giving saline soln b/c of the aortic stenosis. |
|
|
Which hormone is mainly responsible for gestational diabetes? Is the maternal fasting glucose level high or low? why or why not?
|
HPL
Maternal fasting glucose level is low b/c glucose is transferred to the fetus |
|
|
What are the consequences of fetal hyperglycemia?
|
fetal hyperinsulinemia (risk for diabetes later in life)
macrosomia oxygen depletion episodic fetal hypoxia --> catecholamine --> myocardial hypertrophy |
|
|
What is the major problem with macrosmic baby (due to diabetic mother) during the delivery?
|
shoulder dystocia
|
|
|
Should you stop the seizure medicine during pregnancy if the condition preexisted before the pregnancy? why or why not?
|
NO, no drug is higher risk than uncontrolled seizures.
|
|
|
What is the goal of seizure medicine during pregnancy?
|
keep the pt seizure free at lowest effective dose with a single agent.
|
|
|
what type of hypothyroidism is more common during pregnancy? overt or subclinical?
|
subclinical (normal free thyroxine/elevated TSH)
|
|
|
why do you want to treat subclinical hypothyroidism during pregnancy?
|
thyroid hormone is very important in CNS/intelligence development
|
|
|
What should be first on the different dx list with RUQ abdominal pain in a pregnant pt? why?
Is surgery indicated? |
acute appendicitis b/c sepsis and bacteremia increase risk for fetal neurologic injury.
Gallbladder stone is second on the list. yes, surgery is indicated |
|
|
What is the pathogenesis of preeclampsia?
What 3 sxs are associated with it? |
caused by placental ischemia due to impaired vasodilation of spiral arteries resulting in hypoperfusion of the placenta.
HELLP syndrome (on mother): Hemolysis, elevated LFTs, low platelets |
|
|
Compare and contrast preeclampsia with eclampsia.
|
Preeclampsia: BP>140/90 that occurs after 20 weeks of gestation + 0.3g/ proteinuria
Eclampsia: preeclampsia + seizures (unattributed to other causes) |
|
|
What is the most common cause of uterine inversion?
|
iatrogenic (by pulling the cord during the delivery)
|
|
|
What is the definition of postpartum hemorrhage?
|
equal or greater than 500cc of blood loss in first 24 hr of delivery
|
|
|
What drug is used to prevent preterm labor?
|
17 alpha hydroxyprotesterone caproate
|
|
|
why is antenatal steroid recommended for women who are at risk for preterm delivery?
|
to allow full lung development and prevent hyaline membrane disease (NRDS).
|
|
|
A monozygotic twin can be monochorionic, dichorionic, or both?
|
both
|
|
|
Match the following:
timing of embryonic division: 0-72 hrs, 4-8 days, 8-13 days, >13 days types of monozygotic twin: monochorionic/monoamniotic, dichorionic/diamniotic, monochorionic/diamniotic, conjoined twins |
0-72 hrs: dichorionic and diaminotic
4-8days: monochorionic and diaminotic 8-13 days: dichorinoic and diamniotic >13 days: conjoined twins |
|
|
What are potential complications of monozygotic, monoaminotic twin placenta?
|
asymmetric twins due to twin-twin transfusion.
2 umbilical cords communicate and share circulation |
|
|
What are some maternal complications of twin gestations?
|
more likely to be hospitalized (6x)
hyperemesis pregnancy induced HTN Pyelonephritis, acute fatty liver thromboembolism postpartum hemorrhage preterm labor |
|
|
What placental abnormality is associated with 3rd trimester painless bleeding?
How about painful bleeding? (2) |
painless bleeding: placenta previa
painful bleeding: placenta accreta (increta and percreta) and abruptio placenta |
|
|
What does inadequate decidua lead to in pregnancy?
List 4 causes of inadequate decidua. |
Can lead to placenta accreta
4 causes of inadequate decidua 1. placenta previa 2. uterine scar 3. endometritis 4. submucosal leiomyoma |
|
|
What is placenta membranacea? What are some associated complications?
|
a thin placenta due to excessive villi covering of the chorion.
Complications include placenta previa and/or placenta accreta |
|
|
Name 2 causative organisms that cause granulomatous lesions on placenta.
|
Listeria monocytogene and mycobacterium tuberculosis
|
|
|
What is the most likely dx?
1st trimester bleeding increased hCG level karyotype shows 46 xx of the biopsied tissue grape-like tissue larger maternal uterus What pattern is seen on pelvic ultrasound? what are possible complications? |
Complete hydatidiform mole
Snow storm pattern on pelvic ultrasound complications: 16% may develop invasive mole and 2.5% may develop choriocarcinoma |
|
|
What is the most likely dx?
A missed abortion low hCG partial fetal parts present karyotype of the biopsied tissue shows 69, XXY Is there a high chance of complication? |
partial hydatidiform mole
no, very minimal increased risk of invasive mole and choriocarcinoma |
|
|
What is the prognosis of the gestation chriocarcinoma? Explain.
|
very good.
Excellent response to chemotherapy. |
|
|
What is name of the region that secrets GnRH in the hypothalamus?
|
arcuate nucleus of the hypothalamus
|
|
|
What cells are stimulated by FSH? LH? fxn of the cells are?
|
FSH stimulates granulosa cells to make estradiol
LH stimulates theca cells to produce androgen, which are aromatized in the granulosa cells |
|
|
Which phase of the menstrual cycle normally lasts for 14 days?
which phase of the menstrual cycle is variable in length? |
14 days: luteal/secretory phase
variable in length: follicular/proliferative phase |
|
|
What type of dysfunctional uterine bleeding is hypothyroidism associated with? how about hyperthyrodism? hyperprolactinemia?
|
Menorrhagia: hypothyroidism
Oligomenorrhea or amenorrhea: hyperthyroidism and hyperprolactinemia (blocks GnRH) |
|
|
What is the most common complaint of polycystic ovary syndrome (POS)?
List 3 other clinical findings/significance. |
oligomenorrhea
1. causes hirsutism (due to LH:FSH ratio >2) 2. infertility (due to follicle degeneration from FSH suppression) 3. obesity --> increased risk of endometrial cancer (androgen is aromatized in the adipose tissue) |
|
|
what is the most common symptom of leiomyomas? 2nd most symptom?
|
most common: abnormal bleeding
2nd most common: infertility |
|

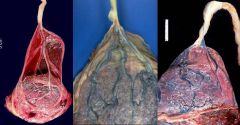
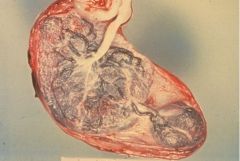
A pregnant woman in 3rd trimester has a sudden onset of painful vaginal bleeding with abdominal pain. The baby was born prematurely and died. The following picture is this baby's placenta.
what is the dx? What is the most likely predisposing factor that led to this event? |
Abruptio placenta
maternal HTN |
|
this is a picture of an abnormal placenta. What is the dx?
What potential complication can occur? why? |
dx: velamentous insertion of the umbilical cord.
Can lead to impaired fetal blood flow b/c a portion of the umbilical cord travels in the placenta without the Wharton's jelly (which protects the vessels from compression) |
|
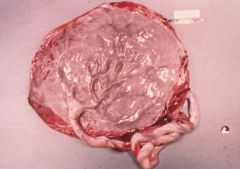
This is a picture of an abnormal placenta.
What is the dx? List one complication. |
Succenturiate lobes
can cause post partum hemorrhage |
|

This is a picture of an abnormal placenta.
What is the dx? |
circumvallate placenta
|
|

This is a picture of an abnormal placenta.
What is the dx? What histological changes can be observed on the surface of the amnion? List 3 associated conditions. |
Amnion nodosum
small nodules of fibrin and desquamated squaous cells associated with oligohydramnios, renal agenesis, and poor fetal outcome |
|
This is an abnormal picture of a placenta.
What is the gray material on the surface of the amnion? list 2 main causes. |
gray material on the surface of the amnion is pus.
2 main causes are staph and E coli. |
|
|
A 20 YO male comes into your office complaining of painful, white, urethral discharge from the penis. He is sexually active. What do you suspect? What is the tx?
|
suspect gonococcal urethritis.
treat it with IM injection of cefixime, or ceftriaxone. for co-chlamydial infection and noncompliant pt, one dose of azithromycin. |
|
|
A 22 YO male with previous hx of gonorrhea complains of dysuria. Physical exam reveals urethritis, conjuctivitis, and arthritis.
What do you suspect? |
Reiter's syndrome
(HLA-B27 associated arthritis) |
|
|
What is the preferred treatment for gonorrhea co-infected with chlamydia?
|
1 gram oral dose of azithromycin
|
|
|
A 25 YO male presents with dysuria, increased frequency, urgency, and fever. Physical exam reveals erythmatic and painful scrotal swelling on the left side. what do you suspect?
|
epidymitis secondary to STD (gonorrhea, chlamydia or syphillis)
|
|
|
what is a common cause of orchitis?
|
virus, esp mumps (a Paramyxovirus/ an RNA virus)
|
|
|
A 65 YO male complains of a sudden onset of chills, fever, malaise, and dysuria. Physical exam reveals painful, warm, swollen prostate.
What is the dx? List 4 common causative organisms. |
prostatitis
E coli, Proteus sps, enterococcus fecalis, staph saprophyticus |
|
|
A sexually active 25 YO female complains of vaginal itch, white/milky vaginal discharge, and fish odor.
What is the dx? causative organism? What special cells are visible under the microscope? Is this an STD? |
bacterial vaginosis due to overgrowth of Gardnerella vaginalis.
Clear cells are visible (vaginal epithelial cells covered with bacteria) Not an STD |
|
|
What is the dx?
thick, white, clumpy, "cottage cheese" vaginal discharge, 2nd most common cause of vaginitis. |
candida vulvovaginitis
|
|
|
What is the dx?
frothy, gray/yellow malodorous vaginal discharge, "strawberry cervix', cervical petechiae |
Trichomonas vaginitis
|
|
|
What organism is associated cervicitis due to intrauterine device?
|
actinomyces
|
|
|
What is chandelier' sign?
What disease is it associated with? What approach is used treating this disease? |
Chadelier's sign: cervical motion tenderness
associated with PID overdiagnose and overtreat; treat early and think broad spectrum b/c PID tends to be subclinical or asymptomatic. |
|
|
A 20 YO sexually active female presents with pain in the pelvis, lower abdomen, abnormal vaginal bleeding, and fever. She has a history of multiple STDs.
What do you suspect? |
pelvic inflammatory disease
|
|
|
Is PID usually caused by a single organism or multiple organisms?
Name 2 most common organisms. List 4 complications of PID. |
usually polymicobial
2 common: Gonorrhea and chlamydia. 4 complications 1. infertility 2. ectopic pregnancy 3. chronic pelvic pain 4. adhesion; Fitz-Hugh-Curtis syndrome (infection of the liver capsule which leads to violin-string adhesions) |
|
|
A pt presents witha painful penile ulcer with fever, myalgia.
List 2 ddx. Which one causes chancroid? |
HSV2
Haemophilus Ducrey: causes cancroids |
|
|
Which organism causes painless chancre on external genitalia.
Name 3 tests to confirm the dx. Which one is most sensitive and specific |
Treponema pallidum (syphilis)
3 tests: 1. RPR (rapid plasmin reagent) 2. VDRL (venereal disease research lab) 3. FTA-ab (flourescent treponema Ab): most sensitive and specfiic |
|
|
List 3 sxs of tertiary syphilis.
What is the tx? |
aortitis (vasa vasorum destruction --> thoracic aneurysm)
tabes dorsalis (CNS) Argyll Robertson pupil treat with penicilin |
|
|
What STD causing organism is associated with lymphadenopathy buboes in the inguinal region? Be specific.
|
Chlamydia trochomitis serotype L1-L3
causes Lymphogranuloma venereum (LGV) |
|
|
What are Donovan bodies?
What organism and disease are associated? |
Donovan bodies are safety pin appearing vacuoles within the macrophages. They are phagocytosed intracellular bacteria.
associated with Calymmatobacterium granuloma and granuloma inguinale |
|
|
What are TORCH infections?
|
infections that may pass from mother to fetus. Nonspecific signs include hepatosplenomegaly, jaundice, thrombocytopenia, and unusual rash.
Toxoplasmosis Other (syphilis) Rubella CMV HSV1 or 2 |
|
|
List 3 sxs of toxoplasmosis infection.
What should mothers avoid to prevent this infection? |
chorioretinitis, hydrocephalus, and intracranial calcification
should avoid cats b/c they are definitive hosts of toxo. |
|
|
A 2 week old neonate presents with snuffles, Hutchison teeth, and cutaneous lesions on palms and soles. Physical exam reveals periostitis and metaphysial dystrophy of long bone.
What is dx? tx? How do you screen for this infection? |
dx: syphilis (treponema palidum)
tx: penicillin Screening via RPR and VDRL |
|
|
A neonate presents with hearing loss, cataracts, patent ductus arteriosus, and "blueberry muffin" rash.
What do you suspect? How do you prevent the disease? |
infection via Rubella
Prevent with vaccine |
|
|
What is the most common congenital viral infection?
What is the unique presentation of this infection? List 3 other presentations. |
CMV
most uniqe: periventricular calcification. also presents with hearing loss, vision impairment, developmental delays. |
|
|
What TORCH infection is primarily transferred through infected maternal genital tract? how do you prevent it?
|
Herpes simplex virus 1 or 2
prevent the spread via C-section delivery. |
|
|
List 3 most common organisms causing post-partum infections in mothers.
|
strep, bacteriodes, and E coli
|
|
|
What is the cause of Nabothian cyst of cervix? Is there any clinical significance?
|
caused by obstruction of endocervical glands
no clinical significance |
|
|
Where does squamous metaplasia of the endocervix occur?
What is a predisposing factor? |
At the transformation zone: the jxn b/t columnar epithelium of the endocervix and squamous epithelium of the ectocervix.
Ectropion is the area where the endocervix everts onto the ectocervix. This area is prone to irritation and trauma, and may develop metaplasia or neoplasia. |
|
|
Is HPV curable?
|
No
|
|
|
How does Cervical squamous cell carcinoma cause renal failure?
|
In the advanced stage of SCC, the cancer can metastasize to the bladder and obstruct ureter causing post-renal azotemia and hydronephrosis.
|
|
|
What other cancer can follow cervical squamous cell carcinoma? What is the prognosis.
|
Adenocarcinoma of the cervix. Poorer prognosis than SCC.
|
|
|
What virus is associated with high grade squamous intrapithelial lesions (be specific)? How do they potentially cause cervical cancer at a molecular level?
|
HPV types 16, 18, 31, 33
high grade viral genes are incorporated in the host cellular DNA allow expression of E6 and E7 genes. E6 binds p53 and E7 binds to Rb gene. These tumor suppressor genes wil be inactivated. |
|
|
Why is PAP smear important clinically?
|
PAP smear is important because dysplasia and CIN are usually clinically asymptomatic and advanced stages of SCC can be fatal.
|
|
|
Describe how the PAP smear is used to screen for cervical cancer? How do you diagnose cervical cancer?
|
PAP smear is used for screening only!
With a positive PAP smear result, a cervical biopsy is used to confirm. The correlation b/t PAP and bx is made if the bx is as atypical or has a worse grade. |
|
|
List 3 risk factors for cervical cancer.
|
1. higher risk for early age of first sexual intercourse
2. number of partners 3. smoking |
|
|
What hormone stimulate the endometrium during the proliferative phase? secretory phase?
|
proliferative phase: estrogen
secretory phase: progesterone |
|
|
What is the presence of benign glandular endometrial tissue in the myometrium called?
|
adenomyosis
|
|
|
A 30 YO obese woman complains of abnormal uterine bleeding. A biopsy of uterus shows crowded irregular glands with cytologic atypia.
What is the dx? most likely cause? Most likely mutated gene? complication? |
Atypical Complex endometrial hyperplasia.
Caused by prolonged estrogen PTEN tumor suppressor gene is mutated in 25% of the cases Can progress to endometrial cancer, esp type II endometrial adenocarcinoma (serous carcinoma) |
|
|
A 70 YO post-menopausal female complains of bleeding, lower abdominal pain, and a palpable abdominal mass. Ultrasounds reveals a mass in the uterus and a biopsy is done. Histology shows atypical squamous cells, keratin pearl, atpyical glandular cells, and chondrocytes.
What is the most likely dx? prognosis? |
malignant Mixed mullerian tumor (Carcinosarcoma)
poor prognosis; <30% 5 yr survival. |
|
|
What hormone influence the growth of leiomyoma?
|
estrogen
|
|
|
What lesion(s) is (are) potentially possible at each location of the breast.
1. stroma 2. lobule 3. terminal duct 4. major duct 5. lactiferous sinus 6. Nipple/areola complex |
1. stroma: fibroadenoma, phyllodes tumor
2. lobule: lobular carcinoma, sclerosing adenosis 3. terminal duct: tubular carcinoma 4. major duct: fibrocystic change, ductal cancer 5. lactiferous sinus: intraductal papilloma, breast abscess, plasma cell mastitis 6. Nipple/areola complex: Paget's disease, breast abscess |
|
|
Breast pathology epidemiology questions.
1. Most common clinical findings in breast pathology? What % are cancerous? 2. Most common location for cancer? 3. Most common disorder of breast? 4. Most common cause of bloody discharge in women <50 YO? 5. Most common benign tumor of female breast <30 YO? 6. Most common bilateral malignancy and found incidentally? |
1. palpable mass. only 10% are cancerous
2. Upper outer quadrant (50%) 3. Fibrocystic changes 4. intraductal papilloma 5. fibroadenoma 6. Lobular carcinoma or Lobular CIS |
|
|
What type of breast pathology is this?
1. most likely due to Staph aureus infection during the first weeks of lactation period. 2. Most likely due to trauma and shows fibrosis, calcification, and lipid-laden macrophages. |
1. acute mastitis
2. fat necrosis of breast |
|
|
List 3 histological changes in fibrocystic disease of the breast.
|
1. fibrosis
2. cysts or cysts with hemorrhage (blue-dome cysts) 3. benign apocrine metaplasia |
|
|
What histological feature of the fibrocystic disease increases the risk of developing breast carcinoma?
|
atypical ductal or lobular hyperplasia
|
|
|
A 25 YO female presents with single, painless, discrete, encapsulated, freely movable mass with no inflammation, no palpable lymph nodes, and no skin abnormalities.
Most likely diagnosis? |
fibroadenoma
|
|
|
what 2 tumor suppressor genes are associated with breast cancer in female? which one associated with male breast cancer?
List 3 oncogenes implicated in breast cancer. |
Tumor suppressor genes: BRCA 1 and BRCA 2 (also associated with male breast cancer)
Oncogenes: HER2/Neu, C-myc, C-RAS |
|
|
what is the most important prognostic factor in breast cancer?
|
lymph node involvement.
5 yr survival rate drastically decreases with lymph node involvement. |
|
|
Nipple shows ulceration, fissuring and hyperemia. What is the dx?
Describe the pathogenesis of this disease. |
Paget's disease
The intraductal carcinoma (adenocarcinoma) arises in the main excretory ducts of the breast and extends into the epithelium of the nipple and areola. |
|
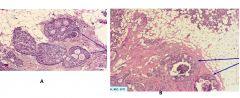
This is a section of pathological breast tissue. What are the arrows pointing in picture A? Picture B?
Most likely diagnosis? |
A: Cribriform pattern of expanded ductal cells showing atypical cytology.
B: Comedocarcinoma (expanded ducts and atpyical cells with central necrosis and calcification) Dx: Ductal carcinoma in situ or DCIS with infiltrating ductal carcinoma |
|
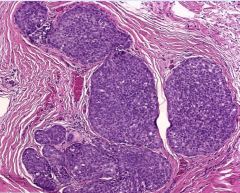
This is a section of pathological breast tissue.
Describe the histology. What is the most likely dx? How are they found clinically? |
uniform expansion of terminal ducts and acini by monomorphic population of small cells; contained within the basement membrane.
Most likely lobular carcinoma in situ found incidentally |
|
This is a gross picture of pathological breast tissue.
What is the most likely dx? what gene is mutated? |
infiltrating ductal carcinoma
amplification of ERBB2/HER2 oncogene |
|
This is a picture of pathological breast tissue. What is the arrow pointing at?
most likely dx? |
The arrow is pointing at Indian filing cells.
dx: infilgrating lobular carcinoma |
|
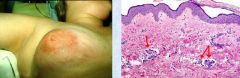
The picture shows gross and microscopic picture of a breast pathology.
What are the red arrows pointing at on the microscopic picture? What is most likely dx? Is this disease advanced or at an early stage? |
Arrows are pointing at dermal lymphatic invasion by neoplastic cells.
Dx: inflammatory breast carcinoma This is an advanced disease findings of breast carcinoma |
|
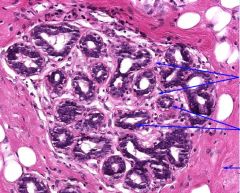
This is a section of normal breast histology.
What structures are pointed by the top 2 arrows? Middle 2 arrows? the bottom arrow? |
Top 2: loose intralobular stroma
middle 2: ductules lined by cuboidal cells bottom: fibrous interlobular stroma |
|
This is a section of fibroadenoma of the breast.
What are the yellow-highlighted arrows indicating? |
compressed and distorted ducts due to overgrowth of the fibrous interlobular stroma
|

