![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
151 Cards in this Set
- Front
- Back
|
Poliomyelitis
|
Caused by poliovirus (fecal-oral transmission). Replicates in the oropharynx and small intestine before spreading via the bloodstream to the CNS. Infection causes destruction of cells in anterior horn of spinal cord (LMN death)
|
|
|
Symptoms of Poliomyelitis
|
LMN lesion signs - weakness, hypotonia, flaccid paralysis, atrophy, fasciculations, hyporeflexia, and muscle atrophy.
|
|
|
Signs of infection associated with Poliomyelitis
|
Malaise, headache, fever, nausea, etc.
|
|
|
Findings associated with poliomyelitis
|
CSF with Increased WBC with slight elevation of protein (with no change in CSF glucose). Virus recovered from stool or throat.
|
|
|
Werdnig-Hoffman Disease
|
Congenital degeneration of anterior horns of spinal cord --> LMN lesion.
"Floppy baby" with marked hypotonia and tongue fasciculations. Infantile type has median age of death of 7 months. Autosomal recessive inheritance. |
|
|
Friedreich's Ataxia
|
Autosomal-recessive trinucleotide repeat disorder (GAA) in gene that encodes frataxin.
|
|
|
What does Friedreich's Ataxia lead to?
|
Impairment in mito functions. Staggering gait, frequent falling, nystagmus, dysarthria, pes cavus, hammer toes, hypertrophic cardiomyopathy (cause of death)
|
|
|
How does Friedrich's ataxia present in childhood?
|
With kyphoscoliosis
|
|
|
|
|
|
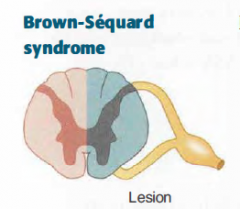
Brown-Sequard Syndrome
|
|
|
|
Brown-Sequard Syndrome
|
Hemisection of spinal cord
|
|
|
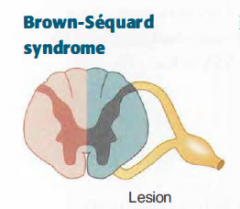
Brown-Sequard Syndrome Findings
|
- Ipsilateral UMN signs below the level of the lesion (due to corticospinal tract damage)
- Ipsilateral loss of tactile, vibration, proprioception sense below the level of the lesion (due to dorsal column damage) - Contralateral pain and temperature loss below the level of the lesion (due to spinothalamic tract damage) - Ipsilateral loss of all sensation at the level of the lesion - Ipsilateral LMN signs (e.g. flaccid paralysis) at the level of the lesion |
|
|
With Brown-Sequard Syndrome - if the lesion occurs above T1, what can happen?
|
The patient can present with Horner's Syndrome due to damage of the sympathetic ganglion.
|
|
|
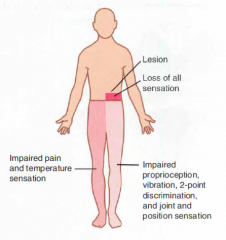
Horner's Syndrome
|
Sympathectomy of face:
- Ptosis (slight drooping of eyelid: superior tarsal muscle) - Anhidrosis (absence of sweating) and flushing of affected side of face - Miosis (pupil constriction) |
|
|
What lesion is Horner's Syndrome associated with?
|
Spinal cord above T1 (like a Pancoast tumor, Brown-Sequard syndrome, late-stage syringomyelia)
|
|
|
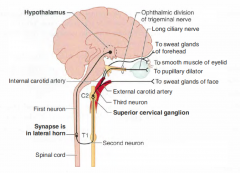
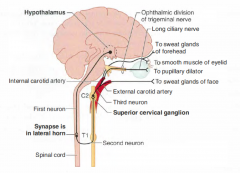
3-neuron oculosympathetic pathway projects from the hypothalamus to the intermediolateral column of the spinal cord, then to the superior cervical (sympathetic) ganglion, and finally to the pupil, the smooth muscle of the eyelids, and the sweat glands of the forehead and face.
Interruption of any of these pathways results in Horner's syndrome |
|
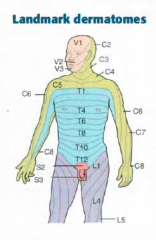
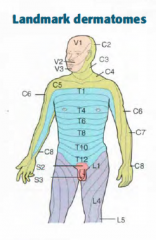
Dermatomes
|
|
|
|
C2 Dermatome
|
Posterior half of a skull "cap"
|
|
|
C3 Dermatome
|
High turtleneck shirt
|
|
|
C4 Dermatome
|
Low collar t-shirt
|
|
|
T4 Dermatome
|
Nipple
|
|
|
T7 Dermatome
|
Xiphoid Process
|
|
|
T10 Dermatome
|
Umbilicus
|
|
|
L1 Dermatome
|
Inguinal Ligament
|
|
|
L4 Dermatome
|
Includes kneecaps
|
|
|
S2, S3, S4 Dermatome
|
Erection and sensation of penile and anal zone
|
|
|
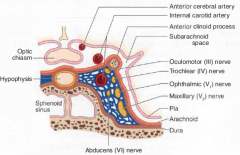
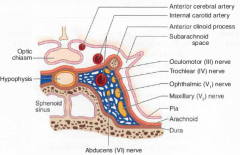
Cavernous Sinus
|
A collection of venous sinuses on either side of the pituitary. Blood from eye and superficial cortex leads to cavernous sinus to the IJV.
|
|
|
What are the nerves that pass through the cavernous sinus?
|
CN III, IV, V1, V2, and VI and postganglionc sympathetic fibers pass through.
Cavernous portion of ICA also pass through |
|
|
|
|
|
Cavernous Sinus Syndrome
|
Due to mass effect, fistula, thrombosis -- ophthalmoplegia and decreased corneal and maxillary sensation with normal vision
|
|
|
CN V Lesion
|
Jaw deviates toward side of lesion due to unopposed force from opposite pterygoid muscle
|
|
|
CN X Lesion
|
Uvula deviates away from side of lesion. Weak side collapses and uvula points away.
|
|
|
CN XI lesion
|
Weakness turing head to the contralateral side of lesion (SCM). Shoulder droop on side of lesion (trapezius)
The left SCM contracts to help turn the head to the right |
|
|
CN XII Lesion
|
LMN
Tongue deviates toward side of lesion due to weakened tongue muscles on the affected side |
|
|
Conductive hearing loss
|
Rinne Test : Abnormal (bone > air)
Weber Test: Localizes to affected ear |
|
|
Sensorineural Hearing loss
|
Rinne Test: Normal (air > bone)
Weber Test: Localizes to unaffected ear |
|
|
Noise-induced Hearing Loss
|
Damage to stereocilliated cells in organ of Corti; high loss of frequency hearing 1st; sudden extremely loud noises can produce hearing loss due to tympanic membrane rupture.
|
|
|
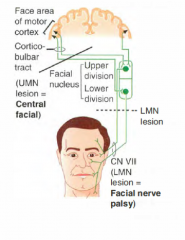
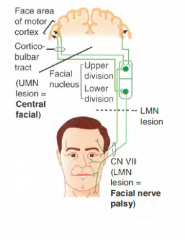
UMN Lesion
|
Lesion of motor cortex or connection between cortex and facial nucleus. Contralateral paralysis of lower face; forehead spared due to bilateral UMN lesion
|
|
|
|
|
|
LMN Lesion
|
Ipsilateral paralysis of upper and lower face
|
|
|
Facial nerve palsy
|
Complete destruction of the facial nucleus itself or its branchial efferent fibers (facial nerve proper)
Peripheral ipsilateral facial paralysis with inability to close eye on involved side. Can occur idiopathically; gradual recovery in most cases. |
|
|
What diseases can cause facial nerve palsy?
|
Seen as a complication in AIDS, Lyme disease, herpes simplex and (less common) herpes zoster, sarcoidosis, tumors, and diabetes.
|
|
|
Which muscles close the jaw?
|
Masseter
Temporalis Medial Pterygoid Innervated by V3 |
|
|
Which muscle opens the jaw?
|
Lateral pterygoid
Innervated by V3 |
|
|
What are refractive errors?
|
Impaired vision that improves with glasses
|
|
|
Hyperopia
|
Eye too short for refractive power of cornea and lens and results in light focused behind the retina.
|
|
|
Myopia
|
Eye too long for refractive power of cornea and lens and leads to light focused in front of the retina
|
|
|
Astigmatism
|
Abnormal curvature of cornea resulting in different refractive power at different axes.
|
|
|
Accommodation
|
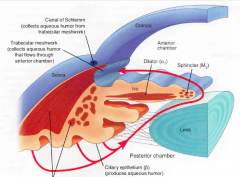
Focusing on near objects --> ciliary muscles tighten --> zonular fibers relax --> lens become more convex. Occurs with convergence and miosis.
|
|
|
Presbyopia
|
Decrease change in focusing ability during accommodation due to sclerosis and decreases elasticity
|
|
|
Uveitis
|
Inflammation of uveal coat (consists of iris, ciliary body, and choroid). Often associated with systemic inflammatory disorders (e.g sarcoid, rheumatoid arthritis, juvenile idiopathic arthritis, TB, HLA-B27-associated conditions)
|
|
|
Retinitis
|
Retinal edema and necrosis leading to scar. Often viral (CMV, HSV, HZV). Associated with immunosuppression.
|
|
|
Central Retinal Artery Occlusion
|
Acute, painful monocular vision loss. Retina whitening with cherry-red spot.
|
|
|
|
|
|
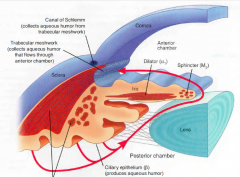
Glaucoma
|
Optic neuropathy, usually with increased intraocular pressure
|
|
|
Open/Wide Angle Glaucoma
|
Characterized by peripheral then central vision loss usually with an increase in intraocular pressure; optic disc atrophy with cupping; associated with increased age, AA race, family history.
Primary cause unclear |
|
|
Secondary causes of open/wide angle glaucoma
|
Uveitis, trauma, corticosteroids, and vasoproliferative retinopathy that can block or decrease outflow at the trabecular meshwork.
|
|
|
Closed/narrow angle glaucoma
|
Enlargement or forward movement of lens against central iris leads to obstruction of normal aqueous flow through pupil. The fluid builds up behind the iris pushing the peripheral iris against the cornea and impeding flow through the trabecular meshwork.
|
|
|
Chronic closure of closed/narrow angle glaucoma
|
Often asymptomatic with damage to the optic nerve and peripheral ganglion
|
|
|
Acute Closure of Closed/Narrow angle glaucoma
|
True ophthalmic emergency. Increased intraocular pressure pushes iris forward and results in the angle closing abruptly. Very painful, sudden vision loss, halos around lights, rock-hard eye, frontal headache. Do not give epinephrine because of mydriatic effect.
|
|
|
Mydriatic Effect
|
Blown-out pupil
|
|
|
Cataract
|
Painless, often bilateral opacification of lens that results in a decrease in vision.
|
|
|
Risk factors for cataracts
|
Age, smoking, alcohol, excessive sunlight, prolonged corticosteroid use, classic galactosemia, galactokinase deficiency, diabetes (sorbitol), trauma, infection
|
|
|
Papilledema
|
Optic disc swelling (usually bilateral) due to an increase intracranial pressure. Enlarged blind spot and elevated optic disc with blurred margins seen on fundoscopic exam.
|
|
|
|
|
|
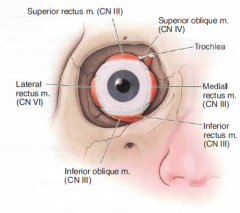
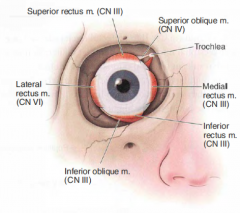
CN VI innervates?
|
Lateral Rectus
|
|
|
CN IV innervates?
|
Superior oblique
|
|
|
CN III Innervates?
|
Inferior oblique
Superior rectus Medial rectus Inferior rectus |
|
|
CN III damage
|
Eye looks down and out; ptosis, pupillary dilation, loss of accommodation
|
|
|
CN IV damage
|
Eye moves upward, particularly with contralateral gaze and ipsilateral head tilt (problems going down stairs).
|
|
|
CN VI Damage
|
Medially directed eye cannot abduct
|
|
|
How do you test the inferior oblique?
|
Have the patient look up
|
|
|
How do the oblique muscles move the eye?
|
In the opposite direction
|
|
|
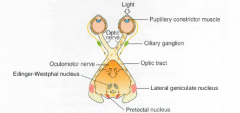
Miosis
|
(constriction, parasympathetic)
1st neuron: Edinger-Westphal nucleus to ciliary ganglion via CN III 2nd neuron: short ciliary nerves to pupillary sphincter mucles |
|
|
Mydriasis
|
Dilation, Sympathetic
1st neuron: hypothalamus to ciliospinal center of Budge (C8-T2) 2nd neuron: exit at T1 to superior cervical ganglion 3rd neuron: plexus along internal carotid, through the cavernous sinus; enters orbit as long ciliary nerve to pupillary dilator muscles |
|
|
Pupillary light reflex
|
Light in either retina sends a signal via CN II to pretectal nuclei (dashed lines) in midbrain that activate in midbrain that activate Edinger-Westphal nuclei; pupils contract bilaterally (consensual reflex)
|
|
Pupillary Light Reflex
|
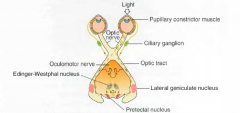
|
|
|
Marcus Gunn Pupil
|
Afferent pupillary defect (like due to optic nerve damage or retinal detachment) results in decreased bilateral pupillary constriction when light is shone in affected eye relative to the unaffected eye. Tested with "swinging flashlight test".
|
|
|
Which cranial nerves have their nuclei located in the medulla?
|
IX, X, XII
|
|
|
Which cranial nerves have their nuclei in the pons?
|
V, VI, VII, VIII
|
|
|
Which cranial nerves have their nuclei in the midbrain?
|
III, IV
|
|
|
What information is communicated at the nucleus solitarius?
|
Visceral sensory information (VII, IX, X)
|
|
|
What information is communicated at the nucleus ambiguus?
|
Motor innervation of pharynx, larynx, and upper esophagus (IX, X)
|
|
|
What information is communicated at the dorsal motor nucleus?
|
Autonomic Information about the heart, lungs, upper GI
|
|
|
A woman involved in an accident cannot turn head to the left and has a right shoulder droop. What structure is damaged?
|
Right IX
|
|
|
A 19 year-old patient present with a furuncle on his philtrum and the cavernous sinus becomes infected. What neurological deficits might you see in this patient?
|
CNs III, IV, VI go through CS
- fever, headache - extraocular m. damage - ophthalmoplegia - hyper or hypoesthesia |
|
|
What are the muscles of mastication?
|
V2, V3
Masseter, Temporalis, Medial Pterygoid, Lateral Pterygoid |
|
|
Which collagen is typically deficient in Ehlers-Danlos syndrome?
|
Type III
|
|
|
Which collagen is deficient in osteogenesis imperfecta?
|
Type I
|
|
|
What regulates the progression of G1 phase of the cell cycle to S phase?
|
p53 and Rb
|
|
|
Which cranial nerves innervate taste in the anterior 2/3?
|
Facial nerve
|
|
|
Which cranial nerve innervates taste in the posterior 1/3 of the tongue?
|
Glossopharyngeal
|
|
|
Which cranial nerve innervates motor in the tongue?
|
CN XII
|
|
|
Which cranial nerve innervates sensation in the anterior 2/3 of the tongue?
|
V3
|
|
|
Which cranial nerve innervates sensation in the posterior 1/3 of the tongue?
|
Glossopharyngeal
|
|
|
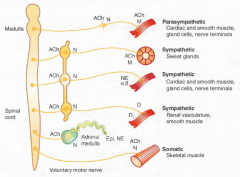
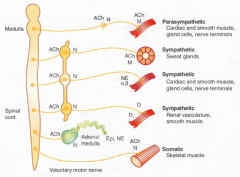
How do sympathetics affect the heart?
|
Increase HR and contractility
|
|
|
How do sympathetics affect the eye?
|
Mydriasis (dilation)
|
|
|
How do sympathetics affect the salivary glands?
|
Viscous secretion
|
|
|
How do sympathetics affect the bronchiolar smooth muscle?
|
Relaxation
|
|
|
How do sympathetics affect the bladder?
|
Prevent urination
|
|
|
How do sympathetics affect the male GU?
|
erection
|
|
|
How do sympathetics affect the GI tract?
|
Decreased digestion, contraction of sphincters, decreased secretion, decreased motility
|
|
|
How do parasympathetics affect the heart?
|
Vagus - decrease heart rate and contractility
|
|
|
How do parasympathetics affect the eye?
|
Miosis (constriction)
|
|
|
How do parasympathetics affect the salivary glands?
|
Watery Secretion
|
|
|
How do parasympathetics affect the salivary glands?
|
Water secretion
|
|
|
How do parasympathetics affect the bronchiolar smooth muscle?
|
contraction
|
|
|
How do parasympathetics affect the bladder?
|
Cause urination
|
|
|
How do parasympathetics affect the male GU?
|
ejaculation
|
|
|
How do parasympathetics affect the GI tract?
|
Increase digestion, increase secretion, increase motility
|
|
|
What are the symptoms of excess parasympathetic activity?
|
DUMBBELSS
D: Diarrhea U: Urination M: Miosis B: Bronchospasm B: Bradycardia E: Excitation of skeletal muscle/ CNS L: Lacrimation S: Sweating S: Salivation |
|
|
What are the Alzheimer disease anticholinesterases?
|
Donepezil
Galantamine Rivastigmine |
|
|
Myasthenia Gravis
|
There are autoantibodies to the postsynaptic acetylcholine receptor. Most common presentation are weakness, ptosis and diplopia that worsens throughout the day. Worsens with muscle use
Most frequent NMJ |
|
|
Tensilon test
|
For myasthenia gravis. Use edrophonium to see if pt symptoms improve
|
|
|
What is myasthenia gravis associated with?
|
Thymoma, Thymic hyperplasia
|
|
|
Thymus Pathologies associated with myasthenia gravis?
|
50% associated with thymic hyperplasia
20% associated with thymic atrophy 15% associated with thymic tumor (thymoma) |
|
|
Myasthenia crisis
|
Rapidly progressing weakness especially in respiratory muscles
|
|
|
Treatment for myasthenia gravis
|
Acetylcholinersterase inhibitors, corticosteroids, thymectomy (remove thymus), plasmaphoresis
|
|
|
What drug regenerates acetylcholinesterase after organophosphate poisoning?
|
Pralidoxine
|
|
|
What is the antidote for organophosphate poisoning?
|
Atropine (antimuscarinic) + pralidoxine (regenerate active acetylcholinesterase)
|
|
|
Which anticholinesterases are used in the treatment of Alzheimer disease?
|
Donepezil
Galantamine Rivastigmine |
|
|
Lambert-Eaton Myasthenic Syndrome
|
Uncommon
Autoantibodies to presynaptic Ca2+ channel that results in a decrease in ACh release |
|
|
Clinical aspects of Lambert-Easton Myasthenic Syndrome
|
Proximal muscle weakness
Improves with muscle use |
|
|
What is Lamber-Easton Myasthenic Syndrome associated with?
|
Small Cell Lung Cancer
|
|
|
What does an AChE Inhibitor administration do to Lamber-Easton Myasthenic Syndrome?
|
No effect
|
|
|
Myositis ossificans
|
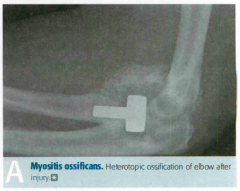
Metaplasia of skeletal muscle to bone following muscular trauma. Most often seen in upper or lower extremity. May present as suspicious mass at the site of known trauma or as incidental finding on radiography.
|
|
|
Fibromyalgia
|
Most commonly seen in women 20-50 years of age. Chronic, widespread musculoskeletal pain associated with stiffness, paresthesia, poor sleep, and fatigue.
|
|
|
Polymyositis
|
Progressive symmetric proximal weakness, characterized by endomysial inflammation with CD8+ T cells. Most often involves shoulders.
|
|
|
Dermatomyositis
|
Similar to polymyositis but also involves malar rash (similar to SLE), Gottron's papules, heloptrope rash, "shawl and face" rash, "mechanic's hand". Increase risk of occult malignancy. Perimysial inflammation and atrophy with CD4+ T cells.
|
|
|
Gottron's Papules
|

|
|

|
Heliotrope rash
|
|
|
Findings associated with Polymyositis/Dermatomyositis
|
Increased creatinine kinase, positive ANA, positive anti-Jo-1 antibodies
|
|
|
Treatment for Polymyositis/Dermatomyositis
|
Steroids
|
|
|
Botulinum toxin prevents?
|
Release of neurotransmitter at all cholinergic terminals
|
|
|
|
|
|
Ach Receptors
|
Nicotinic Ach receptors are ligand-gated Na+/K+ channels; Nn (found in autonomic ganglia) and Nm (found in neuromuscular junction) subtypes.
|
|
|
Muscarinic ACh receptros
|
GPCRs that act through 2nd messengers;
5 subtypes: M1, M2, M3, M4, and M5 |
|
|
a1 receptor
|
Gq
Increases vascular smooth muscle contraction, increase pupillary dilator muscle contraction (mydriasis), increase intestinal and bladder sphincter muscle contraction |
|
|
a2 receptor
|
Gi
Decreased sympathetic outflow, decreased insulin release, decreased lipolysis, increased platelet aggregation |
|
|
b1
|
Gs
Increase heart rate, increased contractility, increased renin release, increased lipolysis |
|
|
b2
|
Gs
Vasodilation, bronchodilation, increased heart rate, increased contractility, increased lipolysis, increased insulin release, decreased uterine tone (tocolysis), ciliary muscle relaxation, increased aqueous humor production |
|
|
M1
|
Gq
CNS, enteric nervous system |
|
|
M2
|
Gi
Decrease heart rate and contractility of atria |
|
|
M3
|
Gq
Increase exocrine gland secretions (e.g: lacrimal, gastric acid), increased gut peristalsis, increased bladder contraction, bronchoconstriction, increase pupillary sphincter muscle contraction (miosis), ciliary muscle contraction (accommodation) |
|
|
D1
|
Gs
Relaxes renal vascular smooth muscle |
|
|
D2
|
Gi
Modulates transmitter release, especially in brain |
|
|
H1
|
Gq
Increases nasal and bronchial mucus production, contraction of bronchioles, pruritus, and pain (allergy symptoms) |
|
|
H2
|
Gs
Increased gastric acid secretion |
|
|
V1
|
Gq
Increased vascular smooth muscle contraction |
|
|
V2
|
Gs
Increased water permeability and reabsorption in the collecting tubules of the kidney (V2 is found in the 2 kidneys) |
|

|

|

