![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
142 Cards in this Set
- Front
- Back
|
How long should it take to breathe out the forced vital capacity? In what circumstances is it lengthened? In what circumstances is it reduced?
|
Forced vital capacity should take 4 s. if it takes 8 s, then there’s obstructive lung disease in the lower airways (asthma, COPD).
Too fast is generally a sign of restrictive lung disease with lung fibrosis (e.g., IPF). |
|
|
What is a normal FEV 1.0/FVC ratio?
|
FEV 1.0/FVC ~ 0.75- 0.8 in a young, healthy person.
It will be lower in obstructive lung disease and higher in restrictive disease. |
|
|
What is a flattened inspiratory loop indicative of?
|
A flattened inspiratory loop is indicative of inadequate effort on the part of the patient or an upper airway problem.
|
|
|
What anatomical/physiological factors determine FRC?
|
FRC is determined by the inward elastic recoil of lung parenchyma and the outward elastic recoil of the chest wall.
|
|
|
Why is the expiratory loop of the flow-volume loop asymmetric?
|
The expiratory loop of the flow-volume loop is asymmetric, because flow rates are greater at high lung volumes, because that is when the airways are most open (i.e., elastic recoil pressure is high and airway resistance is low).
|
|
|
How do obstructive lung diseases and restrictive defects affect lung volumes?
|
• Obstructive lung diseases may increase lung volumes
o Due to decreased elastic recoil pressure (you have holes in the lung tissue in emphysema) • Restrictive defects lower lung volumes o Due to increased elastic recoil pressure |
|
|
In what diseases/disorders does the diffusing capacity decrease? Increase?
|
• Decrease – due to
o Anemia o Emphysema o Interstitial lung disease o Pulmonary vascular diseases • Increases o Polycythemia o Diffuse alveolar hemorrhage (increased hemoglobin in areas of intact ventilation) |
|
|
What pathologies can cause a flattened inspiratory loop on the flow-volume curve (e.g., vocal cord dysfunction)?
|
Upper airway obstructions:
• Vocal cord dysfunction • Epiglottitis • Laryngeal edema • Laryngeal malignancy |
|
|
What are examples of diffusion limitation in hypoxemia?
|
• Idiopathic pulmonary fibrosis
• Emphysema |
|
|
How do you measure the severity of hypoxemia in patients requiring mechanical ventilation?
|
On supplemental oxygen, the FiO2 is not known exactly, which limits calculation using the alveolar gas equation. Thus, the metric used is the PaO2 to FiO2 ratio (P/F). A P/F ratio > 450 is generally viewed as normal.
|
|
|
What are the 3 situations that cause hypoxemia and result in a widened A-a gradient?
|
1) Shunt
2) Low V/Q ratio a. In patients with low V/Q, increasing the fraction of inspired oxygen readily increases PaO2 3) Diffusion limitation a. Increased interstitial thickening (e.g., pulmonary fibrosis can limit diffusion and cause hypoxemia b. Decreased area available for diffusion (emphysema) can limit diffusion and cause hypoxemia |
|
|
What are the 3 situations that cause hypoxemia and do NOT result in a widened A-a gradient?
|
This happens when the reason for low PaO2 is a low PAO2. This can be figured out from the alveolar gas equation.
1. Hypercapnia (hypoventilation) a. As PaCO2 increases, PAO2 falls, lowering PaO2. b. Taking heroin would suppress respiration 2. Low barometric pressure a. In Denver, Patm is 640 mm Hg 3. Low FiO2 (below 0.21) a. Rare, but occurs in inhalation injuries/fires when other gases dilute the FiO2 4. Lowering R a. Silly reason |
|
|
What is a minimum O2 saturation you would look to achieve in a pt with hypoxemia for their safety?
|
90% saturation – 60mm Hg <- good for patient safety
Other saturations: 75% saturation – 40 mm Hg 97.5% saturation – 100 mm Hg |
|
|
Why should you be wary of over-oxygenation of a patient?
|
Over-oxygenation must be avoided in clinical practice, because supplemental oxygen therapy to some patients with COPD causes an increase in PaCO2. The magnitude of this increase is small and insignificant in some patients, but others develop critical hypercapnia and acidemia.
|
|
|
What is the equation for the Partial pressure of carbon dioxide in arterial blood?
|
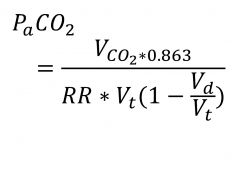
(see image)
|
|
|
What are signs/ symptoms associated with pneumonia?
|
• Symptoms
o Cough (dry or productive of sputum) o Dyspnea o Fever • Signs o Dullness to percussion o Bronchial breath sounds o E->A changes (reflecting presence of fluid in the alveolar air spaces altering the transmission of sound) |
|
|
What’s the most common cause of pneumonia/pathogenesis?
|
Aspiration of upper airway flora
Pneumonia develops when organism load or virulence overwhelms host defenses, resulting in accumulation of organisms, inflammatory cells and fluid in the interstitium and alveolar spaces of the lung. |
|
|
Whenever there’s aspiration/large volume aspiration, where in the lungs does the aspirate tend to go?
|
It tends to go more to the right middle lobe, lower lobe, and left lingulum
|
|
|
What are top causes of community-acquired pneumonia (CAP)?
|
• Steptococcus pneumonia (top dawg)
• Haemophilus influenza • Mycoplasma pneumonia • Chlamydophilia pneuomniae • Legionella pneumophila |
|
|
What are top nosocomial causes of pneumonia?
|
• Pseudomonas aeurginosa
• Enteric GNB o Enterobacter o E. coli o Klebsiella o Proteus o Serratia • H. influenzae |
|
|
What is a standard empiric abx therapy for community-acquired pneumonia?
|
• Respiratory fluoroquinolone (moxifloxacin or levofloxacin)
Or • Beta-lactam plus a macrolide (e.g., ceftriaxone + azithromycin) |
|
|
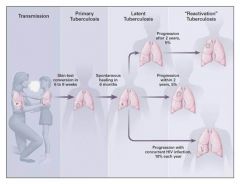
Where does TB initially infect?
|
TB initially infects in the well-ventilated areas: the mid and lower lung fields.
|
|
|
What histopathological characteristics go along with tuberculous infection?
|
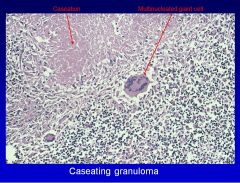
Caseating granulomas
|
|
|
What is the Ghon complex?
|
• The Ghon complex is the residual of the primary infection form tuberculosis and is often present in the lower middle lobes.
• Necrosis and calcification of the initial pulmonary focus and draining regional lymph nodes The lesions consist of a calcified focus of infection and an associated lymph node. |
|
|
Where does reactivation TB tend to present?
|
Reactivation TB tends to present in the apical posterior portion of the lung rather than the lower middle lung field infection of primary TB.
|
|
|
What is the common clinical presentation of TB?
|
• Fever, night sweats, weight loss, SOB, hemoptysis
• Cough > 2 weeks • History of exposure to infectious TB or positive TST • CXR: upper lobe infiltrate, cavitary infiltrate, hilar/paratracheal adenopathy. |
|
|
What CSF formula is indicative of tuberculosis?
|
• Lymphocytic or mixed pleocytosis (Pleocytosis is an increased cell count {Gk. pleion more}, particularly an increase in white blood cell (WBC) count, in a bodily fluid, such as cerebrospinal fluid (CSF). It is often defined specifically as an increased WBC count in CSF. It is indicative of an inflammatory, infectious, or malignant condition.)
• High protein • Low glucose (sometimes later in course) |
|
|
What is the standard regimen of therapy for tuberculosis?
|
• Standard regimen: 2 months of 4 drugs: Isoniazid, Rifampin, Ethambutol plus Pyrazinamide followed by 4 months of two drugs: Isoniazid plus Rifampin
|
|
|
How is MDR TB defined?
|
• Resistance to at least INH and Rifampin
• Primary vs. acquired MDR-TB – Primary = patient initially infected by MDR-TB – Acquired = poor adherence to Rx, selection of resistant bacteria |
|
|
Which nontuberculous mycobacteria (NTM) grow best at body temperature?
|
• The slowly-growing mycobacteria (growth in >7 days) grow best at body temperature:
• MAC (M. avium and M. intracellulare) • M. kansasii |
|
|
What is the standard treatment for MAC/what are the primary agents?
|
The primary agents are macrolides:
– Primary agents • Clarithromycin (or Azithromycin) plus Rifampin (or Rifabutin) plus Ethambutol x 12-18 months • +/- Streptomycin (or Amikacin) x first 2-3 months – Alternative agents • Fluoroquinolones, Clofazimine, Linezolid • Surgical resection – May be useful when medical therapy fails |
|
|
With what organism do you get a mediastinal fibrosis?
|
• Histoplasmosis; you also get:
• Mediastinal lymphadenitis • Cavitary pulmonary histoplasmosis • Progressive disseminated histoplasmosis (PDH) What’s the typical initial immune/inflammatory response to blastomycosis? Clusters of neutrophils and noncaseating granulomas with epithelioid and giant cells. |
|
|
When you hear “broad-based budding yeast,” which organism should you think about?
|

Blastomycosis
|
|
|
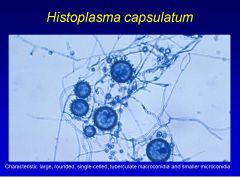
What are important characteristics of Histoplasma capsulatum?
|
• Histoplasma
o Along the Ohio and Mississippi rivers and in the carribean o Acquired by inhalation of dust particles from soil contaminated with bird or bat droppings that contain small spores o Produces epitheliod granulomas (caseating or noncaseating) o Most primary infections are asymptomatic o Yeast visualized poorly by H&E stain, better seen with PAS and Gomori-ethenamine silver stains |
|
|
What are important characteristics of Blastomyces dermatitidis?
|
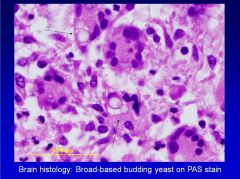
• Blastomyces
o Central and southeastern U.S. o Broad-based budding o Clinical presentation Abrupt illness with productive cough, headache, chest pain, weight loss, fever, abdominal pain, night sweats, chills, and anorexia o Treatment Amphotericin B and itraconazole |
|
|
What are important characteristics of Coccidioides immitis?
|
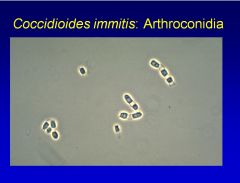
• Cocciodides
o Southwest, Far West of the U.S. and Mexico o Most primary infections are asymptomatic o Vast majority of early infections resolve without specific antifungal treatment o Cannot be detected by gram staining, use cytology for spherules or H&e of tissue o Severe pneumonia, chronic progressive fibrocavitary pulmonary or disseminated disease Amphotericin B, fluconazole or itraconazole |
|
|
What are important characteristics of Aspergillosis?
|
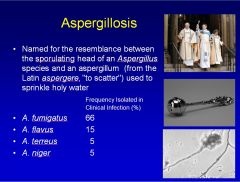
• Clinical manifestations
o Fever, chest pain, SOB, cough, hemoptysis • Treatment o Antifungal therapy: voriconazole (52% response), amphotericin B (31%) o Recovery of neutrophils in patients with neutropenia is critical to recovery |
|
|
What are the 3 most common NTM causes of chronic bronchopulmonary disease?
|
• M. avium complex
• M. kansasii • M. chelnoae-abscessus |
|
|
What are the 3 most common NTM causes of skin abscesses?
|
• M. marinum
• M. chelonae-abscessus • M. fortuitum |
|
|
What is the most common NTM cause of disseminated infection?
|
M. avium complex
|
|
|
What are important characteristics and treatment of Pneumocystis jiroveci?
|
• Typically does not occur until CD4 count < 200
• Treatment of choice o Trimethoprim-sulfamethoxazole |
|
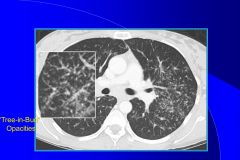
What is the tree-in-bud finding on CT indicative of?
|

Sarcoidosis
|
|
|
Which interstitial lung disease is more likely to have honeycomb change, UIP/IPF or NSIP (nonspecific interstitial pneumonia)?
|
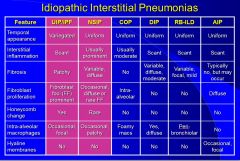
UIP/IPF
Honeycomb change is rare in NSIP |
|

What is this CT finding indicative (hint: it’s an interstitial lung disease)?
|
Traction Bronchiectasis -> IPF
Traction bronchiectasis is a finding of abnormal airway dilation due to lung fibrosis. |
|
|
What are important drug causes of interstitial lung disease?
|
• Bleomycin
• Methotrexate • Nitrofurantoin • Amiodarone (causes IPF in 10-15% of pts) • Hydralazine • Busulfan |
|
|
What are the Wells criteria?
|
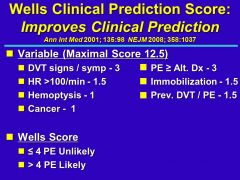
Wells criteria helps determine whether or not PE is present
(see image) |
|
|
What are top signs/symptoms of PE?
|
• Over 90% of patients with PE will present with 1 of 3 syndromes:
o Pleuritic chest pain +/- hemoptysis o Unexplained dyspnea o Shock/loss of consciousness • Top 3 symptoms o Chest pain o Dyspnea o Cough • Top 3 signs o RR>16/min o Loud P2 o Pulse > 100/min |
|
|
Can you describe the pathogenesis of emphysema?
|
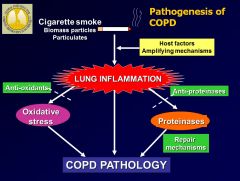
• Environmental exposure (e.g., cigarette smoke) results in exaggerated inflammatory response which results in oxidative stress and proteinases, which destroy the lung, resulting in the formation of emphysema
• COPD is characterized by CD8 influx into the lungs and neutrophils; it’s a neutrophil-predominant disease • Neutrophils release proteases and MMPs which result in matrix wall destruction, which result in alveolar wall destruction • There’s also mucus hypersecretion |
|
|
Why do the upper lobes of the lungs get larger in COPD?
|
Why do the upper lobes of the lungs get larger in COPD?
In COPD, the upper lobes are bigger than the lower lobes, because that’s where more emphysema is, and the lungs lose their elastic recoil pressures |
|
|
What are the 3 disease processes associated with COPD?
|
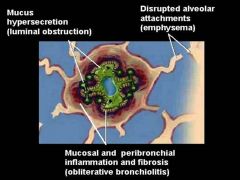
Everyone with COPD has emphysema and chronic bronchitis and peribronchiolar fibrosis, so the 3 are: 1) emphysema (destruction of lung alveolar air sacs), 2) chronic bronchitis (mucus in the airways) 3) peribronchiolar fibrosis (the smaller airways getting squeezed shut)
The problem isn’t air getting in the lung; it’s too much air staying the lung when someone tries to breathe out 3 sources of airway obstruction: 1) Lost of elastic recoil pressure due to emphysema 2) Peribronchiolar fibrosis due to small airway changes 3) Lungs are full of mucus |
|
|
What are 2 important distinguish features between COPD and asthma?
|
1) Unlike asthma, the airway smooth muscles are not enlarged in COPD
2) The subendothelial basement membrane is not thickened in COPD |
|
|
Can you describe the changes in the Flow-Volume and Volume-Time curves in COPD?
|
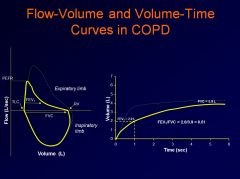
When there’s COPD, you get loss of elastic recoil pressure (due to emphysema) and increased airway resistance (due to peribronchiolar fibrosis – narrowing of airways)
Thus, only 50% of air comes out in the 1st second, and the patient keeps breathing out Note the scooping of the Flow-Volume curve and the extended rise of the Volume-Time curve. Inspiratory flow is not affected at all; it’s air getting out of the lungs that’s the problem. FEV1/FVC of < 0.7 after a bronchodilator = COPD. |
|
|
What is the cause of breathlessness in COPD patients?
|
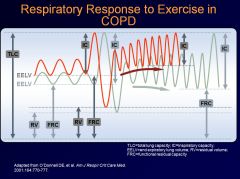
With each successive breath, more and more air gets left in the chest
Inefficient response to exercise: there’s a progressive increase in end expiratory lung volume, and there’s a progressive decrease in inspiratory capacity due to airflow obstruction (air cannot get out of the chest, and more air accumulates in the chest with each successive breath) Breathlessness is a major symptom of COPD Dynamic lung hyperinflation is the cause of breathlessness and exercise limitation in COPD |
|
|
What are the mainline treatments of COPD and asthma?
|
• COPD mainline treatment are bronchodilators, and inhaled steroids are added if there’s recurrent exacerbations
• Asthma mainline treatment is inhaled steorids, and bronchodilators are added if they can’t maintain good control |
|
|
Can the FEV1 be used to predict exercise capacity in COPD patients?
|
FEV1 does not correlate well with exercise capacity or quality of life in COPD patients.
|
|
|
What are the criteria for ARDS?
|
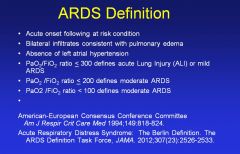
(see image)
|
|
|
What are the mechanisms of injury in ARDS?
|
• Activation of inflammatory mediators and cellular components resulting in damage to capillary endothelial and alveolar epithelial cells
• Increased permeability of the alveolar-capillary membrane • Influx of protein-rich edema fluid and inflammatory cells into airspaces • Dysfunction of surfactant |
|
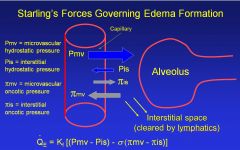
In reference to Starling’s equation, what are some medicinal strategies for lowering Pmv?
|
• Diuresis
• Nitroglycerin • Morphine • Phlebotomy |
|
|
What is the most important cause of ARDS?
|
Sepsis syndrome
Other causes: Severe multiple trauma Aspiration pneumonia |
|
|
What is ARDS?
|
• ARDS is a life-threatening reaction to injuries or acute infection to the lung. It’s a severe lung syndrome (not a disease) with direct and indirect causes.
• Inflammation of the lung parenchyma leads to impaired gas exchange with systemic release of inflammatory mediators, causing inflammation, hypoxemia, and frequently multiple organ failure. |
|
|
Where in the mediastinum would you expect to find thymomas?
|
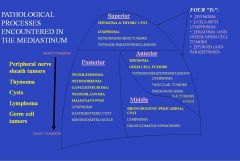
Either anterior or superior mediastinum
|
|
|
What are the most common mediastinal tumors?
|
• The most common mediastinal tumors are neurogenic tumors (20%; typically in the posterior midastinum),
• followed by thymoma (19%; anterior/superior mediastinum), • cysts (18%), • lymphoma (13-15% usually anterior/superior or middle mediastinum), and • germ cell tumors (10%, anterior mediastinum |
|
|
What percentage of symptomatic mediastinal lesions are malignant neoplasms?
|
• 50% of symptomatic mediastinal lesions are malignant neoplasms
• 90% of asymptomatic lesions are benign • Symptoms include: o Chest pain, dyspnea, cough |
|
|
What tumor is indicated typically be elevated levels of beta-HCG? Alpha-fetoprotein?
|
• Beta-HCG->Highly aggressive choriocarcinoma
• Alpha-fetoprotein->yolk sac tumor |
|
|
What’s the best shot at reducing lung cancer mortality?
|
CT screening
|
|
|
What is the most common oncogene in lung cancer?
|
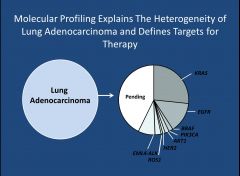
Kras
|
|
|
What’s more common, small cell or non-small cell lung cancer?
|
• Non-small cell lung cancer > 85%
• Small cell lung cancer < 15% |
|
|
Which type of lung cancer is almost always associated with smoking?
|
• Squamous cell carcinoma
• Small cell carcinoma |
|
|
What mutation is seen in 50% of lung cancers?
|
P53
|
|
|
Which respiratory bacterial pathogen is “lancet-shaped?”
|
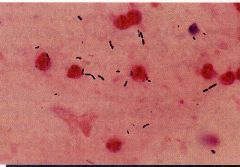
• Streptococcus pneumonia; #1 cause of community-acquired pneumonia
• Has capsule o protects bacteria from phagocytosis o 80 distinct serotypes • Pneumolysin – o degrades Hb to greenish pigment, o activates complement o may form pores in human cells • peptidoglycan fragments and teichoic acid o both activate complement->intense inflammation+tissue destruction |
|
|
S. pneumoniae (aka. Pneumococci) loves to cause secondary infection in people with what ailments?
|

• alcoholism
• HIV infection • liver failure • kidney failure • antecedent viral respiratory infection (e.g. influenza) |
|
|
How would S. pneumoniae appear in a gram stain?
|

• Numerous gram(+) cocci in pairs and chains
• Many PMNs • On blood agar, it’s alpha-hemolytic • Catalase-negative, optochin-susceptible |
|
|
What’s the best way to treat S. pneumoniae?
|

• Penicillin is historically the treatment of choice
• Alternatives o Cephalosporins o Doxycycline o TMP-SMX o Macrolides o Clindamycin o Vancomycin o Newer quinolones (moxifloxacin) • Do NOT use ciprofloxacin! It has limited efficacy<-appears on boards |
|
|
What are important characteristics of Haemophilus influenzae?
|
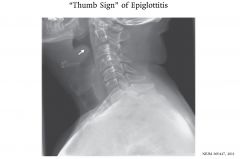
• Small, gram(-) coccobacilli
• Can cause epiglottitis • Infects children mostly, because most adults have protective antibodies • Some isolates have beta-lactamase, so penicillin may not be effective |
|
|
What are important characteristics of mycoplasma pneumoniae?
|
• Extracellular pathogen
• Lacks cell walls, pleomorphic in shape • Smallest organism that can be free-living in nature and self-replicating on lab medium • Tightly adheres to respiratory epithelium with protein adhesion P1 • Causes atypical pneumonia o Gradual onset o Cough w/o sputum o Common in young people o Non-lobar infiltrates on CXR • Treat with erythromycin and tetracycline; due to no cell wall, penicillin won’t work |
|
|
What is the leading cause of hospital-acquired pneumonia?
|
• Staph aureus
Other common causes: • Enterobaceriaceae (E. coli, Klebsiella pneumonia, Enterobacter spp., Serratia spp.) • Legionella pneumophila • Pseudomonas aeruginosa |
|
|
What would be a bacterial ddx for pharyngitis?
|
• S. pyogenes
• Chlamydia pneumonia • Mycoplasma pneumonia • Cornebacterium diphtheria |
|
|
What would be a bacterial ddx for otitis media?
|
• S. pneumonia
• Haemphilus influenza • S. pyogenes • Moraxella catarrhalis |
|
|
What would be a bacterial ddx for sinusitis?
|
• S. pneumonia
• H. influenza • M. catarrhalis |
|
|
Which bacteria can cause an atypical pneumonia?
|
• Chlamydia pneumoniae
• Mycoplasma pneumoniae • Legionella pneumophila |
|
|
What’s the difference between an atypical pneumonia and a typical pneumonia?
|
Atypical pneumonias have gradual onset, SOB, and cough without sputum accompanied by URI symptoms, while typical pneumonias are associated with abrupt onset, production of sputum, and a very ill patient.
|
|
|
What are the remodeling changes that occur with chronic asthma?
|
• Cellular proliferation
o Smooth muscle, mucous • Increased matrix protein deposition • Basement membrane thickening • Angiogenesis Remember that nothing happens to the alveoli; it’s an airway disease. Shortly, • smooth muscle hypertrophy, • sub-epithelial basement membrane thickening, • goblet cell hyperplasia, • angiogenesis |
|
|
What are the criteria for intermittent asthma (vs. persistent asthma)?
|
If they have symptoms 2 or less times/week, night time symptoms 2 or fewer times per month and require rescue inhaler 2 or less times per week…and they have normal FEV1, then they have intermittent asthma
If any of the above is not true, then they do not have intermittent asthma; they have persistent asthma. It’s important to distinguish between the two, because people with persistent asthma need an asthma controller therapy. If you have intermittent asthma, you’re good with a short-acting bronchodilator |
|
|
Which allele is associated with increased risk of OSAH?
|
APOE epsilon4
|
|
|
How do estrogen and testosterone affect sleep apnea?
|
• Estrogen is protective against sleep apnea
• Testosterone helps induce sleep apnea |
|
|
How does muscle tone and fatigability in the apneic patient differ from normal?
|
Apneic patients have greater muscle tone (i.e., stronger muscles), but their muscles are more fatigable (e.g., genioglossus and tensor palatine).
|
|
|
What are the components of the STOP BANG screening tool?
|
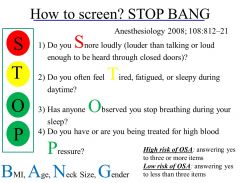
See image
(stop_bang) |
|
|
What’s the Mallampati classification?
|
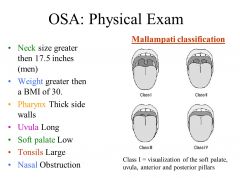
The Mallampati classification is used by anesthesiologists to grade how easy it would be to insert a breathing tube into a patient. It’s also used to determine risk for OSA.
|
|
|
How does OSA affect sympathetic tone and cardiac preload and afterload?
|
OSA elevates sympathetic tone, cardiac preload and afterload
|
|
|
What criteria defines OSA?
|
An apnea hypopnea index (i.e., the number of apneas plus hypopneas per hour of sleep) > 5 defines OSA. However, clinically significant and potentially serious complications do not occur until the AHI > 15.
|
|
|
What are important characteristics of ARDS/Diffuse Alveolar Damage?
|
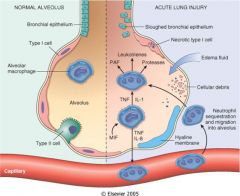
• Clinical and pathological result of acute alveolar injury
• Pathogenesis is damage to alveolar capillaries & epithelium • Could be caused by infections, ionizing radiation, O2 toxicity, chemotherapy, sepsis, gastric aspiration, and other causes • Increased capillary permeability resulting in interstitial and intra-alveolar edema, fibrin exudation and hyaline membrane formation. |
|
|
What histopathological feature is a hallmark for ARDS/DAD?
|
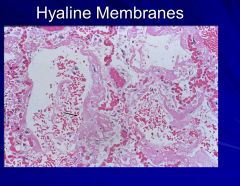
Hyaline membranes
|
|
|
What are important characteristics of usual interstitial pneumonitis (UIP)?
|
• Pathogenesis – alveolitis, interstitial inflammation, diffuse fibrosis
• Morphology – thickening of the interstitial wall alternating with normal lung • End stage lung – honeycomb lung • Grosss findings o Small lung o Cobble-stone appearance of pleural surface o Cut section shows diffuse fibrosis predominantly in the lower lobes o Honeycomb cystic spaces |
|
|
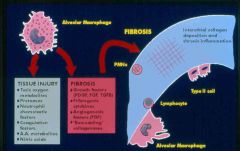
What are important characteristics of sarcoidosis?
|
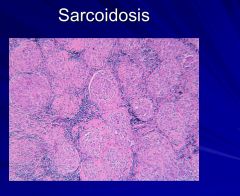
Morphology – noncaseating granulomas
Pathogenesis – exaggerated cellular immune response by helper T lymphocytes to exogenous antigens or autoantigens |
|
|
What are important characteristics of Granulomatosis with polyangiitis (aka. Wegener’s granulomatosis)?
|
• Acute necrotizing granulomas of the upper and lower respiratory tract
• Renal disease – glomerulonephritis • C-ANCA (+) |
|
|
What are important characteristics of pulmonary alveolar proteinosis (PAP)?
|
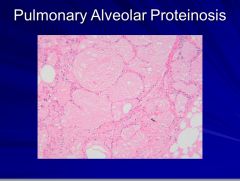
Alveoli filled with dense, homogenous precipitate without any inflammation
|
|
|
What are important characteristics of lymphangioleimyomatosis (LAM)?
|
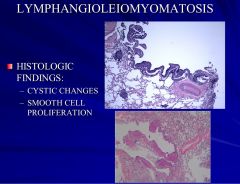
• Abnormal proliferation of smooth muscle cells in the lungs, lymphatics and lymph nodes of the thorax and retroperitoneum
• Affects women of reproductive age group |
|
|
What are important characteristics of desquamative interstitial pneumonitis (DIP)?
|
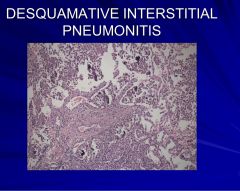
• Smoking related
• Morphology – accumulation of macrophages within alveolar spaces with minimal interstitial fibrosis • Early stage/precursor of usual interstitial pneumonitis |
|
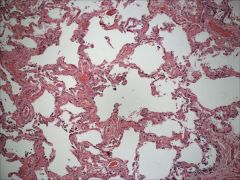
What lung disease is this ?
|
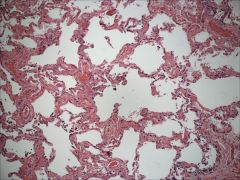
NSIP
|
|
|
What are important characteristics of organizing pneumonia?
|
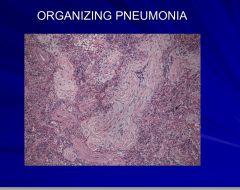
• Infectious –viral or bacterial
• Inflammatory – inhaled toxins, drugs, collagen vascular disease and GVHD • Idiopathic – cryptogenic organizing pneumonia |
|
|
What are important characteristics of hypersensitivity pneumonitis?
|
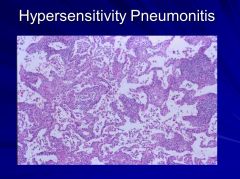
• Pathogenesis – immunologic response to a variety of inhaled antigens. Combination of cell-mediated and immune complex-mediated hypersensitivity reaction
• Thermophilic actinomycetes one of the common etiologic agents • Morphology – bronchiolitis, interstitial inflammation and vague granuloma formation |
|
|
What’s Starling’s equation for the lung?
|
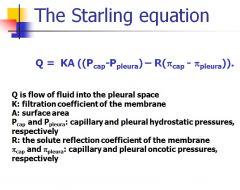
See image
|
|
|
What are Light’s criteria?
|
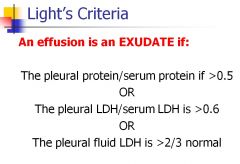
The pleural protein/serum protein if >0.5
OR The pleural LDH/serum LDH is >0.6 OR The pleural fluid LDH is >2/3 normal |
|
|
What are the transudate causes of effusions?
|
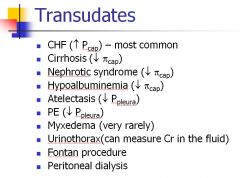
See image
|
|
|
What are the main exudative causes of effusions?
|
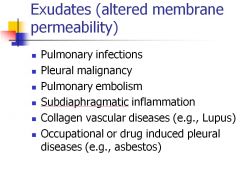
see image
|
|
|
What are the top 4 causes of pleural effusion in the U.S.?
|
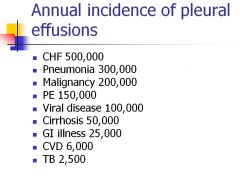
• CHF
• Pneumonia • Malignancy • PE (remember this causes both exudative and transudative effusions) |
|
|
What are the criteria for a complicated pleural effusion?
|
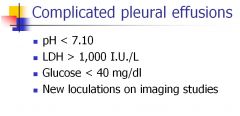
• Ph < 7.0
• LDH > 1,000 IU/L • Glucose < 40 mg/dL • New loculations on imaging studies |
|
|
Besides a complicated pleural effusion, what are causes of low pH effusions?
|
• Parapneumonic effusion
• Malignancy • Esophageal rupture • Urinothorax The pH of pleural fluid is usually higher than serum due to active transport of bicarbonate across the membrane. Low pH pleural effusion are seen almost exclusively in infected parapneumonic effusions (pleural effusions adjacent to a pneumonia), malignancies with extensive pleural involvement, and esophageal perforation. |
|
|
What are common low glucose effusions?
|
• Complicated parapneumonic effusions
• Empyema • Rheumatoid arthritis • Tuberculosis • Malignancy |
|
|
What are common high amylase effusions?
|
• Pancreatitis
• Esophageal rupture • Malignancy • Other intrabdominal processes |
|
|
What’s the definition of a tension pneumothorax?
|
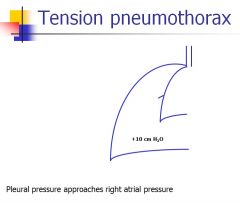
Tension pneumothorax: the pressure in the pleural space starts to approach right atrial pressure, which causes venous return to decrease/be impaired. Tension pnpeumothorax requires immediate drainage of the pleural space.
|
|
|
Why can elevated left atrial pressures lead to pleural effusion?
|
The arterial supply of the pleura arises from the systemic circulation. Venous drainage is into the left atrium. Therefore elevate left atrial pressures (as in heart failure) result in pleural effusions.
|
|
|
What are the different WHO Groups clinical classifications for pulmonary HTN?
|
• Group 1 – PAH
• Group 2 – PH owing to left heart disease o Systolic dysfunction o Diastolic dysfunction o Valvular disease • Group 3 – PH owing to lung diseases or hypoxia o COPD o Interstitial lung disease o Sleep-disordered breathing o etc • Group 4 – Chronic thromboembolic PH • Group 5 – unclear multifactorial mechanisms |
|
|
What is the only curable form of pure pulmonary artery hypertension?
|
WHO Group 4 – chronic thromboembolic PH
|
|
|
What is the gold standard test for patients you think might have pure pulmonary HTN?
|
Right heart catheterization
|
|
|
What are typical symptoms of PAH?
|
Symptoms of PAH are often non-specific and may include:
• Progressive onset of exertional dyspnea (60%) • Fatigue (19%) • Chest pain or discomfort (17%) • Dizziness and light-headedness; possible history of near syncope or syncope (13%) • Raynaud’s phenomenon (10%) • Palpitations (5%) • Ortner’s syndrome: hoarseness from compression of left recurrent laryngeal nerve by enlarged pulmonary artery <1%) |
|
|
What are clinical signs of PAH?
|
• Accentuated second heart sound (loud P2)
• Notable heart murmur—tricuspid valve regurgitation • RV lift • RV Failure – Right sided third heart sound – JVD – Hepatomegaly – Peripheral edema – Ascites |
|
|
Which of the pulmonary HTN WHO groups has pulmonary vasodilators to be indicated?
|
WHO Group 4 can have pulmonary vasodilators used as a bridge to surgery or for non-operative candidates
|
|
|
What is the strongest predictor of morbidity/mortality in a cystic fibrosis patient?
|
Pulmonary manifestations are the strongest predictors of morbidity/mortality in CF patients.
|
|
|
Is there any risk for morbidity in heterozygous carriers of cystic fibrosis mutations?
|
Over the past decade, it was observed that persons who carry one copy or a mutant CF gene are at increased risk for pancreatitis. CFTR mutations have also been associated with increased risk for liver cirrhosis.
|
|
|
What are the predominant organisms causing airway infections in cystic fibrosis?
|
• Staph aureus
• Pseudomonas aeruginosa |
|
|
What are GI tract manifestations of illness in cystic fibrosis patients?
|
• 85% of CF patients have pancreatic exocrine insufficiency and malabsorption due to pancreatic obstruction and fibrosis.
• Abnormally viscous secretions in the intestinal tract lead to various intestinal obstruction syndromes, including meconium ileus in newborns and distal intestinal obstruction syndrome in others. • Liver involvement includes obstructive jaundice in infants and cirrhosis in children and young adults. |
|
|
What is the cause and rate of infertility in cystic fibrosis patients?
|
Obliteration of the vas deferens in males leads to infertility in 98% of CF men.
Females have increased viscosity of cervical and vaginal mucus and increased frequency of anovulatory menstrual cycles which slightly diminish their fertility. |
|
|
What common viral pathogens attack/inhabit the nasopharynx?
|
• Rhinovirus
• Coronavirus • Coxsackie virus |
|
|
What common viral pathogens attack/inhabit the oropharynx?
|
• Epstein-Barr virus
• Adenovirus • Enteroviruses |
|
|
What common viral pathogens attack/inhabit conjunctiva?
|
• Adenovirus
• Herpesviruses |
|
|
What common viral pathogens attack/inhabit larynx-trachea?
|
Parainfluenza viruses
|
|
|
What common viral pathogens attack/inhabit the bronchi?
|
• Influenza viruses
• Measles virus |
|
|
What common viral pathogens attack/inhabit the bronchioles?
|
RSV (Respiratory syncytial virus)
|
|
|
What are important characteristics of adenoviruses?
|
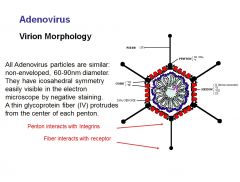
• Frequent cause of URIs
• Linear, nonsegmented d/s DNA genome |
|
|
What are important characteristics of coronaviruses?
|
• Common cause of URIs; occasionally causes enteric infections mostly in infants > 12 mo.
Genome is non-segmented s/s (+) sense RNA • Can cause SARS |
|
|
What are important characteristics of orthomyxovirus (influenza)?
|
• 3 different antigenic types of the virus: A, B, C
o A and B cause most epidemics in the world o by age 15, most people have developed Abs to C • Hemagglutinins (H antigen) and neuraminidases (N antigen) are important in pathogenesis o H required for binding of virus to cell o N helps mature virus escape from the cell • Symptoms o Fevers, chills, rigors, headache, congested conjunctiva, extreme prostration with myalgia in back and limbs, infection of pharynx and conjunctiva |
|
|
What are important characteristics of paramyxoviruses?
|
• 3 genera
o Paramyxovirus: Parainfluenza virus 1-4; mumps o Pneumovirus: RSV o Morbilivirus: measles; canine distemper virus • (-) sense RNA genome • Measles o Dry cough, sore throat, conjunctivitis followed by characteristic red, maculopapular rash and Koplik's spots – raised red spots with white centres in the mouth o Complications include bronchopneumonia and otitis media, encephalitis (rare) |
|
|
What are important characteristics of picornaviruses?
|
• S/s (+) sense RNA virus
|
|
|
What is albuterol?
|
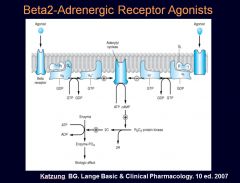
• Albuterol or salbutamol (INN) is a short-acting Beta2-adrenergic receptor agonist (a rescue inhaler) used for the relief of bronchospasm in conditions such as asthma and COPD. It relaxes smooth muscle and causes fast bronchodilation by the following mechanism. It 1) binds to GPCRs 2) adenylate cyclase gets activated 3) inducing cAMP formation 4) phosphorylating muscle regulatory proteins and changing cellular calcium concentrations 5)ultimately relaxing airway smooth muscle.
• (works in 2-5 min) • To be used as needed up to every 4-6 hours • If a pt requires it more than 2x/ week, they’re a candidate for controller therapy • Side effects o Tremor o Palpitations o Arrhythmias o Hypokalemia o hyperglycemia |
|
|
What are Leukotriene modifiers, and what is their use?
|
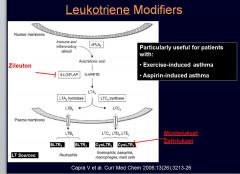
• Leukotriene modifiers are asthma controllers. Some include:
• Zileuton (5-LO inhibitor) • Montelukast (CysLTR1 inhibitor) • Zafirlukast (CysLTR1 inhibitor) |
|
|
What are methylxanthines, how do they work, and what is their use?
|
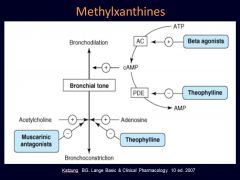
Methylxanthines (e.g., Theophylline) act as bronchodilators, blocking phosphodiesterase and increasing availability of cAMP.
|
|
|
How are long-acting beta-agonists (LABAs) used in asthma? How about COPD?
|
• LABAs (e.g., salmeterol, formeterol) result in long-term symptom control in both asthma and COPD
• In asthma, must be used in combination with inhaled corticosteroid (ICS), because monotherapy is associated with deterioration in asthma control and more frequent exacerbations o Fluticasone-salmeterol combo o Budesonide-formoterol o Mometasone-formoterol • In COPD, combined with inhaled corticosteroid (ICS) o Improved FEV1 vs LABA alone o Fewer exacerbations than LABA alone |
|
|
What long-acting anticholinergic agent would be useful for COPD?
|
• Tiotropium
• Used in COPD – still under investigation in asthma • Better symptom control than short acting agents (1x daily inhalation) • Blocks M1 and M3 as opposed to ipratropium that blocks 1,2, and 3 • Side Effects o Dry mouth o Cough o Blurred vision o Worsening narrow-angle glaucoma o Urinary retention |
|
|
What are 2 examples of dead space conditions?
|
• PE
• Emphysema Dead space is wasted ventilation (V/Q = infinity), favors hypercapnia. |
|
|
What are diffusion limitation diseases?
|
• IPF
• Emphysema |
|
|
What are examples of low V/Q that are not shunt?
|
• COPD
• Asthma • PE |

