![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
44 Cards in this Set
- Front
- Back
|
Epidemiology of UTIs:
|
*Most common bacterial infection
*Women are more likely to experience UTI than men *Almost half of all women will experience a UTI during their lifetime *Estimated annual cost: $1.6 billion |
|
|
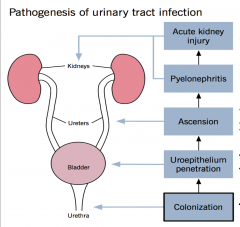
Pathogenesis of UTI:
|
|
|
|
What determines which are uropathogenic bacteria?
|
*Virulence factors
-Enable attachment to urinary tract by overcoming host defenses -Scavenge limiting nutrients (iron) from the host -Perturb host cells and tissues --> symptomatic UTI -E. coli – most common |
|
|
Virulence factors for bacteria in UTI:
adhesins: |
*Adherence to uroepithelium
*Facilitate colonization and subsequent bacterial-host interactions *Resist flushing by urine flow and bladder emptying *Most adhesins are fimbrial *Type 1 fimbriae (common pili)- Bind to mannose receptors *P fimbriae- Bind to galactose receptors |
|
|
Virulence factors for bacteria in UTI:
siderophores: |
*Iron is a limiting micronutrient for host-invading bacteria
*Consequently, bacteria have developed mechanisms that help them extract iron from the host with the help of siderophore-receptor systems. |
|
|
Virulence factors for bacteria in UTI:
toxins: |
*Cause abnormalities in host cell function and morphology, or cellular lysis
|
|
|
Virulence factors for bacteria in UTI:
Evading host defenses: |

*Polysaccharide capsules
-Interfere with phagocytosis -Protect against complement-mediated opsonization or lysis *LPS (lipopolysaccharide) -->Inflammatory cascade, Cytokines, Neutrophil influx, Pain and edema, Fever, leukocytosis |
|
|
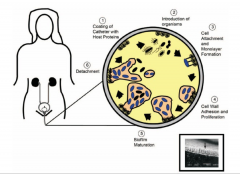
Summary photo of e. coli UTI pathogenesis:
|
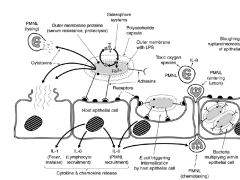
don't need to memorize
|
|
|
Summary photo 2 of e. coli UTI pathogenesis:
|
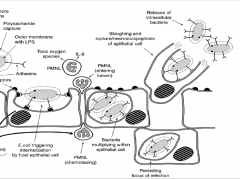
don't need to memorize
|
|
|
Discuss Proteus miravilis:
|
-Common cause of UTI in elderly women. It's a GNR.
-Has urease-->urea-->NH3-->kidney stones |
|

|

top: struvite stones
bottom: carbonate apatite stones *from Proteus mirabilis |
|
|
Urinary tract host defense mechanisms:
|
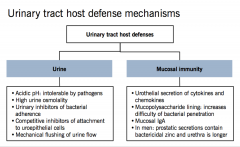
|
|
|
Risk factors for UTIs:
|
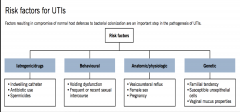
|
|
|
What's an uncomplicated UTI?
|
*UTI in an otherwise healthy, nonpregnant female.
*Always "complicated" in men. |
|
|
Examples of complicated UTIs:
|
-Diabetes
-Pregnancy -Previous acute pyelonephritis within previous year -Symptoms > 7 days prior to treatment -Multi-drug resistant uropathogen -Hospital-acquired infection -Renal failure -Urinary tract obstruction -Functional or anatomic urinary tract abnormality -Indwelling urinary catheter, stent, nephrostomy tube -History of UTI in childhood -Renal transplant -Immunosuppression |
|
|
Risk factors for UTI in kids:
diagnosis: treatment: |
*VUR is a risk factor for recurrent pyelonephritis and possible renal scarring. This can result in increased risk of hypertension and chronic kidney disease
*Diagnosis: voiding cystourethrogram. *VUR treatment: antibiotic prophylaxis and/or surgery. |
|
|
Severity grades of vesicoureteral reflux (VUR):
|
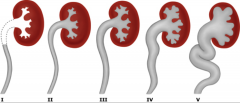
|
|
|
Special UTI considerations in pregnancy:
|
*Physiologic changes
-Increased renal size and glomerular filtration rate -Dilatation of ureters and renal pelvis R > L -Urinary stasis --> Risk of pyelonephritis -Flaccid bladder -Intermittent vesicoureteral reflux |
|
|
Asymptomatic bacteriuria in pregnancy:
screening: diagnosis: |
*2 – 7% of pregnancies
-40% risk of progressing to pyelonephritis -increased risk of preterm birth, low birth weight, and perinatal mortality -Must treat *Screening -at 12-16 weeks gestation *Diagnosis -2 voided specimens with ≥105 cfu/mL of same bacterial strain (in practice treatment is usually started after the first positive specimen, without waiting for second culture) -1 catheterized specimen with 102 cfu/mL |
|
|
Treatment of Asymptomatic bacteriuria in pregnancy:
|
*According to antibiotic susceptibility testing
*Antibiotics safe to use: Nitrofurantoin (Macrobid), Amoxicillin, Amoxicillin-clavulanate, Cephalexin Fosfomycin *Obtain follow-up cultures to document clearance *DO NOT USE in pregnancy: *Macrobid with G-6PD deficiency (hemolytic anemia) *Sulfonamides (Bactrim) last trimester (newborn hyperbilirubinemia) *Trimethoprim (Bactrim) first trimester (folic acid antagonist --> birth defects) *Fluoroquinolones (Ciprofloxacin, Levofloxacin) = chondrotoxicity |
|
|
Most common pathogens in acute cystitis:
symptoms: |
*Most common pathogens
-E coli -Other Enterobacteriaceae (Proteus, Klebsiella) -Staphylococcus saprophyticus *Symptoms -Dysuria -Frequency -Urgency -Suprapubic pain -Hematuria |
|
|
Diagnosis of acute cystitis:
|
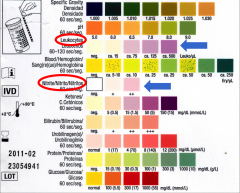
Dipstick urine analysis; look for:
*Leukocyte esterase -Released by leukocytes -Reflects pyuria *Nitrite -Reflects presence of Enterobacteriaceae, which convert urinary nitrate to nitrite -Does not rule out presence of gram-positive bacteria |
|
|
*Pyuria = ≥ 10 WBC/microL
*Examine an unspun (no centrifuge) voided midstream specimen. *Absence of pyuria strongly suggests another diagnosis besides UTI |
|
|
Treatment for acute cystitis:
|
*First line therapies for acute cystitis
-Nitrofurantoin (Macrobid) -Trimethoprim-sulfamethoxazole (Bactrim) -Fosfomycin (NOT to be used if pyelonephritis possible (they do not achieve good renal levels)) *Alternatives -Fluoroquinolones |
|
|
Clinical manifestations of acute pyelonephritis:
|
Symptoms of acute cystitis PLUS:
*FEVER, chills *Flank pain *Costovertebral angle tenderness *Nausea or vomiting *Sepsis and organ failure (rare) |
|
|
|
|
|
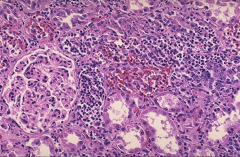
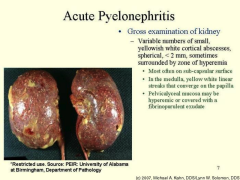
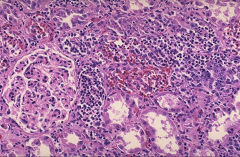
*Acute pyelonephritis
*Numerous PMNs are seen filling renal tubules across the center and right of this picture. These leukocytes may form into a cast within the tubule. Casts appearing in the urine originate in the distal renal tubules and collecting ducts. |
|
|
*WBC cast – diagnostic of upper UTI (pyelonephritis)
|
|

|

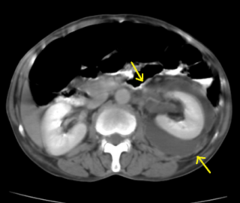
*Acute pyelonephritis. CT scan obtained with intravenous contrast material reveals patchy enhancement of the left kidney. The kidney is minimally enlarged with perinephric stranding, secondary findings that also suggest infection.
|
|
|
*Renal abscess: Fluid-filled collection in the left kidney, with septations and thick walls seen on a contrast-enhanced CT scan
*complication of pyelonephritis *can't be treated with meds alone |
|
|
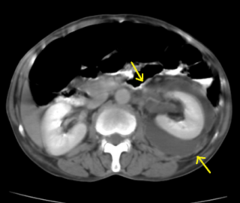
*Perinephric abscess on a CT scan - appears as a soft-tissue mass with a thick wall that may enhance after introduction of intravenous contrast material.
*complication of pyelonephritis *can't be treated with meds alone |
|

|

*Emphysematous pyelonephritis
*Presence of gas in the urinary tract tissue *Associated with diabetes and urinary tract obstruction *Severe cases may require percutaneous drainage or surgical debridement |
|
|
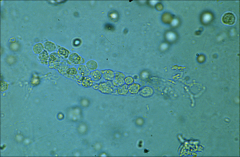
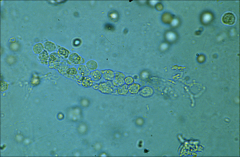
*Urine sediment showing multiple "coffin lid" magnesium ammonium phosphate crystals that form only in an alkaline urine (pH usually above 7.0) caused by an upper urinary tract infection with a urease producing bacteria. Struvite STONES.
|
|
|
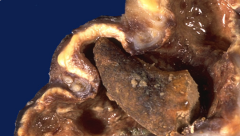
*"Staghorn calculus". Seen here is a horn-like stone extending into a dilated calyx, with nearly unrecognizable overlying renal cortex from severe hydronephrosis and pyelonephritis.
*Nephrectomy may be performed because the kidney is non-functional and serves only as a source for infection. *Extreme struvite stones due to UTI. |
|
|
Treatment of uncomplicated and complicated pyelonephritis:
|
*Uncomplicated pyelonephritis
-Outpatient -Fluoroquinolones *Complicated or severe pyelonephritis -Hospitalize -IV Ceftriaxone or aminoglycosides -If risk of antibiotic-resistant infection, may need broad-spectrum beta-lactam antibiotics -Tailor antibiotic therapy to susceptibility results of urine and/or blood cultures -Urology consultation to address underlying urinary obstruction or neurogenic bladder |
|
|
Describe nosocomial UTIs:
|
*Number one cause of hospital acquired infections.
*Due almost exclusively to indwelling urethral (Foley) catheters *Inevitably infected if use prolonged *Now considered “non-reimbursable” by Medicare. |
|
|
Prevention and treatment of nosocomial UTIs:
|
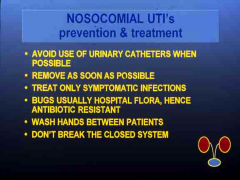
|
|
|
How to obtain a correct specimen for urine analysis:
|
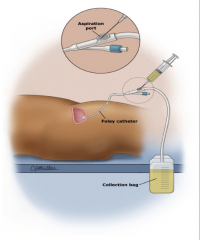
*Put a new catheter in
*Old cath will have bacteria in it for sure. *Don't take specimen from the bag. |
|
|
Discuss biofilms on catheters:
|
*Can't kill bugs on a device
*Have to replace the device! |
|
|
Catheter awareness?
|
*Providers were unaware of the catheter 28% of the time
*Unawareness rates: 21% students, 22% interns, 27% residents, *38% attendings *Providers were more likely to be unaware of the catheter when there was no appropriate indication for use. |
|
|
-Define recurrent UTI:
-Risk factors in young women -Risk factors in post-menopausal -Management? |
≥ 2 infections in 6 months, or ≥ 3 infections per year
*In young women -Risk factors: sexual intercourse, spermicide use, and greater propensity to colonization with uropathogens (genetic) *In post-menopausal women -Risk factors: decreased bladder emptying (urinary incontinence, presence of cystocele, increased post-voidal residual urine) *Antimicrobial prophylaxis highly effective -Continuous, post-coital, or intermittent self-treatment -Bactrim or fluoroquinolone |
|
|
Chronic bacterial prostatitis:
-when do you suspect it? |
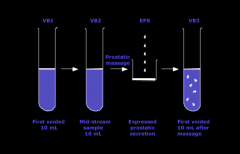
*Repeated UTIs with isolation of the same organism from the urine
*Some men may be asymptomatic with only persistent bacteriuria *Diagnosis ideally should reflect the same organism recovered from urine and prostatic secretions (“the four glass test”; historic only) *Treatment: fluoroquinolones for at least 6 weeks if the organism is susceptible; TMP-SMX as alternative |
|
|
What is Sterile Pyuria?
|
*When sexually active patients present with dysuria and pyuria, but no growth on urine cultures.
Suspect/Exclude: *Vaginitis *Chlamydia infections *Herpes simplex infections |
|
|
How do you diagnose a UTI?
|
-Have to have SYMPTOMS first.
-Then, urine analysis to confirm infection. |

