![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
81 Cards in this Set
- Front
- Back
|
Describe the embryonic structures required for development of the kidney (general).
|
True kidneys form from METAnephros, which develops caudally from ureteric bud and metanephric mesoderm.
Ureteric bud gives rise to collecting system: CDs, minor calyces, major calyces, renal pelvis, ureters Metanephric mesoderm gives rise to glomerulus, Bowman's space, PROXIMAL tubule, LOH, DISTAL TUBULE, COLLECTING TUBULE (Distal Collecting Tubule ≠ Collecting Duct) |
|
|
How does glycosylation result in vascular damage (in diabetes)?
|
Glycosylation products accumulate and cross-link w/collaggen-->facilitates inflammatory cell invasion and deposition of LDL in vascular walls-->atherosclerosis
|
|
|
What structures don't require insulin for glucose transport?
Why is this dangerous in diabetes? |
Lens, peripheral nerves, BVs, kidneys
Hyperglycemia results in inc'd intracell glucose [ ]; glucose converts into sorbitol via ALDOSE REDUCTASE, sorbitol converted into fructose (POLYOL PW) Sorbitol and fructose increase osmotic pressure and stimulate influx of water leading to osmotic cell injury. Inc'd water in lens-->opacification of lens and cataract formation Osmotic injury of Schwann cells-->peripheral neuropathy in DM |
|
|
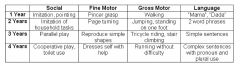
Describe the following milestones for children at 1, 2, 3, and 4 years of age:
Social Fine Motor Gross Motor Language |
|
|
|
Ertyhroblastosis fetalis:
Antibodies involved Hypersensitivity Type |
IgG
Type II (antibody mediated) |
|
|
Infant born with Hgb 6 g/dL
Nucleated erythrocytes Hepatomegaly Generalized edema Extramedullary hematopoiesis Diagnosis |
Erythroblastosis fetalis
|
|
|
Describe how enothelial intimal cells respond to injury.
|
Medial smooth muscle cells migrate across lamina and into intima
Smooth muscle cells proliferate and produce collagen (produces a neointima) Injured endothelial cells can release GFs that promote SMC migration and proliferation, such as PDGF or they can express vascular cell-adhesion molecules (VCAMs) that allow adherence of monocytes/lymphocytes. These WBCs then release cytokines and GFs to promote SMC migration encouraging fibrogenesis. In short, this process is mediated (predominantly) by reactive smooth muscle cells. |
|
|
Infant expresses shrill crying
Tremor, rhinorrhea Sneezing, diarrhea Followed by myoclonic jerks that progress to seizures Diagnosis Treatment |
Acute opioid withdrawal; tx w/tincture of opium
|
|
|
Signs of digoxin toxicity
|
Disturbed color perception
ARRHYTHMIAS due to HYPERKALEMIA also n/v/ano |
|
|
Familial hypercholesterolemia:
Mode of inheritance |
AD
|
|
|
After ingestion of nitrates, chromosomal DNA undergoes accelerated cytosine deamination.
Provide the steps by which this is repaired. |
(Cytosine deamination creates unusual base uracil)
GLYCOSYLASE cleaves altered base leaving an AP site (Apurination or Apyrimidination) ENDONUCLEASE cleaves 5' end, LYASE cleaves 3' sugar phosphate DNA POLYMERASE and LIGASE fill the single nucleotide |
|
|
Cause of acute bacterial arthritis in sexually active young adults.
|
N. gonorrhoeae
(S. aureus septic arthritis common in children and non-sexually active adults) |
|
|
23 year-old female
Complains of restless legs Inability to lie still Diagnosed with schizophrenia A&O x 3 Diagnosis Treatment |
Akathisia--a well-known complication of neuroleptic therapy.
Patients can develop restless leg syndrome or feel "on edge". Tx: decrease dose of neuroleptic or add antiparkinsonian agents |
|
|
Describe the algorithm for coagulase negative staph.
|
Novobiocin sensitive:
S. epidermidis (prosthetic valve endocarditis, catheter related infections, prosthetic joint septic arthritis) Novobiocin RESISTANT: S. saprophyticus (UTIs in sexually active young women) |
|
|
54 year-old male
Recurrent abdominal pain Chronic diarrhea, recent weight loss Consumes alcohol regularly X-ray reveals calcifications in epigastric area Diagnosis |
Chronic alcoholic pancreatitis resulting in pancreatic exocrine insufficiency and malabsorption
|
|
|
Varicose veins:
Pathophys Complications |
Prolonged increases in intraluminal pressure and loss of vessel wall tensile strength
Incompetent enous valves, venous stasis/congestion, edema, and an increased incidence of SUPERFICIAL VENOUS THROMBOSIS. No risk of pulmonary embolus. Venous stasis ulcers very common! |
|
|
What specific cholinergic receptor acts on bronchial smooth muscle?
|
M3
|
|
|
Nonbacterial thrombotic endocarditis:
Pathophys |
Usually bland thrombus w/o accompanying inflammation or valvular damage.
Result of a hypercoagulable state, such as cancer. Similar mechanism: tumor-associated release of procoagulants is thought responsible for migratory thrombophlebitis (Trousseau syndrome) seen in pts w/visceral cancers. |
|
|
Holoprosencephaly:
Definition Predisposing conditions |
Incomplete division of forebrain into two hemispheres--an example of malformation
a/w Trisomy 13, Trisomy 18, Fetal Alcohol Syndrome |
|
|
Amniotic band syndrome is an example of a __________.
|
Disruption (secondary destruction of a previously well-formed tissue or organ)
|
|
|
Congenital hip dislocation, clubbed feet, and flat facies are examples of __________.
|
Deformations (secondary to extrinsic compression)
|
|
|
What is a sequence (developmental definition)?
Give an example. |
When a number of abnlts result from primary defect. Example oligohydramnios sequence (Potter syndrome):
Low volume of amniotic fluid causes fetal compression by uterus, resulting in flattened facies, abnl limbs and hypoplastic lungs |
|
|
Von Hippel-Lindau:
Mode of Inheritance Characteristics |
AD
Capillary hemangioblastomas in retina, cerebellum Congenital cysts/neoplasms in kidney, liver, pancreas Inc'd risk RCC |
|
|
Sturge-Weber Syndrome:
Characteristics |
Cutaneous facial angiomas
Leptomeningeal angiomas MR TRAM TRACK calcifications of skull Seizures, hemiplegia |
|
|
Tuberous Sclerosis:
Characteristics |
Kidney, liver, pancreatic cysts
Cortical and subependymal HAMARTOMAS Seizures |
|
|
Osler-Weber-Rendu:
Mode of Inheritance Characteristics |
AD
Telangiectasias in skin and mucus membranes of lips, nasopharynx, resp tract, GI, urinary tracts Rupture leads to epistaxis, GI bleeds, hematuria |
|
|
What cranial nerves are associated with the pharyngeal/aortic arches?
|
1: CN V (Trigeminal)
2: CN VII ( Facial) 3: CN IX (Glossopharyngeal) 4: Superior laryngeal branch of Vagus (CN X) 6: Recurrent Laryngeal branch of Vagus (CN X) |
|
|
What cell interactions are required for adhesion of cells to the basement membrane and extracellular matrix?
|
Binding of integrins to fibronectin, collagen, and laminin
|
|
|
What is the role of hyaluronic acid?
|
Contributes to water retention in ECM, endowing matrix w/lubricant properties and viscous, gel-like consistencey
|
|
|
24 year-old male
Paroxysmal breathlessness and wheezing No known triggers No history of recent illness Sputum shows granule-containing cells and crystalloid masses Diagnosis Explain findings Key cytokine |
Paroxysmal breathlessness and wheezing in a young pt unrelated to ASA, pulmonary infection, stress, exercise-->EXTRINSIC ALLERGY ASTHMA
Granule-containing cells in sputum likely eosinophils and crystalloid bodies likely Charcot-Leyden crystals (contain ephil membrane protein) This is all due largely in response to IL-5 released by Th2 cells |
|
|
Where in the nephron does ADH bind?
|
Collecting ducts
|
|
|
6 month-old male
Diffuse skin erythema Epidermis comes off easily with gentle pressure Diagnosis Pathophys |
Staphylococcal Scalded Skin Syndrome
Due to production of exotoxin exfoliatin |
|
|
78 year-old male
BP 180/70 HR 75 bpm Diagnosis Pathophys |
Isolated systolic hypertension caused by age-related decreases in AORTIC COMPLIANCE
Note: diastolic pressure is in normal range |
|
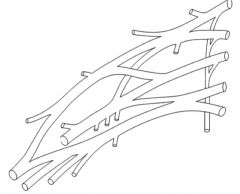
Label
|
|
|
|
What drugs require a cheese/wine dietary restriction?
|
MAOI
|
|
|
What are the first-line treatment for depression?
|
SSRIs, bupropion is an alternative
|
|
|
Which anti-depressant causes sexual dysfunction?
|
SSRIs
|
|
|
Phenelzine:
MOA |
MAOI
|
|
|
Imipramine:
MOA |
TCA; NOT FIRST LINE FOR DEPRESSION
|
|
|
Which anti-depressant causes sedation and priapism?
|
Trazodone
|
|
|
Tranylcypromine:
MOA |
MAOI
|
|
|
Bupropion:
MOA |
Anti-depressant that acts on NE transmission, but doesn't influence 5HT, ACh, or histamine metabolism.
BEWARE OF SEIZURES |
|
|
55 year-old male
Treated for high cholesterol unresponsive to dietary changes Complains of decreased appetite and malaise What test should you order? |
LFTs; not serum creatinine and BUN!!
|
|
|
Cor pulmonale:
Definition Causes |
RVH secondary to pulmonary HTN
Can result from dz of lung parenchyma or pulmonary vasculature In young female, primary pulmonary HTN may be responsible |
|
|
56 year-old male
Smoker Recurrent hemoptysis Facial swelling, conjunctival edema, dilated vessels of neck, upper trunk Heart sounds clear Diagnosis Pathophys |
Superior vena cava syndrome secondary to BRONCHOGENIC carcinoma
i.e., cancer is compressing superior vena cava resulting in dyspnea, cough, swelling of face/neck/upper extremities |
|
|
How does a Pancoast tumor differ in presentation from a Bronchogenic carcinoma?
|
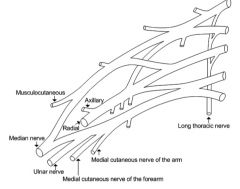
Pancoast tumor arises at lung APEX and may cause shoulder pain due to compression of brachial plexus. Compression of cervival sympathetic ganglia can lead to Horner's syndrome (ptosis, miosis, anhydrosis)
Bronchogenic carcinoma can result in SVC syndrome (facial swelling, head/neck/upper extremities too) |
|
|
What would be the effect of a mutation to 5-PRPP synthetase gene resulting in an increased Vmax?
|
Increased production of purines-->increased degradation-->increased uric acid-->hyperuricemia-->gout
|
|
|
Colchicine:
MOA |
Inhibits chemotaxis of NEUTROPHILS (not eosinophils!) by preventing microtubule formation.
|
|
|
What are the specific (molecular) effects of folate deficiency?
What can be supplemented (besides folate)? |
Dec'd folic acid mean:
-Inhibited formation of dTMP, which limnits DNA synthesis and promotes megaloblastosis and erythroid precursor apoptosis -Thymidine supplementation can moderately increase dTMP levels and reduce erythroid precursor apoptosis |
|
|
32 year-old male
Weakness, tingling that started in feet, but not is in knees 2/5 strength in both legs Absent DTRs in knees Mild respiratory infection two weeks ago Diagnosis Specific Pathophys Histologic findings |
Guillain-Barre Syndrome
Strongly associated with Campylobacter jejuni infection GBS is an acute demyelinating dz; Abs x infectious agents cross-react w/myelin of spinal roots and peripheral nerves. Light microscopy will show endoneural inflammatory infiltrate consisting of lymphocytes and macs |
|
|
Describe the molecular effects of Shiga toxin.
How does they differ from the effects of diphtheria toxin? |
Inhibit 60S ribosomal subunit in human cells thereby blocking protein synthesis by preventing binding of tRNA.
Diphtheria toxin (and exotoxin A of Pseudomonas) act on EF-2, not 60S ribosomal subunit. |
|
|
Why are patients with Down syndrome more likely to develop Alzheimer's?
|
Chromosome 21 contains APP gene (amyloid precursor protein).
Cleavage of APP forms A beta-amyloid, which accumulates in brain tissue and vessel walls. Trisomy 21 entails that three copies of APP gene are present. Note: you'd see neurofibrillary tangles!! |
|

|
Protons dissociate from amino acids when pH exceeds pKA associated w/each proton.
Physiologic pH = 7.4 So at this pH, lysine will have two positively charged amine groups (NH3+--these are protonated bc pH<pKA) and one negatively charged carboxyl group (COO-). Giving us a net charge of +1 at physiologic pH. |
|
|
Describe the histologic changes seen in the first 24 hours after MI.
|
0-4 hours: no change (normal myocardium)
4-12 hours: early COAGULATION necrosis, edema, hemorrhage, wavy fibers 12-24 hours: coagulation necrosis, marginal contraction band necrosis |
|
|
Describe the histologic changes seen in the first 24 hours after MI.
|
0-4 hours: no change (normal myocardium)
4-12 hours: early COAGULATION necrosis, edema, hemorrhage, wavy fibers 12-24 hours: coagulation necrosis, marginal contraction band necrosis |
|
|
What is the best long-term treatment choices for chronic tophaceous gout?
MOA? |
Allopurinol (xanthine oxidase inhibitors)
Probenecid or sulfinpyrazone (Uricosuric drugs) These drugs will reduce the uric acid by allowing for its excretion. |
|
|
61 year-old male
Hyperuricemia after arthritis h/o recurrent renal colic Treatment MOA |
Xanthine oxidase inhibitor (allopurinol)
Don't want to use a uricosuric agent bc this might precipitate renal uric stone (uric acid nephrolithiasis) |
|
|
Unfractionated vs LMW Heparin:
MOA |
Unfractionated heparin can bind antithrombin to increase its activity against factor Xa (as can LMWH), but only unfractionated heparin can bind to both antithrombin and THROMBIN to allow antithrombin to inactivate thrombin.
In short, LMWH has greater activity against Factor Xa than thrombin. Unfractionated heparin would be better for acute coronary syndrome. |
|
|
Which anti-viral binds both viral DNA polymerase and viral reverse transcriptase, and does not require intracellular activation?
|
Foscarnet
|
|
|
MEN2A vs MEN2B
|
MEN2A: parathyroid hyperplasia
MEN2B: medullary ca of thyroid, pheo, oral/intestinal mucosal neuromas MARFANOID HABITUS |
|
|
D-Ala-D-Ala
|
Penicillins
|
|
|
What is the exact mechanism by which penicillin works?
|
Inhibit transpeptidase, enzyme that catalyzes final crosslinking step in peptidoglycan cell wall formation (joints amino acid of one peptidoglycan to terminal D-Alanine-D-Alanine of another peptidoglycan molecule)
PCNs are structural analogs of D-Ala-D-Ala |
|
|
Describe the specific pathologic findings of:
Hyperacute rejeciton Acute rejection Chronic rejection |
Hyperacute: preformed anti-donor antibodies immediately cause vascular fibrinoid necrosis, infarction of graft
Acute rejection causes interstitial mononuclear infiltrate and/or graft vasculitis Chronic rejection results in obliterative intimal smooth muscle hypertrophy and fibrosis of cortical arteries |
|
|
What is the treatment for acute mania?
|
Mood stabilizing agent (lithium, valproate, carbamazepine) plus an atypical antipsychotic (olanzapine)
|
|
|
How is gut iron absorption regulated?
|
Through effect of hepcidin (made in liver)
Inc'd iron levels or inflammatory conditions cause an increase hepatic synthesis of hepcidin, which through its interaction with ferroportin decreases intestinal absorption of iron and decreases release of iron by macrophages. |
|
|
Describe the path iron takes from the gut into the blood.
List all receptors and transporters. |
DMT-1 transports Fe2+ into gut
Ferritin binds intracellularly Ferroportin brings it to brings iron into blood where transferrin picks it up. |
|

|
Protons dissociate from amino acids when pH exceeds pKA associated w/each proton.
Physiologic pH = 7.4 So at this pH, lysine will have two positively charged amine groups (NH3+--these are protonated bc pH<pKA) and one negatively charged carboxyl group (COO-). Giving us a net charge of +1 at physiologic pH. |
|
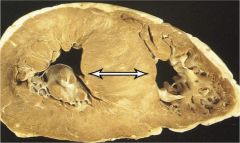
Diagnosis
Type of murmur heard What would exacerbate murmur? |
Asymmetric hypertrophy of interventricular septum-->hypertrophic cardiomyopathy (HCM)
Leads to SYSTOLIC EJECTION MURMUR Obstruction augmented when there are decreases in LV end diastolic volume. Thus, maneuvers that enhance the obstruction by decreasing venous return (sudden standing, Valsalva) increase the murmur of HCM. |
|
|
What are the three MRI findings strongly suggestive of craniopharyngioma?
|
Cystic
Filled with "machinery oil" or liquid Calcification |
|
|
LV hypertrophy vs dilation:
When does each occur? |
LV hypertrophy: longstanding HTN because of inc'd LV afterload (PRESSURE overload)
LV dilation: volume overload as in mitral regurgitation. May also be seen in dilated cardiomyopathy and after MI. |
|
|
Which region of a transplanted lung is affected in chronic rejection?
|
Small airways, i.e., small bronchioli--produces obstructive lung dz known as bronchiolitis obliterans.
Ultimately there is occlusion of hte bronchiolar lumen. |
|
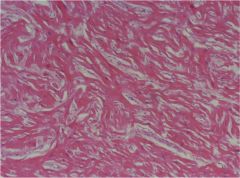
Diagnosis
Gene mutation |
Haphazardly arranged myocytes and myocyte bundles-->hypertrophic CM
Approximately 50% of which are familial; gene mutation to cardiac sarcomere proteins (beta-myosin heavy chain) |
|
|
21 year-old male
Chronic headaches, ataxia Low-lying cerebellar tonsils extending into vertebral canal Diagnosis |
Arnold-Chiari MALFORMATION
|
|
|
Arnold-Chiari Malformation I vs II
|
AC Malformation I: Low-lying cerebellar tonsils extend below foramen magnum into vertebtral canal; manifests in adulthood w/HA and ataxia
Type II is symptomatic in neonatal period; Both cerebellar vermis and medulla extend downward through foramen magnum Presents with difficulty swallowing, dysphonia, stridor, apnea |
|
|
A confidence interval that includes ____ is not statistically significant.
Why? |
1.0
CI is related to relative risk; if Risk of exposure group is equal to risk of control group, then there is no difference between the groups and the results are are not statistically significant. |
|
|
Equation for relative risk.
|
Incidence in experimental group/Incidence in control group
|
|
|
How does hyperglycemia result in neuropathy (2 ways)?
|
1) Non-enzymatic glycosylation of proteins that lead to increased thickness, hyalinization, and narrowing of arterial walls. Leads to microangiopathy of endoneural arterioles. Ischemic nerve damage follows.
2. Intracellular hyperglycemia occurs in peripheral nerves. Accumulating glucose is converted into sorbitol and fructose by ALDOSE REDUCTASE. Sorbitol increases cell osmolarity and facilitates water influx into cell. Result is osmotic damage to axons and Schwann cells. |
|
|
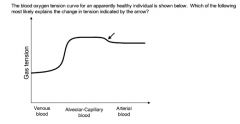
Graph illustrates the pO2 of blood as it moves from the venous system through the lungs and into the systemic circulation.
The arrow points to the admixture of deoxygenated bronchial blood w/oxygenated blood in the pulmonary veins. (First plateau represents blood moving through pulmonary capillaries and becoming progressively more oxygenated until it equilibrates with alveolar pO2) |
|
|
Describe bronchial circulation.
|
L/R bronchial arteries arise from descending thoracic aorta
Together with pulmonary artery, form dual blood supply to lungs Bronchial veins return some of bronchial blood to right heart via azygous, however, MAJORITY OF BLOOD from bronchial arteries is returned to left heart in deoxygenated form via pulmonary veins. |
|
|
17 year-old female
Dark urine, facial puffiness Minor skin infection several weeks ago Microhematuria Diagnosis Specific organism |
Acute Post-Streptococcal Glomerulonephritis due to Group A Strep (S. pyogenes)
|
|
|
Provide the complete Gram positive, catalase negative algorithm.
|
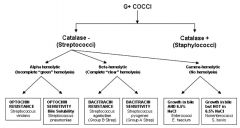
|

