![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
43 Cards in this Set
- Front
- Back
|
What is Hypovolemia?
|
*Loss of intravascular volume:
-Mild (less than 15% volume loss): 1) Compensatory mechanisms to maintain organ perfusion. 2) Attempt to increase intravascular volume. -Severe (greater than 15% volume loss) 1) Compensatory mechanisms become inadequate. 2) Hypoperfusion of vital organs. 3) End-organ damage. |
|
|
What are the Major causes of hypovolemia?
|
*Blood loss:
-Hemorrhage. -Surgery. *Plasma Loss: 1) Renal losses of Na and water. -Osmotic diuresis (e.g. glucosuria in uncontrolled DM). -Diuretics. -Aldosterone deficiency (primary adrenal insufficiency). 2) Extrarenal losses of Na and water: -GI losses: from vomiting/diarrhea. -Skin losses: sweating, weeping from burns. -Sequestration into interstitial space (“third spacing”): crushed limb or intestinal obstruction (pancreatitis). |
|
|
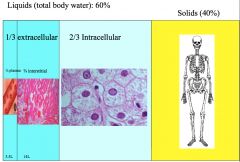
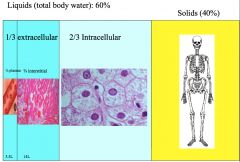
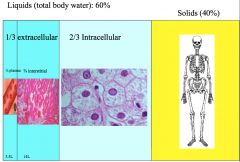
Can plasma loss result from simply dehydration?
|
*Water freely distributed through all liquid compartments.
*“Water follows salt.” *Isolated water losses will cause a shift of water out of cells to (mostly) restore plasma volume. *VOLUME DEPLETION is a result of loss of circulating volume (in the form of blood, plasma, or NaCl). |
|
|
What's the major electrolyte involved in maintaining circulating volume?
|
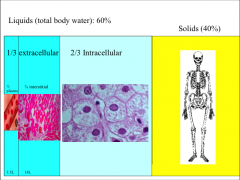
*Blood loss is an obvious source of hypovolemia.
*NaCl are the predominant extracellular electrolytes. *A loss of sodium will lead to a loss of circulating volume. |
|
|
What is the pathogenesis of volume depletion?
|
1) Blood Losses.
2) Extrarenal losses (skin, GI, etc.). 3) Renal Losses: *Osmotic: -Osmotic effect of glucosuria in uncontrolled diabetes mellitus impairs reabsorption of Na and water. *Diuretics: Blocked Na reabsorption leads to Na and water losses in urine. *Adrenal insufficiency: Aldosterone deficiency decreases reabsorption in distal tubule (leading to excess renal losses of Na and water). |
|
|
What are the Clinical features of volume depletion?
Characteristics of the history and PE. |
1) History:
-Blood loss. -Excess GI losses. -Excess urinary losses (polyuria, nocturia). 2) Physical Exam: -Tachycardia. -Hypotension. -Orthostatic hypotension. -Dry mucous membranes. -Reduced skin turgor. |
|
|
How does the body respond to hypovolemia?
|
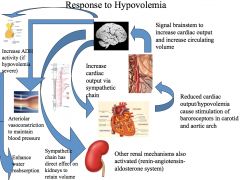
*Maintain perfusion:
-Increase heart rate -Arteriolar vasoconstriction to maintain BP *Conserve intravascular volume: -Reduce filtration by kidneys -Retain Na in kidneys -Retain water in kidneys |
|
|
What are the body's Mechanisms for volume retention?
|
*Decreased loss of sodium from reduced renal perfusion (reduced GFR).
*Increased sympathetic tone to kidneys enhances sodium retention. *Increased activity of renin-angiotensin-aldosterone system enhances sodium retention. *Increased ADH activity leads to more reabsorption of water, reduced urine output. *Decrease in Atrial Natriuretic Peptide activity. |
|
|
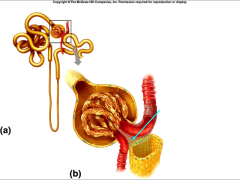
Discuss the change in GFR with volume depletion:
|

*Normal GFR is 100-120ml/min.
*Leads to a filtered load of 170L per day! *Reduction in GFR will decrease the filtered load. *GFR reduced by lower cardiac output, low BP. *This is not too major of a mechanism for volume retention! |
|
|
What are the body's mechanisms to enhance Na reabsorption in the volume depleted state?
|
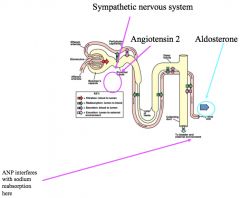
*Enhances sodium reabsorption by minimizing and nearly eliminating urinary Na losses.
*Proximal Tubule Na reabsorption: -Sympathetic nervous system -Angiotensin 2 *Distal: -Aldosterone -Loss of ANP |
|
|
How does the JGA know when there's not enough Na in the tubular fluid?
|
-Macula densa senses amount of NaCl delivered to the distal nephron.
-In response to reduced NaCl delivery (hypovolemia): Increases production of renin--> angiotensin--> aldosterone. |
|
|
Discuss the effect of ADH in a state of volume depletion:
|
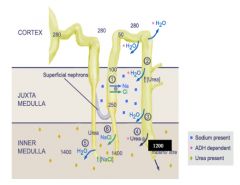
*Hypovolemia is a potent stimulus of ADH (anti-diuretic hormone).
*Elevated ADH levels open water channels in the collecting duct, leading to reabsorption of more water and reduced urine output. |
|
|
What is the role of ANP in volume depletion?
|
*ANP is released in response to stretching of the atria (volume overload).
*Presence of ANP leads to loss of sodium. *Absence of ANP leads to sodium retention. *2 major effects: 1) Vasodilation (of afferent arteriole) -Also causes mild efferent vasoconstriction. 2) Interference with sodium reabsorption -Inhibits sodium channels in medullary portion of tubule. -Suppresses renin and aldosterone release. |
|
|
How do we treat hypovolemia?
|
*The goal should be to restore circulating volume to prevent organ damage:
-Treat cause of volume loss (if possible). -Estimate volume deficit and replace. -Estimate ongoing losses and replace these as well. *The choice of resuscitation fluids will have an impact on their efficacy -E.g. a patient with severe traumatic blood loss will need blood to restore circulating volume. |
|
In hypovolemia, what's the effect of adding pure blood?
|
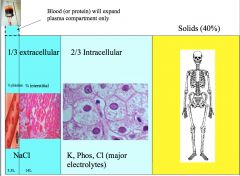
|
|
In hypovolemia, what's the effect of adding isotonic saline?
|
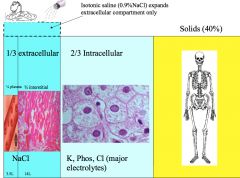
|
|
In hypovolemia, what's the effect of adding salty food?
|
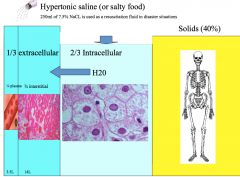
*OR hypertonic saline; this would be only a temporary fix in an emergency situation! Like a disaster situation where you have to treat many people with few supplies.
|
|
|
What is:
-D5W -D5 1/2 NS -NS -LR |
*D5W: 5% dextrose, 0 sodium; osm 0meq/L
*D5 ½ NS: 5% dextrose, 0.45% NaCl: Na 77meq/L Cl 77meq/L; osm = 154meq/L *NS: 0.9% NaCL: Na 154meq/L, Cl 154meq/L; osm = 308meq/L *Lactated Ringers: Na 131meq/L, Cl 109meq/L, K 4meq/L, Lactate 28meq/L, Ca 2.7meq/L (about 10.8mg/dL); osm = 273meq/L |
|
|
Osmolality of various HOME fluids:
|
*Gatorade:
-5% Dextrose; Na 18meq/L, K 3meq/L; osm 42meq/L. *Campbell’s Chicken Noodle Soup: -Na 109meq/L; osm = 218meq/L. Actually a pretty good resuscitation fluid. *V8: -Na 103 meq/L, K 48 meq/L Ca 4 meq/L; osm = 310meq/L. Actually a great resuscitation fluid. *Dirty Martini with 3 olives: -A 6 oz dirty martini with 3 olives will contain 800mg Na. -Na 191meq/L; osm = 382meq/L. |
|
|
What is hypervolemia?
|
*State of excess intravascular volume.
*Frequently accompanied by excess extracellular volume. *Usually caused by impaired renal excretion of sodium. |
|
|
Main causes of hypervolemia:
|
1) Decreased renal Na excretion:
-Heart failure. -Renal failure. -Hyperaldosteronism (adrenal adenoma). 2) Massive Na intake. 3) Increased production of RBCs (polycythemia); much less common than 1 and 2 above. |
|
|
What is the body's response cascade to volume overload?
|
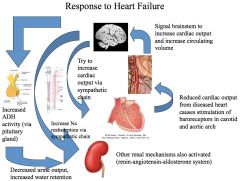
|
|
|
Pathogenesis of HF in a volume overload state:
|
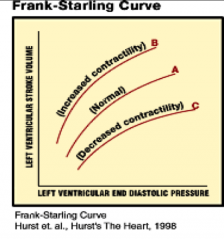
*The same mechanisms that help to compensate for hypovolemia are also involved in heart failure.
*Sympathetic stimulation of a diseased heart does not result in much improvement in cardiac output. *Increasing intravascular volume only results in a small (and inadequate) increase in cardiac output. |
|
|
What's the Renal response to heart failure?
|
1) Decreased GFR from low cardiac output:
-Reduced sodium excretion 2) Decreased NaCl delivery to the distal nephron: -Stimulation of juxtaglomerular apparatus. -Increased production of renin/angiotensin/aldosterone: a. Angiotensin--> proximal Na absorption. b. Aldosterone--> distal Na absorption. 3) Increased sympathetic nervous system activity: -Increased proximal Na absorption. -Increased renin/angiotensin/aldosterone activity. 4) Increased ADH activity: -Increased water reabsorption. -Decreased urine output. |
|
|
How would you get rid of Na and water if your kidneys didn't work at all?
|

*These are patients with impaired kidney function.
*Extreme example: Consider GFR of zero: -Only mechanism for excretion of salt and water are via GI tract and insensible losses. -Inability to handle daily ingestion of fluids and salt. *More commonly, problems with volume overload occur when GFR falls below 10-20. *When GFR falls, kidney compensates by reabsorbing less of filtered sodium load to prevent volume overload. *Limited reserve capacity to handle excess salt/volume. *Prone to developing hypervolemia. |
|
|
Compare filtration and reabsorption traits of normal and diseased kidneys:
|

*Healthy kidney: GFR 100-120ml/min
-Filters 140L per day ->99% Sodium reabsorbed *Diseased kidney: GFR 10-12ml/min -Filters 14L /day -92% Sodium reabsorbed *This 92% is about as low as we can get. |
|
|
Discuss the effects of hyperaldosteronism:
|
*Adrenal adenoma!
*Can produce excess aldosterone (independent of renin/angiotensin system). *Stimulates sodium reabsorption in distal nephron. *Severity of hypervolemia usually limited as other mechanisms of Na regulation are still intact (“Escape phenomenon”): -Increased GFR increases sodium filtration and excretion. -Decreased sympathetic activity and renin-angiotensin activity lead to decreased proximal sodium reabsorption. *Tends not to be as severe as renal failure or HF in causing edema: it may cause peripheral edema, but not pulmonary. |
|
|
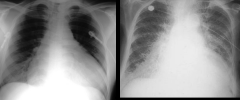
Clinical features of hypervolemia:
|
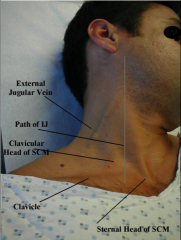
1) Circulatory:
-Increased arterial filling. -Increased blood pressure. -Venous distension: JVD, Hepatomegaly. 2) Cardiac: -Cardiomegaly. -Pulmonary edema (rales on exam). -S3 gallop rhythm. -Tachycardia. 3) Peripheral: -Edema formation (dependent areas of body). -Anasarca (generalized edema). -Ascites (abdominal fluid). |
|
|
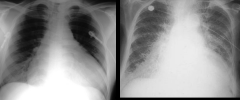
Left: cardiomegaly
Right: pulmonary edema |
|
|
What are the symptoms of volume overload?
|
*Cardiac
-Angina pectoris -Palpitations *Pulmonary -Orthopnea (shortness of breath when lying flat) -Dyspnea on exertion *Peripheral -Ankle swelling -More generalized swelling -Weight gain |
|
|
What do you look for in diagnosing volume overload?
|
*Exam findings of hypervolemia:
-Cardiac: *Murmurs *S3 gallop *Jugular venous distension *Hypertension -Pulmonary: *Rales -Peripheral: *Edema *Anasarca -Heart failure: *History/physical findings (JVD, rales, S3 gallop, etc.) *Swan-ganz catheter -Renal failure: *Elevated serum creatinine (usually > 4-5mg/dL) -Hyperaldosteronism: *Accompanied by metabolic alkalosis and hypokalemia *High plasma aldosterone levels |
|
|
What's the treatment for hypervolemia?
|
*Non-specific treatments:
1) Dietary sodium restriction 2) Diuretics to increase sodium excretion *Disease-specific treatments: 1) Heart failure: -Improve cardiac function with medications (digitalis, inotropes) -Surgery to correct faulty valves or improve function 2) Renal failure: Treat to improve renal function. 3) Hyperaldosteronism: Surgery to remove adenoma. |
|
|
What is the etiology of edematous states?
|
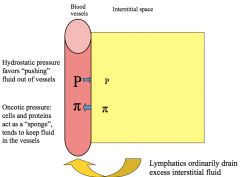
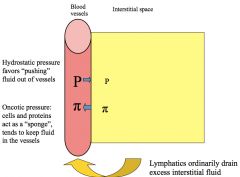
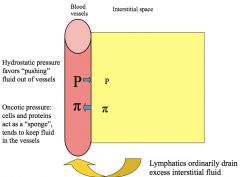
*Increased capillary hydrostatic pressure:
1) Hypervolemia -Massive intake of Na -Reduced excretion of Na (renal failure, heart failure) 2) Venous obstruction or stasis *Decreased plasma oncotic pressure (hypoalbuminemia): 1) Reduced albumin synthesis (liver disease, malnutrition) 2) Urinary protein loss (nephrotic syndrome) *Increased capillary permeability: 1) Inflammation 2) Trauma *Lymphatic obstruction |
|
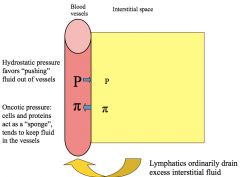
What happens if you have increased hydrostatic pressure in the vessels?
In what states could this occur? |
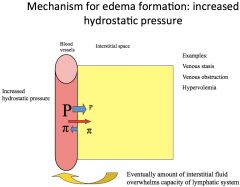
*Massive Na intake, DVT.
*Overwhelmed lymphatics--> edema. |
|
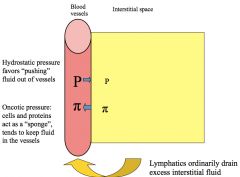
What happens if you have low oncotic pressure in the vessels?
In what states could this occur? |
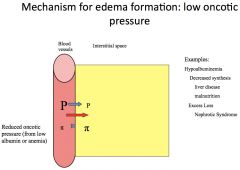
|
|
What happens if you have increased capillary permeability?
In what states could this occur? |
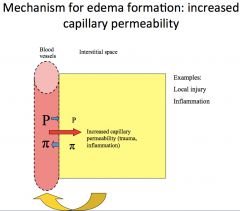
*Ex: getting punched in the eye; swollen eye.
|
|
What happens if you have lymphatic obstruction?
In what states could this occur? |
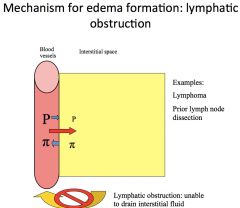
*Normal role of lymphatics is to drain excess fluid. This is why patient with mastectomy + axillary node removal can't have BP taken on that arm.
|
|
What happens in pulmonary edema?
|
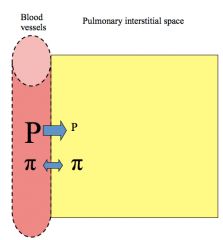
*Pulmonary capillaries are more permeable to albumin.
*Presence of pulmonary edema is more reflective of intravascular volume. *Pulmonary edema tends not to occur in edematous states that are due to hypo-albuminemia. *THIS IS DUE TO SODIUM OVERLOAD. Wouldn't see this in liver disease. |
|
|
What's the role of the kidneys in edema formation?
|
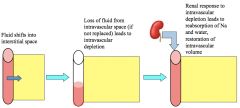
|
|
|
What are the Clinical features of edema?
peripheral and pulmonary? |
*Peripheral edema:
1) Pitting edema enables this to be distinguished from subcutaneous fat. 2) Tends to occur in dependent areas; lower extremities during day while sitting/standing. 3) In cases of venous obstruction, occurs distal to site of blockage. *Pulmonary edema: 1) Dyspnea. 2) Orthopnea. |
|
|
How do you diagnose edema?
|
1) Lymphedema: Swollen lymph nodes
2) Venous obstruction: -Localized to area of obstruction (like DVT). -Distended veins. 3) Hypoalbuminemia: -Malnutrition. -Low serum albumin. -Nephrotic syndrome. -Protein in urine. 4) Hypervolemia: -Look for other features of hypervolemia. -Pulmonary congestion. -Hypertension. -Jugular venous distension. |
|
|
How do you treat edema?
|
*General:
-Diuretics and sodium restriction. -Elevate extremities when at rest. -Support stockings, especially for those who are ambulatory much of the day. *Disease-specific: -Treat hypervolemia. -Treat underlying disease (if possible). |
|
|
Take home points from this lecture:
|
*All of the volume disorders share common mechanisms.
*Mechanisms of renal sodium and water retention: 1) Reduced pressure at baroreceptors: -Increased sympathetic nervous system activity. -Increased renin/angiotensin/aldosterone activity. -Increased ADH activity. 2) Reduced urine flow in nephron; increased renin/angiotensin/aldosterone activity. *Sodium is your best friend in states of volume depletion. *And your worst enemy in volume overload. |

