![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
131 Cards in this Set
- Front
- Back
|
6. Young man has removed his buprenorphine patch on the morning of surgery. What time till PLASMA reaches half original level A. 12 hours B. 18 hours C. 24 hours D. 30 hours E. 36 hours |
A. 12 hours MIMS PI for Norspan “After removal of a Norspan patch, buprenorphineconcentrations decline, decreasing approximately 50% in 12 hours (range 10 to24 hours).” [be careful! This question has been asked previously about both fentanyl and buprenorphine!] |
|
|
7. A 58yo with solitary hepatic metastasis from colon cancer scheduled for resection of R lobe of liver. In order to manage the risk of intra-operative haemorrhage, it is most important to maintain: A. High CVP in anticipation of heavy blood loss B.Decreased MAP to reduce arterial bleeding C.Decreased CVP to reduce venous bleeding D. Normal MAP in anticipation of heavy blood loss E. Normal CVP to ensure adequate filling of the heart. |
C. Decreased CVP to reduce venous bleeding CEACCP Anaesthesia for hepatic resection 2009.pdf |
|
|
8. An 80yo man is having a transuretheral bladder resection, the surgeon is using diathermy close to the lateral bladder wall which results in patient thigh adduction. The nerve involved is: A. Inferiorgluteal B.Obturator C. Pudendal D. Scaitic E. Superiorgluteal |
B.Obturator |
|
|
17. In Conn'ssyndrome, the usual derangement is: A.Hypoglycaemia, hypokalaemia and hypernatraemia B. Hypoglycaemia,hyperkalaemia and hyponatraemia C.Normoglycaemia, hypokalaemia and hypernatraemia D.Normoglycaemia, hyperkalaemia and hyponatraemia E.Hyperglycaemia, hyperkalaemia and hyponatraemia |
C. Normoglycaemia, hypokalaemia and hypernatraemia Conn's syndrome = primary hyperaldosteronism S+S: HT, dec K+,met alkalosis, inc aldosterone, dec renin, rarely inc Na+About 20% have impaired glucose tolerancedue to the inhibitory effect of dec K on insulinaction and secretion, but DM is no more commonhttp://emedicine.medscape.com/article/127080-overview#a4 |
|
|
18. A 60 year old woman is admitted to hospital with subarachnoid haemorrhage. Her GCS is 11,and her blood pressure is 175/110 mmHg. She is administered oral nimodipine.The main reason for this treatment is: A. Control her blood pressure B. Manage acute hydrocephalus C. Prevent delayed cerebral ischaemia D. Reduce the risk of rebleeding E. Treat angiographically-proven cerebral vasospasm |
C. Prevent delayed cerebral ischaemia CEACCP |
|
|
19. You are theanaesthetist at a Caesarean Section for a 36/40 gestation pregnancy. The baby at birth is floppy and apnoea. You decide that positive pressure ventilation via mask is necessary. The recommended FiO2 is: A. 0.21 B. 0.4 C. 0.6 D. 0.8 E. 1.0 |
A - 0.21 For term infants, air should be used initially with supplemental oxygen reserved for those whose saturations do not meet the lower end of the targets despite respiratory support [Class A, expert consensus opinion]. |
|
|
You areinducing a 20-year-old female who has an IV cannula in her antecubital fossa,which was inserted in the emergency department. She complains of pain after 10mL of propofol and it becomes clear that cannula is intraarterial. The best management option is: A.Intraarterial injection of 5mL 1% lignocaine B.Intraarterial injection of 30mL Normal Saline C.Intraarterial injection of 50mg papaverine D.Intraarterial injection of 500u heparin E.Observation |
A. Intraarterial injection of 5ml 1% lignocaine Principles: dilute irritant, reverse vasospasm, prevent thrombosis. OHEIA p410: - stop injecting - leave cannula in place - lignocaine 100mg + papaverine 40mg in 10-20ml NS via cannula - regional blockade upper limb (BP or stellate ganglion) - systemic analgesia - formal anticoagulation with IV heparin and then warfarin - early guidance from vascular surgeon |
|
|
21. When is it necessary to use glycine as irrigation fluid for TURP? A. For monopolar diathermy B. For bipolar diathermy C. ForNd:Yag laser D. Greenlight laser |
A. For monopolar diathermy |
|
|
A 69 yo man is brought into ED by ambulance with a compound fracture of his forearm from an unwitnessed fall. Has a history of schizophrenia and depression with uncertain medication compliance. He is confused and agitated with generalised rigidity but no hyperreflexia. Obs - HR120, BP 160/90, RR 18, Sats 98 Temp 38.8 Likely Dx? A. Heat stress from anticholinergic therapy B. Hypoxic ischaemic encephalopathy C.Neuroleptic malignant syndrome D.Serotonin syndrome E. Pain from the compound fracture |
C. Neuroleptic malignant syndrome NMS = rare idiosyncratic reaction to antipsychotic drugs which resembles MH Autonomic dysfunction (sweating, labile BP, salivation, urinary incontinence, fever) + Extrapyramidal dysfunction (rigidity, dystonia, mental status change) Increased CK and WCC |
|
|
With surgical bleeding, the first clotting factor to reach a critical level is A. I B. II C. VII D. X E. XIII |
A. I (fibrinogen) |
|
|
Anaesthetic and respirable gas supplies to wall outlets in the operating theatre is at pressures of A. 200kPa B. 400kPa C. 500kPa D. 750kPa E. 1200kPa |
B. 400kPa |
|
|
21. The most useful sign to distinguish between severe serotonin syndrome and malignant hyperthermia are A. Clonus B. Hyperthermia C. Metabolic acidosis D. Muscle rigidity E. Wheeze |
A. Clonus B. both C. MH D. both E. neither |
|
|
33. Patient having a laparotomy. On prednisolone for 6/12, 10mg/day. What is the equivalent dose of dexamethasone? A) 2mg B) 4mg C) 6mg D) 8mg E) 10mg |
A. 2mg 4mg dex = 25mg pred = 100mg hydrocort Need to replace perioperatively if >10mg/d of prednisone in the past 3 months. > 3months ago no periop steroids needed |
|
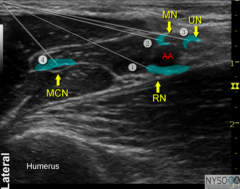
34. Axillary arm block U/S presented similar to this ultrasound image. Nerves marked with numbers 1-4. Patient having an operation of a lacerated index finger under regional anaesthesia.Which combination will provide adequate cover? A) 1 and 2 B) 1 and 3 C) 2 and 3 D) 2 and 4 E) 3 and 4 |
A. 1 and 2 Index finger - plantar surface is median n, dorsal is radial n |
|
|
35. Child 20kg having a caudal. Has a VF arrest post non-responsive to usual treatments. What dose of intralipid 20% would you give? A) 10mL B) 20mL C) 30mL D) 40mL E) 50mL |
C. 30ml Bolus 1.5ml/kg over 1 min * 3 q 5 min Infusion 15ml/kg/h, then 30ml/kg/h after 5 min Max dose 12ml/kg https://www.aagbi.org/sites/default/files/la_toxicity_2010_0.pdf |
|
|
40. Labour epidural placed. Headache postpartum. Which of the following is inconsistent with post partum dural puncture headache. A. Headache located frontal only B. Presents > 24 hrs post partum C. presents immediately post partum D. associated with auditory symptoms E. associated with neck stiffness |
C. Presents immediately post-partum 66% in first 2 days 90% in first 3 days |
|
|
41. Eclamptic patient. Given Magnesium intravenously. Which of these symptoms is often associated with magnesium administration? A. Bradyarrhythmia B. Cardiac arrest C. Hypotension D. Depressed respiratory effort E. |
D. Depressed respiratory effort Magpie trial Most to least: Flushed, N/V, injection problems, weakness, absent or reduced reflexes, respiratory depression (51 women), thirst, headache, hypotension (36 women) or palpitation or tachycardia |
|
|
42. The clinical sign that a lay person should use to decide whether to start CPR is: A. absence of breathing B. loss of central pulse C. loss of peripheral pulse D. loss of consciousness E. obviousairway obstruction |
A. Absence of breathing |
|
|
45. What is the maintenance fluid rate for a 15kg child? A. 60ml/hr B. 50ml/hr |
B. 50ml/h 4:2:1 rule |
|
|
46. Patient's K+ is 7.0 what is the best initial management? A. give Ca B. give insulin/ dextrose |
A. give Ca Stabilise myocardium (Ca) Drive K into cells (15U Actrapid, 50ml 50% glucose) B-agonist NaHCO3 if acidotic Resonium (15g PO, 30g PR q8h) Dialysis OHEIA p 296 |
|
|
47. Which patients require antibiotic prophylaxis? a) Previous mitral valve ring annuloplasty b) Previous patch repair of VSD |
A. if used prosthetic material B. if in the last 6 months OHA p1255 AHA guidelines: - prosthetic valve - previous endocarditis - unrepaired CHD including palliative shunts and conduits - repaird CHD within 6 months - repaired CHD with residual defect at site/adjacent - cardiac transplant with valvuloplasty |
|
|
48. A 63 yo lady has a difficult thyroidectomy for cancer. Immediately post extubation she develops stridor and respiratory distress.The most likely cause is A. Hypocalcaemia B. Recurrent laryngeal nerve palsies C. Tracheomalacia D. Neck oedema and haematoma E. Vocal cord oedema |
B. Recurrent laryngeal nerve palsies http://ceaccp.oxfordjournals.org/content/7/2/55.full |
|
|
49. A 23 yo has a traumatic brain injury. Which fluid is relatively contraindicated? A. Albumin B. Normalsaline C. CSL D. Colloid E. |
A. Albumin SAFE trial |
|
|
50. 50yr old smoker presents for laparotomy. PFTs given, what is the cause? FEV1, FVC both reduced, FEV1/FVC 98%. TLC, RV, DLCO 8 (pred = 30) A. PE B. Obesity C. Bilateral phrenic nerve palsies D. Pulmonary fibrosis E. COPD |
D. Pulmonary fibrosis Diffusion abnormality. Restrictive picture. OHA p102, 1264 |
|
|
51. Traumatic brain injury patient. Cerebral angiogram shows cerebral perfusion =15mL/100g/min, cerebral oxygen consumption 3.5mL/100g/min. This is consistent with: A. Cerebral hyperperfusion B. Reperfusion injury C. Cerebral ischaemia D. Appropriate auto regulation E. ?cerebral vasoconstriction |
C. Cerebral ischaemia Normal perfusion = 50mL/100g brain tissue/min Normal CMRO2 (awake brain) =3.5mL/100g/min, reduced in coma/anaesthesia. 15ml blood carries 3ml O2 (assuming normal value 200ml of O2 per litre blood). Therefore ischaemia is the best choice. [15ml/100g/min is critical threshold for development of irreversible tissue damage.] |
|
|
52. Absolute contraindication to ECT: A. Cochlear implants B. Epilepsy C.Pregnancy D. Raised intracranial pressure E. Recent myocardial infarction |
E. Recent myocardial infarction |
|
|
57. FFP is given to a patient to treat hypofibrinogenaemia. The volume required to raise the fibrinogen by 1g/L is A. 1mL/kg B. 5mL/kg C. 10mL/kg D. 20mL/kg E. 30mL/kg |
E. 30ml/kg |
|
|
58. The diluted thrombin time measures the anticoagulant activity of A. apixaban B. rivaroxaban C. dabigatran D. warfarin E. heparin |
C. dabigatran |
|
|
59. In a trauma patient the main mechanism by which hypothermia exacerbates bleeding is by A. altered blood viscosity B. causing DIC C. inhibition of clotting factors D. potentiation of anticoagulant effect of drugs used to treat DVT E. decreasesplatelet number and function |
C. inhibition of clotting factors Hypothermia+acidosis+coagulopathy = lethad triad in traumapatients |
|
|
60. A patient having a liver resection suffers a haemodynamically significant venous air embolism. During resuscitation how do you best position the patient? A. head up, right side down B. head up, left side down C. head up,no lateral tilt D. head down, right side down E. head down, left side down |
B. head up, left side down OR E. head down, left side down Controversial: - want air entrainment site below the level of the RA (ie head up) - but if already HD significant, want to reduce air lock by moving air bubble out of RVOT so want head down - always want L side down to prevent movement across to L side of heart |
|
|
61. In a normal adult what amount of IV potassium chloride is needed to raise the serum potassium from 2.8 to 3.8mmol/L? A. 10mmol/L B. 20mmol/l C. 50mmol/L D. 100mmol/L E. 200mmol/L |
E. 200mmol/L If serum K<3.0, need 200mmol/L to raise level by 1.0 If serum K >3.0, need 100mmol/L to raise level by 1.0 OHA p 182: 0.3mmol/L drop in K+ means aloss of 100mmol of K+ from total body store |
|
|
In a haemodynamically stable 20 year old man with blunt chest trauma, the best screening test to diagnose cardiac injury requiring treatment is: A. CXR B. serum CK-MB C. serum troponin D. 12 lead ECG E. Transthoracic Echocardiogram |
D. 12 lead ECG If unstable, need TTE |
|
|
63. With regards to medical ethics, the concept of fidelity involves: A. equitable distribution of resources B. following a professional code of conduct C. promoting well being D. wise useof resources E. witholding of futile treatments |
B. following a professional code of conduct Fidelity = do as you say you will do andrespect confidentiality |
|
|
64. What is the correct position for the tip of a PICC in a child A. Carina B. Below right tracheobronchial angle C. Above right heart border D. Sternoclavicular junction E. |
A. Carina "At the level of the tracheal bifurcation" http://www.anzca.edu.au/communications/anzca-e-newsletter/e-news-articles/Coroners%20report%20PICC%20line%20AR%20summary%20Feb%2010.doc/view |
|
|
65. Image of alateral C-spine Xray. Asked what the diagnosis was. [Terrible image quality. Seemed to have anterior atlantoodental interval >9mm.] A. Atlantoaxial instability B. Retropharyngeal haematoma (?or abscess) C. Teardrop fracture D. Epiglottitis E. Unilaterfacet joint dislocation |
A. Atlantoaxial instability |
|
|
66. According to the ANZCA endorsed guidelines, what is the correct colour for the label for a subcutaneous ketamine infusion A. Pink B. Red C. Beige D. Blue E. Yellow |
C. Beige Beige: An infusion is colour coded based on it's route of administration. |
|
|
77. Prior tonasal intubation you spray Lignocaine/Phenylephrine preparation (CoPhenylcaine) into the nose. Some lands in the eye. What happens? A. Ecchymosis B. Myosis C. Midriasis D. Proptosis E. Nystagmus |
C. Midriasis Sympathetic stimulation of eye causes midriasis |
|
|
78. You trial a new drug to prevent PONV. It is 50% more effective than the current drug. Four percent of people still experience PONV with the new drug. How many people need to receive the new drug in place of the current drug to have one person lesss uffering from PONV? a) 2 b) 8 c) 15 d) 25 e) 33 |
D. 25 50% more effective = 8% of people previously experienced PONV. ARR = 8% - 4% = 0.04 NNT = 1/ARR = 1/ 0.04 = 25 |
|
|
79. What does a white cylinder with a Grey coloured shoulders/neck contain? a) Medical air b) Carbon Dioxide c) Helium d) Oxygen e) Argon |
B. Carbon dioxide A. Medical air - black and white C. Helium - brown (Heliox brown and white) D. Oxygen - white shoulders E. Argon - peacock blue N2O = ultramarine Entonox = ultramarine + white |
|
|
80. The best solution to ensure a sepsis prior to neuraxial anaesthesia is A. 0.5% Chlorhexidine B. 0.5% Chlorhexidine with 70% alcohol C. 5% PovidineIodine D. 5% Povidine Iodine with 70% alcohol E. 10% Povidine Iodine |
B. 0.5% chlorhexidine with 70% alcohol PS28 recommends 0.5% chlorhexidine in alcohol |
|
|
81. You are anaesthetising a 25 year male for an open appendicectomy. He has a Fontans circulation on a background of tricuspid atresia. The best strategy to manage his ventilation intraoperatively would be: A. Ensure adequate PEEP B. Decrease inspiratory time C. Shorten I:E Ratio from 1:3 to 1:1.2 D. Increase inspiratory time but with reduced inspiratory pressures E. Ensure adequate spontaneous ventilation |
B. Decrease inspiratory time E. ?? best Management of Fontans: - dec RR - dec insp time - dec PEEP - low TV 5-6ml/kg - RSI |
|
|
82. You are anaesthetising a 70 year old woman for CABG with a pulmonary artery catheter insitu. After separation from bypass you notice frank, copious blood rising inthe endotracheal tube. Your immediate action should be to: A. Check ACT B. Insert adouble lumen tube C.Reinstate bypass D. Administer protamine E. Pull back the pulmonary artery catheter several centimetres |
C - Reinstate bypass (unless full reversal of heparin as the CPB will clot) |
|
|
Penetratinginjury to chest. What part of the heart most likely injured? A. RV B. LV C. RCA D. LA E. RA |
A. RV most anterior / exposed (from EMST) Then LV |
|
|
89. General anaesthesia is preferred for endoluminal stenting because: A.Ischaemic renal pain B.Prolonged periods of apnoea required C.Painful aorta D.Major risk of haemorrhage E.Trash foot pain |
B. Prolonged periods of apnoea required No real best answer as only short apnoea is required and pt staying still for runs "Patient comfort" due to prolonged procedure would be best answer (CEACCP) but definitely wasn't an option. |
|
|
90. Which volatile agent has minimum effect on ICP at 1 MAC A. Isoflurane B. Sevoflurane C. Desflurane D. Enflurane E. Halothane |
B. Sevoflurane Sevo. Current Opinion in Anaesthesiology: October 2006 - Volume 19 - Issue 5 - p 504-508 |
|
|
97. You are inserting a right internal jugular vein CVL. Why is it important to avoid turning the patient's head extremely to the left? A. Uncomfortable for the patient B. Increases risk of internal carotid artery puncture C. Compresses internal jugular vein and makes it more difficult to puncture D. Distorts the anatomy, making the vein more difficult to correctly identify E. Increases risk of external jugular vein puncture |
C. Compresses internal jugular vein and makes it more difficult to puncture D. Distorts the anatomy, making the vein more difficult to correctly identify
TOTW 138. “excessive turning should beavoided as it changes the relationship of the vein and artery and can collapsethe vein” |
|
|
98. Patient two hours after bilateral crush injuries to lower limbs. What would you expect to see? A. Hypocalcaemia B. Hypokalaemia C. Hypophosphataemia D. Hypouricaemia E. Metabolic alkalosis |
A. Hypocalcaemia CEACCP Compartment injury 6: Efflux of intracellular contents into the circulation follows myocyte injury. This can result in the rapid development of hyperkalaemia, hyperuricaemia and hyperphosphataemia. A metabolic acidosis develops in severe rhabdomyolysis secondary to lactic acid production from ischaemic muscle and the release of other organic acids. Hypocalcaemia is frequently recorded in early rhabdomyolysis owing to calcium accumulation in damaged muscle. During the recovery phase, hypercalcaemia can develop as a result of secondary hyperparathyroidism and the extrusion of calcium from recovering muscle cells. |
|
|
99. Delivery of neonate. Meconium liqour. Baby floppy, blue, apnoeic, pulse rate 90bpm. What is the next step in management? A. Commence PPV B. Suction the trachea C. Commence CPR D. Dry andstimulate E. |
B. Suction the trachea |
|
|
103. You inject 10ml ropivacaine into a T5 paravertebral block. Patient becomes bradycardic, hypotensive and apnoeic. What is the cause. A.Contralateral spread B.Intrathecal spread C.Inadvertent intravascular injection D. Local anaesthetic toxicity |
B. Intrathecal spread (IV injection --> seizure, contralateral spread--> bilateral block, not large enough dose for LA toxicity |
|
|
110. Medical therapy vs TAVI in inoperable patients. At 30 days, decreased risk of: A. B. Myocardial infarct C. Death D. Stroke E. Atrial fibrillation |
D. Stroke PARTNER B trial (inoperable) At 30d, - TAVI death higher (non-sig) - TAVI higher major strokes (P 0.06) - MI and AF same At 1y: - medical therapy death higher (sig) |
|
|
111. Glycine 1.5% used during urology case. Osm is: A. B. 200 C. 250 D. 300 E |
B. 200 CEACCP 220mosm/l Glycine is used because it is electrically non-conductive. This prevents dispersion of the diathermy current. |
|
|
112. Volatile analysis in most anaesthetic machines is done via which method? A. Gas chromatography B. Infrared analyser C. Raman spectrometry D. E. |
B. Infrared analyser O2 analysis by paramagnetic sensor. CO2 by in-line infrared. Volatilesby sidestream infrared absorption spectroscopy. CEACCP Respiratory gas analysis 2009 |
|
|
114. What is not a constituent of Prothrombinex VF? A. Antithrombin III B. Factor II C. Factor X D. Protein C E. Heparin |
D. Protein C Prothrombinex VF contains factors II, IXand X and a small amount of factors VII and V. Also ATIII, heparin, citrate,Na, Cl, PO4, human plasma proteins. |
|
|
142. 50yo lady for elective laparoscopic cholecystectomy seen in Preadmission Clinic. No symptoms of heart disease, walks her dog for 30 minutes each day. ECG [no image— described in words] shows LAD, RSR in V1, wide slurred S in V6 and QRS duration 0.13 msec. Your options: A. Give atropine premedication B. She needs a permanent pacemaker C. She needs temporary pacing wires D. Continue with the case E. Refer to cardiology OP prior to doing the case |
D Bifascular block: - LAD = LAFB - RBBB OHA Preoperative management 1. First degree heart block in the absence of symptoms is common. No investigation or treatment is necessary is asymptomatic. 2. Second (especially fixed dropped beats - no Wenckebach) or third degree heart block may need pacemaker insertion. If surgery is urgent this may be achieved quickly by inserting a temporary transvenous wire prior to definitive insertion. 3. Bundle branch, bifascicular, or trifascicular block will rarely progress to complete heart block during anaesthesia and so it is not normal practice to insert pacing wire unless there have been episodes of syncope. Indications for preoperative pacing 1. symptomatic first degree heart block 2. symptomatic second degree Mobitz I heart block 3. Second degree Mobitz II heart block 4. Third degree heart block 5. Symptomatic bifascicular block or symptomatic first degree heart block plus bifascicular block (trifascicular block) 6. Slow rate unresponsive to drugs |
|
|
143. You are performing epidural anaesthesia on an adult patient. To minimise the chance of inserting the epidural catheter into a blood vessel you would: A. Inject saline through the epidural needle prior to threading the catheter B. Perform the procedure with the patient lateral rather than sitting C. Use a loss of resistance to air technique instead of loss of resistance to saline. |
A. Inject saline through the epidural needle prior to threading the catheter, OR B. Perform the procedure with the patient lateral rather than sitting Both A and B reduce the risk. A. from A+A 2009 |
|
|
144. Failed intubation. Difficult ventilation. Rescued with a Classic LMA.Decide to use a bronchoscope to intubate down the LMA. Which device will allow you to intubate the patient safety? A. Aintree catheter B. Airway exchange catheter C.Gum elastic bougie D. Some angiogram wire I’ve never heard of! E. Two paediatric endotracheal tubes side-by-side |
A. Aintree catheter Aintree Intubating Catheter - use with paed bronchoscope and >=#7.0 ETT |
|
|
150. Blalock-Taussig shunt inserts into the right pulmonary artery, originating from the: A. Right subclavian artery B. IVC C. SVC D. Aorta E. Axillary artery |
A. Right subclavian artery BT shunts used as initial treatment of TOFin symptomatic patients prior to definitive surgery.Shunts from R subclavian artery to R pulmonary artery. It improves bloodflow to pulmonary circulation by providing a route for returning systemic bloodthat bypasses the RV outflow obstruction. Arterial O2 sats of 70-85% areoptimal after this as they indicate a balance between pulmonary and systemiccirculation |
|
|
New. Time taken for insulin to reduce K+in hyperkalaemia A. 2 mins B. 4 mins C. 10 mins D. 20 mins E. 30 mins |
D. 20 mins
LITFL 20 mins RCH onset 15-20 mins Peak 60 mins |
|
|
Increased risk with eye block: A. Peribulbar done medial canthus B. Peribulbar done inferior-temporal C. Sub-Tenons D. <45years age E. Anotherclearly wrong |
? A or B Or retrobulbar is highest risk |
|
|
2/12 oldbaby. Initially on 30th centile and now on 5th. Murmur, systolic, loud at apex. Pulses are weak, "most easily felt at the femoral". A: VSD B:Co-arctation C: Venoushum D: PDA |
A. VSD - systolic murmur with all pulses weak B. Coarctation has ESM with dec LL pulses C. Venous hum is continuous D. PDA is machinery murmur with bounding pulses |
|
|
Some diathermy pads have two separate electrodes on the patient pad, each with its own cable back to the machine. Why? A: In case one fails the other can serve as a back-up B: One for coag and one for cutting C: For bipolar? - worded slightly differently D: For capacitance measurement - again wording not right E: For return electrode monitoring |
E. For return electrode monitoring http://www.asit.org/assets/documents/Prinicpals_in_electrosurgery.pdf Wikipedia |
|
|
Cisatracurium left out of fridge for 4 days. It’s efficacy is now: A. 60% B. 70% C. 90% D. 50% E. 99% |
E. 99% Can be left out of fridge for 21 days. Loss of efficacy is 5%/month at room temperature. |
|
|
In which type of von Willebrand's disease is DDAVP contraindicated? A. Type 1 B. Type 2a C. Type 2b D. Type 3 E. None of the above |
C. Type 2b - risk of aggravated thrombocytopaenia and thrombotic complications A. Type 1 - DDAVPapproved for use B. Type 2a - usemust be discussed withhaematologist due to variable effect D. Type 3 -DDAVPuseless E. None of the above |
|
|
This ECG with AAI pacing shows: The12-lead ECG showed pacing spikes followed by p-waves, with QRS's following the p-waves with progressive prolongation of the PR until a QRS was dropped. A. Failure to capture B. CHB C. 2nddegree HB D. AF |
C. second degree heart block Pacemaker codes Position 1 - pacing (O, A, V, D) Position 2 - sensing (O, A, V, D) Position 3 - response to sensing (O = none, I = inhibit, T = triggered, D = dual I+T) Position 4 - programmability Position 5 - multisite pacing (O, A, V, D) |
|
|
The NAP4 audit showed that the most common cause of airway problems/ complications/ disasters in INTENSIVE CARE is: A. Aspiration B. Dislodged tracheostomy tube |
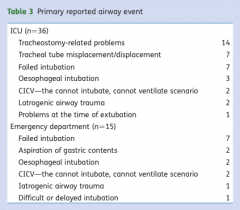
B. Dislodged tracheostomy tube At least one in four major airway events in a hospital are likely to occur in ICU or the ED. The outcome of these events is particularly adverse. Analysis of the cases has identified repeated gaps in care that include: poor identification of at-risk patients, poor or incomplete planning, inadequate provision of skilled staff and equipment to manage these events successfully, delayed recognition of events, and failed rescue due to lack of or failure of interpretation of capnography. The project findings suggest avoidable deaths due to airway complications occur in ICU and the ED. (Aspiration greatest problem with anaesthesia related deaths) |
|
|
The target serum magnesium level in a patient with pre-eclampsia receiving a magnesium infusion is A. 1-2mmol/l B. 2-3.5mmol/l C. 3-6mmol/l D. 4-6mmol/l E. 5-8mmol/l |
B. 2-3.5 mmol/L LITFL 2-4mmol/L. SOMANZ recommends not measuring levels but being guided by reflexes? |
|
|
Timing of peak respiratory depression after intrathecal 300 mcg morphine: A. < 3.5hours B. 3.5 –7.5 hours C. 7 - 12.5hours D. 12.5 -18hours E. > 18hours |
B. 3.5 –7.5 hours CEACCP morphine peak ~6h but up to 24h;fentanyl peak between 0-1h. ANZCA Acute Pain: Scientific evidence 3rdedition p195: resp depression peaked at 3.5-7.5h following ITM of 200-600mcgdoses |
|
|
What part of a modern anaesthesia machine allows jet ventilation to be performed using the oxygen flush button? A.Non-return valve downstream of the vaporisers B.Pressure-limiting valve at the outlet C.The presence of a common gas outlet D.Presence of auxillary oxygen flowmeter |
A.Non-return valve downstream of the vaporisers (Clinical anaesthesia) |
|
|
Red-man syndrome secondary to vancomycin is due to A. Type II hypersensitivity reaction B. Vasodilation C. Mast cell degranulation D. IgE-mediated response E. Serotoninrelease |
C. Mast cell degranulation Up2Date |
|
|
Patientwith IgA deficiency. What is the main issue in anaesthesia? A. Anaphylaxis to blood products B.Renal impairment C. D.Sensitivity to opioids E.Sensitivity to muscle relaxants |
A. Anaphylaxis to blood products |
|
|
Cryo "should be used within" or "must be used within" or "is most effective if used within" : A. 30minutes B. 3 hours C. 6 hours |
C. 6 hours “Transfuse immediately after thawing and use within 4 hours” (pmh.health.wa.gov.au) LITFL: use within 6 hours if a closed single unit, or within 4 hours if open system or units have been pooled. |
|
|
Designing a study on PONV. What is the advantage of designing a study incorporating multivariate analysis? A. Less type 1 error B. Less complex C. Less difficult to interpret D. Less confounding E. Fewer patients required |
C. Less difficult to interpret D. Less confounding E. Fewer patients required Oxford Journals: Advantages: -resemble closely how researcher thinks about the data -easier visualisation and interpretation of data - more data analysed simultaneously so greater statistical power - regression models give more insight into relationships between variables - focus on relationships between variables rather than isolated individual factors http://www.oxfordjournals.org/our_journals/tropej/online/ma_chap1.pdf |
|
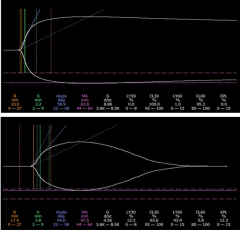
Bleeding intraopratively. TEG shown. What should be used to treat? A. TXA B. Platelets C. Cryo D. FFP E. |
A. TXA to treat fibrinolysis Normal R, K, angle and MA vales. LY30 and LY60 were low, CL30 and CL60 high. It didn't take me long to Google the TEG image that ANZCA lifted for this question! I'm almost certain it was Figure 1B from: Pepperell 2014, "Clinical Application of Fibrinolytic Assays |
|
|
A size Coxygen cylinder (in New Zealand, "A") that reads 5000kpa contains approximately how many litres of oxygen a. 100 b. 150 c. 200 d. 350 e. 600 |
B. 150L BOC guide: Size C contains ~490L when full.Full pressure is ~13700kPa |
|
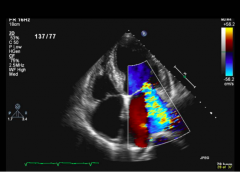
4-chamber TTE view. What lesion is present? |
Mitral regurgitation |
|
|
Appropriate infection control measures when anaesthetising a patient with iatrogenic variant-CJD, the airway equipment should be: A. thrown away B. plastic sheath, reuse C.sterilisation with ethylene oxide D. sterilisation with heat at 134 degrees for 3 minutes. E.autoclave |
A. thrown away |
|
|
A varienton the theme of the previous question referring to PS9. Minimum requirements to provide sedation. This time asked who is necessary to provide conscious sedation, using propofol. A. medical practitioner trained in use of propofol B. medical practitioner trained in use of propofol + their assistant |
B. Medical practitioner trained in use of propofol + their assistant At least 3 people: proceduralist, medicalpractitioner trained in use of propofol, assistant(for more complex patients or procedures,need an extra assistant) |
|
|
Intubation view: Little space between epiglottis and posterior pharyngeal wall. What is the modified C&L classification? A. 2A B. 2B C. 3A D. 3B E. 4 |
C. 3A 1 – most of glottis visible 2A – glottis visible 2B – glottis not visible (only arytenoidsvisible) 3A – Only epiglottis visible, bougiepossible 3B – Only epiglottis visible, bougie notpossible 4 – no laryngeal structures visible |
|
|
What feature most increases vasospasm in setting of SAH? A. Size of aneurysm B. Age of patient C. Positionof Aneurysm D. Large amount of blood on CT E. GCS on arrival to ED |
D. Large amount of blood on CT LITFL: best predicted by radiologicalgrade, amount of blood and location, thick basal cistern blood and blood inlateral ventricles |
|
|
Line isolation monitor alarming at 5ma – what do to? A. Disconnect non essential equipment 1 by 1 to identify fault B. Ignoreit |
A. Disconnect non essential equipment 1 by 1 to identify fault |
|
|
Maintenancefluid rate in 15kg child – mls/hr A. 40mls/hr B. 50mls/hr C. 90mls/hr D.300mls/hr |
B. 50ml/h |
|
|
"Hypothermia makes bleeding in trauma worse because..." A. Reduced platelet function AND Number B. Reduced activity of clotting factors |
B. main thing to increase bleeding (can't remember other options but one about platelets definitely said function AND number...) hypothermia reduces function of plt and function of clotting factors |
|
|
Most effective (?quickest) way to reduce serum K+ level in hyperkalaemia 8.0meq/L? A. Calcium gluconate B. Resonium C. Salbutamol NEB D. 15 units actrapid and 50 mls of 50% Dextrose E. Sodium bicarbonate ?50mmol |
D. 15 units actrapid and 50 mls of 50% Dextrose |
|
|
ECG rhythmstrip. Showed regular pacing spike followed by wide QRS complexes. But once there is a narrow QRS occurring without a pacing spike, followed shortly after by a pacing spike but no capture. What does ECG show? A. AAI with failure to capture B. AAI with failure to sense C D. VVI with failure to capture E. VVI with failure to sense |
? VVI with failure to sense, I think is the answer. The narrow QRS complex was an intrinsic beat, but the pacer didn't sense so paced shortly after at its regular interval. The myocardium was still refractory so there was no capture, but failure to sense was the original problem. |
|
|
Relative contraindications to mediastinoscopy include A.Cervical spondylosis B.Emphysema C.Mediastinal lymphadenopathy D.Poor left ventricular function E.Superior vena cava syndrome |
E.Superior vena cava syndrome Previous mediastinoscopy is a relatively strong contraindication to arepeat procedure because scar tissue eliminates the plane of dissection. Superior vena cava (SVC) syndrome increases the risk of bleeding from distendedveins and is a relative contraindication. Other relative contraindicationsinclude severe tracheal deviation, cerebrovascular disease, severe cervicalspine disease with limited neck extension, previous chest radiotherapy, andthoracic aortic aneurysm |
|
|
How should you dose suxamethonium for intubation in an obese patient? A. Lean body weight B. Ideal body weight C. Ideal body weight + 25% D. Actual body weight E. Actual body weight + 25% |
D. Actual body weight Max 120-140mg |
|
|
Time to onset of TRALI with transfusion? A. 2 hours B. 4 hours C. 12 hours D. 24 hours E. 48 hours |
A. 2 hours OR B. 4 hours P Kam article “during or within 6hours” http://www.transfusionmedicine.ca/articles/transfusion-related-acute-lung-injury-trali "Symptoms of TRALI typically develop during, or within 6 hours of a transfusion. Patients present with the rapid onset of dyspnea and tachypnea. There may be associated fever,cyanosis, and hypotension. Clinical exam reveals respiratory distress and pulmonary crackles may be present with no signs of congestive heart failure or volume overload.Resolves within 72-96h. TRALI in Blood Journal. “Majority of cases occur within 1-2 hours” “ Diagnosis within 6 hours” |
|
|
When performing regional anaesthesia for eye surgery, needle damage to the globe of the eye is more common with: A. a globe axial length of less than 25 mm B. patients aged less than 45 years C. peribulbar block using the inferotemporal approach D. peribulbar block using the medial canthus approach E. sub-Tenon block |
? C. peribulbar block using the inferotemporal approach, or ? D. peribulbar block using the medial canthus approach |
|
|
Best method to assess reversal of neuromuscular blockade? A.Sustained head lift 5 sec B.Sustained leg lift 5 sec C.TOF 0.9 with accelerometer D.DBS no fade E.Tetanus 50Hz F.Tidal volumes... ? |
C. TOF 0.9 with accelerometer |
|
|
The Neonatal Facial Coding Scale (NFCS), used to assess pain in neonates, includes all of the following EXCEPT A. brow bulge B. chin quiver C. closed mouth D. deep nasolabial fold E. eyes squeezed shut |
C. closed mouth p345 3rd ed ANZCA Pain: Scientific evidence Facial actions monitored: (1) brow lowering (lowering and drawing together of the brow can result in brow bulge) (2) eyes squeezed shut (3) deepening of the naso-labial furrow (fold) (4) open lips (any separation of the lips is an occurrence) (5) vertical mouth stretch (6) horizontal mouth stretch (7) taut tongue (cupping of the tongue) (8) chin quiver (high frequency vibration of the chin and lower jaw) (9) lip pursing (tightening the muscles around the lips to form an "oo") In addition a tenth activity was monitored in preterm infants: (10) tongue protrusion (this is a "no pain" response in full term infants) |
|
|
What is the best measure of the anticoagulant effect of Dabigatran? A. APTT B. Dilute thrombin time C.Prothrombin time D. Bleeding time E. TEG |
B. Dilute thrombin time |
|
|
Small air bubbles in the arterial line system will ALWAYS REDUCE the A.Dampening coefficient B.Extrinsic Coefficient C. Measured systolic pressure D. Measured MAP E. Resonant frequency |
E. Resonant frequency |
|
|
A patient undergoing liver surgery has a venous air embolism, what is the most appropriate position to place them in: A. Reverse trendelenburg, right side up B. Reverse trendelenburg left side up C. Reverse trendelenburg, neutral D.Trendelenburg, right side up E. Trendeleburg, left side up |
A. Reverse trendelenburg, right side up, OR D.Trendelenburg, right side up |
|
|
During interscalene block placement get medial movement of the scapula. This is secondary to stimulation of: A: long thoracic nerve B: dorsal scapula nerve C: suprascapular nerve D: supraclavicular nerve E: accessory nerve |
B: dorsal scapula nerve arises from C5 root, innervates rhomboids long thoracic from C5-7 suprascap --> supra and intraspinatus supraclav--> cut to supraspin, shoulder, etc accessory --> SCM and trapezius |
|
|
Blue urticaria is a complication of A. B. Methylene blue C. Patent blue V D. Anaphylaxis E. |
C. Patent blue V |
|
|
Sub-Tenon’sblock. What is the BEST position to insert block? A. Inferonasal B. Inferotemporal C. Superonasal D. Superotemporal E. Medial /canthal |
A. Inferonasal |
|
|
Most cephalic interspace in neonate to perform spinal while minimising the possibility of spinal cord puncture A. L1-L2 B. L2-L3 C. L3-L4 D. L4-L5 E. L5-S1 |
C. L3-L4 SC ends L3, dural sac S3 |
|
|
With respect to a patient with Multiple sclerosis, which of the following alters the risk of a flair post partum A. An epidural B. A spinal C. A flair in the year pre-partum D. A general anaesthetic E. Breastfeeding |
C. A flair in the year pre-partum |
|
|
Adenosine can be used to terminate an arrhythmia due to: A. Atrial fibrillation B. Atrial flutter C. WPW D. ??VT E. ??Torsafes |
C. WPW |
|
|
Mast cell tryptase half life: A. 1 hour B. 3 hours C. 6 hours D. 12 hours |
A. 1 hour, OR B. 3 hours CEACCP 2004 Anaphylaxis: 3h CEACCP 2014 anaphylaxis: 2h |
|
|
Best indicator of severe pulm HT: A. mean PA pressure 45mmHg B. orthopnoea C. PND D. ex tol less than 4 mets E. fev1, ... |
C. PND Indicates RHF Severe pulm HT, mean PAP > 55mmHg |
|
|
Youngpregnant patient with mild mitral regurgitation and moderate mitral stenosis, normal LV function. The best delivery method: A. Epidural anaesthesia LSCS B. Spinal with LSCS C. Epidural analgesia and normal vaginal delivery D. GA LSCS E. Normal vaginal delivery with remifentanil PCA |
C. Epidural analgesia and normal vaginal delivery |
|
|
Contained one of the following St John wort questions from Mar13 or Aug13. Can't remember which one! St John'sWort (Hypericum perforatum) potentiates the effects of A.Dabigatran B. Heparin C. Warfarin D. Aspirin E. Clopidogrel |
E. Clopidogrel Potentiates sedatives, clopidogrel, antidepressants |
|
|
St John's wort will reduce the effect of A. aspirin B.clopidogrel C.dabigatran D. heparin E. warfarin |
E. warfarin Decreases effectiveness of digoxin, antihistamines, immunosuppressants(cyclosporin, tacrolimus), warfarin, anticonvulsants |
|
|
7/7 post laparotomy platelet down to 40, no bleeding or bruising, but has painful swollen lower leg, most appropriate tx? A. Fondaparinux B. lepirudin C. IV heparin D. Clexane E. warfarin |
A. Fondaparinux An indirect factor Xa inhibitor. HITTS: Clexane and heparin contraindicated; warfarin pro-thrombotic; lepirudin discontinued |
|
|
Type 1 diabetes fasting since 2200, insulin infusion commenced 0700, BSL 7, what is MOA of insulin? A. Skeletal uptake B. liver uptake C. inhibit glucagon (release) D. inhibit glycogenolysis |
A. Skeletal uptake |
|
|
A three year old girl for an elective hernia repair is seen immediately prior to surgery. It is revealed she had 100mL of apple juice 2 hours ago. The best course of action is to: A. Postpone surgery for 2 hours B. Postpone surgery for 4 hours C. Postpone surgery for 6 hours D. Cancel surgery E. Continue with surgery |
E. Continue with surgery |
|
|
Acute intermittent porphyria, signs except: A. abdominal pain B. hypotension C. confusion D. tachycardia E. peripheral neuropathy |
B. Hypotension Inc catecholamines --> inc hypertension, tachycardia |
|
|
Audit in department of prevalence of acute myocardial ischaemia in vascular surgery.What type of data is this? A. Nominal B. Ordinal C. Categorical D. non-parametric E. numerical |
E. Numerical |
|
|
Preopclinic carotid endarterectomy asks about GA vs LA, you tell her: A. GA and LA has similar risk of stroke B. GA has slightly increased risk of stroke than LA C. LA has slightly increased risk of stroke than GA D. GA has significantly increased risk of stroke than LA E. LA has significantly increased stroke than GA |
A. GA and LA has similar risk of stroke GALA 2008: 30 day stroke/death similar,possibly decreased stroke at 1y in LA group |
|
|
Threshold for micro shock: A. 10uA B. 100uA C. 1mA D. 5mA E. 10mA |
B. 100uA (1mA for macroshock) http://www.anaesthesia.med.usyd.edu.au/resources/lectures/electricity.html |
|
|
Asystolic arrest adrenaline just given, how often do you give adrenaline? |
Every 2 cycles (4mins) |
|
|
Hepatic tumour resection, purpose of reducing CVP? |
Reduce venous bleeding |
|
|
Child-Pugh score. Components ? A. Bilirubin / albumin / INR, ascites, encephalopathy B. Various other options including AST/ALT, GGT, PT C. ? D. ? E. ? |
Child-Pugh score: bilirubin, albumin, PT, ascites, hepatic encephalopathy. Note GGT not included. Each scored 1-3 so min 5 and max 15. 5-6 = class A, one yr survival 100%, 2 yr85% 7-9 = class B, 81%, 57% 10-15 = class C, 45%, 35% |
|
|
Laser flextube with double cuffs - how to inflate cuff(s)? A. Inflate proximal then distal B. Inflate distal then proximal C. Inflate both with saline? D. Inflate distal only E. Inflate proximal only |
B. Inflate distal then proximal Melbourne course: inflate distal to check seal, then if need it because prox is punctured know that seal is correct. http://www.healthcare21.eu/wp-content/uploads/2014/06/Tracheal-Tubes-Airway-Product-Catalogue.pdf - In the product information says "for adequate protection during laser surgery, both cuffs must be filled with saline" http://webserver.anesthesiologynews.com/download/Cuffs_ANGAM10_WM.pdf: "inflate proximal, then the distal one can be inflated if the prox one is damaged. Designed to be filled with saline." |
|
|
Patient with HOCM has HR 60, SBP 70 post induction, what to do: A. give volume B. adrenaline C. metaraminol D. ?beta-blocker |
C. metaraminol CEACCP Cardiomyopathy and anaesthesia Maintain preload, HR 60-80, maintain SR, slight reduction in contractilitybeneficial, increase afterload slightly or maintain |
|
|
The following changes occur in ageing except: - increased CSF volume |
- |
|
|
Paediatric paracetamol loading dose PR mg/kg: A. 7.5 B. 10 C. 15 D. 20 |
D. 20mg/kg SCH (Sydney Children’s Hospital): 40mg/kgloading dose rectally (max 90mg/kg/day), otherwise 20mg/kg/dose) |
|
|
Postpartum post epidural with peripheral neurology. |
Answer in this case was probably lumbosacral plexus palsy, but be warned there are many variations on this type question with different answer depending on the neurology description. |
|
|
Question not recalled, but the keypoint was: - Posterior cord of brachial plexus --> weakness of wrist extension |
|
|
|
Endocarditis prophylaxis A. Bicuspid valve B. Congenital repair > 12 months ago C. Rheumatic heart valve D. Uncorrected cyanotic heart disease E. MVP + ?MR |
D. Uncorrected cyanotic heart disease |
|
|
Variation of sugammadex question. 1mg/kg rocuronium given in 70kg patient. Now CICO. What is the total dose of sugammadex that you will give? |
70x16=1120mg |
|
|
(New) Max size vessel for CVC insertion (New) How do you prevent breath stacking in COPD (New) Biggest risk factor for vasospasm post SAH? (New) CVC just inserted into patient. LIMthen goes off. What do you do? (New) Pneumoperitoneum created, sinus brady down to 20BPM. What to do? (New) Cell salvage results in less what? |
? Allow time for expiration. Large volume of blood Disconnect most recently connected piece of equipment Cease insufflation / Atropine/Glyco (OHA p 555) Less allogenic blood products being given. |
|
|
TAVI vs Max medical therapy nonoperable aortic stenosis reduction in risk at 30 days of A. AMI B. AKI C. Death D. Atrial fibrillation E. Stroke |
E. Stroke |
|
|
6 week old baby is booked for elective right inguinal hernia repair. An appropriate fasting time is A.2 hours for breast milk B.4 hours for formula C.5 hours for breast milk or formula D.6 hours for solids E.8 hours for solids, 4 hours for all fluids. |
B. 4 hours for formula <6 weeks: 2 clear fluids / 4 breastmilk or formula >6 weeks: 2 clear fluids/ 4 breastmilk /6 formula |
|
|
The size (in French gauge) of the largest suction catheter which can be passed through a size 8 endotracheal tube which will take up not greater than half the internal diameter is size: A.6 B.8 C.10 D.12 E.14 |
D. 12 Need <4.0mm.Divide French gauge by 3 to get diameter. |
|
|
70year old post TKJR. On sub-cut heparin. Develops clinical DVT and platelets 40.Management: A.Enoxaparin B.Fondoparinux C.Heparin by infusion D.Lepirudin E.Warfarin |
B. Fondaparinux |
|
|
A 20 year old man was punched in the throat 3 hours ago at a party. He is now complaining of severe pain, difficulty swallowing, has a hoarse voice and had has some haemoptysis.What is your next step in his management? A. Awake Fibreoptic Intubation B. CT scan for laryngeal fractures C.Direct laryngoscopy after topicalising with local anaesthetic D. Nasopharyngoscopy by an ENT surgeon E. Soft tissue xray of the neck |
D. Nasopharyngoscopy by an ENT surgeon |
|
|
What gestation to monitor uteroplacental flow in lady having coiling? A. 20 weeks B. 24 weeks C. 28 weeks D. 32 weeks E. 36 weeks |
B. 24 weeks |
|
|
A nulliparous woman in labour for 8 hours with epidural analgesia has a fever 37.6 degrees. The most likely reason for this is A.altered thermoregulation B.chorioamnionitis C.urinary tract infection D.inflammatory response E.neuraxial infection |
D.inflammatory response |
|
|
What is not an element of ChildPugh score? a.GGT b.Albumin c.Bilirubin d.INR e.Encephalopathy |
A |

