![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
45 Cards in this Set
- Front
- Back
|
What tissues are melanocytes found in? |
skin (DOI) uveal tract (choroid and iridial) stria vascularis of the inner ear leptomeninges retinal pigment epithelium (posterior layer of the retina)
|
|
|
Where are melanocytes derived from? |
NEURAL CREST CELLS!!!
All melanocytes come from here EXCEPT: retinal pigment epithelium comes from diencephalic neuroepithelium |
|
|
Syndromes due to death of melanocytes include:
1. Vogt-Koyanagi-Harada:
2. Alezzandrini Syndrome:
Describe these |
1. Vogt-Koyanagi-Harada: vitiligo, aseptic meningitis, otic involvement, severe uveitis, poliosis
2. Alezzandrini Syndrome: ONE SIDED --> unilateral poliosis, unilateral deafness, unilateral degenerative retinitis |
|
|
Where are melanocyte stem cells located? |
Melanocytic stem cells are located in the bulge of the hair |
|
|
How do melanocytes migrate? Which melanocytes are most affected in errors of migration? What directs proper migration? |
Melanocytes migrate in a DORSOLATERAL manner
Mutation in KIT can interfere with proper migration
Melanocytes on the anterior aspect of the body have the furthest to travel and thus are most affected by errors in migration |
|
|
How does chronic sun exposure affect melanocytes? |
Increases the density of melanocytes |
|
|
Errors in melanocytic migration include:
Piebaldism and Wardenberg syndrome. What gene mutations are affected? |
Piebaldism: KIT (need instructions in a KIT to make a PIE)
Wardenberg: your WARDrobe consists of mittens and socks, PACK your MITTENS, PACK your SOX
Wardenberg 1: PAX3 Wardenberg 2: MITF, SLVG Wardenberg 3: PAX3 Wardenberg 4: SOX10, EDN3 |
|
|
Errors in melanocytic migration include:
Piebaldism and Wardenburg syndrome. What are the characteristics of these diseases? |
Piebaldism: depigmented patched on central body and extremities with a white forelock
Wardenberg 1: PAX3, white forlock, heterochromic irides, DYSTOPIA CANTHORUM*
Wardenberg 2: MITF, SLVG, same as 1 except NO dystopia canthroum, includes deafness (mittens cover ears)
Wardenberg 3 (klein wardenburg syndrome): PAX3, similar to 1, includes limb abnormalities*
Wardenberg 4 (shah wardenburg syndrome): SOX10, EDN3, white forelock, heterochromic irides, HIRSHPRUNGS disease
**remember Marie's macarena dance for this!! |
|
|
Why is hirschprungs disease present in wardenburg syndrome 4? |
Wardenberg syndrome 4 has mutations in SOX and in EDN3 --> endothelin 3 is required for maturation of melanoblasts and ganglion cells, hence the findings of Hirshsprings disease (aganglionic megacolon) |
|
|
When are melanocytes present in the epidermis? When do they start to produce melanin? |
Melanocytes are present at 7 week
Melanin production starts at 12 weeks (beauty week!) |
|
|
By birth, most melanocytes that were in the dermis have migrated to the DEJ or have died off. What mutation can lead to dermal melanocytic survival and proliferation? |
GNAQ |
|
|
What gene is implicated in uveal melanomal? |
GNAQ |
|
|
Persistent dermal melanocytes can lead to... |
Mongolian spots, nevus of Ota, blue nevus |
|
|
Ratio of melanocytes in basal layer? Epidermal melanin unit? |
1:10 melanocytes to basal cells
1:36 dendritic unit |
|
|
Stimulation of melanocytes occurs by what? |
FGF IL-1 KIT UVR |
|
|
Stimulation of melanocytes occurs by FGF, IL-1, KIT and UVR... what do they all stimulate? |
MITF, which increases tyrosinase and TYRP1/2 |
|
|
What inhibits melanosomes? |
TGFB, IL-1a, IL-6, TNF-a, INFB, direct suppression of tyrosinase |
|
|
Melanocytes transport melanosomes to keratinocytes via their dendritic processes. What is a melanosome? |
Melanosomes are intracellular organelles, similar to lysosomes, that synthesize and store melanin |
|
|
What melanosome characteristics are responsible for the color of someone's skin? |
1. Type of melanosome-- I-IV
2. Size-- 0.3 to 0.5 microns for light skin, 0.5 to 0.8 microns for dark skin
3. Distribution-- lighter skin types tend to have 2-10 smaller melanosomes grouped together, darker skin types singly dispersed and larger melanosomes
4. Rate of degredation-- light skin types will degrade them by the mid stratum, darker skin types will not degrade them until the stratum corneum
5. Number of melanosomes
**note- number of melanocytes same regardless of skin type |
|
|
Immediate or delayed darkening/erythema with UVA vs UVB? |
UVA (ATE)-- immediate darkening (oxidation of pre-existing melanin, mc in darker pigment), later erythema
UVB (BET)-- immediate erythema, delayed tanning |
|
|
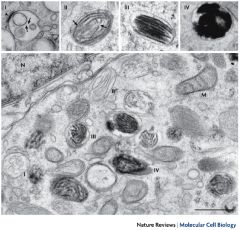
There are 4 types of eumelanosomes, what are they? |
I: spherical vacuoles with amorphous content, TYR negative
II: becomes elliptoid with lamellae and vesiculoglobular bodies, TYR +
III: melanization begins wtih vesiculoglobular bodies, TYR ++
**pheomelanosomes are similar, but no lamellae and melanization occurs both within and outside the vesiculoglobular bodies |
|
|
What is the major matrix protein in eumelanosomes? |
gp100/PMEL17
|
|
|
What stains the major matrix protein in eumelanosomes (gp100/PMEL17)? |
HMB45 |
|
Name these: |
|
|
|
Gene defect in Hermansky-Pudlak type 1? Features? |
HPS1
hypopigmented skin, hair and eyes and platelet storage problems --> bleeding diathesis
most of the life threatening manifestations occur in adulthood --> progressive pulmonary fibrosis (MCC death**), granulomatous colitis, cardiomyopathy, renal failure
5 P'S --> puerto rican, pooper (colitis), pulmonary fibrosis, platelets (bleeding) |
|
|
What is the most common cause of death in hermansky pudlak? |
pulmonary fibrosis
|
|
|
What is the gene defect in Hermansky Pudlak type 2? Features? |
ADTB3A
hypopigmented skin, hair and eyes and platelet storage problems --> bleeding diathesis, same as 1, but you can get more infections with 2
most of the life threatening manifestations occur in adulthood --> progressive pulmonary fibrosis (MCC death**), granulomatous colitis, cardiomyopathy, renal failure
5 P'S --> puerto rican, pooper (colitis), pulmonary fibrosis, platelets (bleeding) |
|
|
What is absent in Hermansky Pudlak 4? |
What ever it is.... it will be a test question, so figure it out!! |
|
|
mutation decreasing KIT? Increasing KIT? |
Decrease KIT-- piebaldism
Increase KIT-- mastocytosis |
|
|
What gene is mutated in Chediak Higashi? Features? |
LYST
remember, chediak higashi is in cats (LYNX)
Features- silver hair, nystagmus, severe immunosuppression, photophobia |
|
|
How does melanin migrate to the tip of the keratinocyte? |
Rab27 (gRabs the melanin) binds to the melanosome, which binds to melanophilin
When melanophilin is boud to myosin, it can bind to microtubules
Dynactin is what bridges the melanosome to kinesin (for anterograde movement) or dynein (for retrograde movement) **kinesin/kinetics move you forward |
|
|
How does UVR stimulate melanosome migration? |
UVR exposure increases kinesin production and activity over dyenien --> UVR increases anterograde movement into keratinocytes!!!
Also increases PAR-2 expression from keratinocytes, which is responsible for phagocytosis of melanosomes by keratinocytes |
|
|
What is the gene defect in Griscelli syndrome type 1? Features? |
MYO5
silvery gray hair, primary neurologic impairment without immune defects (whereas all patients with GS2 have immune defects)
'muscle head'--> myo muscle, head neuro impairment** |
|
|
What is the gene defect in Griscelli syndrome type 2? Features? |
RAB27A
silvery gray hair, neurologic impairment WITH immune defects (whereas all patients with GS1 do NOT have immune defects)
lots of IMMUNE DEFECTS, esp lymphophagocytic syndromes** |
|
|
What are the two types of melanin? How is melanin synthesized? |
Eumelanin (black/brown, Elliptical melanosomes)
Pheomelanin (red/yellow, sPherical melanosomes) |
|
|
What is the rate limiting step of melanin synthesis? |
conversion of tyrosine to DOPA via tyrosinase |
|
|
If body lacks copper, how does this affect melanin synthesis? |
TYROSINASE is a copper dependent enzyme |
|
|
These drugs are competative inhibitors of tyrosinase... |
hydroquinone, L-phenyalanine |
|
|
OCA 1-4, what are the gene defects? |
OCA1a: tyrosinase absent --> complete pigment loss
OCA1b: tyrosinase reduced --> partial activity of yellow pigment bc less TYR is needed for pheomelanin, also temperature sensitive bc abnormal tyrosinase enzymes loses its activity at >35C therefore melanin synthesis doesn't happen in warmer areas (Siamese cats!!)
OCA2: P gene (regulates melanosome pH)
OCA3: TYRP1--> no eumelanin produced RUFUS
OCA4: mutation in MATP/SLC45A2 |
|
|
How are the oculocutaneous albinism disorders inherited?
|
all are autosomal recessive |
|
|
Presentation of OCA? |
OCA1a: absent TYR --> white hair, white skin, blue eyes at birth, strong predisposition to skin cancer, reduced visual acuity
OCA1b: decreased TYR --> partial activity of yellow pigment (less TYR is needed to make pheomelanin) so diverse presentation
OCA2: P gene --> hypopigmentation, prader willi, angelman
OCA3: TYRP1--> RUFUS!!! think of that little black kid who was white because of the disease
OCA4: MATP --> variable |
|
|
What cancers are associated with ocular cutaneous albinism? |
SCC > BCC >MM |
|
|
a-MSH secreted by keratinocytes affects melanin production how? |
stay with me here...
a-MSH stimulated melanocytes to produce eumelanin by binding MC1R --> increases cAMP --> activates protein kinase A --> activates CREB --> activates MITF --> increases tyrosinase and TYRP1
|
|
|
If MC1R is mutated, makes gingers. Why?! |
If MC1R is mutated, DOP is unable to enter into eumelanin synthetic pathway, so it feeds into the pheomelanin pathway --> increased risk of melanoma, red hair, freckles, fair skin |
|
|
Defect in Griscelli syndrome type 3? Characteristics? |
Defect in melanosome migration
MLPH
cutaneous albinism and silverly hair ONLY
unlike type 1 that has neurologic impairment and type 2 that has immunologic impairment |

