![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
41 Cards in this Set
- Front
- Back
|
MC locations for lupus panniculitis? |
cheeks, shoulders, chest, upper back, outer thighs |
|
|
MC locations for a1-antitrypsin deficiency panniculitis? |
butt and hips |
|
|
MC location for erythema nodosum? |
anterior shins |
|
|
MC location for erythema induratum? |
calves |
|
|
Location erythema nodosum vs erythema induratum? |
EN is on the anterior shins EI is on the calves |
|
|
MC location of lipodermatosclerosis? |
wine bottle!! medial shins |
|
|
Septal panniculitis includes which entities? |
EN, a1AT, morphea profundus |
|
|
Causes of erythema nodosum? |
SHOUT BCG!!!
Sarcoidosis/sulfa/strep, histo, OCP/preg, UC, TB, Bechets, Chrons, GI (yersenia)
NODOSUM No cause is found in 30-50% of cases Drug (OCP, sulfa, minocycline, PCN( Oral contraceptives Sarcoidosis (Lofgren's syndrome) Ulcerative colitis Malignancy/microbiology (URI, strep, tb, yersinia, mycoplamsa, HSV, HBV, lymphomas) |
|
|
Lesions of EN re often bilateral and preceded by a prodrome of fever, malaise, leukocytosis and arthralgias. How long do they last? |
they DO NOT ulcerate they resolve spontaneously within 3-6 weeks new lesions continue to develop over a period of weeks to months |
|
|
What is a miescher granuloma? |
pathognomonic for EN, collection o fhistiocytes in radial array around vessels |
|
|
Treatment for EN? |
They will resolve spontaneously in 3-6 weeks
But, bed rest, elevation NSAIDS, ASA (avoid if presents with IBD), SSKI, IL or oral steroids, colchicine, antimalarials |
|
|
Dosing regimen and side effects of SSKI? |
5 drops TID, increase by 1 drop per dose per day up to 30 drops TID, once controlled, taper over 2-3 weeks
SE: acute--> nausea, bitter taset, salivation, urticaria, vasculitis, angioedema chronic--> hypothryoidism > hyperthyroidism, enlargement of salivary and lacrimal glands, acneiform eruption, iododerma |
|
|
Erythema nodosum migrans? |
same as erythema nodosum, except UNILATERAL
less painful and more chronic than EN (course is months to years)
TX: SSKI |
|
|
Alpha 1 antitrypsin deficiency, gene found on which chromosome? How does it present? |
Chromosome 14, found in PIZZ individuals (PIMM individuals are normal)
Presents with multiple painful subQ nodules (fluctuant, ulcerate and drain) on butt and lower back, will also see LUNG issues and LIVER issues |
|
|
Which panniculitic nodules can ulcerate and drain? |
panniculitis of alpha 1 antitrypsin deficiency |
|
|
Histopathologic progression of alpha-1 antitrypsin deficiency? |
early septal panniculitis with neutrophilic infiltrate
later stages include septal and lobular infiltrate with lymphocytes, foam cells and fibrosis |
|
|
Treatment of alpha-1 antitrypsin deficiency? |
doxy 200mg BID x 3 months for mild disease
dapsone, colchicine, IV a-1
liver transplant is curative |
|
|
Lobular panniculitis includes:
|
subcutaneous fat necrosis of the newborn sclerema neonatorum postersteroid panniculitis pancreatic fat necrosis sclerosing panniculitis cold panniculitis cytophagic histiocytic panniculitis |
|
|
healthy, full term infant born via c section, at birth, notice firm subcutaneous nodules on cheeks, buttocks and back. Workup? |
This is subcutaneous fat necrosis of the newborn
Baby is HEALHTY
Most times related to some sort of fetal distress: birth trauma, cord accidents, meconium aspiration, C section, placenta previa, neonatal asphyxiation, hypothermia
Get a calcium level! can be associated with hypercalcemia, so you need to get levels on these little guys for the next 4 months
this will spontaneously regress in a few months |
|
|
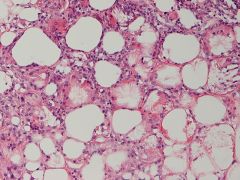
Histology of subcutaneous fat necrosis of the newborn? |
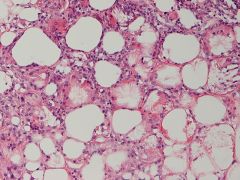
Needle shaped clefts arranged in radial fashion within adiposites
Crystals are formed from dissolved TG
Can have focal calcium deposition |
|
|
fat necrosis of the newborn- see needle shaped clefts
can have focal calcium deposition in SQFNNB, calcs are rare in sclerema neonatorum
path looks the same as sclerema neonatorm, so get the clinical! |
|
|
Pull baby out, he's cold and hypoglycemic, put him in the NICU and within 3 days he starts developing symmetric, diffuse induration on the legs spreading upwards to the truck. Work up? |
Thsi is sclerema neonatorum- presents in first week of life
Cold and hypoglycemia? sepsis. Other associated illnesses: sepsis, pneumonia, diarrhea, dehydration, intestinal obstruction or congenital heart disease
presents in first week of life, a/w high morbidity and mortality |
|
|
What is post steroid panniculitis? |
rare complication of rapid systemic steroid WITHDRAWAL in children
see firm, red nodules/plaques on cheeks, arms trunk within 1-40 days
path looks identical to SQFNNB
resolves spontaneously within weeks or when steroids are started again |
|

|
Pancreatic panniculitis- lobular panniculitis with 'ghost cells' (saponification of fat) |
|
|
49 year old male smoker comes in to the ER with diffuse jaundice, periumbilical abdominal pain, 20 pound weight loss over the past 2 months, fever and tender, red subcutaneous nodules on pretibial legs and buttocks. Derm is paged for the nodules. What are we worried about? |
20# weight loss and fever, periumbilical pain, diffuse jaundice? Sounds like pancreatic cancer to me. Now has pancreatic panniculitis on legs and butt (a/w pancreatitis and carcinoma)
Thought to be d/t release of trypsin, lipase, amylase by disease pancreatitis --> trypsin damages the vasculature allowing lipase to enter fat and necrose it |
|

|
Lipodermatosclerosis! aka sclerosing panniculitis.
occus in middle aged and older women with vascular insufficiency, mc on medial LE
venous stasis --> ischemia and infarction of subcutaneous fat |
|
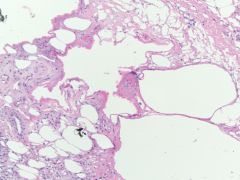
biopsy from a woman with 'bilateral cellulitis'. What is this finding called? |
Lady has venous stasis change and resulting sclerosing panniculitis (lipodermatosclerosis)
membranous fat necrosis with lipomembranous change (feathering) |
|
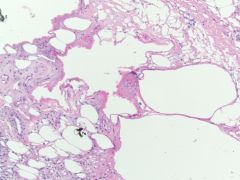
This can be found in which conditions? |
LIPOMEMBRANOUS CHANGE
venous insufficiency diabetes erythema nodosum nodular vasculitis infective panniculitis pancreatic panniculitis sarcoidosis morphea profundus |
|
|
What is cold panniculitis? |
Erythematous and indurated plaques and nodules found in infants and young children after exposure to cold or cold substances, secondary to higher saturated to unsaturated fatty acid ratio in infants
resolve in 1-3 weeks |
|
|
Lupus erythematous panniculitis (lupus profundus) can be seen in either localized cutaneous or systemic lupus. Most common locations? |
head, UPPER ARMS, buttocks, thigh
deep, firm, asymptomatic, single or multiple subQ nodules |
|
|
SLE patient develops several deep, firm, asymptomatic subQ nodules on her cheeks bilaterally, what is this? What do we need to check for? |
Lupus panniculitis (lupus profundus) most likely, BUT, need to rule out subcutaneous panniculitis like T cell lymphoma, so STAIN IT!
more indolent form is CD8+, BF1+ and should be classified as subcutaneous panniculitis like T cell lymphoma
more aggressive form is CD8+ and BF- |
|
|
Cytophagic histiocytic panniculitis is a chronic recurrent disease of immune dysregulation. Develops in association with what infections and a/w which malignancies? |
Infections: CMV, EBV, HIV, various bacterial
Malignancies: subcutaneous panniculitic T cell lymphoma, angiocentric T cell lymphoma |
|
|
Histiocytes stuffed with lymphocytes, erythrocytes, platelets, neuts aka beanbag cells are pathomneumonic for... |
cytophagic histiocytic panniculitis |
|
|
Calciphylaxis has an uncertain pathogenesis, but is almost exclusively occurs in what population? |
patients with ESRD, often undergoing dialysis --> abnormality of calcium/phosphate matabolism followed by calcification of the vasculature in subcutaneous fat |
|
|
How does calciphylaxis present? |
unilateral or bilateral pruritic and painful livedoid, violaceous plaques and nodules on legs
morbility and high mortality of up to 60% |
|
|
Labs to check when you suspect calciphylaxis? |
calcium phosphate product > 60-70mg/dL
strangely, most patients have normal calcium and phosphate |
|
|
Treatment for calciphylaxis? |
phosphate binders, cinacalet, IV sodium thiosulfate, parathyroidectomy |
|
|
Type II reactions typically occur in lepromatous leprosy and can be subdivided into three clinical variants:
|
erythema nodosum leprosum
erythema polymorphous-like reaction
Lucio's phenomenon (mainly considered type II reaction, but may be classified as type III)
Attending to the clinical and histopathological manifestations, leprosy reactions may be separated in 2 or 3 different variants: reverse reaction (type I), erythema nodosum leprosum (type II), erythema polymorphous (type II) and Lucio's phenomenon, mainly considered a type II reaction, but sometimes designated type III. |
|
|
treatment of erythema nodosum leprosum? |
thalidomide |
|
|
What is Lucio's Phenomenon? |

Type II/III (depending on what you read) reaction to lepromatous leprosy, see crops of painful hermorrhagic infarcts forming crusted ulcerations |
|

type X hypersentisitivity? |
Erythema induratum/nodular vasculitis- likely a type IV hypersensitivity cell mediated response
look for TB with PPD or quantiferon gold
Will see fat necrosis + vasculitis |

