![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
58 Cards in this Set
- Front
- Back
|
pathogenicity |
ability to cause disease by evading or overcoming the host defenses |
|
|
virulence |
the extent to which the microorganism is pathogenic |
|
|
virulence factors |
molecules produced by pathogens that contribute to their pathogenicity |
|
|
portals of entry for pathogens |
1. cracks in mucous membranes 2. skin, abrasions and cuts 3. parenteral route |
|
|
surgical sites |
can provide routes to bypass traditional means for pathogens as surgical sites open up cavities |
|
|
preferred portal of entry |
some microorganisms have a preferred portal of entry, only capable of causing disease via a specific route ex. stds |
|
|
tropism |
pathogens with a preferred type of cell to infect |
|
|
determinants of tropism |
1. distribution of cell receptors for microbes 2. accessibility of correct host cell types 3. requirement for appropriate cellular elements that will allow the microbe to grow 4. physical and innate defences at the site of infection, strong immune system= no infection 5. other microbes may be competing |
|
|
some pathogens do not have to penetrate the body's tissues to cause disease |
microbes can produce exotoxins that get into cells through proteins that attaches to the host cell, spreading the disease process |
|
|
process of infection |
1. adhere to host 2. proliferate and multiply 3. break off and infect new host |
|
|
process of infection indepth look of proliferation |
during proliferation, infected cells also: 1. invade host cells 2. avoid destruction by producing toxins to kill WBC 3. share virulence factors |
|
|
Adherence |
first step towards establishment of infection facilitated by structures on pathogens called adhesins or ligands and structures on the host cells that recognize and bind with these "receptors" |
|
|
most adhesins are |
glycoproteins are or lipoproteins |
|
|
most receptors are |
sugars like mannose |
|
|
factors that help the bacteria evade or penetrate host defenses Capsules |
Glycocalyx; initially prevents the phagocyte from recognizing adn ingesting bacteria bacteria can produce capsules in the right environmental conditions, sugars, etc. |
|
|
factors that help the bacteria evade or penetrate host defenses cell wall components Fc receptors |
Fc receptors on microorganism binds the Fc portion of antibodies produced to the capsule of bacteria. Phagocytes also have Fc receptors and are looking to bind the Fc portion on organisms that are opsonized. Fc portion of the molecule is not available for binding to the phagocyte |
|
|
factors that help the bacteria evade or penetrate host defenses cell wall components M protein |
in streptococcus pyogenes heat an acid resistant protein in the cell wall that allows attachment of the bacteria epithelial cells and inhibits phagocytosis, it holds itself away from phagocyte wit protein M, which acts like a stick |
|
|
factors that help the bacteria evade or penetrate host defenses cell wall components mycolic acids |
in mycobacterium tuberculosis, waxy substances in cell walls that make the bacterium resistant to digestion inside the phagocyte |
|
|
factors that help the bacteria evade or penetrate host defenses biofilms |
community of bacteria, often surrounded by shared glycocalyx reduces antibiotic penetration, increasing resistance |
|
|
factors that help the bacteria evade or penetrate host defenses exoenzymes leucocidin |
destroys WBC cells |
|
|
factors that help the bacteria evade or penetrate host defenses exoenzymes kinase |
break down fibrin and dissolve clots formed by the body to isolate infection |
|
|
factors that help the bacteria evade or penetrate host defenses exoenzymes hemolysin |
breakdown red blood cells |
|
|
factors that help the bacteria evade or penetrate host defenses exoenzymes coagulase |
clots: converts fibrinogen to fibrin, clot can wall the bacteria off from host defenses ex. staphlycoccus aereus not epidermidis |
|
|
factors that help the bacteria evade or penetrate host defenses exoenzymes collagenase |
break down collagen, a connective tissue |
|
|
factors that help the bacteria evade or penetrate host defenses exoenzymes |
destroy plasma membrane |
|
|
factors that help the bacteria evade or penetrate host defenses exoanyzmes proteases |
inactivate antibodies and other body proteins, like IgA protease |
|
|
factors that help the bacteria evade or penetrate host defenses
invasins |
surface proteins on some bacteria which activate actin, the cytoskeleton on eukaryotic cell, rearranging and facilitating bacterial engulfment into the host cell |
|
|
other use of invasins |
some bacteria use their invasins to move from one host cell to another, moving laterally and from the outside in. |
|
|
factors that help the bacteria evade or penetrate host defenses super antigens |
also called type 1 exotoxins protein antigens that stimulate a large immune response, activating 20% of T cells |
|
|
super antigens result |
result in excessive release of cytokines due to binding to MHC II and TCR which results in nausea, fever, diarrhea, shock, death |
|

|
L |
|
|
factors that help the bacteria evade or penetrate host defenses toxins |
1. often primary virulence factor 2. usually proteuns that can produce fever, cause heart failure, diarrhea, edema or shock 3. can destroy cells as well as inhibit protein synthesis leading to cell death |
|
|
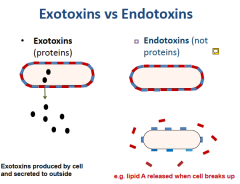
endotoxin |
something that contributes to the structure of the bacteria ex. LPS, Lipid A portion |
|
|
exotoxins |
ex. superantigens an extra protein that is made by bacterium to affect cells other than itself heat sensitive |
|
|
L |
|
|
endotoxins effects |
causes chills, fevers, weakness, aches, shock adn death activates the blood clotting system (DIC- disseminated intravascular coagulation) |
|
|
Shock |
life threatening loss of blood pressure |
|
|
septic shock |
if caused by bacteria |
|
|
endotoxic shock |
if caused by gram - bacterium |
|
|
genes for exotoxins |
are carried on bacteriophages or plasmids |
|
|
3 types of exotoxins |
1. cytotoxins 2. neurotoxins 3. enterotoxins |
|
|
body produces what to neutralize exotoxins? |
antitoxins |
|
|
factors that help the bacteria evade or penetrate host defenses secretion systems |
type III secretion apparatus allows bacteria to inject proteins into a host cell, killing or altering it |
|
|
pathogenicity island |
a chromosomal region in some bacteria, esp. Gram - have genes encoded for pathogenic characteristics like that of a type III secretion apparatus |
|
|
factors that help the bacteria evade or penetrate host defenses antigenic variation |
pathogens have antigens on their surfaces to which B cells produce antibodies some pathogens change the makeup of their antigens= immune system sees them now as new pathogens |
|
|
factors that help the bacteria evade or penetrate host defenses intracellular growth obligate intracellular bacteria |
can only grow inside of host cells, often in a protected vacuole |
|
|
factors that help the bacteria evade or penetrate host defenses intracellular growth facultative intracellular bacteria |
bacteria that can multiply outside of host cells, but often use intracellular growth as a means of evading host defenses |
|
|
Bacterial mutation |
mutate or take up small pieces of DNA that can change their virulence pieces of DNA can either be integrated into the bacterial chromosome or exist as free floating genes in the bacterial cell advantage for pathogens |
|
|
pathogenicity islands and being more efficient |
more efficient to have them packed closely together to be transferred as a unit between bacteria |
|
|
conjugation |
transferral of plasmids containing genes for virulence or antibiotic ressitance |
|
|
transduction |
acquisition of genes for toxin production |
|
|
transformation |
acquiring gene for toxin, capsule production, etc. |
|
|
Plasmids |
small circular DN molecules separated from main bacterial chromosome |
|
|
R factro |
responsible for transferring the genes for antibiotic resistance |
|
|
BACTERIOPHAGES |
viruses which infect specific bacteria transfer genes by transduction |
|
|
viruses pathogenic effects |
most effects caused by inflammation and activation of the immune system, producing disease |
|
|
viral pathogenesis |
cytopathic effects: alteration of cells 1. killing or damaging of host cell 2. different strains of virus cause different CPE |
|
|
syncytiu formation |
1. infected cells fuse to from giant cell with many nuclei 2. giant cell dies when virus use up all building material and cause necrosis of tissue 3. permits viral multiplication w/o exposing virus to antibodies |

