![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
76 Cards in this Set
- Front
- Back
|
What is occlusion? |
blockage beyond = ↓O2 = ischemia |
|
|
What does ischemia do to the retina? |
Ischemia causes the retina to lose transparency • Loss of red-reflex |
|
|
Where in the retina doesn't lose its transparency due to ischemia? |
• Except macula – underlying choriocapillaris • “Cherry-red spot” |
|
|
What results following a total infartion? |
• Following total infarction – retinal tissue dead • No release of vasoformative agents (∴minimal risk of neovascular-related complications (5% of CRAO, vs. 50% of CRVO)) |
|
|
How do occlusion arise? |
• Thrombus • Embolus |
|
|
The ophthalmic artery is the first branch from which artery? |
Internal carotid artery |
|
|
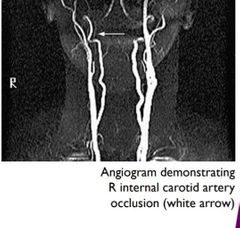
How can occlusion risk arise from the internal carotid artery? |
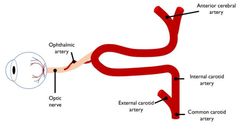
Matter present in the ICA (e.g. emboli) more likely to enter OA |
|
|
Name the types of retinal emboli RAO. |
• Cholestrol • Calcific • Fibrin-platelet |
|
|
What is cholesterol retinal emboli? |
• Cholesterol (Hollenhorst plaque): intermittent, (multiple) bright, highly reflective. • Often found at vessel bifurcations. • Rarely cause total obstruction. |
|
|
What is a calcific retinal emboli? |

• Aortic/carotid plaques/calcified heart valves. • Single, white, non-shiny. Often at/near to disc. • Often cause permanent occlusion. |
|
|
What is a Fibrin-platelet retinal emboli? |

Dull, grey, elongated.
Often multiple. |
|
|
What causes Fibrin-platelet retinal emboli? |
• Caused by atherosclerotic changes in the heart and coagulopathies.
• Can fill entire lumen –cause transient occlusion (amaurosis fugax) or complete obstruction. |
|
|
What is Giant cell (temporal) Arteritis? |
• Inflammation of blood vessels around temple / scalp (auto-immune? Age-related; ♀>♂) • Interrupts blood flow around head |
|
What does Giant cell (temporal) Arteritis more commonly cause? |

more commonly causes anterior ischaemic optic neuropathy (AION) Stoke of the optic nerve |
|
|
What are the symptoms of Giant cell (temporal) Arteritis? |
• Headache • Scalp tenderness • Jaw claudication • Weight loss |
|
|
What is Amaurosis Fugax? |
• Painless, temporary loss of vision (monocular) – few minutes. •Gradual recovery. • “Curtain coming down over vision” |
|
|
What can Amaurosis Fugax indicate? |
• Precursor to occlusion • Often associated with GCA – precedes actual infarction of ON |
|
|
How do you manage Amaurosis Fugax? |

• Refer for cardiovascular / neurological work-up
• Risk of occlusive disease, stroke etc.
• Check for Sx of GCA |
|
|
State the other causes of occlusion. |
• Giant cell (temporal) Arteritis • Blood disorders • Retinal migraine • Severe raised IOP |
|
|
What are the categories for retinal artery occlusion? (Location) |
• Central Retinal Artery (complete retina) (CRAO) • Branch Retinal Artery (partial retina) (BRAO)
• Cilioretinal Artery Occlusion |
|
|
What is Central Retinal Artery (CRAO)? |
a disease of the eye where the flow of blood through the central retinal artery is blocked (occluded) |
|
|
What are the signs and symptoms of CRAO? |
• Sudden onset, profound, unilateral, loss of vision
• Painless (except GCA)
• RAPD – profound (amaurotic* pupil) |
|
|
What would be seen with CRAO? |
• Retinal vessels: attenuated, segmented blood column (box-carring)
• Retina: pale, opaque, oedematous, cherry-red macula |
|
|
What is the treatment for CRAO 24-48/24 after onset? |
• Supine position - ↑ ocular perfusion
• Anterior chamber paracentesis (results variable)- ↓IOP • Embolysis • Thrombolysis • Vasodilator
• Rebreathing / carbogen (95% O2) - Vasodilate (raise CO2levels)- Also helps retard ischemia (↑O2)
• Ocular massage - collapse artery (10s) followed by release (5s) – build pressure to manually dislodge embolism |
|
|
What is the treatment for CRAO >24-48/24 after onset? |
• Refer to ophthalmology for review • Monitor over 3-4/52 for signs of neovascularisation (esp. anterior segment) • Systemic workup (esp. haematological) |
|
|
What is the prognosis for CRAO? |
• POOR (retinal infarction) • Retinal oedema / haze & cherry-red spot ↓over few days/weeks • Arterial attenuation remains • Optic/retinal (RGC) atrophy • RPE changes |
|
|
What is the CRAO cilioretinal artery? |
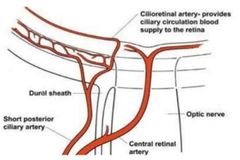
• Extra blood vessel (not part of CRA)
• Originates from Short Posterior Ciliary Artery |
|
|
What does the ciliretinal artery do in a case of CRA occlusion? |

• if CRA occluded, still provides blood to portion of macula • “Spare power supply” • Functionally blind in eye? or • Small central island of vision? |
|
|
What are the causes of CRAO Cilioretinal artery occlusion? |
• Isolation: vasculitis (younger Px)
• Non-ischemic CRVO
• Anterior ischemic optic neuropathy AION |
|
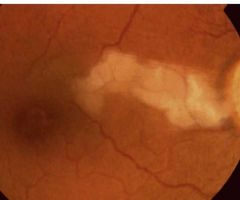
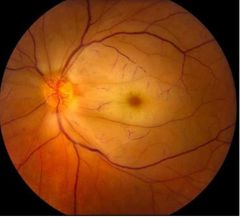
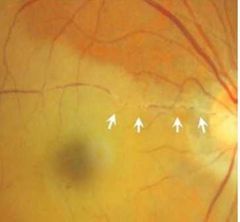
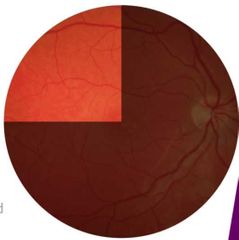
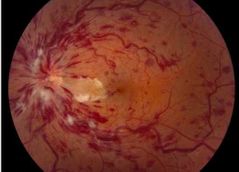
What is this? |
CRAO Cilioretinal artery occlusion Isolation: vasculitis |
|
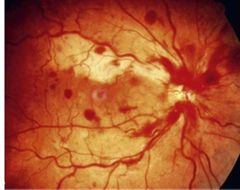
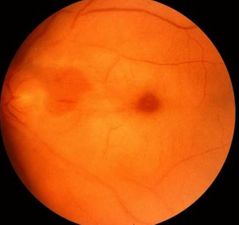
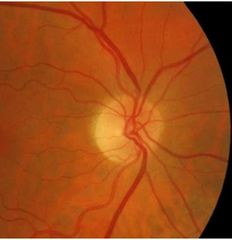
What is this? |
CRAO Cilioretinal artery occlusion Non-ischemic CRVO |
|

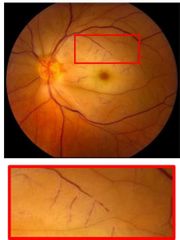
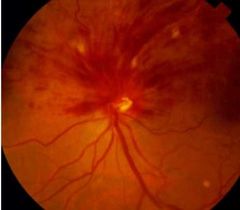
What is this? |
AION • Posterior Ciliary Artery supplies ON also • Poor prognosis (due to AION) |
|
|
What would be seen with CRAO Cilioretinal artery occlusion? |
• Sudden, profound central scotoma • Retina: localised oedema and clouding to region supplied by cilioretinal artery |
|
|
What are the signs and symptoms of Branch Retinal Artery occlusion? |
• Sudden onset, profound, unilateral, altitudinal/sectoral scotoma • VA – variable, depends on location of occlusion • RAPD – usually |
|
|
What would be seen with Branch Retinal Artery occlusion? |

• Retinal vessels: attenuated, segmented blood column (box-carring)
• Retina: pale, opaque, oedematous in region supplied post-occlusion (embolus may be visible) |
|
|
What is the treatment/management for Branch Retinal Artery occlusion? |
• No therapy of clinical value
• Refer for:- Systemic work-up - 3/12 review to assess recovery- neovas |
|
|
What is the prognosis for Branch Retinal Artery occlusion? |
• Generally poor • Visual field defect permanent • Affected artery remain attenuated • If artery reopens – subtle/absent signs on ophthalmoscopy |
|

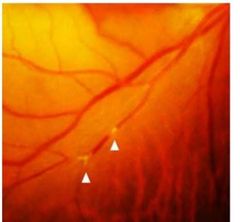
What is this? |

Astmptomatic emboli |
|
|
If an asymptomatic emboli is seen on fundoscopy, what does this indicate? |
Px at significant risk of developing complications (CRAO, BRAO, stroke…)
• Plaque / embolus had to come fromsomewhere… |
|
|
What should you do if an asymptomatic emboli is seen on fundoscopy? |
Urgent referral for system evaluation |
|
|
What is Ocular ischemic syndrome (OIS)? |
is a rare, but vision-threatening condition associated with severe carotid artery occlusive disease (stenosis or occlusion) leading to ocularhypoperfusion. |
|
|
What are the symptoms of Ocular ischemic syndrome (OIS)? |
• Gradual VA↓
• Occasional (peri-)ocular pain (~40%)
• Persistent after-images - ↓VA in increased illumination & slow adaptation (↓PRP turnover) |
|
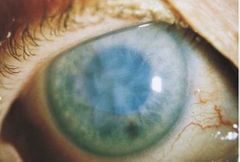
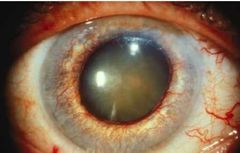
With Ocular ischemic syndrome (OIS), what would be seen on the anterior eye? |

• Episcleral (vein) injection • ∴ ↑ IOP
• Corneal oedema • Aqueous flare • Iris atrophy (mid-dilated, poorly reactive pupil) • Rubeosis iridis (90%) - Progress to neovascular glaucoma |
|
|
With Ocular ischemic syndrome (OIS), what would be seen on the posterior eye? |

• Arterial narrowing, venous congestion • Haemorrhages, papilloedema, cotton wool spots - ∴ neovascularisation • Macular oedema |
|
|
What is the prognosis for Ocular ischemic syndrome (OIS)? |
• VA dependent on how early Tx’d (if good at initial presentation, better prognosis) • 25% progress to LP by 12/12 • 5-year mortality: 40% (MI 67%; stroke 19%) |
|
|
What is the treatment for Ocular ischemic syndrome (OIS)? |
• Anterior eye: topical steroids (if at all) • Posterior eye: intravitreal injections / anti-VEGF • Carotid surgery |
|
|
How can Retinal venous occlusion occur? |

• ↑ artery thickening = ↓ vein • Constriction = ↑ flow & turbulence • Endothelial damage & thrombus pre-disposition |
|
|
How is Retinal Venous Occlusion defined by location? |
• Central Retinal Vein Occlusion (CRVO) • Branch Retinal Vein Occlusion (BRVO) • Hemiretinal BRVO • Peripheral BRVO • Macular BRVO • Major branch at disc BRVO |
|
|
How is Retinal Venous Occlusion defined by type? |
• Ischaemic • Non-ischaemic |
|
|
Where is the most common location for venous occlusion? |
• A:V crossings (esp. with nipping)
• Most common: superior-temporal quadrant |
|
|
Describe the process leading to a venous occlusion. |
• Blockage → ↓ blood outflow = ↑ venous pressure
• Lower pressure gradient between arteries, capillaries and veins = blood stagnation & hypoxia
• Damages endothelium; leakage of blood |
|
|
What are the risk factors for retinal venous occlusion? |
• Age (50% > 65yrs) • HT/↑ blood pressure • Hyperlipidaemia, DM…
• Thyroid dysfunction • ↑ IOP • Oral contraceptive pill • Smoking?? |
|
|
What are the 2 main complications to retinal venous occlusion? |
• Cystoid Macular Oedema (CMO)
• Neovascular (“100 Day”) Glaucoma • Rubeosis Iridis |
|
What is the aetiology for Cystoid Macular Oedema (CMO)? |
• ↑ hydrostatic pressure within retina (due to occlusion)
• deteriorated endothelium…
• Inflammatory response (VEGF; C-reactive proteins)…
• Cell death = impaired Blood-Retinal Barrier… → Oedema |
|
|
What are the presenting symptoms of Cystoid Macular Oedema (CMO)? |
• Blurred vision (=↓V/A)
• Metamorphopsia?
• Depends on extent of CMO |
|
|
What is the treatment for Cystoid Macular Oedema (CMO)? |
• PRP* Grid Laser • Intravitreal steroids • Anti-VEGF |
|
|
What is the aetiology of Neovascular (“100 Day”) Glaucoma? |
• Severe, chronic retinal ischaemia
• VEGF released to ↑ retinal circulation
• Factors diffuse to anterior eye
• Promote new vessels on iris (NVI; rubeosis iridis) and into angle (NVA)
• Occludes angle & trabecular meshwork
→ Raised IOP |
|
|
What are the symptoms of Neovascular (“100 Day”) Glaucoma? |
• ASx if early (100-day glaucoma) • Time taken for vessels to grow
• Significant, relentless pain • Leading cause of enucleation in Western world |
|
|
How would you examine Neovascular (“100 Day”) Glaucoma? |
• Photography / Slit lamp assessment • Gonioscopy • Fluorescein angiography (FA) |
|
|
What should you NOT do to examine Neovascular (“100 Day”) Glaucoma? |
• Do NOT dilate!!! • Vessels start as small tufts at pupil margin • Grow radially
|
|
|
What would be the issue with the new vessels with neovascular glaucoma? |

• Fragile ∴ prone to haemorrhage→ Hyphaema |
|
|
What is the treatment for neovascular glaucoma? |
• PRP Grid Laser • Anti-VEGF • Experimental techniques - Laser-induced chorioretinal venous anastomsis |
|
|
What is NON-ischaemic CRVO? |
Nonischemic CRVO is the milder form of the disease.
Sudden onset, unilateral, moderate ↓V/A |
|
|
What might NON-ischaemic CRVO present with? |

• good vision • few dor, blot and flame hemorrhages • no relative afferent pupillary defect • good perfusion to the retina
→ slower transport of blood, but oxygenation retained ∴ non-ischemic |
|
|
What is the trratment for NON-ischaemic CRVO? |
• Low-dose aspirin?
• Discontinue oral contraceptives
• Check and Tx neovascular glaucoma (PRP)
• Monitor every 3-4/52 for 3/12 - 100-day glaucoma
• Discharge if stable / resolved in 24/12 |
|
|
What is Ischaemic CRVO? |
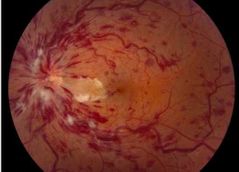
Sudden onset, unilateral, severe ↓V/A (CF) |
|
|
What would be seen with Ischaemic CRVO? |
• RAPD • Retinal veins: dilated, tortuous • Retina: - extensive dot - blot & flame haemorrhages - papilloedema - cotton wool spots |
|
|
What is the treatment for Ischaemic CRVO? |
• Prophylactic PRP • 1/12 reviews for 6/12 • Iris border and angle (prior to mydriasis) • Review up to 24/12 |
|
|
What is Papillophlebitis? |

• Optic disc vasculitis (inflammation of blood vessels)
• Rare
• Induces “secondary CRVO” - swelling of ON congests CRV |
|
|
In who does Papillophlebitis occur in? |
Occurs in younger (♀) Px (<50y.o. (20-35)) with no Hx of vascular disease. |
|
|
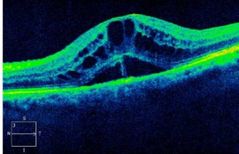
What would be seen with Papillophlebitis? |
• Mild blurring (esp. when waking – supine)
• No RAPD, enlarged blind spot
• OCT: Possible CMO • FA: Delayed transit; good perfusion • Often mis-Dx’d as papilloedema / optic neuritis |
|
|
What is the treatment for Papillophlebitis? |
• Corticosteroids to ↓ inflammation
• Anticoagulants (underlying coagulopathy?)
• If not treated promptly, CRVO and subsequent complications (CMO) likely |
|
|
What is Hemiretinal retinal vein occlusion? |
• Similar to CRVO (ischemic / non-ischemic)
• Occurs close to / at the ONH
• Less common |
|
|
What would be seen with Hemiretinal retinal vein occlusion? |
• ↓VA? (Depends on involvement of macular) • Retina: Occlusion localised to one hemisphere • VF: altitudinal defect |
|
|
What is Branch retinal vein occlusion (BRVO)? |
• 2-3x more common than CRVO • Localised blockage (disc, macula, peripheral) |
|
|
What are the signs and symptoms of branch retinal vein occlusion (BRVO)? |

• depend on location (macula (Sx) > periphery (ASx)) • ↓VA, metamorphopsia, scotoma? • Retina: localised findings, (haemorrhages, oedema, CW spots) • Ischemic if >5DD of non-perfusion on FA Good prognosis |

