![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
62 Cards in this Set
- Front
- Back
|
Macule
|
Flat, non-palpable lesion that differs from surrounding skin only by color <5mm
|
|
|
Papule
|

Solid, raised lesion, lesion less than 1cm in diameter
|
|
|
Nodule
|

Raised, palpable
Deeper in dermis Similar to papule but located deeper in the dermis or subcutaneous tissue; differentiated from papule by palpability and depth, rather than size |
|
|
Plaque
|

Raised, flat top
Larger than 1cm in diameter |
|
|
Pustule
|

Pus-filled papule
Circumscribed elevation of skin containing purulent fluid of variable character (i.e., fluid may be white, yellow, greenish or hemorrhagic) |
|
|
Vesicle
|

Fluid filled papule
Circumscribed, elevated, fluid-containing lesion less than 0.5 cm in greatest diameter; may be intraepidermal or subepidermal in origin |
|
|
Bulla
|

A cyst larger than 1cm in size
|
|
|
Cyst
|

Raised, fluid filled sac
|
|
|
Open Comedone
|

Blackhead
|
|
|
Closed Comedones
|

White Head
|
|
|
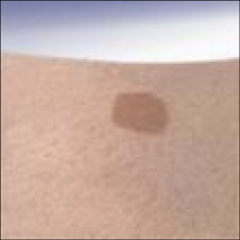
Tumor
|

A large nodule
Picture of NF |
|
|
Wheal
|

Edematous, slightly raised
Firm, edematous, flat topped papue or plaque resulting from infiltration of dermis with fluid that lasts <24hrs. Uticaria |
|
|
List secondary dermatologic terms
|
- scale
-crust (hemorrhagic or moist) - excoriated (scratched, rubbing) - oozing erosion ulceration |
|
|
Board Buzz Words:
Slapped Cheeks |
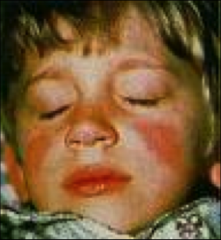
Erythema Infectiosum (fifth disease)
|
|
|
Erythema Infectiosum (fifth disease)
Cause: Incubation: Prodrome: |
Cause: Parvovirus B19
Incubation: 4-14 days but can be up to 21 days Prodrome: Mild URI symptoms for 2-3 days with rash 7-10 days later |
|
|
Erythema Infectiosum:
Characteristics of Rash |
Slapped Cheeks with circumoral pallor
Maculopapular eruption (lace-like) on proximal extensor surfaces of extremities and often to trunk, neck and buttocks, palms/soles are spared |
|
|
Erythema Infectiosum:
Complications |
Arthritis, aplastic crisis, fetal infection- hydrops fetalis (overall risk of fetal death 1-9%)
|
|
|
Boards Buzz:
What diagnosis would be appropriate for an infant with high fever followed by diffuse rash after fever subsides |
Roseola
|
|
|
Roseola :
Cause: Incubation: Prodrome: Peak Age: |
Cause: Human HerpeseVirus 6
Incubation: 5-15 days Prodrome: During period of high fever (3-4 days prior to inset of rash) Peak Age:6months to 3 years |
|
|
Roseola:
Characteristics of Rash |
Generalized erythematous, maculopapular rash;
Starts on trunk and spreads to arms and neck with less involvement of face and legs; TRUNK FIRST Color: Pink-Red Duration: 2 days Suboccipital Lymphadenopathy |
|
|
Roseola:
Complications |
Febrile Seizure
|
|
|
Boards Buzz:
Sandpaper rash and strawberry tongue |
Scarlet Fever
|
|
|
Scarlet Fever:
Cause: Incubation: Prodrome: |
Cause: GABHS
Incubation:3-5 days following pharyngitis or skin infection Prodrome: 12 hours to 2 days; fever, pharyngitis, vomiting |
|
|
Scarlet Fever:
Characteristics of Rash |
Erythematous, sandpaper texture, starts on neck, axillae, ingunal areas then spreads to rest of body
Petechiae in antecubital and axillary skin folds (Pastia’s lines) are helpful in making diagnosis Lasts 7 days then desquamates; Strawberry tongue |
|
|
Scarlet Fever:
Complications Management |
Complications: Rheumatic fever, acute glomerulonephritis
Management: Penicillin first line, erythromycin, cephalexin, or azithromycin for PCN allergic, augmentin for treatment failures |
|
|
Aplastic crisis is a complication of what condition?
What is the etiology of Roseola? What is the treatment for GAS pharyngitis/scarlet fever in PCN allergic pt? What specific lymphadenapathy can be present in Roseola? |
Aplastic crisis is a complication of what condition?
- Erythema Infectiosum What is the etiology of Roseola? -Herpesvirus 6 What is the treatment for GAS pharyngitis/scarlet fever in PCN allergic pt? -erythromycin, cephalexin, azithromycin What specific lymphadenapathy can be present in Roseola? -suboccipital |
|
|
Hand, Foot, and Mouth Disease:
-Causes -Incubation -Transmission - Prodrome |
Causes: Enteroviruses: Coxsackie virus a16, a5, a10
Incubation: 4-6 days Transmission: Exposure through enteric route: oral-oral, oral-fecal), highly contagious Prodrome: 1-2 days before rash, low-grade temperature, sore throat/mouth, malaise, lymphadenopathy |
|
|
Hand, Foot and Mouth Disease:
Characteristics of Rash |
Aphthae-like lesions anywhere in the mouth, followed by 3-7mm red macules on palms and soles
Lesions on palms/soles develop into cloudy vesicles with red halos Can also see mild peri-orbital edema |
|
|
Boards Buzz Words:
"desquamating rash, strawberry tongue, and dry, cracked lips" |
Kawasaki's Disease
|
|
|
Kawasaki's Disease:
Description Prodrome |
Mucocutaneous lymph node syndrome
Prodrome: Abrupt, high spiking fever (101-104 F) for 5 days!!!!! unresponsive to anti-pyretics Occasionally diarrhea, cough, or abdominal pain |
|
|
Kawasaki's:
Characteristics of Exanthem |
Within 3 days of fever
Bilateral bulbar conjunctival congestion Erythematous mouth and pharynx with strawberry tongue and red, cracked lips Cervical lymphadenopathy Generalized rash - morbilliform, maculopapular, scarlatiniform or may resemble erythema multiforme |
|
|
Kawasaki's:
Complications? Management? Echo dates? |
Complications: arthritis, meningitis, coronary aneurysm (20-25%)
Management: supportive care, anti-inflammatories, (IVIG and Aspirin) within first 10 days after fever Hospital Admission, serial echo (at diagnosis, 2wks, 6-8wks, 6-12 months) |
|
|
Boards Buzz:
Recent febrile illness without specific identifying sx and non-specific rash |
Non-specific Viral Exanthem
Viral Exanthem Not Otherwise Specified |
|
|
What are presentations of Viral Exanthems NOS?
|
Morbilliform or rubelliform
Vesicular Petechial (typical of echovirus 9) urticarial |
|
|
Which enterovirus is responsible for Hand, Foot, and Mouth disease?
|
Coxsackie virus a16, a5, a10
|
|
|
What is the pharmacologic therapy recommended in Kawasaki’s disease?
|
IVIG, Aspirin
|
|
|
Which disease may have a rash that resembles EM or scarlatina?
|
Viral Exanthem NOS
|
|
|
Chicken Pox (Varicella Zoster) :
Incubation Prodrome |
Incubation: 10-20 days
Prodrome: malaise low grade fever |
|
|
Varicella Zoster
Characteristics of Rash |
Develops over 3-6 day period, usually starts at hairline or face
Lesions begin as macule, papule, vesicle, then crusted vesicle Rash emerges in crops over trunk, finally the extremities |
|
|
Chicken Pox:
Complications Management |
Complications: bacterial infection of vesicular lesions, pneumonia, hepatitis, arthritis, glomerulonephritis, CNS disease
Management: Cut nails to prevent scratching Wash lesions BID with soap and water Benadryl, cold washcloth/oatmeal baths Acyclovir for high risk/immunocompromised |
|
|
Boards Buzzwords:
pearly, umbilicated, dome-shaped lesions |
Molluscum Contagiousum
|
|
|
Molluscum Contagiousum:
Transmission Appearance |
Transmission: Spread by direct skin-skin contact, autoinoculation by scratching or touching a lesion
Can spread by contact sports or fomites Dome-shaped, often umbilicated, translucent to white papules, 1mm-1cm, with tiny keratotic core Often surrounded by scaling and erythema that resemble eczema May appear inflamed and secondarily infected when undergoing spontaneous involution |
|
|
Molluscum Contagiousum:
Complications Management |
Complications: secondary infections, cosmetic issues, widespread infection in immunocompromised
Management: self-limited (most resolve in 6 months up to 4 years), curettage, cryotherapy, laser therapy, imiquimod, potassium hydroxide, cantharidin, Retin-A |
|
|
Boards Buzz:
Intertriginous, linear, severely itchy Intensely puritic rash in webs of finger |
Scabies
mite Sarcoptes scabiei results in an intensely pruritic eruption (itching worse at night) with a characteristic distribution pattern Transmission is person-person/direct contact Hypersensitivity reaction to mite, feces, and eggs |
|
|
Scabies:
Characteristics of Rash |
small, erythematous, nondescript papule, often excoriated and tipped with blood crusts
burrow is a thin, grayish, reddish, or brownish line that is 2 to 15 mm, often absent or obscured by excoriation or secondary infection Miniature wheals, vesicles, pustules, and rarely bullae may also be present |
|
|
Scabies:
Characteristics of Distribution |
sides and webs of the fingers
flexor aspects of the wrists, the extensor aspects of the elbows the skin immediately adjacent to the nipples (especially in women) the periumbilical areas, waist, male genitalia (scrotum, penile shaft, and glans) back is relatively free of involvement, and the head is spared except in very young children |
|
|
Scabies:
Management |
Management: topical permethrin, oral ivermectin, antihistamine or topical steroid for itching, transmission control (treat close contacts simultaneously
|
|
|
Tinea Capitus:
AKA description complication: |
- "ringworm of the scalp,"
- primarily affects school-aged children one or more annular patches of inflammatory or noninflammatory alopecia Complicaitons: Kerion, a severely inflammatory, boggy, indurated, tumor-like mass that may occur in tinea capitis. |
|
|
Tinea Capitus:
management |
Griseofulvin for 8 weeks
Shampoo with selenium sulfide 2-3x per week or ketoconazole |
|
|
Tinea Corporis:
Classic Presentation |
classic presentation - circular plaque with a well-demarcated red, scaly border, with central clearing
|
|
|
Tinea Corporis:
Management |
Topical Antifungals: Clotrimazole, Miconazole, Ketoconazole; may take up to 8 weeks
Oral if recurrent, unresponsive: Griseofulvin |
|
|
Tinea Pedis:
aka presentation Management |
Athletes Foot
Presentation: white, macerated areas in toe webs or chronic dry, scaly hyperkeratosis of the soles and heels MGMT: topical therapy (Lotrimin, Nyzoral), oral agents provide better skin penetration than most topical preparations: Itraconazole, terbinafine and griseofulvin are good choices for oral therapy |
|
|
How do you diagnose and Tinea infection?
|
KOH scraping of lesion boarders confirms hyphea and spores
Dermatophyte test medium: Confirms diagnosis |
|
|
Infantile Atopic Dermatitis:
Common Locations |
infantile stage may present with pruritic, red, scaly, and crusted lesions on the EXTENSORE SURFACES and CHEEKS or SCALP
acute lesions can include vesicles and there can be serous exudate in severe cases |
|
|
Childhood Atopic Dermatitis:
|
often demonstrates lichenified plaques in a flexural distribution, especially of the ANTECUBITAL and POPLIEAL FOSSAE, volar aspect of the WRISTS, ANKLES, and NECK
|
|
|
BUZZWORDS:
Rash on earlobes or front of abdomen under waistband |
Allergic contact dermatitis (ACD) -localized pruritic dermatitis after exposure to a contact allergen
The configuration and location of the dermatitis often is a clue to the offending allergen Acute – vesicles/bullae filled with clear fluid, erythematous/edematous skin Chronic – lichenified plaques with minimal erythema, minimal edema, possible scales |
|
|
An 8 y/o white male present with a 4-day h/o erthematous cheeks. Examination of the extremities reveals a mildly pruritic, reticulated, erythematous, maculopapular rash. The most likely etiologic agent is:
Human parvovirus Adenovirus Cytomegalovirus Coxsackievirus |
Human parvovirus
|
|
|
The most appropriate initial treatment for scabies in an 8 y/o male is:
0.5% malathion lotion 5% permethrin cream 5% precipitated sulfur in petroleum Trimethoprim/sulfamethoxazole orally for 10 days |
5% permethrin cream
|
|
|
A 4 y/o male has a fever of 1 wk duration around 101o F that has responded poorly to Tylenol. He has a sore throat and his lips are cracked and red. He has anterior cervical lymphadenopathy and he palms and soles are erythematous. The most appropriate management at this time would be:
Intramuscular Bicillin L-A 600,000 units Intravenous nafcillin Intravenous immune globulin and ASA Prednisone, 2-3mg/kg/day A fine-needle biopsy of the lymph nodes |
Intravenous immune globulin and ASA
|
|
|
Maternal parvovirus poses which of the following risks to the fetus?
Hydrops Laryngeal papillomas Chronic active hepatitis Seizures Pneumonia |
HYDROPS
|
|
|
The primary reason for treating uncomplicated scarlet fever is to:
Reduce the severity of acute symptoms Reduce the incidence of subsequent rheumatic fever Reduce the risk of poststreptococcal glomerulonephritis Prevent peritonsillar abscess Shorten the duration of illness |
Reduce the incidence of subsequent rheumatic fever
|
|
|
An 8 month old infant is brought to clinic by her mother with 1 week history of fever and runny nose. The mother reports that the fever “broke” yesterday, but the child awoke with a rash this morning. The rash is shown below. All of the following statements regarding the child’s condition are true except:
Associated febrile seizures are uncommon It is caused by a herpes virus Suboccipital LAD may be present Rash is initially present on chest then spreads to extremities |
Associated febrile seizures are uncommon
|

