![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
164 Cards in this Set
- Front
- Back
|
How many medullary pyramids are there in a kidney?
|
6-18 conical medullary periods
|
|
|
How many nephrons are there in a kidney?
|
1.3-1.5 million nephrons / kidney
|
|
|
Where is urine collected and drained?
|
Calyces --> Renal Pelvis --> Ureter
|
|
|
What is the precursor tissue for the urinary system?
|
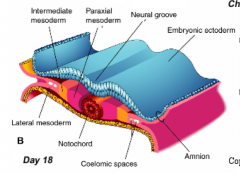
- Intermediate Mesoderm (IM) - component of the intraembryonic mesoderm (condensed mesenchyme cells)
- Endoderm (epithelium of bladder and urethra) |
|
|
Where is the Intermediate Mesoderm (IM) located?
|
In between the medial paraxial mesoderm and the laterally positioned lateral plate mesoderm
|
|
|
When does the Intermediate Mesoderm (IM) separate from the medially located Paraxial Mesoderm?
|
During folding of the embryo in the horizontal (transverse) plane
|
|
|
What kidney and gonad precursor forms from the Intermediate Mesoderm?
|
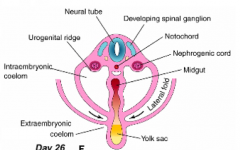
Nephrogenic Ridge or Cord - distinct ridge on posterior wall of coelom
|
|
What forms from the Nephrogenic Ridge / Cord? Where is it?
|
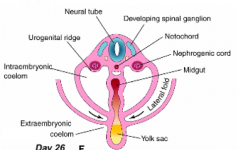
- Later called the Urogenital (UG) Ridge
- Becomes Kidney and Gonad precursors - Distinct ridge on posterior wall of coelom |
|
|
What are the implications of urinary and gonadal precursors originate from the same tissues?
|
If you have anomalies in the urinary system you will also probably have anomalies in the genital system (and vice versa)
|
|
|
What Urinary System structures are derived from Intermediate Mesoderm?
|
- Kidney
- Calyces - Renal Pelvis - Ureter - Gonads - Genital Ducts |
|
|
What Urinary System structures are derived from Endoderm?
|
Epithelial lining of urinary bladder and urethra
|
|
|
What Urinary System structures are derived from Splanchnic Mesoderm?
|
Smooth muscle and CT in walls of the components of the urinary system
|
|
|
What mediates the specification of kidney-forming ability to the Intermediate Mesoderm?
|
Signals from the Paraxial Mesoderm: transcription factors Pax2, Pax8, Lim1
|
|
|
What happens if you knock out of these transcription factors: Pax2, Pax8, and Lim1?
|
You would have abnormal kidney formation
|
|
|
What kidney structures appear along the nephrogenic ridge?
|
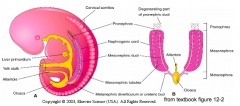
- Mesonephric Kidney
- Metanephric Kidney |
|
|
Where does the Mesonephric Kidney form?
|
- Within the Nephrogenic Ridge
- Thoracolumbar Region of embryo ("middle kidney") |
|
|
When is the Mesonephric Kidney functional?
|
Transient structure that is functional from weeks 6-12
|
|
|
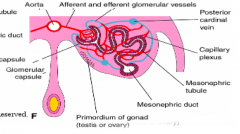
What are the two components of the Mesonephric Kidney?
|
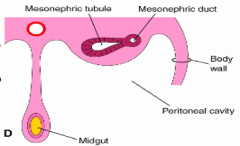
- Mesonephric Duct
- Mesonephric Tubules |
|
|
What does the Mesonephric Duct begin as? What happens to it?
|
- Solid cord of cells that extend caudally through the nephrogenic ridge on each side of embryo
- Lumen forms within duct - Duct fuses w/ the cloaca (dilated, caudal end of primitive hindgut) |
|
|
What does the lumen of the Mesonephric Duct fuse with? What is the purpose of this?
|
- Fuses with the Cloaca (dilated, caudal end of primitive hindgut)
- Serves as a transient common outlet for the UG and GI systems |
|
|
What does the Mesonephric Tubule begin as? What happens to it?
|
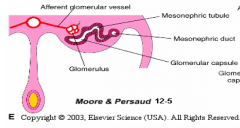
- S-shaped structure that forms at regular intervals along the nephrogenic cord
- One end is associated with a tuft of capillaries - Differentiation occurs in cranial to caudal direction along nephrogenic ridge (inductive signals from mesonephric duct) |
|
|
What are Mesonephric Tubules essentially?
|
Immature Nephrons (simple form of the mature kidney tubules)
|
|
|
What induces tubule formation of the mesonephric tubules?
|
Inductive signals from the Mesonephric Duct
|
|
|
How many mesonephric tubules form along the ridge in each kidney? How many remain in the functioning mesonephros?
|
- 40 tubules originally (not all tubules are present at the same time, many of the cranial tubules disappear before the caudal tubules form)
- 20 remain in functioning mesonephros |
|
|
What is the fate of the Mesonephric Ducts?
|
- The ducts distal to the metanephric diverticulum exhibit sexual dimorphism
- Males: forms Vas Deferens, Epididymis, Seminal Vesicles, Ejaculatory Ducts - Females: atrophies (remnant structures in the uterine mesentery) |
|
|
What is the fate of the Mesonephric Tubules?
|
- Tubules also exhibit sexual dimorphism
- Males: subset of tubules form efferent ductules - Females: atrophies (remnant structures in the ovarian mesentery) |
|
|
What parts of the Mesonephric Kidney remain in males? What does it form?
|
- Mesonephric Ducts (distal to the metanephric diverticulum) form Vas Deferens, Epididymis, Seminal Vesicles, Ejaculatory Ducts
- Mesonephric Tubules form subset of tubules form efferent ductules |
|
|
What parts of the Mesonephric Kidney remain in females? What does it form?
|
- Mesonephric Ducts atrophy (remnant structures in the uterine mesentery)
- Mesonephric Tubules atrophy (remnant structures in the ovarian mesentery) |
|
|
What structure is the precursor to the permanent kidney? Where is it located?
|
Metanephros (Metanephric Kidney) - located in the pelvic region of the embryo
|
|
|
What is the original location of the Mesonephros and the Metanephros?
|
- Mesonephros: throacolumbar region of embryo
- Metanephros: pelvic region of embryo |
|
|
What does the Metanephric Kidney form from?
|
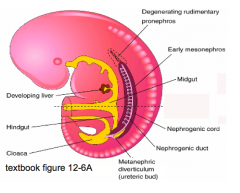
Caudal aspect of the nephrogenic cord
|
|
|
What are the precursors of the Metanephric Kidney? What tissues are they derived from?
|
- Metanephric Diverticulum (Ureteric Bud) - derivative of mesonephric duct
- Metanephrogenic Mesenchyme (Metanephric Blastema) - Both derived from Intermediate Mesoderm |
|
|
What does the Metanephric Diverticulum begin as? What happens to it?
|
- Derivative of the mesonephric duct (intermediate mesoderm)
- Buds off of the mesonephric duct as it bends medially to contact the epithelium of the cloaca - Forms the Ampulla d/t inductive signals from metanephric mesenchyme |
|
|
What does the Metanephric Mesenchyme begin as?
|
Accumulation of mesenchyme at the caudal end of the nephrogenic ridge
|
|
|
How do the precursors of the Metanephric Kidney (diverticulum and mesenchyme) interact?
|
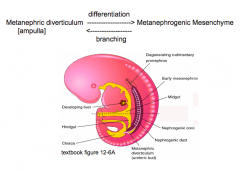
- Inductive interactions between these precursors results in formation of nephrons and a collecting system of the kidney
- Reciprocal interactions mediated by growth factors, secreted factors, and ECM molecules |
|
|
What structure forms the Ampulla? How? Function?
|
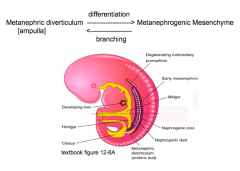
- Inductive signals cause distal end of the metanephric diverticulum to dilate and form the ampulla
- Primary source of inductive signals for nephron formation |
|
|
What can happen if the inductive signals between the metanephric diverticulum and the metanephric mesenchyme are altered or absent?
|
Renal Agenesis: absence of the kidney
|
|
|
What happens in Renal Agenesis?
|
- Inductive signals between the metanephric diverticulum and the metanephric mesenchyme are altered or absent
- Absence of the kidney(s) |
|
|
What are the types of Renal Agenesis? How common are they?
|
- Unilateral (1 / 600-1000) - usually on L side
- Bilateral (1 / 2000) |
|
|
What are the features of Unilateral Renal Agenesis?
|
- 1 / 600-1000
- Usually asymptomatic - 30-40% of children have associated anomalies in other organs - Usually on L side - Can be associated w/ a single umbilical artery |
|
|
What are the features of Bilateral Renal Agenesis?
|
- 1 / 2000
- Incompatible w/ extra-uterine life - Associated with Oligohydramnios and Pulmonary Hypoplasia - Compression of the face d/t decreased amniotic fluid → Potter's facial sequence - Associated w/ GI, heart, UG, and nervous system anomalies |
|
|
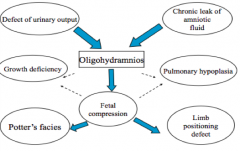
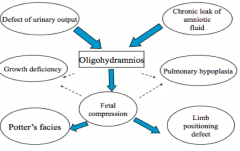
What are the abnormalities associated with the amount of Amniotic Fluid?
|
- Oligohydramnios: too little amniotic fluid
- Polyhydramnios: excessive amniotic fluid |
|
|
What can cause Oligohydramnios?
|
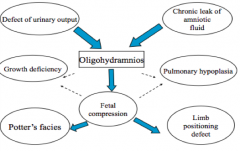
Defect of urinary output (urine = amniotic fluid)
- Renal agenesis (bilateral) - Polycystic kidney disease - Urethral obstruction Chronic amniotic leak |
|
|
What are the features of children born in association w/ Oligohydramnios?
|
1. Facial anomalies (Potter's Facies: low set ears, recessed chin, flat nose, widened subcanthal fold)
2. Limb deformities (d/t abnormal positioning) 3. Pulmonary Hypoplasia 4. Fetal growth restriction |
|
|
What can cause Polyhydramnios?
|
Most common:
- Multiple gestations Associated with: - Maternal diabetes mellitus Interference with fetus swallowing amniotic fluid: - Anencephaly - Esophageal or duodenal atresia |
|
|
What is the function of Amniotic fluid?
|
Physical Roles:
- Shock absorber - Enables fetus to move about freely, enhancing muscular development (especially limbs) - Maintains fetal body temperature - Essential for normal lung development - Barrier to infection Nutritive Role: - Source of nutrients early in development that can diffuse into embryo Excretory Role: - Assists in homeostasis by maintaining fluid and electrolytes (especially prior to keratinization of skin) |
|
|
What are the physical roles of the Amniotic Fluid?
|
- Shock absorber
- Enables fetus to move about freely, enhancing muscular development (especially limbs) - Maintains fetal body temperature - Essential for normal lung development - Barrier to infection |
|
|
What are the nutritive roles of the Amniotic Fluid?
|
Source of nutrients early in development that can diffuse into embryo
|
|
|
What are the excretory roles of the Amniotic Fluid?
|
Assists in homeostasis by maintaining fluid and electrolytes (especially prior to keratinization of skin)
|
|
|
What is the source of amniotic fluid?
|
- First 10 weeks: Amnion - interstitial fluid diffuses across the amniochorionic membrane from decidua parietalis (lining of uterus not involved in placenta formation)
- After 10 weeks: Fetus - swallows and excretes it into urine (also from tracheobronchial secretions) |
|
|
What helps direct the definitive arrangement of nephrons and collecting ducts found in the kidney?
|
Ampulla (expanded terminal end of the metanephric diverticulum)
|
|
|
When do nephrons stop forming?
|
When the ampullae disappear (~32 weeks)
|
|
|
How do kidneys grow during childhood? Are new nephrons formed?
|
- Growth of kidney during childhood is d/t elongation of nephron tubules
- No new nephrons are formed because the ampullae are gone |
|
|
How do the nephrons in mesonephros compare to metanephros?
|
Metanephros nephrons are much more complex and are also the adult nephrons
|
|
|
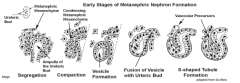
How do nephrons form?
|
1. Signals from Metanephric Mesenchyme (MM) - GDNF, RA - induce formation of Metanephric Diverticulum (MD) - receptors for GDNF
2. MD branches 3. Tips of MD expand (= ampulla) - key signaling center for nephron induction 4. Signals from ampulla direct arrangement of nephrons and collecting ducts 5. MD signals (Fgf2, Bmp7) prevent MM cell apoptosis and induces aggregation around the ampulla = COMPACTION 6. Mass of MM transforms into an epithelium bounded cavity = VESICLE FORMATION 7. Epithelial vesicle fuses w/ ampulla = FUSION OF VESICLE W/ URETERIC BUD 8. Elongates to form an S-shaped tubule = S-SHAPED TUBULE FORMATION |
|
|
What happens after ampulla formation?
|
Metanephric mesenchyme condenses around the ampulla = COMPACTION
|
|
|
What happens after metanephric mesenchyme condenses around the ampulla (Compaction)?
|
Mass of MM transforms into an epithelium bounded cavity = VESICLE FORMATION
|
|
|
What happens after the vesicle formation?
|
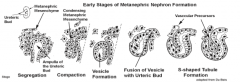
Epithelial-lined vesicle fuses w/ ampulla = FUSION OF VESICLE W/ URETERIC BUD
|
|
|
What happens after the epithelial-lined vesicle fuses w/ ampulla?
|
Elongates to form an S-shaped tubule = S-SHAPED TUBULE FORMATION
|
|
|
What results in the formation of the mature nephron?
|
Elongation and differentiation of the parts of the S-shaped tubule
|
|
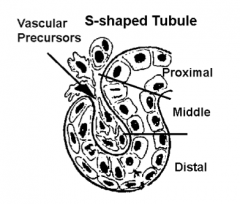
What do the proximal, middle, and distal portions of the S-shaped tubule become in the adult nephron?
|
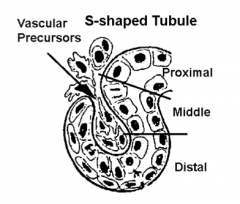
- Proximal: Distal Tubule (convoluted and straight) and Loop of Henle
- Middle: Proximal Tubule (convoluted and straight) - Distal: Double walled capsule of the Renal Corpuscle (Bowman's Capsule), invaded by capillary plexus that forms glomerulus |
|
|
What part of the S-shaped tubule forms the Distal Tubule?
|
Proximal section of S-shaped Tubule
|
|
|
What part of the S-shaped tubule forms the Loop of Henle?
|
Proximal section of S-shaped Tubule
|
|
|
What part of the S-shaped tubule forms the Proximal Tubules?
|
Middle section of S-shaped Tubule
|
|
|
What part of the S-shaped tubule forms the Renal Corpuscle?
|
Distal section of S-shaped Tubule
|
|
|
What is the origin of "vascular sprouts"? What do "vascular sprouts" become?
|
- They come from intersegmental arteries (located between somites)
- Remodel to form the blood supply to the kidney |
|
|
How do "vascular sprouts" become the blood supply of the kidney?
|
- Inductive signaling that is directing nephron formation causes the vascular sprouts to grow towards the forming kidney
- Only induced metanephrogenic mesenchyme is competent to secrete angiogenic growth factors (VEGF) that stimulate vascular sprouting |
|
|
What structures does branching of the Metanephric Diverticulum form? Which branching "generations"?
|
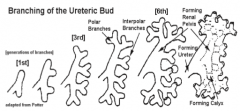
- Collecting ducts (>6th generation branches)
- Calyces (3rd-6th generation branches) - Renal pelvis (3rd-6th generation branches) - Ureter (3rd-6th generation branches) |
|
|
What are the features of branching in the Metanephric Diverticulum?
|
- Early generations branch and have little growth or elongation before next branching event occurs
- Initial branches are short - Polar end branches grow faster than central branches |
|
|
Why is the kidney, "kidney-shaped"?
|
Polar (end branches) grow faster than the central branches
|
|
|
Can you see the individual kidney lobes?
|
- Visible externally in embryo and fetus
- As kidney grows during childhood, lobes usually merge and become indistinct |
|
|
What are kidney / renal lobes?
|
Pyramidal-shaped organization of nephrons and collecting ducts
|
|
|
Are anomalies of the urinary system common? Clinically significant?
|
- They are common (3-4% of newborns have some variation or anomaly)
- But not always clinically significant |
|
|
What are some anomalies of kidney size, number, or histological organization?
|
- Hypoplastic kidneys - small, but normal (d/t abnormal development)
- Duplications - all or part of kidney or ureter - Dysplastic kidney development - cysts or primitive looking tissue arrangement |
|
|
What is the most common cause of multi-cystic kidneys?
|
Dysplastic kidney development
|
|
|
What is the outcome of bilateral dysplastic kidney development?
|
- Commonly causes multi-cystic kidneys
- Fatal post-natally w/o some sort of intervention like dialysis |
|
|
What is the term for a kidney in an abnormal location? On what side is this more common? How common in general?
|
Ectopic Kidney - more common on L side (1/800 live births)
|
|
|
In what location does a normal kidney grow? In what locations do Ectopic Kidneys grow?
|
- Normal: metanephric kidney develops in pelvis and then ascends into abdomen (because of differential growth of the embryonic body)
- Ectopic: Pelvic (60%) or Lumbar region (d/t failed or incomplete ascent to normal position in abdomen) |
|
|
What is often the reason for the presence of accessory renal arteries? How common is this?
|
Ascent of kidney from pelvis to abdomen (30%)
|
|
|
How common is a "horseshoe kidney"? What causes this?
|
- 1 / 425-600 live births
- Often occurs because of fusion of the caudal poles of the kidney - Ascent to normal position is blocked by inferior mesenteric artery - May be associated with additional anomalies |
|
|
What happens in "Crossed Renal Ectopia"?
|
- Both kidneys are located on the same side of the body
- They may fuse or remain unfused |
|
What is the term for both kidneys being on the same side of the body?
|
Crossed Renal Ectopia
|
|
|
What are the possible causes (differential diagnosis) of a R flank mass in an infant?
|
- Hydronephrosis (obstruction of urinary tract)
- Cystic kidney disease (polycystic or multicystic dysplastic) - Renal tumor (rare) |
|
|
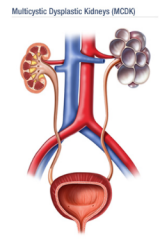
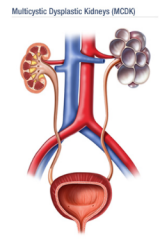
Does multicystic dysplastic kidney disease affect one or both kidneys? Polycystic?
|
- Multicystic - usually unilateral (bilateral is rare and fatal)
- Polycystic - bilateral |
|
|
What are the gross features of Multicystic Dysplastic Kidney Disease?
|
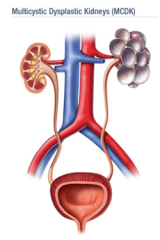
- Multiple cysts of varying sizes on one of the kidneys
- Contralateral (normal) kidney hypertrophies to compensate for lost functional kidney mass |
|
|
What are the pathologic features of Multicystic Dysplastic Kidney Disease?
|
- Primitive ductules and cartilage
- Atretic ureter (abnormally closed or absent) |
|
|
What other abnormalities are associated with Multicystic Dysplastic Kidney Disease?
|
- 28% have vesicoureteral reflux in contralateral kidney (movement of urine from bladder → ureters → kidney)
- Hypertension (potential complication) |
|
|
What happens to the diseased kidney in Multicystic Dysplastic Kidney Disease? How do you treat this?
|
- Usually regresses on its own
- If it does not regress by the time they are a toddler, a nephrectomy is indicated |
|
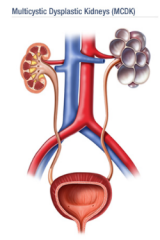
Is Multicystic Dysplastic Kidney Disease caused by a genetic abnormality?
|
No, non-genetic
|
|
|
What are the types of congenital polycystic kidney disease? How common are they?
|
- Autosomal Recessive Polycystic Kidney Disease (ARPKD) - 1 / 6000-14,000 live births
- Autosomal Dominant Polycystic Kidney Disease (ADPKD) - 1 / 1000 live births |
|
|
What are the morphological features of Autosomal Recessive Polycystic Kidney Disease?
|

- Kidney contains enlarged cortical cysts
- 90% of collecting tubules are dilated - Normal reniform (kidney-bean) shape persists |
|
|
What are the outcomes of Autosomal Recessive Polycystic Kidney Disease depending on the age of onset?
|

- Manifested in newborns (most common): fatal
- Manifested in infants or children: develop liver problems, HTN, CHF - Manifested in adults: develop liver fibrosis and portal HTN |
|
|
What are the morphological features of Autosomal Dominant Polycystic Kidney Disease?
|
- Cysts are located in cortex and medulla
- Bilateral enlarged kidneys |
|
|
When do patients become symptomatic from Autosomal Dominant Polycystic Kidney Disease?
|
30s-50s (but can occur in children)
|
|
|
What mutations cause Autosomal Dominant Polycystic Kidney Disease?
|
Mutations on two genes on chromosome 16: PKD1 and PKD2
|
|
|
What happens if someone has mutations in PKD1 or PKD2 on chromosome 16?
|
- Loss of function of the primary cilium on renal tubular epithelial cells
- These proteins (polycystin 1 and 2) may be part of the signaling pathway that regulates renal tubular size and growth |
|
|
What are the outcomes of Autosomal Dominant Polycystic Kidney Disease?
|
- 50% develop HTN
- 33% develop berry aneurysms on their internal carotid arteries - 80% develop intestinal diverticulosis |
|
|
What kind of kidney neoplasm is common in children? What gene is involved? How common?
|
- Nephroblastoma (Wilm's Tumor)
- Wilm's tumor gene, Wt-1, is on chromosome 11p1 - 1 / 15,000 live births |
|
|
What part of the kidney does Nephroblastoma (Wilm's Tumor) affect?
|
- Early onset occurs in medulla
- Later progresses to cortex |
|
|
What is Nephroblastoma (Wilm's Tumor) associated with?
|
- Horseshoe kidney
- May be associated with other anomalies and certain syndromes |
|
|
What causes Hydronephrosis? What does it result in?
|
- Caused by obstruction of urinary flow, usually at the ureter-pelvic junction (UPJ)
- Leads to distention of the renal pelvis and calyces |
|
|
What is the most frequent cause of a neonatal abdominal mass?
|
Hydronephrosis
- Caused by obstruction of urinary flow, usually at the ureter-pelvic junction (UPJ) - Leads to distention of the renal pelvis and calyces |
|
|
What can enhance an obstruction in the urinary tract?
|
- Diuresis (increased water excretion)
- Eg, EtOH |
|
|
What symptoms in an infant would make you believe they had a Utero-Pelvic Junction obstruction (Hydronephrosis)?
|
- Flank mass
- UTI - Failure to thrive - Sepsis |
|
|
What symptoms in an older child or adult would make you believe they had a Utero-Pelvic Junction obstruction (Hydronephrosis)?
|
- Flank pain
- Colicky pain - UTI - Hematuria |
|
|
How can you diagnose a Utero-Pelvic Junction obstruction (Hydronephrosis)?
|
- Ultrasound (anatomy)
- Renal scan - IV pyelogram (functional study) |
|
|
How does the Cloaca get subdivided?
|

Urorectal Septum (wedge of mesoderm located between alantois and hindgut)
|
|
|
What is the function of the Urorectal Septum?
|

- Subdivides the cloaca into UG Sinus (ventral) and Anorectal Canal (dorsal)
- Expands ventrally to fuse w/ the cloacal membrane (driven by embryo growth and caudal folding in sagittal plane) |
|
|
What forms the perineal body?
|
Area between the Urorectal Septum and the Cloacal Membrane
|
|
|
What separates the cloaca from communicating with the amniotic cavity?
|

Cloacal Membrane - fusion of ectoderm and endoderm that covers the ventral surface of the cloaca
|
|
|
What does the Cloacal Membrane cover?
|

- Covers the ventral surface of the cloaca
- Extends from the Allantoic Stalk to the Tailbud |
|
|
When does the Cloacal Membrane rupture? Why?
|

- Ruptures around day 49
- Caused by apoptosis and pressure from urine in Amniotic Cavity - Results in distinct openings for the UG tract and the GI tract |
|
|
What are the subdivisions of the UG Sinus?
|

- Cranial / Vesicle part (aka vesicourethral canal)
- Middle / Pelvic part - Caudal / Phallic part (Sometimes pelvic and phallic parts are grouped together as the definitive UG sinus) |
|
|
What part of the UG sinus do the Mesonehpric Ducts open into?
|

Cranial / Vesicle part (aka vesicourethral canal)
|
|
|
What happens to the pelvic and phallic parts of the UG sinus?
|

- Pelvic (middle) part narrows
- Phallic (caudal) part flattens and is pulled ventrally as the genital tubercle elongates |
|
|
What develops from the cranial part of the vesicle of the UG sinus?
|

- Urinary bladder
- Part of the urethra |
|
|
What is the vesicle part of the UG sinus continuous with?
|

Cranially it is continuous with the regressing allantois
|
|
|
What is the cranial extension of the forming urinary bladder called?
|
Urachus
|
|
|
What is the urachus?
|
Cranial extension of the forming urinary bladder
|
|
|
Eventually, what happens to the urachus and alantois?
|
- Narrow to a fibrous cord called the Median Umbilical Ligament
- Inner surface of the ventral wall of the abdomen - Ligament tracks from the apex or cranial surface of the urinary bladder to the umbilicus |
|
|
What are the origins of the components of the urinary bladder?
|
- Cranial part of UG Sinus (forms bladder and part of urethra) - intermediate mesoderm
- Lining derived from endoderm - Smooth muscle and CT in wall derived from surrounding splanchnic mesoderm |
|
|
What forms the ureters?
|

Metanephric Diverticula (Ureteric Bud)
|
|
|
What opens into the vesicle part of the UG sinus?
|

- Caudal end of the mesonephric ducts
- Metanephric diverticula (forming ureters) |
|
|
What happens to the mesonephric ducts in relation to the urinary bladder?
|

- Ends exstrophy (expand and flatten)
- Greater superiorly, causes the ureters to open into the forming urinary bladder - Distal end of ducts appear as if they are moving caudally and open into pelvic portion of UG sinus - They also move closer together |
|
|
Where are the openings of the ureters in relation to the mesonephric ducts?
|

Lateral and superior to the mesonephric ducts
|
|
|
What is the thickened triangular area of the posterior bladder that is bounded by the openings of the ureters and urethra?
|

Trigone of Urinary Bladder
|
|
|
What is the Trigone derived from?
|

- Extrophied mesonephric duct distal to the metanephric diverticulum (mesodermal origin)
- Internally the trigone is overgrown by endoderm |
|
|
What do the derivatives of the mesonephric ducts in males drain into?
|

Form components of the male reproductive system that empty into the prostatic urethra
|
|
|
What happens to the bladder after birth?
|
Bladder descends and drags the cord-like median umbilical ligament (derived from urachus and alantois) with it
|
|
|
What does the caudal portion of the vesicle part of the UG sinus form?
|

Contributes to the forming urethra
|
|
|
How is the urethral primordium sexually dimorphic?
|
- Males: only the proximal part of the prostatic urethra is formed from the vesicular part of the UG sinus
- Females: most of the urethra is derived from the vesicular part of the UG sinus |
|
|
What forms from the pelvic part of the UG sinus?
|
- Males: epithelium of Distal Prostatic and Membranous Urethra
- Females: epithelium of lower half of vagina |
|
|
What forms from the phallic part of the UG sinus?
|
- Males: epithelium of Penile Urethra
- Females: epithelium of the vestibule |
|
|
What do the portions of the UG sinus form in females?
|
- Vesical: most of the urethra
- Pelvic: epithelium of lower half of vagina - Phallic: epithelium of vestibule |
|
|
What do the portions of the UG sinus form in males?
|
- Vesical: epithelium of Proximal Prostatic Urethra
- Pelvic: epithelium of Distal Prostatic Urethra and Membranous Urethra - Phallic: epithelium of Penile Urethra |
|
|
What are the types of anomalies that are associated with the Urinary Bladder?
|
- Urachal anomalies
- Exstrophy of the bladder |
|
|
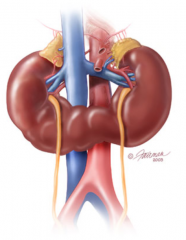
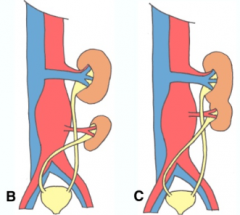
What are the Urachal Anomalies of the Urinary Bladder? Cause?
|

- Urachal cysts (C)
- Vesical diverticulum (B) - Vesico-umbilical fistula (A) - Failure of regression of the urachus and alantois |
|
|
What kind of anomaly is a Urachal Cyst? What causes them?
|

- Type of urachal anomaly of the urinary bladder
- Derived from epithelial lining of the urachus - Caused by failure of regression of urachus (C) |
|
|
What kind of anomaly is a Vesical Diverticulum? What causes them?
|

- Type of urachal anomaly of the urinary bladder
- Communication between bladder and a remnant of the urachus (B) - Caused by failure of regression of urachus |
|
|
What kind of anomaly is a Vesico-Umbilical Fistula (aka Patent Urachus)? What causes them?
|
- Type of urachal anomaly of the urinary bladder
- Communication of bladder w/ the umbilicus d/t patency of the urachus and alantois; with this condition urine at umbilicus is possible (A) - Caused by failure of regression of urachus |
|
|
What does the term exstrophy mean?
|
Eversion of a hollow organ so that its epithelial lining is exposed to the surface of the body or the inside of an organ
|
|
|
What happens in Exstrophy of the Urinary Bladder? What is it associated with?
|
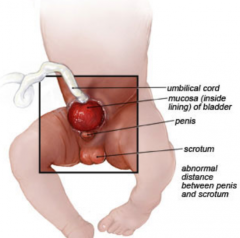
- Mucosal lining of the posterior bladder wall is exposed on the ventral abdominal wall
- Males: often associated w/ Epispadias (dorsal opening of penile urethra) - Females: often associated w/ a shortened vagina and a bifid clitoris - Also associated w/ UG and skeletal anomalies (separation of pubic bones) - 1 / 30,000 - 50,000 live births and 3.5x more common in males |
|
|
What causes Bladder Exstrophy?
|
Failure of medial mesenchymal migration
|
|
|
What happens in Exstrophy of the Cloaca?
|
- More severe form of Exstrophy of Urinary Bladder
- Also includes Omphalocele (abdominal organs protrude into umbilical cord), impeforate anus, and spinal anomalies - 1 / 250,000 births |
|
|
What is Epispadias? What is it associated with?
|
Dorsal opening of penile urethra - associated with males with Exstrophy of the bladder
|
|
|
How should Bladder Exstrophy be treated? What are the complications?
|
- Surgery performed shortly after birth
- Babies hospitalized 10-14 days - Incontinence is a major long term issue; upper tracts at risk after repair |
|
|
What happens in Primary Ureteral Reflux? Cause?
|
- Backing up of urine from bladder into ureter and kidney
- Occurs when ureter enters bladder abnormally in a more lateralized position - Leads to loss of tunneling of ureter within wall of bladder - May be related to abnormal location of metanephric diverticulum (ureteral bud) coming off of mesonephric duct |
|
|
What are the complications of Primary Ureteral Reflux?
|
- Allows bacteria to have ascending access to kidneys, and thus is a risk for developing pyelonephritis (kidney infection)
- Also may cause subsequent atrophy of the kidney |
|
|
What is associated with a higher grade of ureteral reflux?
|
- Greater risk for scarring
- More abnormal anatomy - Spontaneous resolution less likely - Surgical intervention may be necessary |
|
|
How should you treat primary ureteral reflux?
|
- Antibiotic prophylaxis and/or
- Surgical repair |
|
|
What are the anomalies associated with the ureter
|
- Duplications
- Ectopic Ureter - Megaureter - Ureterocele |
|
|
What happens in a Ureter Duplication?
|
- All or part of ureter may be duplicated
- Most ar partial, with each ureter draining a separate pelvic coordinating system and then joining distally before entering bladder - Can be unilateral or bilateral |
|
|
What happens in an Ectopic Ureter?
|
- When ureter duplication is complete, one may empty into vagina, urethra, uterus, seminal vesicles, verumontanem (median elevation of prostatic urethra), or ejaculatory ducts
- Ureter than inserts ectopically is always the one that drains the more superior part of the kidney - If the ureter does not have a sphincter, it may lead to continuous dribbling |
|
|
When there is a complete duplication of a ureter, what part of the kidney does it attach to? How do you know which is the ectopic ureter?
|
- It drains more superior part of kidney
- It is inserted into vagina, urethra, seminal vesicles, verumontanem, or ejaculatory ducts |
|
|
What happens in a Megaureter? Cause?
|
- Obstructred and enlarged ureter w/ a normal insertion site and orifice
- Distal ureter is adynamic - functionally obstructed d/t abnormal orientation of smooth muscle in wall |
|
|
What happens in Ureterocele?
|
- Dilation of terminal ureter as it enters bladder d/t small ureter orifice
- More common in females and often associated w/ ureter duplication - Often causes obstruction of affected ureter |
|
|
What kind of anomaly causes a ureter to drain into the vagina, uterus, seminal vesicles, verumontanem, or ejaculatory ducts?
|
Ectopic Ureter
|
|
|
What kind of anomaly is caused by an abnormal orientation of the smooth muscle in the wall of the ureter? Outcome?
|
Megaureter - leads to obstructed and enlarged ureter w/ a normal insertion site and orifice
|
|
|
What kind of anomaly is associated w/ a dilation of the terminal ureter as it enters the bladder d/t a small ureter orifice?
|
Ureterocele
|
|
|
What are the anomalies associated with the Urethra?
|
- Agenesis / Atresia
- Posterior Urethral Valves |
|
|
What happens if there is agenesis or atresia of the urethra? Who more commonly gets it?
|
- Obstruction of urine flow
- Development of prune belly (wrinkling of abdominal wall) d/t atresia of ventral abdominal wall muscles - More common in males |
|
|
What are posterior urethral valves?
|
- Urethral anomaly
- Tissue folds of posterior urethra mucosa that act like valves and obstruct the urethra |
|
|
What happens if there are posterior urethral valves? Who can get this?
|
- Most common cause of uropathy leading to renal failure in children (irreversible renal dysplasia)
- Tissue folds of posterior urethra mucosa act like valves and obstructs the urethra - Only found in MALES (1/5000 live births) |
|
|
What is a common cause of renal failure in boys?
|
Posterior Urethral Valves - tissue folds of posterior urethral mucosa that act like valves and obstruct the urethra
|

