![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
39 Cards in this Set
- Front
- Back
|
Which 2 areas of the GI tract are under voluntary control? |
- UOS - external anal sphincter |
|
|
Which cells mediate enteric neurotransmission |
- cells of Cajal |
|
|
Which 2 external factors have excitatory and inhibitory contol over the enteric nervous system? |
- vagal control (excitatory) - sympathetic control (inhibitory) |
|
|
What muscle layers are present in the oesophagus? |
- inner circular - outer longitudinal |
|
|
What oesophageal disorder is associated with an impaired ability of the LES to open when swallowing? |
- achalasia |
|
|
What is nutcracker/jackhammer oesophagus? |
- condition of hypertensive peristalsis |
|
|
What is meant by the interprandial period and fed state? |
- interprandial period: the period between meals - fed state: the period where food is being digested |
|
|
What is the purpose of the interprandial period? How often does it happen? What hormone regulates it? |
- cleanse the stomach and intestines - every 90 minutes - motilin |
|
|
What are the 4 phases of the interprandial period? |
- 1: prolonged period of quiescence - 2: increase frequency of contractility - 3: few minutes of peak electrical and mechanical activity - 4: declining activity as it approaches the nect cycle |
|
|
What cells produce motilin? Where is it produced? |
- M cells - small intestine |
|
|
What are the 3 phases of digestion? |
- cephalic, gastric and intestinal |
|
|
Which nerve regulates the cephalic phase? What percentage of gastric secretin is produced during this phase? |
- vagus nerve - 20% |
|
|
What physical changes occur in the stomach during the gastric phase (2)? |
- stomach expands (without an increase in pressure) - migrating motility complex is replaced by contractions of variable amplitude and frequency |
|
|
How long does it take for the stomach to empty following a meal? |
- 20 mins for inert liquids - 3-4 hours for solids |
|
|
Give 2 conditions associated with accelerated gastric emptying |
- dumping syndrome - diarrhoea |
|
|
Give 3 symptoms of delayed gastric emptying |
- abdominal pain - nausea and vomiting - weight loss |
|
|
Give three causes of delayed gastric emptying |
- diabetes with microvasscular disease - drugs (e.g. opiates) - post-viral |
|
|
What dietry adjustments could be made to help manage delayed gastric emptying (3)? |
- small meals - more liquid food (better tolerated) - nutritional support |
|
|
What type of medications are used to treat delayed gastric emptying? Give 3 examples. |
- Prokinetics - 5HT4 agonists, D2 anatagonists, motilin agonist (erythromycin) |
|
|
Give 2 surgical treatments for delayed gastric emptying |
- endoscopic injection of botulinum toxin - gastric electrical emptying |
|
|
What type of GI motility is active during fasting? |
- migrating motility complex |
|
|
What is chronic intestinal pseudo-obstruction of the small bowel? Give 4 symptoms Broadly, state its causes |
- condition where there is signs of mechanical obstruction - though without actual mechanical obstruction - chronic abdomina pain, constipation, vomiting, weight loss - neuropathy or myopathy (primary); other diseases (secondary) |
|
|
What is acute post-operative ileus (3)? |
- occurs after abdominal surgery - results in constipation and intolerance or oral intake - not due to mechanical obstruction |
|
|
How long does physiological ileus last for in the stomach, small intestine and colon, respectively |
- stomach: 24-48 hours - small intestine: 0-25 hours - colon: 48-72 hours |
|
|
Give 5 risk factors associated with prolonged ileus |
- open surgery (rather than laproscopic) - duration of abdominal/pelvic surgery - delayed enteral nutrition - complications during surgery - opiates |
|
|
Describe acute colonic psuedoobstruction |
- also known as Ogilvie's syndrome - caused by large bowel parasympathetic dysfunction - causes symptoms associated with mechanical obstruction, though without actual obstruction: abdominal pain, nausea, severe distension, vomiting, dysphagia, diarrhea and constipation - in severe cases can cause caecal perforation |
|
|
Give 6 ways of managing acute colonic pseudo-obstruction |
- gut rest - IV fluids - nasogatric decompression (uses suction to empty stomach) - colonoscopic decompression (uses suction to empty colon) - IV neostigmine (acetylcholinesterase inhibitor) - surgery |
|
|
Give 1 example of chronic intestinal psuedo-obsruction caused by myopathy, neuropathy, endocrine and drugs |
- myopathic: scleroderma - neuroathic: Parkinson's - endocrine: Diabetes - drugs: anti-parkinsonian drugs |
|
|
What is the differnce between enteral and parenteral feeding? |
- enteral: via the GI tract (preferred) - parenteral: venous |
|
|
What is the name of the reflex which occurs in the colon after a meal? - how long is transit from the caecum to the rectum? - why is faecal weight hgher in men? |
- gastrocolic reflex (increase in colonic activity) - 1-2 days - transit time is shorter in men: means there is a higher water content |
|
|
How would you measure colonic transit? |
- serial X-rays using radio-opaque markers |
|
|
Give examples of 3 types of drugs which reduced gastric motility |
- opiates (via Mu receptor) - anti-cholinergics |
|
|
Give an example of a opiate which is used to reduce gastric motility Briefly describe how it works |
- loperamide (immodium) - gut selective opiate Mu receptor agonist. - decreases the tone and activity of the myenteric plexus - slows transit whcih increases water absorption |
|
|
Describe the drug, prucalopride |
- gut selective 5HT4 agonist - increases colonic (and other gut) motility |
|
|
Describe the drug, linaclotide |
- guanylate C receptor agonist - increase secretion of chloride and bicarbonate, which increases intestinal fluid, and increases colonic transit |
|

|
|
|
|
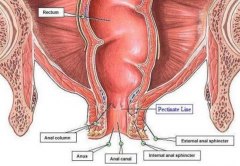
Describe the difference between the interanal and external anal sphincters |
- internal: smooth muscle (involuntary); contracted during rest external: skeletal msucle (voluntary); recruited in reflex to coughing/sneezing |
|
|
Give 2 causes of faecal incontinence with examples |
- excessive rectal distension: acute or chronic diarrheoa, chronic constipation - anal sphincter weakness: sphincter damage, damage to the pudendal nerve |
|
|
Other than medications, give causes of anorectal constipation |
- Hirschrung's disease (children) - obstructive defacation (parodoxical contraction of the puborectalis muscle and externa sphincter during defacation) - rectocoele (prolapse between the reectum and vagina) - anal fissures (due to pain) |

